Abstract
Background
The emergency care practitioner (ECP) is a generic practitioner who combines extended nursing and paramedic skills. The "new" role emerged out of changing workforce initiatives intended to improve staff career opportunities in the National Health Service and ensure that patients' health needs are assessed appropriately.
Objective
To describe the development of ECP Schemes in 17 sites, identify criteria contributing to a successful operational framework, analyse routinely collected data and provide a preliminary estimate of costs.
Methods
There were three methods used: (a) a quantitative survey, comprising a questionnaire to project leaders in 17 sites, and analysis of data collected routinely; (b) qualitative interpretation based on telephone interviews in six sites; and (c) an economic costing study.
Results
Of 17 sites, 14 (82.5%) responded to the questionnaire. Most ECPs (77.4%) had trained as paramedics. Skills and competencies have been extended through educational programmes, training, and assessment. Routine data indicate that 54% of patient contacts with the ECP service did not require a referral to another health professional or use of emergency transport. In a subset of six sites, factors contributing to a successful operational framework were strategic visions crossing traditional organisational boundaries and appropriately skilled workforce integrating flexibly with existing services. Issues across all schemes were patient safety, appropriate clinical governance, and supervision and workforce issues. On the data available, the mean cost per ECP patient contact is £24.00, which is less than an ED contact of £55.00.
Conclusion
Indications are that the ECP schemes are moving forward in line with original objectives and could be having a significant impact on the emergency services workload.
Keywords: emergency care practitioner, intermediate care, extended skills, avoided admission
A key strategy to meet the increasing demands for patient centred healthcare is to extend the existing clinical skills of health service staff and develop new ways of working to maximise the effective use of resources, and improve the efficiency in how health services are delivered. These challenges are especially present in the area of emergency and unscheduled health care where a demand driven, high profile service with limited resources has to be responsive to a fluctuating (and increasing) workload while ensuring safe, effective, and efficient delivery of care. Both TheNHS plan1 and Reforming emergency care2 emphasised the problems encountered by people in using the present emergency services and the need for greater flexibility and opportunities in the future for NHS staff to extend their roles. Despite the introduction of new services such as minor injury units (MIUs), walk in centres (WICs), and NHS Direct to complement hospital based models such as the emergency department (ED), attendances at EDs in the UK rise by around 2% per annum.3,4 In addition, calls to ambulance services rose by 7% in the year 2002–2003.5 An Audit Commission report6 questioned the need for a fully crewed ambulance to attend all 999 calls. It suggested that ambulance services should be allowed to decide who should be sent to each type of emergency and to treat some patients at home without transfer to hospital. The most recent figures indicate that 37.3% of emergency calls do not result in an emergency patient journey.7 Indeed, the Department of Health (DoH) has recently recognised this and has issued guidance that services will no longer be expected to provide an emergency response to category C (non‐urgent) calls, and that the response times for these calls will no longer be monitored. The DoH have advised strategic health authorities, local primary care trusts, and ambulance services to decide between them how best to care for patients with such non‐urgent healthcare needs.8
Skill mix
There is a dearth of evidence evaluating the impact of skill mix change in the health service. Most of the published work relates to doctor‐nurse substitution in primary and secondary care.9 While there is evidence that bringing primary care professionals into the ED may result in costs savings,10 nothing is known about the impact changes to the workforce in one setting have on other settings.
The emergency care practitioner (ECP) is a generic role that combines extended nursing and paramedic skills, arising out of a reconfiguration of emergency services and a series of changing workforce initiatives such as nurse practitioners and paramedic practitioners. The ECP role is intended to develop the skills of practitioners to enable them to be utilised across traditional organisational boundaries, to carry out initial assessment of patient need, and to either treat or refer to the appropriate care pathways.11,12
Evaluation
A national evaluation of the ECP schemes in England is currently underway. This paper reports the results of phase I of the evaluation. Phase II will examine the issues, including patient satisfaction, acceptability, and appropriateness and safety of care, in greater depth. Phase I examined the early development of ECP schemes as they become fully operational; identified the factors considered by key participants in the development of the schemes contributing to successful, safe, and appropriate operational frameworks; identified the patient groups who were receiving health services from an ECP; and provided initial estimates of the costs and cost consequences of the schemes.
METHODS
The evaluation consists of two phases. The study design of phase I (reported here) took an integrated mixed methods approach consisting of (a) quantitative studies (a primary survey and analysis of data collected routinely by the provider organisations); (b) an applied qualitative study; and (c) economic analysis.
Quantitative studies
Primary survey
A questionnaire was e‐mailed to ECP project leads in all 17 ECP sites in England. The questionnaire gathered data under several main headings:
Person specification
Training and education
Competences and scope of role
Operational settings
Local barriers to development of the scheme
Whether audit and evaluation systems were in place
Demand and workload
Financial information.
Routine data
Audit data is routinely collected on a voluntary basis by each ECP scheme. The data for 8575 first patient contacts between 1 January 2004 and 28 December 2004 were available for analysis from 11 of the 17 ECP sites. The age of the patients, how they accessed the ECP service, and their outcome pathways were recorded by first contact episodes. Ambulance use and avoidance was recorded for patients who accessed the service via a 999 emergency ambulance call. For patients accessing the ECP via primary care, the data recorded whether a general practitioner (GP) was required. For those self presenting at the ED, MIU, or WIC, the data recorded whether the patient required referral to a doctor or nurse practitioner within the acute setting. Finally, length of consultation was calculated from times recorded on the data sheets.
Applied qualitative study
Using a semi structured interview schedule, taped telephone interviews were conducted with 12 participants selected purposively by virtue of their key role in the ECP schemes in six pre‐selected sites (three urban and three rural areas) in England. The transcriptions were analysed thematically using framework principles for applied qualitative research.13
Economic analysis
The analysis of costs and cost consequences of adopting the local frameworks for service delivery was undertaken based on the information provided by project leaders in the descriptive survey. Information included recurrent costs (ECP salaries, consumables, administration costs, and overheads) and non‐recurrent costs (ECP training and transport where this information was made available by project leaders). The total costs were calculated per year according to their expected duration or lifetime to provide annual recurring cost estimates for each cost category (recurrent and non‐recurrent costs), based on a conservative sensitivity analysis of ECP contacts with between two and seven patients per ECP per shift.
Mixed methods framework
The results of all three studies were integrated around the central theme identifying the key factors influencing the configuration, implementation, and integration of the ECP schemes into the local health economy during the initial stages of their development.
RESULTS
Survey of ECP provider sites
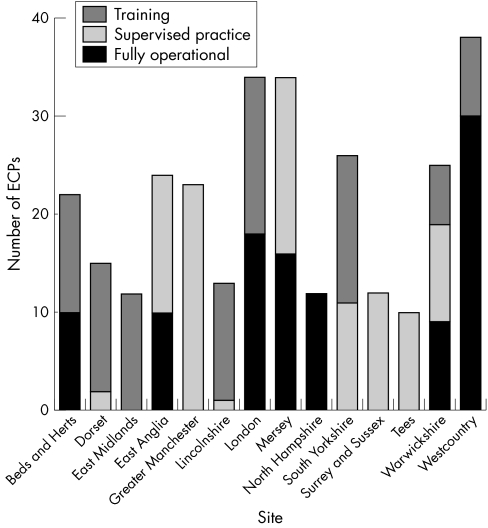
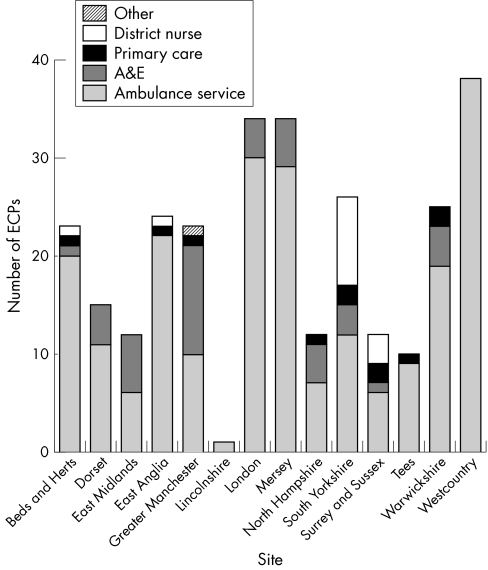
Of 17 sites, 14 (82.5%) responded to the questionnaire. The schemes are moving forward in different ways and at a different pace. Most of the operational ECPs had trained as paramedics in the ambulance service (77.4%). Some also had nursing qualifications (fig 1). The mean number of weeks for the ECP training course was 16.1 weeks (SD 3.4). The core skills covered by the courses are shown in table 1. With the exception of one site, all responding sites were allied to a higher education institution. The mean (SD) period of posteducation supervised practice was 19 (5.9) weeks. All sites conducted some form of assessment of competency at the end of each course. Of 14 sites, 12 (85.7%) had plans for continuing professional development of the ECPs. The ECP schemes were operating or planned to operate from a range of settings, which involved the recommended spread of ambulance service, ED, MIU, primary care, and WIC. Of the 14 sites, 10 (71.4%) were rotating, or planning to rotate, operationally across different settings within their local areas (fig 2). Clinical support and supervision was variable. At the time of the survey, some schemes did not have any formal systems in place. Two sites planned to provide a 24 hour service, and three further sites were focusing mainly on out of hours support for primary care. Four sites were running daytime services or spanning daytime and part out of hours support. One site had a discrete system of call activation. The others were either not running a discrete service or were in the course of developing it. Factors that were reported to explain the variation between the areas in how the ECP schemes were developing were (a) the providers that were partnered to the ECP schemes initially and (b) the configuration of existing services and local responses to wider legislative changes, for example, the new General Medical Services contract and European regulations on working times.
Figure 1 Status of ECP by site.
Table 1 Core skills taught by each course.
| Core skill | n (%)* | |
|---|---|---|
| Cardiovascular system assessment | 11 (91.7) | |
| Respiratory system assessment | 11 (91.7) | |
| Gastrointestinal system assessment | 10 (81.8) | |
| Neurological system assessment | 11 (91.7) | |
| Urological system assessment | 11 (91.7) | |
| Musculoskeletal system assessment | 12 (100) | |
| Dermatological system assessment | 10 (83.3) | |
| ENT system assessment | 11 (91.7) | |
| Ophthalmology system assessment | 12 (100) | |
| Consultation/communication skills | 12 (100) | |
| Assessment of minor illness | 12 (100) | |
| Assessment of minor injury | 12 (100) | |
| Assessment of the paediatric patient | 12 (100) | |
| Assessment of the elderly patient | 11 (91.7) | |
| Assessment of the acutely disturbed patient | 12 (100) | |
| Pharmacology | 10 (83.3) | |
| Legal and ethics issues | 12 (100) | |
| Evidence based practice | 12 (100) | |
| Research and audit | 10 (83.3) | |
| Paramedic skills: scene safety | 9 (75.0) | |
| Paramedic skills: recognition of death | 9 (75.0) | |
| Paramedic skills: advanced life support | 9 (75.0) | |
| Paramedic skills: driving course D1 level | 8 (66.7) | |
| Other | 5 (41.7) |
*Total responders, n = 12,
Figure 2 ECP background by site.
Routinely collected data
Data for 8575 patient episodes from 11 ECP sites were available. However, most of the data were drawn from three sites: West Country Ambulance Service, County Durham and Darlington, and South Yorkshire. These three sites accounted for 6122 of the 8575 records (71.4%).
ECPs attended patients of all ages, but 79% (n = 6803) were adults older than 16 years. The 11 schemes were operating from a variety of health settings. Patients accessed the ECPs by a variety of routes, and the spread between patients accessing the service via prehospital (32%); primary care (in hours and out of hours home visits) (29%); and acute care (self presenting to ED, MIU, or WIC) (39%) routes was fairly even.
The length of each ECP consultation was calculated by measuring time from when the ECP started the patient consultation to when it was completed. Overall, valid times were available for calculation from 7673 patient episodes (89.5%). The median time was 25.0 minutes with a range of 1 minute to 2 hours. In the sections below, times have been calculated for each service in which the ECPs were operating.
Outcomes (disposal of patients)
Overall, 4587 (53.4%) of patients accessing the ECP service via any route were discharged to their place of residence without immediate or later referral to another healthcare professional. Immediate referrals were made in 2260 cases (26.3%). From the data available, of these cases, around half (n = 1164, 51.5%) were referred to an ED, 267 (11.8%) to a GP, and 829 (9.6%) to health professionals in another hospital department via existing care pathways. The referral details for a further 1015 patients (44.9%) is not known because the relevant data were missing.
Ambulance
In total, 2724 patients (32%) accessed the ECP via the 999 service. ECPs were able to assess, treat, and discharge 43.5% of patients seen through this service route, with a further 52.6% being transferred to the ED or referred through the existing ECP care pathways. This referral may have been immediate or delayed (table 2).
Table 2 Referral by ECPs.
| Service | n (%) | |
|---|---|---|
| Ambulance service | 2724 | |
| Discharged by ECP | 1184 (43.5) | |
| Immediate referral to ED | 1046 (38.4) | |
| Discharged via ECP care pathway | 387 (14.2) | |
| Missing data | 107 (3.9) | |
| Primary care | 2500 | |
| Discharged by ECP | 1445 (57.8) | |
| Immediate referral to ED | 118 (4.7) | |
| Discharged via ECP care pathway | 233 (9.3) | |
| Immediate referral to GP | 267 (10.7) | |
| Missing data | 437 (17.5) | |
| Acute care | 3351 | |
| Discharged by ECP | 1958 (58.4) | |
| Discharged via ECP care pathway | 93 (2.8) | |
| Immediate referral within ED | 829 (24.7) | |
| Missing data | 471 (14) |
The available data shows that in 27% (n = 735) of cases no ambulance was sent out, while in a further 27.5% of cases (n = 746) the ambulance was stood down while en route. An emergency response from an ambulance was required in 29% (n = 779) of cases. The time for an ECP consultation referred by the 999 service was identified from 2490 (91.4%) episodes. The median time was 31 minutes (range 1 minute to 2 hours).
Primary care
Data from the 2500 records for patients who saw the ECP via a primary care route (a home visit, or an in or out of hours presentation to a GP surgery or a primary care centre) were analysed together. Approximately two thirds (67%) of patients who accessed the ECP via a primary care setting were discharged by the ECP either with or without referral via an ECP care pathway. There were 267 patients (10.7%) referred to a GP, and a further 5% (n = 118) were referred immediately to the ED (table 2). The time for an ECP consultation referred by the primary care service was identified from 2185 (87.4%) episodes. The median time was 20 minutes (range 2 minutes to 1 hour and 45 minutes).
Acute care
Of the patients who self presented to acute care settings, (MIC, ED, or WIC) (n = 3351), the ECP referred 25% (n = 829) immediately to another acute care professional within the acute care setting itself. The ECP managed more than 58% of the cases without further referral (table 2). The time for an ECP consultation referred by the primary care service was identified from 2998 (89.5%) episodes. The median time was 25 minutes (range 2 minutes to 2 hours).
Telephone interviews
Twelve interviews were completed with key personnel in six of the ECP sites. The participants were all involved at key stages in the development of the ECP schemes locally and/or nationally. Their direct experience provided strategic, managerial, medical, and clinical perspectives shaping the ECP service in its formative period. Factors perceived as contributing to a successful operational framework were a strategic vision that cut across traditional organisational boundaries and health professional roles, a well motivated and skilled workforce, integrating as a team with other services, which rotated across different clinical settings to provide the most appropriate level of care safely to patients.
Five of the six sites had introduced changes to their original plans. These changes had been driven by the local partnerships, case mix, and national initiatives, such as the new GMS contract. In the remaining site, the ECP scheme was developing very much in accordance with the original plans.
Strategies in place or considered to optimise ECP skills and foster a team based approach were appropriate targeting of 999 calls made to the ambulance services, amd localising response within defined geographical boundaries coinciding with market town or PCT areas. Involvement of senior executive and nursing personnel in the initial negotiations, continuing integration of ECP and other services, and moderated or brokered introduction of ECPs into the more formal structures of ED departments were seen as vital. Recurring themes emerging as important across the ECP schemes in these six participant sites were: patient safety; the need for appropriate levels of clinical governance and supervision, particularly in a pre‐hospital setting; a generic element to the education and training to facilitate the transferability of skills between NHS providers; and workforce issues around the safety, recruitment, and retention of staff.
Economic analysis
Data were provided by 12 of the 14 sites responding to the questionnaire. Not all the data were complete. The estimated number of ECP patient contacts per site annually was between 368 and 1288. The estimated costs per ECP were £32 754 (range £31 119 –36 407) and, based on a conservative assumption that ECPs will have between two and seven patient contacts per shift, the cost of an ECP contact ranged between £24 and £29. This is equivalent to the estimated cost of an ED visit of around £55.14
DISCUSSION
Main findings
The early indications are that the ECP schemes are moving forward in different ways and at a different pace. At the time of study, half the 17 sites investigated were operational. Most ECPs had trained as paramedics; some had nursing qualifications. Their existing skills and competencies have been extended through a range of educational programmes (mostly in higher education establishments), training, and assessment. In areas where the schemes were well established, the routine data available show that ECPs are dealing with 54% of patients without the need for an immediate referral to another healthcare professional or emergency transportation to ED. However, in the remaining 46% of contacts, a further referral or contact was made, and this raises the question of whether the ECPs were merely adding another stage to the patient pathway. The ECP service would appear to be operating in a timely way, with consultation time taking around 30 minutes. However, control data would be required to compare how long patients spend in consultation with other professionals such as GPs, ambulance paramedics, ED doctors, and nurse practitioners.
In a subset of six sites, five had adapted their original plans for how the ECP service would operate. The stimuli for change were the GMS contract and UK regulations around working time, and local partnerships and differences between the actual case mix that ECPs were dealing with and those anticipated at the outset. Without exception, the study revealed a positive commitment to the development of the schemes. Criteria for a successful scheme were identified as strategic vision unfettered by traditional organisational and health professional boundaries, an appropriately skilled workforce integrating with other services, rotating across different settings in a team based approach to provide a safe and optimum level of care to patients. Important themes to emerge were patient safety, the need for generic standards of practice with sufficient flexibility to respond to local need, appropriate levels of clinical governance and supervision especially in a pre‐hospital setting, and workforce issues around recruitment and retention of staff.
Limitations
The studies took place within tight deadlines, which restricted more detailed data collection and analysis. Only 50% of the sites surveyed were operational. Phase II will conduct a detailed study of four selected sites, and will revisit the emergent themes identified as important in phase I. Patient contact data were incomplete and limited in content. This is primarily because data submission by each ECP scheme was voluntary, and data collection was not designed for research purposes, but to monitor activity in each site. Consequently, we do not know how representative our quantitative findings are. However, the patient contact data available in respect of the proportion of cases dealt with entirely by an ECP, representing an emergency ambulance journey avoided or a saved contact with another health professional, corresponded closely with those predicted when the schemes were set up.
Comparability with other studies
A number of studies15,16,17 investigating the possibility of paramedics identifying patients who did not require ED care concluded that paramedics could not safely or accurately determine which patients required ambulance transport or ED care. These findings were reflected in the report on the future of ambulance services in the UK.18 This stated that ambulance services needed to develop a wider range of types of responses and clinical roles for staff in order to provide a variety of appropriate care pathways for patients, and concluded that, potentially, practitioners in emergency care:
“…..could bring ED doctors, nurses, and paramedics together in providing emergency care in a way which current organisational models could not. Breaking down professional boundaries and raising the clinical skills of paramedics could lead to new ways of working, closer partnerships and better outcomes for patients”.
The ECP scheme is currently the subject of phase II of the national evaluation. Whether the early findings will be maintained in phase II has yet to be confirmed. However, our initial findings suggest that the ECP schemes are beginning to reach targets and fulfil expectations. Based on the routine data from three sites, the actual proportion of cases being dealt with by ECPs without the need for referral (54%) is in line with the predicted figures.
CONCLUSIONS
The early indications are that ECP schemes are becoming established and achieving their objectives. If the estimates provided are supported by further study into patient outcomes and satisfaction, then the ECP, by extending existing practitioner skills and utilising NHS resources more efficiently, may provide patients with an appropriate level of emergency care to meet their needs.
ACKNOWLEDGEMENTS
We would like to acknowledge the help of C Horton from the Modernisation Agency who undertook an enormous amount of data entry relating to the routine data collected from ECP sites.
Abbreviations
DoH - Department of Health
ECP - emergency care practitioner
ED - emergency department
GP - general practitioner
MIU - minor injury unit
WIC - walk in centre
Footnotes
Funding: This study has been funded by the Department of Health Changing Workforce Programme.
Competing interests: there are no competing interests
Ethics committee approval for this study was granted by Central Manchester Multi‐Research Ethics Committee, reference no. 04/Q1407/281.
References
- 1.Department of Health The NHS plan. London: DoH, 2001
- 2.Department of Health Reforming emergency care. London: DoH, 2001
- 3.Audit Commission By accident or design: improving accident & emergency services in England and Wales. London: HMSO, 1996
- 4.Audit Commission Review of national findings. Accident & emergency. London: Audit Commission, 2001
- 5.Department of Health Statistical bulletin 2000/13: ambulance services, England: 2002–3. London: DoH, 2003
- 6.Audit Commission Life in the fast lane: value for money in emergency ambulance services. London: Audit Commission, 1998
- 7.Government Statistical Service National Statistics: Ambulance services, England, 2003–04. London: DOH,
- 8.Department of Health Freedom for ambulance staff to deliver healthcare tailored to patients' needs. London: DoH 2004, 0311
- 9.Horrocks S. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002324819–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts E, Mays N. Can primary care and community based models of emergency care substitute for the hospital accident and emergency department. Health Policy 199844191–214. [DOI] [PubMed] [Google Scholar]
- 11.Mason S, Wardrope J, Perrin J. Developing a community paramedic practitioner intermediate care support scheme for older people with minor conditions. Emerg Med Jl 200320196–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NHS Modernisation Agency/Department of Health The emergency care practitioner, report 3990. London: DoH, 2004
- 13.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In Bryman A, Burgess RG, eds. Analysis of qualitative data. London: Routledge, 1995
- 14.Sheffield Health Economics Group Reference costs. Sheffield: Sheffield Health Economics Group, University of Sheffield, 2003
- 15.Hauswald M. Can paramedics safely decide which patients do not need ambulance transport or emergency department care? Prehosp Emerg Care 20026383–386. [DOI] [PubMed] [Google Scholar]
- 16.Silvestri S, Rothrock S G, Kennedy D.et al Can paramedics accurately identify patients who do not require emergency department care? Prehosp Emerg Care 6387–390. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt T, Atcheson R, Fedruik C.et al Evaluation of protocols allowing emergency medical technicians to determine need for treatment and transport. Acad Emerg Med 7663–669. [DOI] [PubMed] [Google Scholar]
- 18.Nicholl J.The future of ambulance services in the UK Draft Report to Department of Health. Sheffield: Sheffield University, 2000