Abstract
Two cases of acute pericarditis presented with interesting electrocardiograms resembling Brugada‐like or early repolarisation patterns. This report emphasises that proper interpretation of the electrocardiogram in patients with ST‐segment elevation assists the clinician in arriving at the correct diagnosis in making appropriate diagnostic and therapeutic decisions, and also that the saddleback‐type ST‐segment elevation cannot be a sensitive finding for the Brugada syndrome.
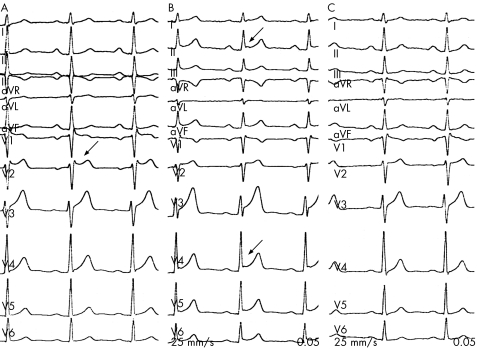
A previously healthy 28‐year‐old male patient presented to the emergency department with sharp, pleuritic‐type chest pain exacerbated by deep inspiration and supine position. He had no family history of sudden death, nor had he experienced any episodes of syncope. Pertinent physical examination showed the following results: blood pressure, 130/80 mm Hg; pulse rate, 80 beats/min; and temperature, 37.5°C. No precordial friction rub was heard. Initial laboratory data showed a negative troponin T test, an abnormal white cell count of 12 500/mm3, a raised C reactive protein concentration of 14.2 mg/dl and a normal chemistry profile including D‐Dimer levels. The 12‐lead electrocardiogram (ECG) on admission showed sinus rhythm with incomplete right bundle branch block (RBBB) and saddle‐back type ST‐segment elevation (ST‐SE) in V2 (fig 1A). Chest radiographs showed normal heart size and no consolidation in the lungs. A transthoracic echocardiography showed normal wall motion throughout, with no evidence of pericardial effusion. During hospitalisation, serial cardiac enzyme measurements, including creatine kinase‐monoclonal band (CK‐MB) and troponin I, were normal. Several hours after his admission, repeated ECG showed widespread ST‐SE resembling early repolarisation with reciprocal ST segment depression in aVR (fig 1B). On the basis of clinical and electrocardiographic findings, an acute pericarditis, with the most likely aetiology being either idiopathic or postviral, was diagnosed and the patient was given oral ibuprofen. Two days later, his chest pain resolved gradually and on the ECG, only incomplete RBBB was seen (fig 1C). Cardiac ischaemia was not induced during a maximal treadmill exercise test. Provacation test with intravenous propafenone was negative. At present, this patient is being followed up at the outpatient clinic.
Figure 1 (A) The electrocardiogram (ECG) on presentation showing saddle‐back type ST‐segment elevation (ST‐SE; arrow) and incomplete right bundle branch block (RBBB). (B) The ECG taken several hours later shows widespread ST‐SE resembling early repolarisation (arrow). (C) Two days later, the ECG shows only incomplete RBBB.
Case 2
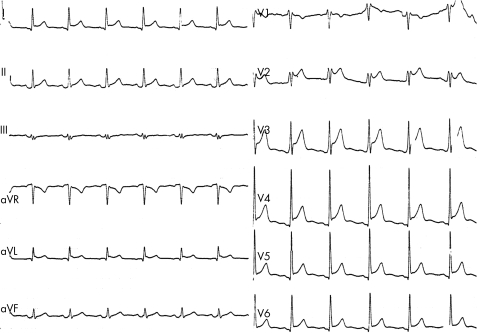
A 36‐year‐old man was admitted to the emergency department because of non‐exertional, pleuritic chest pain exacerbated by deep inspiration and recumbency. His medical history was unremarkable and he was not taking any prescribed drugs. At the time of admission, the patient is afebrile and has a friction rub. The ECG showed widespread ST‐SE and concomitant PR‐segment depression, more prominent in D2 with saddle‐back type ST‐SE in V2 (fig 2). The echocardiography showed normal left ventricular systolic function and a trivial pericardial effusion. The levels of CK‐MB and troponin were found to be normal when measured twice that day. His ECG was interpreted as acute pericarditis because of the diffuse ST‐SE and PR‐segment depression. His chest pain gradually resolved with oral ibuprofen. At the 6 month follow‐up visit, the patient had no cardiac symptoms and his ECG showed sinus rhythm with incomplete RBBB without previous ST‐SE.
Figure 2 The electrocardiogram (ECG) shows diffuse ST‐segment elevation (ST‐SE) with saddle‐back type ST‐SE pattern in V2 and PR segment depression in D.
Discussion
As ST‐SE was seen in many conditions, such as acute and subacute myocardial infarction, Prinzmetal angina, old myocardial infarction with ventricular aneurysm, acute pericarditis, normal variants including early repolarisation, massive pulmonary embolism, electrolyte abnormalities (hyperkalaemia and hypercalcaemia), cerebrovascular accidents, hypothermia, pneumothorax, post‐DC shock, Brugada syndrome or hypertrophic obstructive cardiomyopathy, it should be considered to avoid missing the diagnosis.1 Many times, the clinical setting, in which the elevation occurs, the shape of the ST‐SE, the leads involved and other features of the ECG, and echocardiographic findings can help differentiate these conditions and prevent misdiagnosis,1 resulting in unwarranted thrombolytic treatment or emergency angiography.2 It is particularly important to distinguish acute pericarditis from acute myocardial infarction, because thrombolytic treatment could have disastrous effects on patients with pericarditis. In acute pericarditis, the ECG typically shows ST‐SE in all leads, with an upward concavity of the elevation (so‐called “smiling face”). There may also be ST‐segment depression in leads aVR and V1; however, this is not specific for acute pericarditis, as early repolarisation of atrial tissue or atrial infarction can also cause the depression.1,3 Early repolarisation is characterised by a marked, constant elevation of the J point and the concave ST‐segment in both right and left precordial leads (most marked in V4, accentuated more septally or more laterally) or the inferior leads DIII and aVF. The T waves are tall and are not inverted.1
Brugada syndrome is an inherited cardiac disease causing life‐threatening ventricular tachyarrhythmias in patients with a structurally normal heart and a characteristic ECG showing a pattern of RBBB and ST‐SE in right precordial leads V1–V3. The ECG abnormalities in BS include three subgroups: one with a coved‐type ST‐SE (type 1) and two with a saddle‐back type (type 2 and 3 patterns).3 Although the saddle‐back type is often seen in people with true Brugada syndrome at the time of near normalisation of the ECG, it is reported that this type of ST‐SE is not a rare observation among asymptomatic patients and can be a normal variant rather than a specific predictor of life‐threatening ventricular arrhythmias.3 Both patients had only saddleback‐type BS ECG pattern, and were asymptomatic for arrhytmic family and personal history, therefore, the term “Brugada‐like” was used. We believe that, in case 1, the dynamic changes in ECG without increased cardiac enzymes are probably related to acute pericarditis or simultaneously fever.4 The ECG in case 2 was more consistent with acute pericarditis with previously incomplete RBBB. This report emphasises that proper interpretation of the ECG in patients with ST‐SE assists the clinician in arriving at the correct diagnosis and in making appropriate diagnostic and therapeutic decisions.
Abbreviations
CK‐MB - creatine kinase‐monoclonal band
ECG - electrocardiogram
RBBB - right bundle branch block
ST‐SE - ST‐segment elevation
Footnotes
Competing interests: None declared.
References
- 1.Wang K, Asinger R W, Marriott H J. ST‐segment elevation in conditions other than acute myocardial infarction. N Engl J Med 20033492128–2135. [DOI] [PubMed] [Google Scholar]
- 2.Ozeke O, Aras D, Deveci B.et al Brugada‐like early repolarization pattern misdiagnosed as acute anterior myocardial infarction in a patient with myocardial bridging of the left anterior descending artery. Mt Sinai J Med 200673627–630. [PubMed] [Google Scholar]
- 3.Antzelevitch C, Brugada P, Borggrefe M.et al Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 2005111659–670. [DOI] [PubMed] [Google Scholar]
- 4.Ozeke O, Aras D, Geyik B.et al Brugada‐type electrocardiographic pattern induced by fever. Indian Pacing Electrophysiol J 20055146–148. [PMC free article] [PubMed] [Google Scholar]