Abstract
Objective
The social etiology of adolescent injury remains poorly understood. The Population Health Framework suggests that the etiology of adolescent injury involves interactions between individual risk factors and the natures of adolescent environments. The purpose of this study was to apply this framework to examination of relationships between adolescent risk taking and injury, and the potential modifying effects of supportive home and school environments.
Methods
The analysis was conducted in a representative sample of 7235 males and females (10–16 years old) from Canada. Results were based on records from the 2001/02 World Health Organization Health Behaviour in School‐Aged Children Survey. Individual items and factor analytically derived scales were used to describe and then model injury outcomes, risk behaviors, perceived home, and school climates, and the relationships between these variables in a theory driven etiological analysis.
Results
Adolescents with supportive home and school environments experienced lower relative odds of engagement in risk taking behavior and lower relative odds of injury. Gradients were observed between the extent of adolescent risk taking and the occurrence of injury. Interactions were not observed between risk taking behavior, perceived support in home and school climates, and injury.
Conclusions
Risk taking is common among adolescents and plays a role in the etiology of injury. Supportive social climates clearly protect adolescents from engaging in these behaviors, and also the occurrence of some forms of injury. However, once an adolescent chooses to engage in risk taking behaviour, a supportive environment may not protect them from injury.
Keywords: adolescent behaviour, social support, etiology
The population health approach to the study of injury suggests that the etiology of adolescent injury involves interactions between individual risk factors and the environments in which children live.1 The exact nature and effects of these interactions remain poorly understood. Study of these interactions is likely to lead to advances in understanding about injury etiology as much of the existing literature is based upon conventional risk factor analyses of an atheoretical nature.
Adolescent risk taking has been identified as a leading determinant of injury. Multiple risk behavior (the simultaneous engagement in overt risks such as smoking, drug and alcohol use, and truancy)2 is an established individual risk factor for adolescent injury that exists independently of other fundamental risk factors3,4,5 including socioeconomic status.6 The multiple risk behavior and adolescent injury relationship has been observed consistently across groups defined by demographics,3 different injury types,4 and nationalities5 The conceptualization of risk behavior as a multiple risk concept mirrors concepts such as sensation seeking and antisocial behavior that are prominent in the behavioral literature.7
At an environmental level, supportive social climates can minimize engagement in risk taking and may also protect adolescents from the occurrence of injury.8 In addition, supportive social environments possibly mitigate the strength of associations between risk behavior and injury. Some adolescent social environments (for example, homes, schools) are especially modifiable through policy and other preventive strategies.9,10
We had the opportunity to use a large national survey to simultaneously examine individual (multiple risk behavior) and environmental (perceived social climates) risk factors for adolescent injury, and their potential interactive effects. We hypothesized the following: (1) perceived climatic support at home and school is inversely associated with adolescent engagement in risk behaviors; (2) perceived climatic support at home and school is inversely associated with the occurrence of various types of adolescent injury; (3) interactions exist between risk behaviors, social climate, and injury such that high perceived levels of climatic support attenuate associations between risk behaviors and the occurrence of injury.
Methods
Study population and procedures
The study was based on Canadian records (n = 7235) from the Health Behaviour in School‐Aged Children Survey (HBSC), a World Health Organization collaborative cross national study.11 School based anonymous surveys were conducted during the 2001–02 academic year according to a common international protocol.12 Schools and then school classes (grades 6–10) were selected for study using a weighted probability technique to ensure that the sample was representative by regional geography and key demographic features (religion, community size, school size, language of instruction).11,12 The sample size was sufficient to provide confidence intervals of +/− 3% for national estimates with sample design effects no more than 1.4 times greater than would be obtained from a simple random sample.12 Institutional ethics approval was obtained from the Queen's University General Research Ethics Board.
Measures
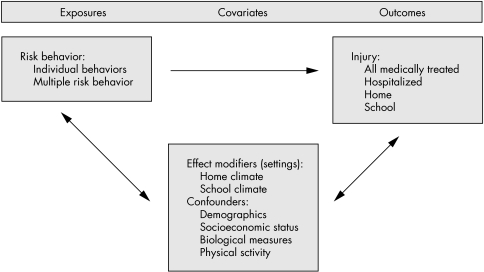
Variables used in this study were obtained from the self‐report questionnaire consisting of 122 core questions. Individual items and factor analytically derived scales were used to describe and model injury outcomes, risk behaviors, perceived home and school climates, and the relationships between these variables in a theory driven etiological analysis. For statistical modeling purposes, items were organized conceptually according to a variation of the population health framework (see fig 1).1
Figure 1 Theoretical basis for modeling, based on the Population Health Framework.
Injuries
Participants were asked to report the frequency of all injury events during the 12 months prior to the survey that required medical attention from a doctor or a nurse. Additional questions identified specific types of injury by severity (for example, hospital admissions) and location of injury (for example, home and school injuries).
Risk behaviors
Common risk behaviors were documented as follows: current smoking (four response categories: smoke every day through I do not smoke), drunkenness during lifetime (five categories: never through more than 10 times), current use of seatbelts (five categories: always through never), cannabis use during lifetime (seven categories; never through 40 or more times), other illicit drug use (for example, ecstasy, cocaine, LSD) during lifetime (seven categories, never through 40 or more times), non‐use of condoms during most recent sexual intercourse (three categories: never had sexual intercourse, yes, no). Participant responses for each item were classified into three categories corresponding to frequency of engagement in the risk behavior (never, occasional, frequent). These reclassified measures were converted into a factor analytically derived scale that describes engagement in multiple risk behavior (see below).4
Perceived home and school climates
HBSC contains a series of questions describing perceptions about home and school settings.12,13,14 These were rated by students using five‐point Likert scales, with response options of (1) strongly agree through (5) strongly disagree. Examples of individual home climate items included students' opinions about parental understanding, parental trust, ease of communication with parents, and happiness of home life. Examples of school climate items included perceptions of safety at school, adolescents' sense of belonging at school, the fairness of school rules, and the school atmosphere. Confirmatory factor analyses were also used to construct a series of factors that reflected home and school climates, respectively. Following their construction, participant scores for individual scales indicated by these factors were categorized into three levels (high, medium, low levels of support) based upon mean values of items included in the scales.
Scale confirmation
Maximum likelihood factor analyses were run with oblique rotations using SPSS (version 12.0 for Windows). Model fit was determined using the Scree plot, the interpretability of the pattern matrix, and the value of the root mean square error of approximation (RMSEA). RMSEA values of 0.085 or less were considered an acceptable fit; values of 0.086 to 0.10 were considered marginal fits. Following the exploratory factor analyses, confirmatory factor analyses with the maximum likelihood method of estimation were run in LISREL (version 8.0). Four goodness of fit indices were used to evaluate the tested models.
For the multiple risk behavior scale, exploratory analyses indicated a one‐factor model that included the six risk behavior items as the best fit, with an RMSEA = 0.082 (CI = 0.070 to 0.095). The confirmatory factor analysis indicated an acceptable fit (for example, RMSEA = 0.085). Exploratory analysis for the home climate scales indicated a three‐factor model as the best fit, with an RMSEA = 0.059 (CI = 0.056 to 0.062). The factor (six item scale) used in subsequent analyses captured parent/student trust, communication, support, and happiness at home. The confirmatory factor analysis indicated an acceptable fit (for example, RMSEA = 0.058). Exploratory analyses for the school climate scales indicated a four‐factor model, with an RMSEA = 0.035 (CI = 0.033 to 0.037). The factor (four item scale) used subsequently captured the concept of fairness and safety at school. The confirmatory factor analysis indicated an acceptable fit (for example, RMSEA = 0.051).
Confounders
Items treated as confounding variables included standard demographic measures (sex, grade level), physical activity (using a scale developed by Prochaska15), and two measures of socioeconomic status (self‐rated family affluence16 a measure of food poverty as indicated by going to bed or school hungry). Inclusion of these variables was based upon existing etiological literature3,4,5,6,17 and a priori arguments surrounding the epidemiological definition of confounding.18
Analyses
Descriptive analyses were used to estimate the prevalence of frequent engagement in individual risk behaviors (six types) then frequent engagement in multiple risk behavior, stratified by perceived level of climatic support (high, medium, low support) and grade level (6–8, 9–10). Multiple logistic regression analyses, with adjustment of standard errors surrounding β‐coefficients for clustering (design effect of 1.2),11,12 were used to estimate the adjusted relative odds for frequent engagement in the risk behaviors by perceived climate within grades. Similar analyses (descriptive, logistic regression) were then used to estimate the prevalence and relative odds of different types of injury by perceived level of climatic support and grade. We then applied our theoretical framework (fig 1) to examine potential interactions between multiple risk behavior and the occurrence of various types of injury, stratified by climate (high v medium/low support) and grade level (6–8, 9–10). Statistical interactions between perceived level of climatic support (continuous scale), multiple risk behavior (continuous scale), and injury (dichotomous outcomes) were also assessed by including a product term in the multiple logistic regression models. This analysis was used to investigate the protective roles of home and school settings as potential modifiers of associations between engagement in risk taking and the occurrence of injury. All analyses were performed in SPSS (version 12.0, Chicago, IL, USA).
Results
Sample
A total of 7235 children participated in the 2001/02 Canadian HBSC, of which 4851 were in grades 6–8 and 2384 in grades 9–10. 74.2% of the students selected for the study completed the questionnaire, and their demographic profile was representative of Canadians in the same age range.19 6757 and 7106 records with complete information on key exposures, outcomes, and covariates were included in the home and school etiological analyses, respectively (completion rates of some of the more sensitive (for example, home climate) items were modestly lower than other items).
Perceived climate and risk behavior
Prevalence of engagement in risk behaviour varied by grade level, and levels of support at home and at school. This finding was true for each of the six individual risk behaviors under study, as well as for the multiple risk behavior scale (table 1). The strength and consistency of the observed gradients in risk behavior by perceived level of climatic support was further illustrated in the multiple logistic regression analysis (see online table A at http://www.injuryprevention.com/supplemental). For both home and school settings, the relative odds of frequent engagement in each of the individual risk behaviors, as well as frequent engagement in multiple risk behavior, rose in association with lower perceived levels of climatic support.
Table 1 Prevalence of individual and multiple risk behaviors among students in grades 6–10, stratified by perceived climate at home and school.
| Setting: risk behavior | Prevalence of frequent engagement in risk behaviour, by perceived climate (prevalence; % (SE)) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Grades 6–8 | Grades 9–10 | |||||||||||
| High support | Medium support | Low support | High support | Medium support | Low support | |||||||
| Home | (n = 3726) | (n = 904) | (n = 199) | (n = 1506) | (n = 685) | (n = 187) | ||||||
| Multiple risk behavior | 2.9 | (0.3) | 7.6 | (1.0) | 20.9 | (3.4) | 9.4 | (0.9) | 20.1 | (1.8) | 33.9 | (4.1) |
| Smoking | 1.5 | (0.2) | 3.8 | (0.7) | 13.9 | (2.9) | 7.0 | (0.7) | 13.5 | (1.5) | 24.7 | (3.7) |
| Drunkenness | 5.7 | (0.5) | 13.2 | (1.3) | 29.4 | (3.8) | 31.3 | (1.4) | 42.8 | (2.2) | 61.2 | (4.2) |
| Non‐use of seatbelts | 9.4 | (0.6) | 13.6 | (1.3) | 29.1 | (3.8) | 13.4 | (1.0) | 18.8 | (1.7) | 27.6 | (3.9) |
| Cannabis use | – | – | – | 21.6 | (1.2) | 36.7 | (2.2) | 56.1 | (4.3) | |||
| Other drug use | – | – | – | 5.4 | (0.6) | 12.3 | (1.5) | 23.0 | (3.6) | |||
| Non‐use of condoms | – | – | – | 4.5 | (0.6) | 7.9 | (1.2) | 17.5 | (3.3) | |||
| School | (n = 2381) | (n = 1578) | (n = 697) | (n = 1033) | (n = 699) | (n = 272) | ||||||
| Multiple risk behavior | 2.0 | (0.3) | 4.6 | (0.6) | 12.5 | (1.5) | 9.1 | (1.0) | 15.0 | (1.6) | 28.8 | (3.2) |
| Smoking | 1.2 | (0.2) | 2.6 | (0.4) | 5.9 | (1.0) | 5.4 | (0.8) | 10.9 | (1.4) | 23.2 | (3.0) |
| Drunkenness | 4.2 | (0.4) | 9.1 | (0.8) | 18.3 | (1.7) | 29.9 | (1.7) | 39.4 | (2.2) | 53.3 | (3.6) |
| Non‐use of seatbelts | 7.4 | (0.6) | 11.8 | (0.9) | 20.2 | (1.8) | 11.6 | (1.1) | 17.3 | (1.7) | 26.4 | (3.2) |
| Cannabis use | – | – | – | 21.7 | (1.5) | 31.2 | (2.1) | 43.8 | (3.6) | |||
| Other drug use | – | – | – | 4.2 | (0.7) | 8.9 | (1.2) | 21.8 | (3.0) | |||
| Non‐use of condoms | – | – | – | 4.5 | (0.7) | 6.8 | (1.1) | 11.7 | (2.3) | |||
–, HBSC items were not assessed in this age group.
Perceived climate and injury
There was mixed evidence for gradients in risk for injury in association with the perceived levels of climatic support at home and at school (table 2; and online table B at http://www.injuryprevention.com/supplemental). In the younger grades, in both settings there were modest gradients in risk for the different types of injury by perceived level of climatic support. In the older grades, there was no consistent evidence for these gradients.
Table 2 Prevalence of injury among students in grades 6–10, stratified by perceived climate at home and school.
| Setting: injury type | Prevalence of injury, by perceived climate (prevalence; % (SE)) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Grades 6–8 | Grades 9–10 | |||||||||||
| High support | Medium support | Low support | High support | Medium support | Low support | |||||||
| Home | (n = 3276) | (n = 904) | (n = 199) | (n = 1506) | (n = 685) | (n = 187) | ||||||
| Any medically treated | 53.0 | (1.0) | 56.5 | (1.9) | 61.8 | (4.1) | 55.8 | (1.5) | 53.0 | (2.2) | 50.3 | (4.3) |
| Hospitalized | 3.6 | (0.3) | 3.6 | (0.7) | 7.5 | (2.2) | 3.1 | (0.5) | 2.2 | (0.6) | 7.5 | (2.3) |
| Home | 13.0 | (0.7) | 15.4 | (1.4) | 19.2 | (3.3) | 10.1 | (0.9) | 11.6 | (1.4) | 14.5 | (3.0) |
| School | 10.7 | (0.6) | 13.1 | (1.3) | 11.9 | (2.7) | 10.5 | (0.9) | 11.0 | (1.4) | 9.8 | (2.6) |
| School | (n = 2443) | (n = 1600) | (n = 708) | (n = 1143) | (n = 828) | (n = 384) | ||||||
| Any medically treated | 52.1 | (1.2) | 53.9 | (1.4) | 61.0 | (2.1) | 54.3 | (1.7) | 52.7 | (2.0) | 58.9 | (3.0) |
| Hospitalized | 3.4 | (0.4) | 3.5 | (0.5) | 5.6 | (1.0) | 2.6 | (0.5) | 3.0 | (0.7) | 4.9 | (1.3) |
| Home | 12.9 | (0.8) | 14.0 | (1.0) | 15.8 | (1.6) | 9.9 | (1.0) | 10.6 | (1.2) | 13.6 | (2.0) |
| School | 9.9 | (0.7) | 11.3 | (0.9) | 14.7 | (1.5) | 10.3 | (1.0) | 9.9 | (1.2) | 13.9 | (2.1) |
Perceived climate as a modifier of associations between risk behavior and injury
In table 3, we present results describing the application of the Population Health Framework1 to the study of interactions between multiple risk behavior, home and school climate, and the occurrence of injury. This addressed the hypothesis that high perceived levels of climatic support would attenuate associations between risk behavior and the occurrence of injury. There was little evidence in support of this hypothesis. For outcomes of medically treated injury, home injury, and school injury there was no clear pattern in the strength and direction of any gradients in risk observed across perceived levels of climatic support. When the product terms of the multiple risk behavior scale with each of the home and school climate scales were included in logistic regression models, there was minimal evidence of statistically significant (p<0.05) effect modification of the associations between risk behavior and injury (note: this result was also found for the interaction term that was created using categorical versions of the multiple risk behavior and social climate scales).
Table 3 Associations between multiple risk behavior and injury among students in grades 6–10, stratified by perceived climate at home and school.
| Setting: injury type | Perceived climate | Relative odds of injury by frequency of risk taking (adjusted OR* (95% CI)) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Grades 6–8 | Grades 9–10 | ||||||||||||
| None | Occasional | Frequent | p Value‡ | None | Occasional | Frequent | p Value‡ | ||||||
| Home | |||||||||||||
| Medically treated | High support | 1.00 | 1.57 | (1.31–1.88) | 2.69 | (1.56–4.64) | 0.14 | 1.00 | 1.79 | (1.36–2.36) | 1.81 | (1.12–2.93) | 0.72 |
| Medium/low support | 1.00 | 1.80 | (1.30–2.50) | 1.84 | (1.07–3.17) | 1.00 | 1.49 | (0.97–2.31) | 2.90 | (1.70–4.93) | |||
| Home | High support | 1.00 | 1.57 | (1.20–2.05) | 2.07 | (1.07–3.99) | 0.09 | 1.00 | 1.24 | (0.78–1.96) | 1.41 | (0.68–2.95) | 0.32 |
| Medium/low support | 1.00 | 1.56 | (0.98–2.46) | 1.46 | (0.70–3.06) | 1.00 | 1.43 | (0.66–3.09) | 2.97 | (1.31–6.75) | |||
| School | High support | 1.00 | 1.07 | (0.79–1.44) | † | 0.49 | 1.00 | 1.28 | (0.81–2.02) | 1.08 | (0.49–2.38) | 0.68 | |
| Medium/low support | 1.00 | 1.04 | (0.64–1.70) | † | 1.00 | 1.28 | (0.61–2.69) | 1.29 | (0.54–3.08) | ||||
| School | |||||||||||||
| Medically treated | High support | 1.00 | 1.66 | (1.32–2.08) | † | 0.03 | 1.00 | 1.92 | (1.41–2.61) | 1.84 | (1.06–3.17) | 0.24 | |
| Medium/low support | 1.00 | 1.61 | (1.29–2.01) | 1.85 | (1.21–2.84) | 1.00 | 1.38 | (0.98–1.95) | 2.45 | (1.56–3.85) | |||
| Home | High support | 1.00 | 1.81 | (1.31–2.51) | † | 0.16 | 1.00 | 1.28 | (0.75–2.17) | 1.02 | (0.40–2.60) | 0.01 | |
| Medium/low support | 1.00 | 1.41 | (1.03–1.95) | 1.60 | (0.91–2.82) | 1.00 | 1.17 | (0.65–2.11) | 2.63 | (1.37–5.06) | |||
| School | High support | 1.00 | 1.00 | (0.67–1.47) | † | 0.71 | 1.00 | 1.40 | (0.83–2.36) | 1.06 | (0.41–2.75) | 0.82 | |
| Medium/low support | 1.00 | 1.11 | (0.79–1.55) | 0.76 | (0.37–1.55) | 1.00 | 1.23 | (0.69–2.18) | 1.28 | (0.62–2.62) | |||
*Adjusted for sex, amount of physical activity, two dimensions of socioeconomic status.
†Suppressed due to small cell sizes.
‡Test for interactive effect between multiple risk behavior and climate (both measured continuously) on risk for injury outcome.
Discussion
This paper presents a novel analysis of the etiology of adolescent injury. In addition to reaffirming the prevalence of overt risk taking in the lives of young people, the findings indicate the importance of contextual settings as possible determinants of health. It is not surprising that the nature of a child's home or school environment will have a direct bearing on the frequency of engagement in risk taking behaviors. A supportive environment at home or at school may sometimes result in amelioration of adolescents' risks for various types of injury. The novel finding of this study is that relationships between adolescent risk taking and injury do not appear to be modified by the presence of a supportive environment. Indeed, if a child chooses to engage in multiple risk behavior, increases in risk for injury appear to occur independent of the support received at home or at school.
Our results indicate the presence of gradients in risk for injury; one indication of the potential for adolescent health inequalities. Non‐supportive environments are associated with adverse health outcomes. Such inequalities in health are a known priority for the pediatric research agenda.20 The methodology employed in our etiological analysis is considered to be novel. The statistical modeling was grounded in an accepted theoretical framework.1 To our knowledge, this study represents one of the first such analyses to examine individual risk factors for adolescent injury while simultaneously examining the roles of settings (contextual risks) as injury determinants. Preliminary analyses3,4,5 and existing social theory21 led us to believe that statistical gradients between risk taking and injury would exist, but be attenuated in protective settings. This hypothesis was not supported by our findings. This suggests a need to consider both environmental strategies to prevent adolescent injuries, as well as preventive strategies that focus on at‐risk children.
A recent systematic review synthesized the available empirical evidence surrounding risk taking behavior in the etiology of injury. Turner et al22 identified 33 potentially eligible studies with only seven meeting a priori selection criteria. Most excluded studies were of poor methodological quality or were in the form of theoretical commentaries. Risk taking behavior, however it was measured, was associated with an increased chance of sustaining an unintentional injury except in the case of high skilled sports where the effect may be in the other direction. However, the review demonstrated that considerable work needs to be done to provide a convincing evidence base on which to build public health interventions around risk behavior.22 None of the included studies focused on youth—risk taking was examined mainly in the form of individual behaviors as opposed to behavior/environment interactions, and most studies were devoid of a theoretical base. To inform prevention efforts, there is a need for additional analyses like ours that use a well defined construct of risk behavior, are based in theory, and focus on specific populations such as adolescents.
Our findings suggest that a direct link exists between the social environments that adolescents find themselves in, the risk taking behaviors that they engage in, and at least some patterns of injury. Some environments are notably protective. In our study, home climates that are notably protective are those where the child feels trusted, understood, and valued. Protective school climates are those where students feel safe, they possess a sense of belonging, and school rules are perceived to be fair. While it would be naïve to assume that simple solutions exist that would prevent risk taking and injury in every social context, optimization of social environments remains a laudable goal that may form the basis of efficacious risk reduction strategies. Enhancing the quality of these environments will serve as a protective measure with respect to injury.23
While optimization of social environments may lead to reductions in risk taking, if a child chooses to engage in a risk taking lifestyle then the natures of social climates appear to have little influence on resultant associations with injury. This suggests a need to intervene directly with these high risk adolescents, as opposed to just modifying the social environment around them.
Strengths of this analysis warrant recognition. These include the size and scope of our analysis, our use of standard measures and survey procedures, our application of a theoretical framework to our etiological modeling, and the anonymous nature of reporting. The latter should promote accuracy in responses. Patterns of injury reported to the HBSC have been shown to be representative of adolescent injuries treated in Canadian emergency departments,24 and our results are likely generalizable to Canada and other countries with similar cultures and access to medical care. We also made efforts to minimize the possibility of confounding. To illustrate, the observed social gradients in risk for injury likely exist independently of socioeconomic explanations that are prominent in the literature.6,17 Two dimensions of socioeconomic status were included as potential confounders in all logistic regression models and their inclusion had little influence on the main effects of the associations under study.
Limitations of this analysis include our use of self‐reported data and the cross sectional nature of the survey. When compared with medical records, adolescent recall of injury events is excellent for three months but less accurate for longer recall times, with the exception of major traumatic events.25 Such errors in recall are likely to occur randomly and hence bias risk estimates towards no effect. The cross sectional design limits our ability to infer causal relationships and our analyses must be viewed as exploratory in the absence of longitudinal data. The HBSC questionnaire items have been subjected to extensive piloting and validation efforts, yet the possibility of biased reporting of health risk behaviors motivated by a desire to provide socially desirable responses must also be recognized. Because these findings are based upon classroom samples, they will not be representative of adolescents in non‐classroom settings. Finally, there was lower participation in the survey in the older grades; however, there is no reason to suspect that this differential participation introduced any selection bias.
Key points
Adolescent risk taking behavior has been determined as a leading determinant of injury.
Supportive social climates can minimize adolescent engagement in risk taking behavior.
If a child chooses to engage in a risktaking lifestyle, the presence of a protective home or school setting does not appear to influence the association with injury.
This suggest a need to intervene directly with high risk youth.
There is a need to further build an evidence base for public health interventions around adolescent risk behavior.
Conclusions
Risk taking is common among adolescents and plays a role in the etiology of injury. Supportive social climates clearly protect adolescents from engaging in these behaviors and also the occurrence of some forms of injury. Optimization of social environments has great potential as a primary prevention strategy, and is in fact a lead recommendation for both injury and violence prevention from the US Centers for Disease Control and Prevention.23 However, relationships between adolescent risk taking and injury do not appear to be modified by the presence of a supportive climate at home or in school. Beyond environmental intervention, this suggests an additional need for targeted injury prevention strategies that centre upon high risk youth who engaged in multiple risk behaviour.
Acknowledgements
This study was supported financially, in part, by research agreements with the Canadian Institutes of Health Research (Operating Grant: 2004MOP‐CHI‐128223‐C) and the Public Health Agency of Canada (Contract: HT089‐05205/001/SS) which funds the Canadian version of the Health Behaviour in School‐Aged Children Survey; a World Health Organization/European Region collaborative study. The theory behind this analysis was influenced by the conceptual thinking of colleagues Parminder Raina (McMaster University), Colin Macarthur (Hospital for Sick Children), and Barbara Morrongiello (University of Guelph) and the IPALS (Injury Prevention Across the Lifespan) initiative.
Abbreviations
HBSC - Health Behaviour in School Aged Children Survey
RMSEA - root mean square error of approximation
Footnotes
Competing interests: none.
References
- 1.Health Canada Strategies for Population Health: Investing in the Health of Canadians. Ottawa, ON: Health Canada, Minister of Supply and Services Canada, 1994
- 2.Galambos N L, Tilton‐Weaver L C. Multiple‐risk behavior in adolescents and young adults. Health Rep 1998109–20. [PubMed] [Google Scholar]
- 3.Pickett W, Garner M J, Boyce W F.et al Gradients in risk for youth injury associated with multiple‐risk behaviors: a study of 11,329 Canadian adolescents. Soc Sci Med 2002551055–1068. [DOI] [PubMed] [Google Scholar]
- 4.Koven R, McColl M A, Ellis P.et al Multiple risk behaviour and its association with head and neck injuries: a national analysis of young Canadians. Prev Med 200541240–246. [DOI] [PubMed] [Google Scholar]
- 5.Pickett W, Schmid H, Boyce W F.et al Multiple risk behaviours and injury: an international study of youth in 12 countries. Arch Pediatr Adolesc Med 2002156886–893. [DOI] [PubMed] [Google Scholar]
- 6.Peteridou E, Zavitsanos X, Dessypris N.et al Adolescents in high‐risk trajectory: clustering of risky behavior and the origins of socioeconomic health differentials. Prev Med 199726215–219. [DOI] [PubMed] [Google Scholar]
- 7.Steinberg L. Risk taking in adolescence: what changes, and why? Ann NY Acad Sci 2004102151–58. [DOI] [PubMed] [Google Scholar]
- 8.Black D, Morris J, Smith C.et alInequalities in health: The Black Report. Markham: Penguin Books, 1982
- 9.Bahr S J, Hoffmann J P, Yang X. Parental and peer influences on the risk of adolescent drug use. J Prim Prev 2005151–23Epub. [DOI] [PubMed] [Google Scholar]
- 10.Kasen S, Cohen P, Brook J S. Adolescent school experiences and dropout, adolescent pregnancy, and young adult deviant behavior. J Adolesc Res 19981349–72. [DOI] [PubMed] [Google Scholar]
- 11.In: Currie C E, Roberts C, Morgan A. (eds) et alYoung People's Health in Context: international report from the HBSC 2001/02 survey. WHO Policy Series: Health policy for children and adolescents Issue 4, WHO Regional Office for Europe, Copenhagen, 2004
- 12.In: Currie C, Samdal O, Boyce W. (eds) et alHealth Behaviour in School‐aged Children: a WHO Cross‐National Study. Research Protocol for the 2001/2002 Survey. Edinburgh, UK: University of Edinburgh, Child and Adolescent Health Research Unit, 2001
- 13.Nutbeam D, Smith C, Moore L.et al Warning! Schools can damage your health: alienation from school and its impact on health behaviour. J Paediatr Child Health 199329(Suppl 1)S25–S30. [DOI] [PubMed] [Google Scholar]
- 14.Toorsheim T, Wold B, Samdal O. The Teacher and Classmate support scale: factor structure, test‐retest reliability and validity in samples of 13‐ and 15 year old adolescents. Sch Psychol Int 200021195–212. [Google Scholar]
- 15.Prochaska J J, Sallis J F, Long B. A physical activity screening measure for use with adolescents in primary care. Arch Pediatr Adolesc Med 2001155554–559. [DOI] [PubMed] [Google Scholar]
- 16.Currie C. Socioeconomic circumstances among school‐aged children in Europe and North America. In: Vleminckx K, Smeeding RM, eds. Child well‐being, child poverty and child policy in modern nations. Bristol: Policy Press, 2001347–364.
- 17.Simpson K, Janssen I, Craig W M.et al Multilevel analysis of associations between socioeconomic status and injury among Canadian adolescents. J Epidemiol Community Health 2005591072–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothman K J, Greenland S.Modern epidemiolgy. 2nd Edition. New York: Lippincott, Williams and Wilkins, 1998
- 19.Boyce W, King M. Introduction. In: Boyce W. Young people in Canada: their health and well‐being. Ottawa: Health Canada, 20041–7.
- 20.Canadian Institutes of Health Research Reducing Health Disparities & Promoting Equity for Vulnerable Populations. Available at http://www.cihr‐irsc.gc.ca/e/15986.html#a (accessed October 2005)
- 21.Jessor R. Risk behavior in adolescence: a psychological framework for understanding and action. J Adolesc Health 199112597–605. [DOI] [PubMed] [Google Scholar]
- 22.Turner C, McClure R, Pirozzo S. Injury and risk‐taking behavior—a systematic review. Accid Anal Prev 20043693–101. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention School health guidelines to prevent unintentional injuries and violence. MMWR Recomm Rep 2001501–73. [PubMed] [Google Scholar]
- 24.Pickett W, Brison R J, Mackenzie S G.et al Youth injury data in the Canadian Hospitals Injury Reporting and Prevention Program: do they represent the Canadian experience? Inj Prev 200069–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harel Y, Overpeck M D, Jones D H.et al The effects of recall on estimating nonfatal injury rates for children and adolescents. Am J Public Health 199484599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]