Abstract
Background
This study set out to quantify the immediate costs to the North East Ambulance Service (NEAS) of attending to fallers.
Methods
Data from the Newcastle, UK area were collated by NEAS to identify those aged over 65 who had fallen and required an assistance only call or were subsequently transported to an Accident and Emergency (A&E) department. The 2001 census data for the total population served by NEAS in Newcastle were obtained.
Results
The total population of Newcastle over the age of 65 was 41 338. Over 7 months NEAS attended to 1504 falls in Newcastle (at £115 per call out, this equates to £172 960). The faller was transported to A&E on 1339 occasions, while 165 falls required assistance only (11% of total) (36 falls requiring NEAS assistance per 1000 Newcastle population aged over 65 in 7 months). The total time on site for ambulance crews attending to fallers was 377.1 h (15.7 days in 7 months or 2.25 days per month). As the cost of emergency ambulance time is £123/h, the total cost was £46 383.30. Therefore, in Newcastle, attending to fallers in the community costs NEAS £376 018 per year (£145.83 per fall or £9.10 per person over the age of 65 per year).
Conclusion
NEAS attend to a significant number of older people who fall in the community. In Newcastle alone the cost of this service equates to over 2 days of emergency ambulance crew time per month. Studies are needed to determine whether responding to falls in the community differently would be cost effective.
Keywords: ambulance, cost, falls
Current data suggest that 35% of those over 65 years of age fall annually.1 The numbers of fallers actually presenting to medical services are considered to significantly underestimate the size of the problem. Falls guidelines recommend proactive identification of fallers, and innovative strategies need to be introduced to achieve this.2 Surprisingly, the true prevalence of community falls in older people who do not present directly to medical services is unclear.
Falls are costly in terms of morbidity for an individual, and also in terms of expense to health care systems. Previous studies examining health care expenses suggest costs of approximately £2000–£3000 per faller with hospital costs accounting for 50% (UK) to 80% (NZ) of these costs.3,4 The costs of falls to other agencies such as the ambulance service are currently unknown. However, it is recognised that falls do come to the attention of the ambulance service and it has been suggested that the ambulance service is in a unique position of having access to a potentially high risk population who might otherwise not seek medical attention.5 Ambulance crews called to those who fall may either provide assistance only (pick up service) or they may provide assistance and then transfer the faller to hospital.5
This study set out to quantify the number of fallers who call an ambulance in the North East of England and then to use these data to calculate the immediate costs of attending to fallers for the North East Ambulance Service (NEAS) and to ascertain outcome. This study sought to document the costs of falls in older people to an organisation outside hospitals as a means of highlighting how interventions to prevent falls could be cost effective.
Methods
We set out to determine the number of fallers coming to the attention of NEAS and to use these data to calculate the immediate costs of attending to these fallers in the community.
NEAS has operational boundaries from Northumberland in the north to the south of County Durham. The NEAS have identifiable ambulance costs of £115 per call out and £123 per hour of site time; these data are readily available from the NEAS annual financial report 2004–2005 (see http://www.neambulance.nhs.uk/Annual%20Accounts.htm).
Data were collated prospectively between 1st June and 31st December 2004 from the Newcastle upon Tyne area utilising existing NEAS data bank information. Data considered concerned (i) all assistance only calls to those over 65 years of age who had fallen and did not subsequently require attendance at Accident and Emergency (A&E), and (ii) all ambulance calls to those over 65 years of age who had fallen and were subsequently transported to the one A&E department in the city. The proportions of those over 65 years of age presenting with a fall were compared to the normal population in the same area served by NEAS in Newcastle using data from Census 2001 (http://www.newcastle.gov.uk/pr.nsf/a/censuspopulationnew#Age%20Profile).
When attending to fallers, to determine whether transfer to A&E is required NEAS perform a standardised assessment which includes history, physical examination for injuries, heart rate, and blood pressure.
Data were stored anonymously and Caldicott Guardians in all organisations were aware of the use of data.
Results
The total population of Newcastle (Census 2001) was 259 536 with 41 338 of these being over the age of 65 (16%). The total number of falls coming to the attention of NEAS in Newcastle in the 7 month study period was 1504. As the cost per NEAS call out is £115, this equates to a total call out cost of £172 960 over 7 months.
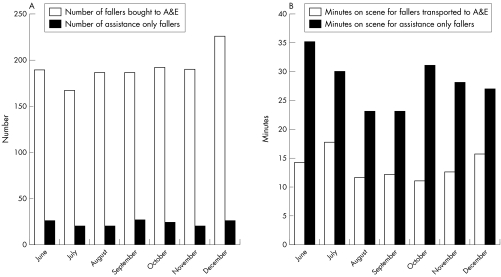
The total number of falls where NEAS took the faller to A&E was 1339, while 165 fallers (11% of total) required assistance only (fig 1). The number of fallers coming to the attention of NEAS remained relatively constant month by month, varying between 167 and 226 fallers subsequently being taken to A&E and 20 and 26 fallers who required assistance only. Using the 2001 census data allowed us to crudely estimate that this equated to 36 falls coming to NEAS attention per 1000 Newcastle population over the age of 65 in 7 months (or 62 per 1000 population per year).
Figure 1 (A) Number of fallers seen by NEAS in a 7 month period who were subsequently transported to A&E. (B) Number of fallers seen by NEAS in a 7 month period where assistance only was provided and the mean number of minutes on scene.
The costs for NEAS as a business include not only the original call out costs but also costs related to the length of time each ambulance crew spends on scene, which is costed at £123 per hour of crew time.6 The total number of hours on site for the ambulance crews attending to fallers in Newcastle over the 7 month period was 377.1 h (15.7 days in 7 months or 2.25 days per month) of emergency crew time. This is a total on scene cost of £46 383.30. Therefore, taken together with the original call out costs for ambulance crews, in Newcastle the costs for NEAS to attend to fallers in the community was £219 343.30 over 7 months or approximately £376 018 per year. This is an average of £145.83 per fall or £9.10 per person over the age of 65 in Newcastle per year.
However, the cost differential between those fallers transported by NEAS to A&E and those where assistance only was provided is seen when the time on scene is considered. Mean (SD) number of minutes on scene for assistance only fallers was significantly longer (30 (10) min; p<0.05) compared to the minutes on scene to attend to fallers who were subsequently taken to A&E (14 (16) min). Despite there being proportionately fewer fallers where assistance only is provided (11% of total), the time on scene leads to a cost differential between fallers transported to A&E of £142.40 per case compared to £173.16 per faller where assistance only is provided.
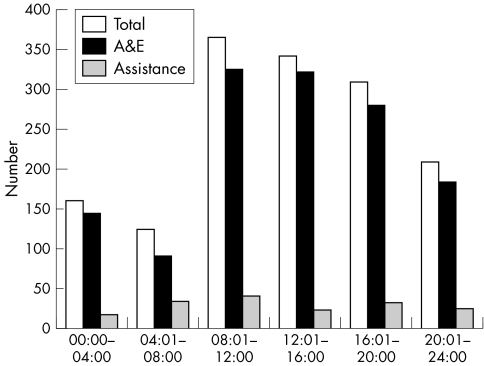
Falls reported to NEAS were predominantly during the daytime (08:01–20:00 h) (67%; fig 2A). However, when considering those who were brought to A&E, significantly more falls (69%; fig 2B) occurred during the daytime compared to only 56% for those requiring assistance only (fig 2C) (χ2: p<0.0001).
Figure 2 The times of day when NEAS attended to fallers over a 7 month period.
Interestingly, for those requiring assistance only calls (pick up), 34% of calls received by NEAS for fallers were from sheltered housing organisations with 14% of these calls coming from one sheltered accommodation organisation alone. For those fallers transported to A&E, 14 were from residential care, 21 from nursing care, and only four from sheltered accommodation.
Audit data confirm that 26% of fallers over the age of 65 attending A&E were admitted, with 10% being referred to a liaison nurse service. The other 64% were seen and discharged.
Discussion
This study confirms that NEAS attend to a significant number of older people who fall in the community. The costs of this service in Newcastle alone equate to over 2 days of emergency ambulance crew time per month spent dealing entirely with falls in the community. Previous studies suggest that there is a cost of £2000–£3000 per faller.4,5 Our study confirms that the costs to ambulance services account for almost an additional 10% of these costs in the UK.
Although the proportion of falls where assistance only is provided, that is where NEAS are not required to transport the patient to A&E, is small compared to those where transport is required, the time on scene with these patients is significantly longer and as a result the costs of this service are higher compared to transporting fallers to A&E. Our data suggest that agencies who care for older people, such as sheltered accommodation services, may be utilising the emergency ambulance service as a first line for assistance with fallers. It could be argued that the use of emergency ambulances to provide this service is inappropriate and that studies examining the relative cost effectiveness of alternative pathways, such as care alarms or lifting teams, are needed.
Similarly, only 26% of fallers who attended A&E were admitted, suggesting that as regards those who have not sustained injuries requiring hospitalisation, investing in rapid response multidisciplinary community falls teams may be more appropriate and have a cost benefit. Further work needs to be carried out to determine whether fallers in the community have reversible risk factors and how appropriate interventions can best be delivered.
The use of ambulance crews to respond to fallers has been controversial. Some suggest that the use of ambulance paramedics could be increased by allowing them to treat some patient groups (such as fallers) at home,6 while opponents suggest that the use of an alternative response could have major benefits, both in terms of increasing the ability of the ambulance crew to respond faster to clinically more urgent calls and improving the cost effectiveness of the health service.7
One study performed in the UK has shown that there are differences in those fallers where the ambulance crew provided assistance only compared to those who were transported to hospital, with the untransported (assistance only) fallers being significantly older and more likely to be housebound, require the use of assistive devices, and have lower mental test scores.5
Our study has several limitations. We performed the study over a 7 month period and it could be argued that data could be skewed by acquiring a monthly rate of fallers (or costs) derived from information covering 7 months. We would suggest, however, that by examining June to December we have probably under‐represented the number of fallers (and hence the costs) as we have excluded the winter months. We have utilised data from one city and the findings need to be replicated in rural and smaller urban areas to determine whether the results from Newcastle are applicable to other ambulance services. Newcastle has had a Falls Service since 2001 and it could be suggested, therefore, that the number of fallers (because active interventions to prevent further falls have been delivered on a population basis in Newcastle) is underestimated in this study. All data sources used in this study are currently immediately available through all Ambulance Trusts and this process of data sharing and active collaboration in service development could be used as an example to other Ambulance Trusts and Falls Services.
This study highlights for the first time the fact that reducing the number of falls in the community will have financial and operational benefits for organisations such as the ambulance service. Developing cross‐organisational initiatives to identify fallers to local falls teams allowing early intervention to prevent recurrence will potentially have benefits beyond the NHS.
Footnotes
Competing interests: none declared
References
- 1.Tinetti M E, Speechley M, Ginter S F. Risk factors for falls among elderly persons living in the community. N Engl J Med 19883191701–1707. [DOI] [PubMed] [Google Scholar]
- 2.American Geriatrics Society et al Guideline for the prevention of falls in older persons. J Am Geriatr Soc 200149664–672. [PubMed] [Google Scholar]
- 3.Hall S, Hendrie D. A prospective study of the costs of falls in older adults living in the community. Aus N Z J Public Health 200327343–351. [DOI] [PubMed] [Google Scholar]
- 4.Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the UK. J Epidemiol Community Health 200357740–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Close J, Halter M, Elrick A.et al Falls in the older population: a pilot study to assess those attended by London Ambulance service but not taken to hospital. Age Ageing 200231488–489. [DOI] [PubMed] [Google Scholar]
- 6.Mason S, Wardrope J, Perrin J. Developing a community paramedic practitioner intermediate care support scheme for older people with minor conditions. Emerg Med J 200320196–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marks P J, Daniel T D, Afolabi O.et al Emergency (999) calls to the ambulance service that do not result in the patient being transported to hospital: an epidemiological study. Emerg Med J 200219449–452. [DOI] [PMC free article] [PubMed] [Google Scholar]