Abstract
Renal angiomyolipoma (AML) is a benign renal tumour and is nowadays considered a relatively common lesion. When an AML increases in size or becomes symptomatic, embolisation via the renal artery should then be considered, because rupture is an important complication and interventional therapies are required to stop bleeding. We present a 21 year old woman who was seen at the emergency department following a low velocity trauma. After a period of 9 weeks, clinical examination and radiological examination revealed a haemorrhage from a renal AML, which was treated by selective embolisation. A discussion of the relevant literature is also presented.
A 21 year old woman presented to the emergency department after a low velocity bicycle to scooter trauma, where the diagnosed injuries were a cerebral contusion and fractures of the metatarsal IV and V in the left foot. She was treated conservatively and discharged the same day. Nine weeks later, she was admitted to our hospital with general fatigue, nausea, vomiting, and sudden abdominal and right flank pain. Physical examination revealed a painful right abdomen with guarding and no palpable tender mass.
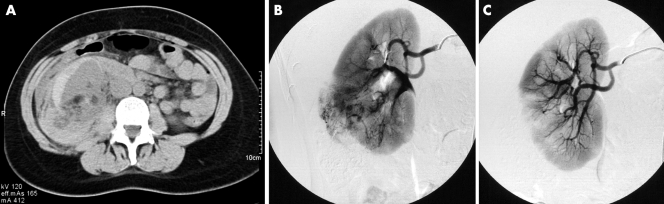
Laboratory examination showed a decrease in haemoglobin level (from 8.2 to 5.6 mmol/l) and microscopic haematuria. There were no other abnormalities, and vital signs were stable. Subsequent abdominal computed tomography (CT) scan was performed, revealing a right renal rupture with per‐renal haemorrhage (fig 1). The patient was treated conservatively.
Figure 1 (A) Abdominal computed tomography scan showing a renal angiomyolipoma with perirenal haematoma in the right kidney. (B, C) Renal angiography showing (B) the right kidney with the angiomyolipoma; (C) after selective embolisation of the renal angiomyolipoma.
Two months later, follow up abdominal ultrasonography confirmed a renal angiomyolipoma (AML), 45×35 mm in size, as the cause of the retroperitoneal haemorrhage. The patient later underwent a successful selective embolisation of the blood supply of the AML through the right renal artery using a microcatheter and polyvenylalcohol particles (figs 2 and 3). The patient recovered without complications. She has remained free of recurrent disease and symptoms during 15 months' follow up.
DISCUSSION
Renal AML is one of a family of neoplasms derived from perivascular epithelial cells.1,2 Pathophysiologically there are two types of AML: classic renal AML containing smooth muscle, vascular, and fat tissue, and very rarely infiltrating perirenal tissue; and a second type of AML containing a large fourth component, perivascular epithelioid cells, making it more aggressive than the classic renal AML.1,2,3,4,5
Renal AML is nowadays considered a relatively common benign lesion, and it is estimated that over 10 million people worldwide have the lesion. A large study involving 17 941 Japanese patients showed an incidence of 0.1% in male and 0.22% in female patients.6 Approximately 64–77% of tumours < 40 mm in diameter are asymptomatic, although 82–90% of AML ⩾ 40 mm produce symptoms.3 In symptomatic patients, the classic Lenḱs triad includes flank pain, a palpable tender mass, and signs of internal bleeding (haematuria), caused by intracapsular or retroperitoneal haemorrhage. Other symptoms may include nausea, vomiting, fever, anaemia, renal failure, and hypotension.1,2,7,8
There are three types of haemorrhagic aetiology. Wünderlich's syndrome, a spontaneous retroperitoneal haemorrhage of non‐traumatic origin originating from the AML occurs in up to 50% of patients with tumours > 40 mm.7 Secondly, after trauma, a renal AML can manifest with bleeding or rupture, even after low velocity trauma. Third is the seldom seen rupture of renal AML during pregnancy, which can be mistaken for extra‐uterine gravidity or solution.1,2,8 It can be debated whether our patient had a spontaneous retroperitoneal haemorrhage or whether it was due to delayed effects after low velocity trauma. The relatively short period of 9 weeks between trauma and clinical symptoms is highly suggestive, but hypothetical.
Abdominal CT scanning is the diagnostic tool of choice to diagnose and differentiate between various causes of a renal mass, and assess the size of the AML and the extent of haemorrhage.1,4,8 Fat density within a non‐calcified renal mass remains the most important diagnostic finding of AML.8 Calcification is very important; if calcification is detected, a renal cell carcinoma is the most important differential diagnosis.8 Biopsies in the artery rich tissue can be hazardous and are often not necessary to establish the diagnosis. On ultrasonography, the fat content will be seen as a hyperechoic lesion, strongly suggesting the diagnosis of AML. Ultrasonographic diagnosis can be difficult when the AML has a relatively large proportion of muscle tissue or when there is haemorrhage, thus for these situations a CT scan is advised.
Oesterling et al have proposed the following treatment protocol based on size and symptoms of AML.3 Patients may be followed conservatively with yearly CT scans for those with isolated AML < 40 mm in diameter and 6 monthly scans for those with lesions ⩾ 40 mm for assessment of growth. Patients with TSC and AML < 40 mm in diameter should be followed by a semiannual CT scan. When an AML increases in size or becomes symptomatic then embolisation via the renal artery should be considered. Patients with TSC and an AML ⩾40 mm in diameter have a high risk of development of symptoms and may also require arterial embolisation.1,2,3,5 The principal use of angiography for AML is for therapeutic embolisation after the diagnosis has been established by other means. Embolisation is the preferred therapy and appears to be the most successful nephron sparing procedure. A large tumour can be managed with selective arterial embolisation to reduce the size or to stop bleeding during acute situations. The recurrence of a treated AML in the unilateral kidney or a metachronous presentation of a new AML in the contralateral kidney rarely occurs.5
One should always be watchful for retroperitoneal haemorrhage in patients with renal AML after trauma of which the patient had no abdominal complaints at the time of presentation. Vice versa, familiarity with AML may prompt recognition of this disease as a possible cause in a patient presenting with a retroperitoneal haemorrhage. Life threatening complications can then be avoided for diagnostic tests and therapeutic interventions are readily available.
Abbreviations
AML - angiomyolipoma
CT - computed tomography
Footnotes
Competing interests: there are no competing interests.
References
- 1.Bissler J J, Kingswood J C. Renal angiomyolipomata. Kidney Int 200466924–934. [DOI] [PubMed] [Google Scholar]
- 2.Eble J N. Angiomyolipoma of kidney. Semin Diagn Pathol 19981521–40. [PubMed] [Google Scholar]
- 3.Oesterling J E, Fishman E K, Goldman S M.et al The management of renal angiomyolipoma. J Urol 19861351121–1124. [DOI] [PubMed] [Google Scholar]
- 4.Pruijm M T, Falke T H, Peltenburg H G. [Retroperitoneal bleeding caused by renal angiomyolipoma]. Ned Tijdschr Geneeskd 20031471696–1699. [PubMed] [Google Scholar]
- 5.Steiner M S, Goldman S M, Fishman E K.et al The natural history of renal angiomyolipoma. J Urol 19931501782–1786. [DOI] [PubMed] [Google Scholar]
- 6.Fujii Y, Ajima J, Oka K.et al Benign renal tumors detected among healthy adults by abdominal ultrasonography. Eur Urol 199527124–127. [DOI] [PubMed] [Google Scholar]
- 7.Albi G, del Campo L, Tagarro D. Wunderlich's syndrome: causes, diagnosis and radiological management. Clin Radiol 200257840–845. [PubMed] [Google Scholar]
- 8.Lemaitre L, Claudon M, Dubrulle F.et al Imaging of angiomyolipomas. Semin Ultrasound CT MR 199718100–104. [DOI] [PubMed] [Google Scholar]