Abstract
Although the overall injury rate in volleyball and beach volleyball is relatively low compared with other team sports, injuries do occur in a discipline specific pattern. Epidemiological research has revealed that volleyball athletes are, in general, at greatest risk of acute ankle injuries and overuse conditions of the knee and shoulder. This structured review discusses both the known and suspected risk factors and potential strategies for preventing the most common volleyball related injuries: ankle sprains, patellar tendinopathy, and shoulder overuse.
Keywords: ankle sprain, injury prevention, patellar tendinopathy, shoulder pain, volleyball
Volleyball enjoys one of the highest participation rates of any sport in the world. By most estimates, volleyball ranks second only to football (soccer) in terms of global popularity. One of the most appealing aspects of the sport is that it can be played indoors and outdoors, by the young and the old, by males and females, and by both the able bodied and those with physical impairments. Volleyball is furthermore unique among team sports in that it has evolved into two distinct Olympic disciplines: an indoor version featuring six players on each team, and a two person per side outdoor game typically played on sand (beach volleyball). Although the essential skills of the two disciplines are identical, important differences between indoor volleyball and beach volleyball do exist, including certain rules, the court dimensions, the composition of the playing surface, the environmental conditions in which the players must compete, and subtle differences in the size and weight of the indoor and outdoor balls. The physiological demands of the two disciplines also differ to some extent: the average indoor match during the 2005 FIVB World Grand Champions Cup lasted about 95 minutes, with nearly 165 rallies over the course of the contest, whereas the average match on the FIVB Beach Volleyball World Tour lasts about 50 minutes with 90 rallies contested.
As with all sports, those who enjoy either of the two volleyball disciplines assume a certain risk of injury the moment they step on to the court. According to van Mechelen's model, one must first understand the injury pattern characteristic of the sport before it is possible to design effective prevention programmes.1 Data collected prospectively since 1984 by the National Collegiate Athletic Association's (NCAA) Injury Surveillance System (ISS)2 consistently reveal acute ankle sprains to be the most common injury suffered by women's collegiate (indoor) volleyball athletes, followed by overuse conditions of the knee, shoulder, and lower back.
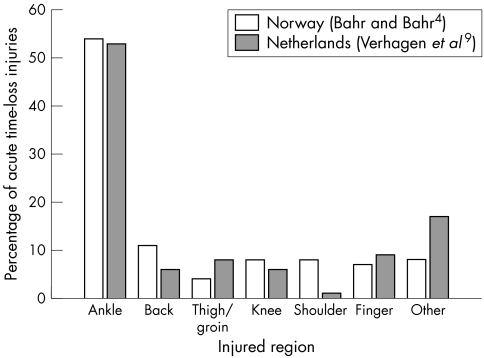
In addition to the ISS data, there are numerous published epidemiological studies that have attempted to characterise the injury pattern typical of, and quantify the risk factors for injury inherent to, volleyball.3,4,5,6,7,8,9,10 Regrettably, differences in methodology and design make direct comparison of these studies difficult, if not impossible. In some instances, the studies are too small to permit meaningful statistical comparison of the data. Nevertheless, at least two prospective cohort studies have been published that reveal similar patterns of acute injuries among men and women competing in the traditional indoor version of the sport (fig 1). Bahr and Bahr4 documented an incidence of 3.5 injuries/1000 hours during competition and 1.5 injuries/1000 hours during training (overall injury rate of 1.7/1000 hours) among 273 male and female athletes competing over one season in the Norwegian Volleyball Federation amateur league. More recently, Verhagen et al9 found an overall injury rate of 2.6 injuries/1000 hours (representing a competition injury rate of 4.1/1000 hours and a training injury rate of 1.8/1000 hours) among a cohort of 486 male and female athletes competing in the 2nd and 3rd Dutch leagues. These data suggest that indoor volleyball is a relatively safe sport, particularly compared with contact sports such as team handball and collision sports such as ice hockey. Indeed, research conducted during the Athens 2004 Olympics confirms that volleyball enjoyed the lowest injury rate of any team sport contested in those Games.11
Figure 1 A comparison of the acute injury patterns observed in two different prospective epidemiological studies. The data presented from each study represent the number of acute injuries sustained by both male and female volleyball players during both training and competition (combined) while participating in a European national adult competitive amateur league.
The discipline of beach volleyball may be even safer than the indoor variety. Bahr and Reeser5 investigated the injury pattern at the professional level—that is, athletes competing on the FIVB World Tour—documenting an acute time‐loss injury rate of 3.1/1000 competition hours (2.9 for men and 3.3 for women) and 0.7/1000 training hours (0.8 for men and 0.7 for women). Knee injuries (30%), ankle injuries (17%), and finger injuries (17%) accounted for more than half of all acute time‐loss injuries. However, both male and female players reported a high prevalence of overuse injuries of the lower back, knee, and shoulder (25% of which resulted in missed training or competition).
Volleyball, whether played indoors or on the beach, is therefore not a particularly dangerous sport. The published data suggest that the injury pattern is similar for men and women, and that volleyball athletes appear to be at greatest risk of acute inversion sprains of the ankle and overuse injuries of the knee (predominantly patellar tendinopathy) and shoulder (impingement and functional instability). Although it should be noted that volleyball athletes are at risk of other injuries, including lower back pain, finger sprains, and contusions and abrasions, the remainder of this review will discuss strategies for preventing the three most common volleyball related injuries.
Strategies for preventing ankle sprains
The extent of the problem
Ankle sprains are the most common acute injury suffered by volleyball players. With a reported incidence of about 1/1000 hours of participation (training and competition combined), acute ankle sprains account for up to half of all volleyball related injuries among male and female players participating indoors at all skill levels.2,4,12 Ankle sprains are not trivial injuries. An ankle sprain can be expected to result in (on average) 4.5 weeks of time lost from volleyball training or competition.9
Mechanism of injury
The vast majority of volleyball related ankle injuries are contact related inversion sprains. Indoors, ankle sprains occur most often at the net, as the result of contact between the attacker and the opposing blocker(s) across the centre line. Research has consistently revealed that approximately half of all such sprains occur when a blocker lands on the foot of an opposing attacker who has legally penetrated the centre line.9,12 Often the attacker is trying to “catch up” to a set that is too low and too close to the net, and his momentum and jump trajectory takes him across the centre line. The blocker, who for tactical reasons jumps later than the attacker, may land on the attacker's foot within this “conflict zone” under the net. Approximately one quarter of indoor volleyball related ankle sprains occur when a blocker lands on a teammate's foot when participating in a multi‐person block. Consequently, middle blockers and outside attackers are at greatest risk of ankle sprains, and setters and defensive specialists are at comparatively low risk.
Risk factors
The leading risk factor for ankle inversion injury is a history of a prior ankle sprain involving the same ankle (table 1). Up to 80% of sprains involve previously injured ankles.4,12 Furthermore, the risk of injury is greatest within the first six months of the previous injury. Athletes who have sustained an ankle inversion injury within the previous 6–12 months are about 10 times more likely to suffer a repeat injury than those without a history of recent injury.4 NCAA ISS data confirm Bahr's finding4,12 that the rate of ankle sprains during competition is nearly twice the practice related injury rate, presumably because of the more aggressive net play that occurs during matches. Ankle sprains occur less often outdoors than indoors.3,5 It is not well understood whether this is the result of reduced player density in the beach game (thereby reducing the risk of landing on an opponent's or a teammate's foot), if it is due to the biomechanical effects of playing on soft sand, or whether it results from a combination of these (and possibly other) factors. Lastly, there is at present no compelling evidence in the volleyball literature to suggest that sex is a significant risk factor for acute ankle injuries. However, in 2005 the NCAA ISS began collecting injury data on men's collegiate volleyball, which should eventually permit a more definitive analysis of the effect of sex on the risk of volleyball related ankle sprains (as well as other injuries).
Table 1 Risk factors for acute ankle sprain among volleyball athletes.
| Risk factor | Modifiable |
|---|---|
| Intrinsic | |
| Neuromuscular control | Yes |
| Previous injury | No |
| Spike approach | Yes |
| Extrinsic | |
| Centre line rule | Yes |
| Competitive situation | Yes |
| Court surface | Yes |
| Position played | Yes |
| Taping/bracing | Yes |
Potential prevention strategies
Several intervention strategies have been proposed in an effort to reduce the risk of ankle sprains, including modification of the centre line rule, improving attacker spike approach technique, the quality of rehabilitation after the index (or most recent) sprain, and the use of an external support (tape or brace) in an effort to protect the ankle from injury. Each of these strategies will be considered in turn.
Rule changes
In recognition of the fact that most indoor ankle sprains occur at the net and involve (legal) penetration of the centre line, Bahr13 proposed a rule change that would have made any contact with the centre line a fault. When tested during a Norwegian tournament, however, nearly 20‐fold more centre line violations were whistled than under the existing rule, and therefore the proposed intervention was abandoned. Interestingly, despite the introduction of a more liberal rule permitting complete penetration of the centre line (as long as such penetration does not interfere with play on the opponent's side of the court), the incidence of ankle sprains in women's collegiate volleyball has not increased significantly over the last several years.14 This suggests that a rule limiting centre line penetration only within the “conflict zone” may prove effective in reducing the incidence of ankle sprains without adversely affecting the flow of the game, but this hypothesis has yet to be tested. No centre line exists outdoors, and beach athletes are permitted to cross over into the opposition's side of the court provided that they do not interfere with their opponents.
Technique
Bahr et al15 successfully reduced the incidence of ankle sprains among amateur male and female Norwegian volleyball players through a multifaceted intervention programme that included technical training (emphasising proper spike approach, take off, and landing technique, in addition to block movement drills), balance board training, and injury awareness information. The study showed that the number of injuries resulting from opponent contact under the net was lower after the introduction of the training programme, as was the number of cases resulting from landing on a teammate's foot after a two‐person block. More recently, Stasinopoulos16 showed that technical training alone appeared to reduce the incidence of recurrent ankle sprains in a small cohort of second division female volleyball players in Greece.
Rehabilitation
Neuromuscular (proprioceptive) training, such as that performed using a wobble or balance board, reduced the risk of ankle injuries among volleyball players when included as part of the multifaceted intervention discussed above.15 A recent, large scale, controlled intervention study, the Amsterdam balance board ankle study, showed that a minimal prophylactic programme of balance board training during warm up effectively reduced the incidence of ankle inversion injury among both male and female indoor volleyball players, but only among athletes with a history of prior ankle sprain.17
External ankle supports
Although no study has been conducted proving the benefit of taping or bracing in preventing volleyball related ankle sprains specifically, volleyball players often wear ankle orthoses in an effort to prevent injury.18,19 The work of Sitler et al20 and Surve et al21 suggests that external orthoses are effective in preventing recurrent ankle sprains in basketball and soccer respectively. However, as the environmental risk factors for volleyball related ankle sprains may be unique to the discipline, the preventive effect of taping and/or bracing should be confirmed through volleyball specific research.
Strategies for preventing patellar tendinopathy
The extent of the problem
Volleyball athletes often complain of anterior knee pain. By far the most common diagnosis among those with knee pain is patellar tendinopathy. Also known as “jumper's knee,” this condition has consistently been reported to afflict about 50% of male indoor volleyball players.2,7,14,22 Ferretti23,24 found that about 40% of elite male volleyball players had jumper's knee. Similarly, Lian et al25 diagnosed patellar tendinopathy in 25 of 47 elite male volleyball players examined, and an additional seven athletes gave a history of prior symptoms consistent with the diagnosis. This high prevalence was recently confirmed by a large study of elite athletes from different sports in which 45% of elite male volleyball players reported current symptoms of jumper's knee, and an additional 5% gave a past history of the condition.22 NCAA ISS data reveal that jumper's knee has an incidence of 0.2/1000 athlete exposures among female collegiate volleyball athletes2 but, as the ISS records only time‐loss injuries, the actual prevalence of symptomatic jumper's knee among female volleyball players can be safely assumed to be much greater. However, the exact prevalence of jumper's knee among female volleyball players is not known.
Although anterior cruciate ligament (ACL) trauma does occur in volleyball,26 this devastating injury is considerably less common in volleyball than in women's soccer and basketball. NCAA ISS data2 reveal an incidence of about 0.1 ACL injuries/1000 athlete exposures among female collegiate volleyball athletes in the United States (compared with a rate of 0.4/1000 athlete exposures in soccer and 0.27/1000 athlete exposures in basketball). Prospective cohort studies from Norway4 and the Netherlands9 also indicate that ACL injuries are relatively uncommon in women's volleyball in contrast with team handball (where such injuries appear to be epidemic).27 On the basis of these data, it appears evident that jumper's knee affects far more volleyball athletes than does acute knee trauma. Consequently, the present review focuses on the prevention of patellar tendinopathy.
Mechanism of injury
Patellar tendinopathy is an overuse injury. Symptom onset typically occurs gradually after a threshold of cumulative tissue injury has been exceeded. However, it is not well understood why some athletes become symptomatic and others do not, despite equivalent training loads. Histological inspection of patellar tendon biopsies from affected athletes consistently reveals degeneration and fibrotic scarring of the tendon, particularly at the bone‐tendon junction. The normally parallel collagen bundles are disorganised, and the observed tenocytes display altered morphology. It has been proposed that the initial pathology in tendinopathy involves the tenocyte rather than the collagen fibres themselves.28 The theory is that excessive tendon loading somehow induces tenocyte apoptosis (programmed cell death),29 but at present the link between excessive loading and subsequent pathology is not well understood.
Microscopic examination of areas of structural tendon degeneration also reveals a notable absence of inflammatory cells, despite prominent angiogenesis and capillary proliferation. Recent ultrasonographic imaging studies suggest that neovascularisation within the area of tendon degeneration correlates with (and may be predictive of) symptoms among volleyball players.30,31 Interestingly, although similar findings have yet to be reported for patellar tendinopathy, neovessels have been observed to disappear in those athletes with symptomatic Achilles tendinopathy who responded to therapeutic eccentric exercise protocols.32
Risk factors
There is some evidence to suggest that the prevalence of patellar tendinopathy is sex dependent. For example, a recent study showed that in team handball and soccer the prevalence of jumper's knee is 2–3 times greater among men than women.22 Jumper's knee is more prevalent among volleyball players who train on hard, unforgiving surfaces, and symptoms may be precipitated after increases in the volume of jump training.23,24 Not surprisingly therefore, beach volleyball athletes have a lower prevalence of symptomatic patellar tendinopathy than do indoor volleyball athletes,5 and middle blockers tend to suffer from jumper's knee more than do players at other positions. Anatomical factors do not appear to be a significant risk factor for patellar tendinopathy,25 although (as alluded to above) at the tissue level the presence of neovessels may prove to be predictive of symptom onset. Biomechanical studies have revealed an increased incidence of jumper's knee among those athletes who jump highest and in those who develop the deepest knee flexion angle during landing from a spike jump.33,34 Another study suggested that valgus knee strain during the eccentric loading phase of the spike jump take off may contribute to the observed asymmetric onset of patellar tendinopathy.35 In summary, it appears that factors that increase the dynamic load on the patellar tendon increase the risk of developing jumper's knee (table 2).
Table 2 Risk factors for jumper's knee among volleyball athletes.
| Risk factor | Modifiable |
|---|---|
| Intrinsic | |
| Core stability | Yes |
| Jumping ability | Yes |
| Prior history of similar symptoms | No |
| Sex | No |
| Spike approach/landing technique | Yes |
| Extrinsic | |
| Court surface | Yes |
| Volume of training | Yes |
Potential prevention strategies
Although patellar tendinopathy is quite common among volleyball athletes, only one volleyball specific intervention study has been published to date. Strategies for prevention of this potentially severe and incapacitating condition may be classified in the following ways.
Technique
More research is needed to determine whether instructing athletes to use specific spike jump approach and landing techniques (in order to minimise valgus strain on the lead knee during the jump approach and to keep knee flexion to a minimum on landing respectively) may help to reduce cumulative load on the patellar tendon.
Training
Given the effect of surface and training volume on jumper's knee, it makes sense to minimise the volume of jump training on hard playing surfaces. Overloading the knee extensor mechanism beyond the capacity of the patellar tendon to regenerate will precipitate jumper's knee. However, more research is needed to quantify how often and by what percentage the volume of jump training can be safely increased over a given time period. Unpublished data from Norway suggest that the risk of developing patellar tendinopathy may be quite high when young, promising players are promoted from the junior to the senior level (L Øystein, R Bahr, personal communication, 2006). These talented young players are abruptly moved from a relatively safe training environment—for example, practice two to three days a week, no weight lifting—to an elite club or sports school that practices daily and has a structured programme of weight training. Of course, these promising talents are also likely to possess superior jumping ability which, when coupled with sudden increases in strength, muscle mass, and training load, further amplifies their risk of developing anterior knee pain.
Rehabilitation
Eccentric training protocols (particularly those using decline squats)36,37 have been proven to be an effective means of treating patellar tendinopathy, although a recently published study reported that eccentric training of the quadriceps was ineffective in treating symptomatic jumper's knee in volleyball players during the competition season.38 There is preliminary evidence that such knee extensor eccentric training protocols, used prophylactically, can effectively prevent sports related anterior knee pain from patellar tendinopathy.39 However, volleyball specific prevention studies have yet to be conducted. It has been speculated that core weakness may contribute to the risk of developing anterior knee pain, as might functional imbalances of the lower limbs,40 although no prospective studies have proven these possible associations. Finally, when treating jumper's knee, it is important to rehabilitate beyond the absence of symptoms, and to avoid return to play before the athlete is adequately rehabilitated, in order to maximise secondary prevention of recurrent injury and thus minimise the risk of chronicity.
External orthoses
Although anecdotal reports of benefit abound, there is no research based evidence to suggest that patellar straps (ostensibly designed to redistribute the forces acting on the patellar tendon) are an effective method of treating or preventing jumper's knee.
Strategies for preventing shoulder overuse injury
The extent of the problem
Shoulder pain syndromes represent the third most common injury among both female and male volleyball athletes and the second most common overuse related condition, accounting for 8–20% of all volleyball injuries.2,41,42 Furthermore, Verhagen et al9 found that shoulder conditions result, on average, in 6.5 weeks of lost training and/or competition time, by far the longest mean absence from sports participation compared with other time‐loss injuries described in their study. Despite the widespread nature of the problem, with the exception of suprascapular neuropathy,43,44,45,46 relatively little is known about the epidemiology of shoulder pain among volleyball athletes.
Mechanism of injury
Our understanding of the natural history of shoulder overuse pathology among “overhead athletes” has evolved significantly over the last decade.47,48,49 Although there has been extensive research into the kinetics and kinematics of the overhead throwing motion, most of the published studies have focused on baseball,50 with comparatively few studies focusing specifically on volleyball related shoulder pathology.41,42,51,52 Nevertheless, there are sufficient similarities between the biomechanical aspects of the different overhead sports that we have come to appreciate the fact that the majority of the force imparted to the volleyball during a spike originates from the torso. The scapula, which serves as a “funnel” for the efficient transfer of kinetic energy to the upper limb,53 is furthermore responsible for providing a stable base of support so that the upper limb can be correctly positioned in space during the performance of overhead skills. The glenohumeral joint, which is capable of exceptional range of motion, is unfortunately inherently anatomically quite unstable. Consequently, the dynamic stabilisers of the scapula and the humeral head are critical to maintaining the functional integrity of the glenohumeral joint, and to the ability to successfully serve and spike a volleyball.
It has been estimated that the elite volleyball athlete performs as many as 40 000 spikes in a season,41 but this may be an underestimation of the true volume. The resultant load probably depends on a number of factors, including the mechanics of the arm swing and the distribution of overhead swings between practice and competition. Although the kinetics of the volleyball spike have not been reported, it is clear that the shoulder girdle is exposed to tremendous cumulative load as the result of repetitive spiking and serving.
The consequences of such chronic overload have been well described by Kugler et al,41 who identified a set of clinical findings commonly seen in the dominant shoulder girdles of a small cohort of elite volleyball attackers. Characteristic findings included depression and lateralisation of the dominant scapula compared with the non‐dominant side. Interestingly, similar physical adaptations have subsequently been reported to occur among other overhead athletes, and the constellation of findings has been characterised in the literature as the “SICK scapula” (scapular malposition, inferior medial border prominence, coracoid pain and malposition, and scapular dyskinesis).48 The SICK scapula is associated with shoulder pain due to the spectrum of rotator cuff pathology and functional instability. It is also tempting to speculate that the SICK scapula may contribute to the development of suprascapular neuropathy, a peripheral mononeuropathy occurring in up to 45% of elite volleyball athletes. Although the aetiology of suprascapular neuropathy has been debated in the literature,43,44 we propose that the scapular lateralisation and dyskinesis typical of the SICK scapula syndrome may provide sufficient traction to compromise the suprascapular nerve as it traverses the spinoglenoid notch.45,46
Risk factors
The risk factors for developing shoulder pain among volleyball athletes have not been rigorously defined. It seems intuitive that the risk factors should include a history of prior shoulder pain and the magnitude of the load to which the athlete is exposed (table 3). Other suspected risk factors that have yet to be verified through epidemiological research include the effect of the environment on both the trajectory of the outdoor ball during the set (to which the beach athlete must spontaneously adjust) and the weight of the volleyball (should it become wet and thus heavier). Sex may be a risk factor for shoulder pain, as data presented by Mjaanes and Briner54 suggest that elite female athletes may be more prone than male athletes to developing symptomatic instability. It is not clear to what extent biomechanical considerations influence the prevalence of shoulder pain. Oka et al55 described two types of spiking styles, and although subsequent studies suggest that these styles may not accurately describe the more common techniques used in recent years, it seems logical to assume that how and where a volleyball athlete contacts the ball during the spike or serve would influence the load on the glenohumeral joint. Whether strength ratios (such as that between isokinetic eccentric external rotation and concentric internal rotation) are predictive of the development of shoulder pain, or indeed whether it is reasonable to use these measurable variables as benchmarks for determining when an injured athlete should be cleared to return to play,52 needs to be determined through further research. Burkhart et al have suggested that a deficit of internal rotation at the glenohumeral joint that exceeds 10% of the total rotation arc of the contralateral shoulder should be considered a risk factor for the development of shoulder pain among overhead athletes. It is interesting to note that Burkhart has reported that overhead athletes with shoulder pain also often have demonstrable core weakness, suggesting that the symptomatic athlete may be overloading the shoulder girdle through altered biomechanics in an effort to compensate for insufficient power generated by the core musculature early in the throwing motion.47,48 Whether this holds true for volleyball players is not known.
Table 3 Proposed risk factors for shoulder pain among volleyball athletes.
| Risk factor | Modifiable |
|---|---|
| Intrinsic | |
| Anatomy | No |
| Biomechanics | Yes |
| Conditioning/core stability | Yes |
| Glenohumeral internal rotation deficit | Yes |
| Previous injury | No |
| Scapular dyskinesis (SICK scapula) | Yes |
| Sex | No |
| Extrinsic | |
| Competitive situation | Yes |
| Load | Yes |
Potential prevention strategies
No volleyball specific prevention intervention studies have been published to permit development of an evidence based guideline for the prevention of shoulder pain. Common sense preventive interventions that need to be further investigated include the following.
Technique
Once defined, it would seem appropriate to instruct symptomatic athletes in a spiking technique that minimises the kinetic load on the glenohumeral joint.
Training
Reduction in the load/volume of training should result in less shoulder overload and provide a greater opportunity for tissue recovery. Burkhart et al48 claim dramatic reduction in the prevalence of shoulder complaints in tennis and baseball players by addressing posterior capsular tightness and the resultant glenohumeral internal rotation deficit through a consistent season long stretching programme. Such an intervention has yet to be investigated in volleyball athletes. Volleyball athletes should also engage in a year round programme of predominantly eccentric resistance training designed to maintain coordinated scapular/rotator cuff function, strength, and endurance.56 Lastly, it would appear important to maintain the elite volleyball athlete on a programme of core strengthening/stability training.
Rehabilitation
Secondary prevention of shoulder pain is almost entirely dependent on effective rehabilitation. This means providing the symptomatic athlete with an accurate, comprehensive diagnosis from the outset and subsequently restricting return to play until he/she is both asymptomatic and has undergone a careful biomechanical analysis to ensure that no lingering underlying maladaptations exist that might precipitate reinjury.
External orthoses
There are no published data to prove that shoulder orthoses or taping of the shoulder girdle to control scapular mechanics is helpful in the prevention (or long term treatment) of shoulder pain syndromes.
Summary
Although sports medicine has, through research as well as trial and error, made tremendous advances in the treatment and rehabilitation of serious injuries, its ultimate goal should be to prevent injuries so that athletes can remain competitive in the arena rather than inactive in the training room. Although volleyball is a relatively safe sport, participants are at risk of a characteristic pattern of acute and overuse injuries that can have both short and long term sequelae to both the individual athlete and his/her team. Despite a growing understanding of the unique, sport specific risk factors for volleyball related injuries, the existing literature on the prevention of volleyball injuries is relatively sparse.57 More research is needed to identify effective interventions that will help to reduce not only the risk of primary injury among both male and female volleyball athletes, but also secondary reinjury, so that their ability to participate in and enjoy the sport is not compromised.
ACKNOWLEDGEMENTS
We are grateful to Alice Stargardlt of the Marshfield Clinic Research Foundation for her assistance in preparing the manuscript.
Footnotes
Competing interests: none declared
References
- 1.Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med 200539324–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NCAA Injury Surveillance System http://www1.ncaa.org/membership/ed_outreach/health‐safety/iss/index.html (accessed 19 Sep 2005)
- 3.Aagaard H, Scavenius M, Jorgensen U. An epidemiological analysis of the injury pattern in indoor and in beach volleyball. Int J Sports Med 199718217–221. [DOI] [PubMed] [Google Scholar]
- 4.Bahr R, Bahr I A. Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports 19977166–171. [DOI] [PubMed] [Google Scholar]
- 5.Bahr R, Reeser J C. Federation Internationale de Volleyball. Injuries among world‐class professional beach volleyball players. The Federation Internationale de Volleyball beach volleyball injury study. Am J Sports Med 200331119–125. [DOI] [PubMed] [Google Scholar]
- 6.Briner W W, Ely C. Volleyball injuries at the 1995 United States Olympic Festival. International Journal of Volleyball Research 199917–11. [Google Scholar]
- 7.Goodwin‐Gerberich S G, Luhmann S, Finke C.et al Analysis of severe injuries associated with volleyball activities. Phys Sportsmed 19871575–79. [Google Scholar]
- 8.Schafle M D, Requa R K, Patton W L.et al Injuries in the 1987 national amateur volleyball tournament. Am J Sports Med 199018624–631. [DOI] [PubMed] [Google Scholar]
- 9.Verhagen E A, Van der Beek A J, Bouter L M.et al A one season prospective cohort study of volleyball injuries. Br J Sports Med 200438477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watkins J, Green B N. Volleyball injuries: a survey of injuries of Scottish National League male players. Br J Sports Med 199226135–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Junge A, Langevoort G, Pipe A.et al Injuries in team sport tournaments during the 2004 Olympic Games. Am J Sports Med 200634565–576. [DOI] [PubMed] [Google Scholar]
- 12.Bahr R, Karlsen R, Lian O.et al Incidence and mechanisms of acute ankle inversion injuries in volleyball. A retrospective cohort study. Am J Sports Med 199422595–600. [DOI] [PubMed] [Google Scholar]
- 13.Bahr R. The effect of a new centerline violation rule on the quality and flow of volleyball games. International VolleyTech 1996214–19. [Google Scholar]
- 14.Reeser J C, Agel J, Dick R.et al The effect of changing the centerline rule on the incidence of ankle injuries in women's collegiate volleyball. International Journal of Volleyball Research 2001412–16. [Google Scholar]
- 15.Bahr R, Lian O, Bahr I A. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports 19977172–177. [DOI] [PubMed] [Google Scholar]
- 16.Stasinopoulos D. Comparison of three preventive methods in order to reduce the incidence of ankle inversion sprains among female volleyball players. Br J Sports Med 200438182–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verhagen E, van der Beek A, Twisk J.et al The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med 2004321385–1393. [DOI] [PubMed] [Google Scholar]
- 18.Verhagen E A, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med 200010291–296. [DOI] [PubMed] [Google Scholar]
- 19.Verhagen E A, van der Beek A J, van Mechelen W. The effect of tape, braces and shoes on ankle range of motion. Sports Med 200131667–677. [DOI] [PubMed] [Google Scholar]
- 20.Sitler M, Ryan J, Wheeler B.et al The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball. A randomized clinical study at West Point. Am J Sports Med 199422454–461. [DOI] [PubMed] [Google Scholar]
- 21.Surve I, Schwellnus M P, Noakes T.et al A fivefold reduction in the incidence of recurrent ankle sprains in soccer players using the Sport‐Stirrup orthosis. Am J Sports Med 199422601–606. [DOI] [PubMed] [Google Scholar]
- 22.Lian O B, Engebretsen L, Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross‐sectional study. Am J Sports Med 200533561–567. [DOI] [PubMed] [Google Scholar]
- 23.Ferretti A. Epidemiology of jumper's knee. Sports Med 19863289–295. [DOI] [PubMed] [Google Scholar]
- 24.Ferretti A, Puddu G, Mariani P P.et al Jumper's knee: an epidemiological study of volleyball players. Phys Sportsmed 19841297–106. [Google Scholar]
- 25.Lian O, Holen K J, Engebretsen L.et al Relationship between symptoms of jumper's knee and the ultrasound characteristics of the patellar tendon among high level male volleyball players. Scand J Med Sci Sports 19966291–296. [DOI] [PubMed] [Google Scholar]
- 26.Ferretti A, Papandrea P, Conteduca F.et al Knee ligament injuries in volleyball players. Am J Sports Med 199220203–207. [DOI] [PubMed] [Google Scholar]
- 27.Myklebust G, Maehlum S, Holm I.et al A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports 19988149–153. [DOI] [PubMed] [Google Scholar]
- 28.Cook J L, Feller J A, Bonar S F.et al Abnormal tenocyte morphology is more prevalent than collagen disruption in asymptomatic athletes' patellar tendons. J Orthop Res 200422334–338. [DOI] [PubMed] [Google Scholar]
- 29.Scott A, Khan K M, Heer J.et al High strain mechanical loading rapidly induces tendon apoptosis: an ex vivo rat tibialis anterior model. Br J Sports Med 200539e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gisslen K, Alfredson H. Neovascularization and pain in jumper's knee: a prospective clinical and sonographic study in elite junior volleyball players. Br J Sports Med 200539423–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cook J L, Malliaras P, De Luca J.et al Vascularity and pain in the patellar tendon of adult jumping athletes: a 5 month longitudinal study. Br J Sports Med 200539458–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alfredson H. The chronic painful Achilles and patellar tendon: research on basic biology and treatment. Scand J Med Sci Sports 200515252–259. [DOI] [PubMed] [Google Scholar]
- 33.Lian O, Engebretsen L, Ovrebo R V.et al Characteristics of the leg extensors in male volleyball players with jumper's knee. Am J Sports Med 199624380–385. [DOI] [PubMed] [Google Scholar]
- 34.Richards D P, Ajemian S V, Wiley J P.et al Knee joint dynamics predict patellar tendinitis in elite volleyball players. Am J Sports Med 199624676–683. [DOI] [PubMed] [Google Scholar]
- 35.Lian O, Refsnes P E, Engebretsen L.et al Performance characteristics of volleyball players with patellar tendinopathy. Am J Sports Med 200331408–413. [DOI] [PubMed] [Google Scholar]
- 36.Young M A, Cook J L, Purdam C R.et al Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med 200539102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee: a prospective randomised study. Br J Sports Med 200539847–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Visnes H, Hoksrud A, Cook J.et al No effect of eccentric training on jumper's knee in volleyball players during the competitive season: a randomized clinical trial. Clin J Sport Med 200515227–234. [DOI] [PubMed] [Google Scholar]
- 39.Fredberg U, Bolvig L. Prophylactic training reduces the frequency of jumper's knee but not Achilles tendinopathy. Br J Sports Med 200539384 [Google Scholar]
- 40.Sommer H M. Patellar chondropathy and apicitis, and muscle imbalances of the lower extremities in competitive sports. Sports Med 19885386–394. [DOI] [PubMed] [Google Scholar]
- 41.Kugler A, Kruger‐Franke M, Reininger S.et al Muscular imbalance and shoulder pain in volleyball attackers. Br J Sports Med 199630256–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang H K, Cochrane T. A descriptive epidemiological study of shoulder injury in top level English male volleyball players. Int J Sports Med 200122159–163. [DOI] [PubMed] [Google Scholar]
- 43.Ferretti A, De Carli A, Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med 199826759–763. [DOI] [PubMed] [Google Scholar]
- 44.Sandow M J, Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. J Shoulder Elbow Surg 19987516–521. [DOI] [PubMed] [Google Scholar]
- 45.Reeser J C. Infraspinatus syndrome. eMedicine J. 2005. http://www.emedicine.com/sports/topic54.htm (accessed 23 Sep 2005)
- 46.Safran M R. Nerve injury about the shoulder in athletes, part 1: suprascapular nerve and axillary nerve. Am J Sports Med 200432803–819. [DOI] [PubMed] [Google Scholar]
- 47.Burkhart S S, Morgan C D, Kibler W B. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy 200319404–420. [DOI] [PubMed] [Google Scholar]
- 48.Burkhart S S, Morgan C D, Kibler W B. The disabled throwing shoulder: spectrum of pathology. Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy 200319641–661. [DOI] [PubMed] [Google Scholar]
- 49.Christoforetti J J, Carroll R M. The thrower's shoulder. Curr Opin Orthoped 200516246–251. [Google Scholar]
- 50.Fleisig G S, Barrentine S W, Escamilla R F.et al Biomechanics of overhand throwing with implications for injuries. Sports Med 199621421–437. [DOI] [PubMed] [Google Scholar]
- 51.Cools A M, Witvrouw E E, Mahieu N N.et al Isokinetic scapular muscle performance in overhead athletes with and without impingement symptoms. J Athl Train 200540104–110. [PMC free article] [PubMed] [Google Scholar]
- 52.Wang H K, Macfarlane A, Cochrane T. Isokinetic performance and shoulder mobility in elite volleyball athletes from the United Kingdom. Br J Sports Med 20003439–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kibler W B. The role of the scapula in athletic shoulder function. Am J Sports Med 199826325–337. [DOI] [PubMed] [Google Scholar]
- 54.Mjaanes J M, Briner W W. Trends in shoulder injuries among elite volleyball players in the USA. Br J Sports Med 200539397 [Google Scholar]
- 55.Oka H, Okamato T, Kumamoto M. Electromyographic and cinematographic study of the volleyball spike. In: Komi PV, ed. Biomechanics V‐B. Baltimore: University Park Press, 1976326–331.
- 56.Jonsson P, Wahlstrom P, Ohberg L.et al Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc 20061476–81. [DOI] [PubMed] [Google Scholar]
- 57.Bahr R. Playing volleyball safely. Am J Med Sports 20035262–268. [Google Scholar]