Abstract
Aims
To determine ambulance transport rates and investigate predictors for ambulance use by patients with acute myocardial infarction (AMI) in Australia.
Methods
A prospective, cross‐sectional descriptive survey using structured interviews. It included patients who were admitted to two hospitals (Western, Bendigo, Melbourne, Victoria, Australia) with AMI between 1 October 2004 and 31 March 2005, and data were collected by semistructured interview and medical record review. Data were analysed by descriptive statistics, univariate and multivariate analysis using SPSS.
Results
105 patients were interviewed. 48 (46%) participants called for an ambulance as their initial medical contact. Participants who called for an ambulance had a shorter interval between symptom onset and presentation to hospital than those who did not (non‐ambulance participants)(median 2.1 v 7.8 h; p = 0.001). Predictors of ambulance transport were older age (p = 0.008), symptom onset on the weekend (p = 0.022), presence of sharp chest pain (p = 0.011), self‐administered anginine (p = 0.007), symptom onset at home (p = 0.027) and having a lower income (<$A20 000; p = 0.022). After multivariate analysis, self‐administered anginine, sharp chest pain and occurrence of symptom onset at home remained as independent predictors of ambulance use.
Conclusion
A substantial number of patients do not call for an ambulance as their first medical contact after the onset of AMI symptoms. Public education on the benefits of ambulance transport and early treatment, as well as recognition of AMI symptoms, is required.
Coronary heart disease (CHD) remains one of the world's greatest health problems,1 and is the leading cause of premature death and disability for Australian men and women.2 After acute myocardial infarction (AMI), the time to reperfusion treatment for appropriate cases is the key factor in determining survival and quality of life.3,4,5 Minimising delays to treatment remains a priority for emergency services in the setting of AMI.
Patient delay, the time between the onset of symptoms and the patient's decision to seek care, represents the most important factor in delay to treatment.6,7,8,9,10,11 It has been reported that a large proportion of patients (48%) with AMI die before accessing health services.12
Use of ambulance transport expedites definitive medical care, usually reperfusion treatment, for patients with AMI.13,14,15 However, it has consistently been shown that ambulance transport rates for patients with AMI are low (45–73%).6,16,17,18
Several studies have tried to determine why patients with AMI do not use ambulance transport (non‐ambulance participants).7,17,18 They report the main problems as patient's belief that the symptoms are not severe enough to warrant calling for an ambulance, and believing that self‐transport will be quicker. Australian data suggest that patients with AMI have longer delays from onset of pain to presentation to hospital when compared with patients from other countries (US, Japan, UK and South Korea).19
To date, there are no Australian data specifically investigating reasons for non‐ambulance use by patients with AMI. This study aimed to establish current ambulance transport rates and to identify predictors for ambulance transport use by patients with AMI in Australia.
Method
This prospective, cross‐sectional survey was conducted between 1 October 2004 and 31 March 2005. The study population consisted of consecutive patients with AMI admitted to either Western or Bendigo Hospitals, Melbourne, Victoria, Australia. Western Hospital is a 320‐bed adult teaching hospital in metropolitan Melbourne with an emergency department census of 34 000 patients a year. Bendigo Hospital is a large rural hospital with 200 beds and an emergency department census of 35 000 patients a year.
Screening all coronary care unit admissions via presentation to the emergency department with presumed AMI was used to identify eligible participants. Patients were eligible for inclusion to the study if they had a primary diagnosis of AMI (confirmed during hospitalisation based on increase in troponin I levels and electrocardiography changes, and affirmed by the treating cardiologist) and were living independently before admission to hospital. Admission to hospital was chosen as the criterion to limit the sample to patients who had control over when and whether an ambulance was called. Patients were excluded if they did not speak English and an interpreter was not available, if AMI onset occurred after hospitalisation with another clinical presentation, if their clinical condition (as judged by treating clinicians) did not permit them to be interviewed or if they did not consent to participate.
Data were collected using semistructured interviews and reviewing medical records. No validated survey instrument was available, hence an instrument was developed based on data collected in similar studies.17,18 The survey was piloted on 10 patients before starting the study and was modified accordingly.
Consenting eligible patients were interviewed by trained researchers during hospitalisation and within a week of presenting to hospital. Information collected included demographics, place and time of onset of symptoms, presence of other people, first medical contact (ambulance, general practitioner or hospital), characteristics of chest pain, self‐management, prior knowledge of AMI symptoms and main reason for going to hospital. We also collected personal information, including income and employment status, educational level, and health insurance and ambulance service subscription. Documentation in the medical history of an ischaemic heart disease (IHD) event, including AMI, coronary intervention (coronary artery bypass grafts and percutaneous transluminal coronary angioplasty) and angina, was noted and categorised as previous IHD event. Validation of IHD diagnosis was not confirmed.
Patients who were not transported by ambulance directly from place of onset of symptoms to hospital were asked the specific question “Why did you not come to hospital by ambulance?” In addition, all participants were asked “What was the reason for you coming to hospital?” Medical records were used to obtain data relating to clinical presentation (characteristics on electrocardiography, time of presentation to hospital and risk factors for CHD). We categorised interviewed patients into two groups: those who called an ambulance as their first medical contact (ambulance) and those who did not (general practitioner first, driven or drove themselves).
For patients who refused to participate in the interview or who were discharged before being approached about participation in the study, de‐identified demographic data (age, sex and hospital) was collected. This was carried out to determine whether the study sample was representative of the broader population with AMI.
Data were analysed using SPSS V.11.1.1, and are presented as descriptive statistics, and univariate and multivariate analyses. Non‐parametric tests (Mann–Whitney U test) were used for comparison of age, distance to hospital and prehospital delay (onset of symptoms to arrival at hospital). Factors included in the multiple logistic regression analysis were those that achieved univariate significance at p<0.2. Responses to the question about why patients did not call for an ambulance were assessed qualitatively and grouped into common themes.
Human research ethics committees of Bendigo Health Care Group and Melbourne Health, Australia, approved the study, and no external funding was used.
Results
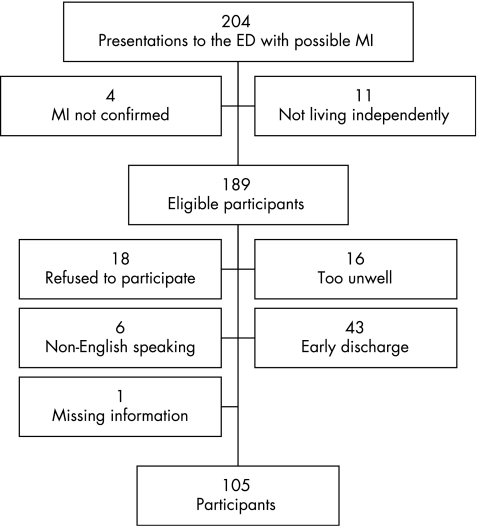
Over the study period, there were 204 presentations to the emergency department with presumed AMI who were admitted to the coronary care unit. After exclusions, the final sample consisted of 105 participants. Figure 1 shows the derivation of the sample used in this study. We compared our sample (n = 105) with eligible non‐participants (n = 83) for age, sex, ambulance use and hospital of presentation. Participants were more likely to be younger (median 64 years) than non‐participants (median 69 years; p = 0.042), but there were no significant differences for hospital of presentation (participants 28% v non‐participants 27%), ambulance use (67% v 76%) or female sex (28% v 38%).
Figure 1 Flow chart showing the derivation of the sample used in this study. ED, emergency department; MI, myocardial infarction.
Only 46% (48/105) of the study sample called for an ambulance as their first medical contact. Table 1 shows the comparisons of demographics and personal information. Ambulance users were older (median 70 years v 57 years; p = 0.008) and more likely to earn <$A20 000 per annum (75% v 53%; p = 0.022) compared with non‐ambulance users. Participants with ambulance cover used ambulance transport more often (90% v 75%; p = 0.061), but this was a non‐significant trend.
Table 1 Comparison of demographic information for ambulance and non‐ambulance participants.
| Variable (n = 105) | Ambulance (48) | Non‐ambulance (57) | p Value |
|---|---|---|---|
| n (95% CI or %) | n (95% CI or %) | ||
| Age (years) | |||
| Range | 38–84 | 25–84 | 0.008 |
| Median | 70 | 57 | |
| Distance to hospital (km) | |||
| Range | 1–50 | 1–140 | 0.765 |
| Median | 9.5 | 10.5 | |
| Male sex | 31 (64.6) | 44 (77.2) | 0.154 |
| Australian born | 28 (58.3) | 26 (45.6) | 0.194 |
| English language spoken | 43 (89.6) | 45 (78.9) | 0.141 |
| Lives with other | 33 (68.8) | 47 (82.5) | 0.1 |
| Married | 29 (60.4) | 42 (75.0) | 0.111 |
| Private health insurance | 8 (16.7) | 10 (17.8) | 0.873 |
| Western Hospital | 35 (72.9) | 40 (70.2) | 0.757 |
| Income <A$20,000 per annum | 35 (74.5) | 30 (52.6) | 0.022 |
| Ambulance cover | 43 (89.6) | 43 (75.4) | 0.061 |
| Employment | |||
| Retired | 35 (72.9) | 33 (57.9) | 0.268 |
| Blue collar (eg, trade, factory) | 11 (22.9) | 21 (36.8) | |
| White collar (eg, office) | 2 (4.2) | 3 (5.3) | |
| Educational level | |||
| Secondary | 29 (60.4) | 28 (50.9†) | 0.423 |
| Presecondary | 13 (27.1) | 13 (23.6) | |
| Undergraduate/trade | 5 (10.4) | 11 (20.0) | |
| Postgraduate | 1 (2.1) | 3 (5.4) | |
| Prior knowledge | |||
| Chest pain | 38 (79.2) | 40 (70.2) | 0.294 |
| Nausea/vomiting | 5 (10.4) | 9 (15.8) | 0.420 |
| Neck pain | 8 (16.7) | 6 (10.5) | 0.356 |
| Arm pain | 23 (47.9) | 21 (36.8) | 0.252 |
| Jaw pain | 8 (16.7) | 9 (15.8) | 0.903 |
| Shortness of breath | 14 (29.2) | 14 (24.6) | 0.595 |
| Collapse | 4 (8.3) | 3 (5.3) | 0.530 |
†Information missing for two cases.
Prior knowledge of AMI symptoms seemed to have no effect on the patient's decision to call an ambulance. Most participants (n = 78, 74%) were aware of chest pain as a warning sign for AMI, but were less aware of other typical signs, including sweating (n = 4, 3.8%), nausea or vomiting (n = 14, 13.3%) and shortness of breath (n = 28, 26.7%). Prior IHD event (44% v 28%; p = 0.094) and AMI (19% v 19%; p = 0.844) did not increase the likelihood of ambulance transport for participants.
Prehospital delay was shorter for those who came directly by ambulance (median 2.1 v 7.8 h; p = 0.001).
Table 2 compares the characteristics related to the AMI event on univariate analysis. Participants were more likely to call for an ambulance if symptom onset was on the weekend (33% v 14%; p = 0.022), if symptom onset occurred at home (85% v 67%; p = 0.027), if chest pain was “sharp” in nature (25% v 7%; p = 0.011) or if they had self‐administered anginine (27% v 7%; p = 0.007). A trend was shown for time of onset of symptoms, with increased ambulance usage outside standard general practitioner hours (weekend and between the hours of 17:00 and 07:59; (83% v 68%; p = 0.054), but this did not achieve significance.
Table 2 Comparison of variables relating to acute myocardial infarction event for ambulance and non‐ambulance users.
| Variable | Ambulance (48) | Non‐ambulance (57) | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| After hours (presentation on weekendor between 17:00 and 07:59) | 40 (83.3) | 39 (68.4) | 0.054 |
| Weekend | 16 (33.3) | 8 (14.3) | 0.022 |
| Risk factors | |||
| Smoking | 21 (43.8) | 34 (59.6) | 0.104 |
| Hypertension | 28 (58.3) | 31 (54.4) | 0.685 |
| Lipids | 21 (43.8) | 25 (43.9) | 0.991 |
| Family history | 18 (37.5) | 18 (31.6) | 0.524 |
| Overweight | 14 (29.2) | 12 (21.1) | 0.337 |
| Diabetes | 10 (20.8) | 15 (26.3) | 0.511 |
| Previous IHD event | 21 (43.8) | 16 (28.1) | 0.094 |
| Prior AMI | 9 (18.8) | 11 (19.3) | 0.844 |
| Type of symptoms | |||
| CP | 34 (70.8) | 43 (75.4) | 0.595 |
| Nausea | 17 (35.4) | 22 (38.6) | 0.737 |
| Vomiting | 12 (25.0) | 6 (10.5) | 0.05 |
| Neck pain | 9 (18.8) | 7 (12.3) | 0.358 |
| Dizziness | 8 (16.7) | 6 (10.5) | 0.356 |
| Arm pain | 26 (54.2) | 30 (52.6) | 0.875 |
| Shortness of breath | 18 (37.5) | 25 (43.9) | 0.509 |
| Sweating | 16 (33.3) | 18 (31.6) | 0.848 |
| CP type* | |||
| Tightness | 10 (20.8) | 10 (17.5) | 0.669 |
| Dull | 2 (4.2) | 6 (10.5) | 0.221 |
| Heavy | 10 (20.8) | 12 (21.1) | 0.978 |
| Sharp | 12 (25.0) | 4 (7.0) | 0.011 |
| Burning | 4 (8.3) | 7 (12.3) | 0.751 |
| Stabbing | 2 (4.2) | 5 (8.8) | 0.45 |
| Cramp‐like | 4 (8.3) | 6 (7.5) | 0.751 |
| CP in the ED | 27 (56.3) | 33 (57.9) | 0.865 |
| STEMI | 22 (45.8) | 24 (42.1) | 0.701 |
| Anginine at home | 13 (27.1) | 4 (7.0) | 0.007 |
| CP onset at home | 41 (85.4) | 38 (66.7) | 0.027 |
| Other person present | 33 (68.8) | 44 (77.2) | 0.33 |
AMI, acute myocardial infarction; CP, chest pain; ED, emergency department; IHD, ischaemic heart disease; STEMI, ST‐elevation myocardial infarction.
*Not all patients were able to describe characteristics of chest pain.
After multivariate analysis, self‐administered anginine (p = 0.037), sharp chest pain (p = 0.046) and occurrence of symptom onset at home (p = 0.033) remained as independent predictors of ambulance use.
Table 3 presents the reasons given for going to hospital. More participants who came directly by ambulance reported pain and symptoms as the main reasons for going to hospital (60% v 25%; p<0.000). They were also more likely to have been told by family or friends to come to hospital (21% v 7%).
Table 3 Comparison of reasons for going to hospital for ambulance and non‐ambulance participants.
| Reasons for going to hospital | Ambulance (48) | Non‐ambulance (57)* | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Pain/symptoms | 29 (60.4) | 14 (25.0) | <0.001 |
| Family/friend advised | 10 (20.8) | 4 (7.1) | |
| GP advice | 2 (4.2) | 25 (44.6) | |
| Worried | 3 (6.3) | 3 (5.4) | |
| Persistent pain | 3 (6.3) | 7 (12.5) | |
| Other professional advice | 1 (2.1) | 3 (5.4) |
GP, general practitioner.
*One participant could not give a reason.
Responses from non‐ambulance participants for not calling an ambulance varied, with only 38 participants able to give a reason for non‐ambulance use. The main reasons cited included that patients did not think they were having an AMI (n = 11, 19.3%), their general practitioner did not advise them to use ambulance transport (n = 6, 10.5%), they did not have ambulance cover (n = 4, 7.0%) or they thought that self‐transport would be quicker (n = 4, 7.0%).
Discussion
Calling an ambulance is the recommended response for patients with chest pain in Australia.20 There are several reasons for this. Most deaths due to CHD take place out of hospital,21 presumably from arrhythmia, which can be detected and treated by ambulance paramedics. Additionally, patients who take this approach usually reach the hospital earlier in their clinical course,13 allowing earlier access to reperfusion treatment that has been clearly shown to reduce morbidity and mortality.3,4,5 Unfortunately, this study shows that most patients (53%) who have an AMI do not access ambulances as their first medical contact.
This is the first Australian study to examine in detail the nature of request for emergency medical services for patients with AMI. Previous local studies6,16 have examined ambulance transport rates to hospital, but did not reliably detect alternate emergency care sought (general practitioner used by patients before ambulance transport). This may explain the higher rates of non‐ambulance transport observed in this study.
Our findings are broadly consistent with other research in this field. In Glasgow, 20% of patients presented directly to the emergency department, 55% called a general practitioner and 25% of patients called an ambulance as their first course of action.7 Similar findings were found in a Swedish study,18 where 32% of patients with AMI presented to their general practitioner in the first instance.
In our study, the group of patients who did not initially call for an ambulance had a longer prehospital delay time by a median of 5 h. This has serious implications as suitability for, and effectiveness of, reperfusion treatment is time dependent.3,4,5 Several factors may contribute to this delay, including increased deliberation time before seeking medical care and waiting to see a general practitioner. Patients also reported pain or symptoms as the main reason for going to hospital, in contrast with the group who did not seek ambulance transport immediately from symptom onset, who reported advice from the general practitioner as the main reason for going to hospital. Severity of symptoms seems to have been an important difference between the two groups. Our findings replicate those of another Australian study,22 which found that prehospital delay is shortened for patients with chest pain who are transported by ambulance. That study also showed that time from onset of pain to initiation of thrombolysis was significantly longer in the group of patients who called their general practitioner first instead of the ambulance service (median 130 v 248 min; p = 0.005).
We found that patients were more likely to call an ambulance if they took anginine at home and onset of symptoms occurred at home. These predictors have not previously been reported. Taking anginine at home may be a surrogate for experience or education, as patients prescribed anginine have known CHD and may have been educated about an action plan for chest pain. In our study, patients who had experienced a previous IHD event were more likely to be transported by ambulance, although this feature did not reach statistical significance before or after multivariate analysis. It is possible that those who took anginine may not have had it prescribed. For these patients, it is possible that the anginine belonged to a partner or friend, who may have advised self‐administration.
Our study also confirmed the findings of other studies15,17 that older patients with AMI are more likely to call an ambulance directly. Possible explanations include prior knowledge, having ambulance cover (a pensioner entitlement in the State of Victoria, Australia) or lack of other available transport options.
Overall, we found that awareness of the various AMI symptoms is poor, a finding that is consistent with the reports of Goff et al23 and Smith et al.24 Patients in our study who described their chest pain as “sharp” in nature were more likely to arrive at hospital by ambulance. Sharp chest pain, as experienced by patients with AMI, may be more uncomfortable prompting an emergency alert. In our study, 38% of non‐ambulance patients did not think their symptoms were related to an AMI. This finding is in accordance with other data17,18 that suggest that patients with AMI who do not call for an ambulance do not think their symptoms are severe enough. Increasing the knowledge of the general public, particularly those at risk for AMI, about symptoms, patterns and an appropriate response may be advantageous. Unfortunately, previous attempts to do so in Australia have been disappointing.25
Currently, the perception of a heart attack by the public is similar to that portrayed in the media. Most patients with AMI perceive heart attack to be associated with chest pain.23,24 Symptoms such as sweating, shortness of breath and nausea are less well recognised.23,24 In our study, only 4% of participants were aware that sweating may be a sign of AMI, 13% were aware of nausea and vomiting, and 27% were aware of shortness of breath. These symptoms were experienced by 32%, 37% and 41% of patients, respectively, in our study. This shows the need for education to include atypical symptoms as well as typical symptoms of AMI.
It is of concern that a proportion of study participants were not referred to hospital by ambulance after presenting initially to their general practitioner (25/57, 44%). Perhaps general practitioners underestimate both the risks of self‐transport and potential benefits of ambulance use. The message to general practitioners in relation to AMI symptoms needs to be reinforced to ensure that they are encouraging or organising patients to access ambulance services.
Limitations
Our study sample was small. Only 189 patients were eligible for participation during the study period. Interviews were conducted for 105 of these patients, resulting in a positive interview rate of 55%. The study sample was representative of the population after comparing for sex, mode of transport and hospital of presentation. However, given only two study sites, the small sample, a limited collection of variables to assess whether the recruited sample was representative and the barriers to consenting patients who could communicate in English, the sample may not be truly representative.
The study group was younger than the population with AMI for the study sites. They might therefore have had other confounders to explain differences in transport options used during an AMI event, including more access to their own transport. Results to the broader population with AMI should be extrapolated with caution.
In addition, information collected during the patient interview relied on recall of events by patients. However, to minimise the possibility of recall bias, the interview was conducted within a week of presentation to hospital.
As with such studies, there will have been potential participants who were not included as a consequence of death before presentation to hospital (en route or at home). Clearly, it was impossible to collect data for these patients. Factors influencing their decision making may have been different from the group studied.
Conclusion
This study found that most patients with AMI (53%) do not call an ambulance as their first medical contact. Predictors of ambulance transport are symptom onset during the weekend, self‐administered anginine and sharp chest pain.
Failure to call an ambulance initially had a significant effect on the prehospital component of the delay to definitive treatment. Further efforts need to be made to develop and implement an effective educational campaign that deals with symptoms and recommended action for patients with possible AMI.
Acknowledgements
We thank Dr John Edington and Mr Ian Patrick for reviewing the manuscript, and the nursing staff of the Coronary Care Unit at Western Hospital and Critical Care Unit at Bendigo Hospital for assisting in participant identification.
Abbreviations
AMI - acute myocardial infarction
CHD - coronary heart disease
IHD - ischaemic heart disease
Footnotes
Competing interests: None.
References
- 1.American Heart Association International cardiovascular disease death rates. The World Health Organization NCHS and NHLBI. who.int/whosis/ (accessed 14 Sept 2006).
- 2.Mathur S.Epidemic of coronary heart disease and its treatment in Australia. Cardiovascular disease series number 20. Canberra: Australian Institute of Health and Welfare, 2002
- 3.Maynard C, Althouse R, Olsufka M.et al Early versus late hospital arrival for acute myocardial infarction in the western Washington thrombolytic therapy trials. Am J Cardiol 1989631296–1300. [DOI] [PubMed] [Google Scholar]
- 4.Newby L K, Rutsch W R, Califf R M.et al Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO‐1 Investigators. J Am Coll Cardiol 1996271646–1655. [DOI] [PubMed] [Google Scholar]
- 5.Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico ( G I S S I. Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet 19861397–402. [PubMed] [Google Scholar]
- 6.Dracup K, McKinley S, Moser D. Australian patient's delay in response to heart attack symptoms. Med J Aust 1997166233–236. [DOI] [PubMed] [Google Scholar]
- 7.Leslie W S, Urie A, Hooper J.et al Delay in calling for help during myocardial infarction: reasons for the delay and subsequent pattern of accessing care. Heart 200084137–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wielgosz A T, Nolan R P, Earp J A.et al Reasons for patients' delay in response to symptoms of acute myocardial infarction. CMAJ 1988139853–857. [PMC free article] [PubMed] [Google Scholar]
- 9.Dracup K, Moser D K, Eisenberg M.et al Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med 199540379–392. [DOI] [PubMed] [Google Scholar]
- 10.Goff D C, Jr, Feldman H A, McGovern P G.et al Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Rapid Early Action for Coronary Treatment (REACT) Study Group. Am Heart J 19991381046–1057. [DOI] [PubMed] [Google Scholar]
- 11.Leizorovicz A, Haugh M C, Mercier C.et al Pre‐hospital and hospital time delays in thrombolytic treatment in patients with suspected acute myocardial infarction. Analysis of data from the EMIP study. European Myocardial Infarction Project. Eur Heart J 199718248–253. [DOI] [PubMed] [Google Scholar]
- 12.Fitzpatrick B, Watt G C, Tunstall‐Pedoe H. Potential impact of emergency intervention on sudden deaths from coronary heart disease in Glasgow. Br Heart J 199267250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hutchings C B, Mann N C, Daya M.et al Rapid Early Action for Coronary Treatment Study. Patients with chest pain calling 9‐1‐1 or self‐transporting to reach definitive care: which mode is quicker, Am Heart J 200414735–41. [DOI] [PubMed] [Google Scholar]
- 14.Zed P J, Abu‐Laban R B, Cadieu T M.et al Fibrinolytic administration for acute myocardial infarction in a tertiary ED: factors associated with an increased door‐to‐needle time. Am J Emerg Med 200422192–196. [DOI] [PubMed] [Google Scholar]
- 15.Canto J G, Zalenski R J, Ornato J P.et al Use of emergency medical services in acute myocardial infarction and subsequent quality of care. Observations from the National Registry of Myocardial Infarction 2. Circulation 20021063018–3023. [DOI] [PubMed] [Google Scholar]
- 16.Kelly A M, Kerr D, Patrick I.et al Call‐to‐needle times for thrombolysis in acute myocardial infarction in Victoria. Med J Aust 2003178381–385. [DOI] [PubMed] [Google Scholar]
- 17.Meiscke H, Ho M T, Eisenberg M S.et al Reasons patients with chest pain delay or do not call 911. Ann Emerg Med 199525193–197. [DOI] [PubMed] [Google Scholar]
- 18.Johansson I, Stromberg A, Swahn E. Ambulance use in patients with acute myocardial infarction. J Cardiol Nurs 2004195–12. [DOI] [PubMed] [Google Scholar]
- 19.Dracup K, Moser D K, McKinley S.et al An international perspective on the time to treatment for acute myocardial infarction. J Nurs Scholarship 200335317–323. [DOI] [PubMed] [Google Scholar]
- 20.National Heart Foundation Australia Guidelines Reperfusion therapy for acute myocardial infarction. Melbourne: The National Heart Foundation, 2002, http://www.heartfoundation.com.au/downloads/reperfusion_guidelines
- 21.Engdahl J, Holmberg M, Karlson B W.et al The epidemiology of out‐of‐hospital ‘sudden' cardiac arrest. Resuscitation 200252235–245. [DOI] [PubMed] [Google Scholar]
- 22.Hitchcock T, Rossouw F, McCoubrie D.et al Observational study of prehospital delays in patients with chest pain. Emerg Med J 200320270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goff D C, Jr, Sellers D E, McGovern P G.et al Knowledge of heart attack symptoms in a population survey in the United States: The REACT trial. Arch Intern Med 19981582329–2338. [DOI] [PubMed] [Google Scholar]
- 24.Smith K L, Cameron P A, Meyer A.et al Knowledge of heart attack symptoms in a community survey of Victoria. Emerg Med (Fremantle) 200214255–260. [DOI] [PubMed] [Google Scholar]
- 25.Bett N, Aroney G, Thompson P. Impact of a national educational campaign to reduce patient delay in possible heart attack. Aust N Z Med J 199323157–161. [DOI] [PubMed] [Google Scholar]