Abstract
Background
Shortage of donor organs is one of the major problems for liver transplant programmes. Living liver donation is a possible alternative, which could increase the amount of donor organs available in the short term.
Objective
To assess the attitude towards living organ donation in the general population to have an overview of the overall attitude within Germany.
Methods
A representative quota of people was evaluated by a mail questionnaire (n = 250). This questionnaire had 24 questions assessing the willingness to be a living liver donor for different potential recipients. Factors for and against living liver donation were assessed.
Results
Donating a part of the liver was almost as accepted as donating a kidney. The readiness to donate was highest when participants were asked to donate for children. In an urgent life‐threatening situation the will to donate was especially high, whereas it was lower in the case of recipient substance misuse. More women than men expressed a higher disposition to donate for their children. Sex, religion, state of health and age of the donor, however, did not influence other questions on the readiness to consider living organ donation. The will for postmortem organ donation positively correlated with the will to be a living organ donor.
Conclusions
The motivation in different demographic subgroups to participate in living liver transplantation is described. Differences in donation readiness resulting from the situation of every donor and recipient are thoroughly outlined. The acceptance for a living liver donation was found to be high – and comparable to that of living kidney donation.
The shortage of donor organs is one of the key problems in solid organ transplantation. Many patients with clear indications for transplantation have to wait for several months (lung, heart or liver) or even years (kidney) in a declining state of health and with a decreasing quality of life.1 In some cases, patients requiring transplant die while on the waiting lists. To overcome the gap between organs needed for transplantation and those available, various strategies have been considered.
The first studies on xenotransplantation were started in the 1960s using non‐human primates, pigs and other animals as potential donor. Although some of the immunological and infectious obstacles have been overcome during the past two decades, xenotransplantation is still far from being introduced into clinical practice.2 Replacing organ function by artificial devices is a standard procedure in cases of progressive kidney failure. Although long‐term dialysis can keep patients alive with an acceptable state of health, kidney transplantation is considered to be the better alternative in most cases, increasing the patients' life standard and decreasing the overall sociomedical costs.3,4 Distinct methods of replacing other organs with substitution devices, with or without the use of living cells (eg, intracorporal heart pumps or bioartifical liver reactors) may be of additional use in the future. The first preclinical trials utilising these techniques have been initiated; the broad application of such methods, however, cannot be predicted. In addition, promising approaches for using stem‐cell‐based treatments have been described recently. Some of the new stem cell techniques may have the potential to solve the problem of organ shortage in the future. Today, their clinical application is still far away.
In contrast, living organ donation can be immediately applied to compensate for the lack of donor organs without major technical problems. The first experiences with transplantation of parts of the liver were made in the early 1980s (mostly with children as recipients).5 In the late 1980s and 1990s, split liver transplantation was developed, offering the possibility to treat two recipients with only one cadaveric organ graft.6 Later, reduced size liver transplantation and split techniques formed the basis on which living related liver transplantation was introduced. The first reports of living related liver transplantation were published in the late 1980s and 1990s.7,8 Living related liver transplantation as a widely used procedure for children and adults has been reported throughout the past decade.9 Today, recipient outcome in the hands of experienced centres is at least as good as that for cadaveric donation.10,11 A certain risk for the organ donor, however, remains. Living liver donation has a donor mortality of approximately 0.2–0.6% for right liver lobe donation and less than 0.1% for left lateral lobe donation (estimated by reported donor deaths) and is associated with some typical complications, mostly affecting the biliary system.12,13 This leads to considerable ethical problems for all who are associated with the process, including the donor, the recipient and the transplant team.14,15,16
This study focused on the overall motivation to become a living liver donor among the general population in Germany. Two hundred and fifty citizens, who were not directly linked to a situation of organ transplantation, were asked for their attitude towards living organ donation. Here, we detail the social circumstances and demographic factors that result in changes of the donation readiness, thereby providing important data that will allow improved communication between potential donors and their transplant centres.
Methods
Participants and the questionnaire
The questionnaire used in this study had 24 questions. The following demographic items were assessed: age of participant, sex, marital status, current state of health, education, religion, willing to be a postmortal organ donor and possession of an organ donor card. Three sections of scored questions were evaluated separately, discussing the following subitems: donation for children, for partners or spouses and for parents. For each item the same following questions were asked: will to donate in different circumstances and arguments for and against living liver donation. For each of these items several questions were asked, which could be scored on a 5‐point scale. Subgroups were formed according to demographic variables, to assess whether different parameters—for example, religion and employment status, influenced donation readiness.
We included 250 people in the study. Participants were selected and questioned using a mail questionnaire. A professional institute for media research (TNS Infratest, Munich, Germany) carried out the data acquisition. The participants were randomly chosen from a database of people who generally agreed to participate in surveys. The composition of the quota was chosen representatively to reflect the distribution of sex, age and residence among the German population. The total return rate of questionnaires was 70%.
Computation and statistical analysis
Answers were coded in nominal (sociodemographic questions) or ordinal (scored questions) manner and introduced into a SPSS system file (SPSS V.12.0 for Windows). Means of scored questions were compared using a one‐way multivariate analysis between all groups (H0: μ1 = μ2 = μ3 = μ4) and by Student's t test for independent univariate analysis between all possible pairs of groups (H0: μ1 = μ2, μ1 = μ3, …). Pearson's χ2 test for cross‐table analysis was used to compare nominal coded data and demographic items.
Sociodemographic distribution of the participants
The mean age of the participants was 45 (SD 14) years; 53.2% of the participants were women, indicating a balanced distribution of the participants with regard to age and sex. About the self‐assessed state of health, most of the participants felt very good or good (70.4% together). The participants were married in 40% of cases, whereas 38.8% were unmarried. In all, 15.6% of the participants were divorced and 5.6% were widowed. Most of the participants were Christians (65.2%); 33.2% did not belong to any religion. Of the participants, 46.8% had received a higher education (diploma from a German secondary school qualifying for admission to university). Among the participants, 49% worked full time, 13.2% worked part time, 8.6% were students and 29.2% were jobless.
Results
General readiness for live and postmortal organ donation and acceptance
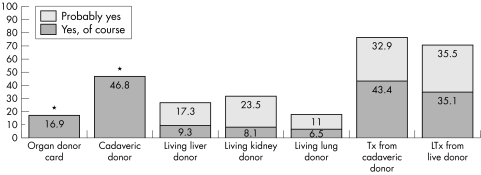
When asked for their motivation for postmortal organ donation, 46.8% of the participants stated that they would donate their organs, whereas 14.0% would not donate an organ (39.2% were undecided). In contrast with this, only 16.9% of the interviewed population stated that they possess a donor card. The basic question of the readiness to be a live donor was discussed in a general fashion (“Generally speaking, would you be willing to be a live donor for parts of the liver, one kidney or parts of the lung?”). Of the participants, 26.6% were willing to donate a part of their liver with a high or medium likelihood (31.6% one kidney, 17.5% part of their lung; fig 1). Of the participants, however, 13.3% would never give away a part of the liver, 13% and 19.9% would never donate a kidney and a part of the lung, respectively. Most participants stated, they needed several days' consideration time to decide whether to donate. Here, men needed significantly (Pearson's χ2, p<0.05) more time than women to come to a decision. On assessing the general donation readiness, however, we observed no differences when comparing men and women. Subdividing the general population of the participants as below and over 45 years resulted in no difference in the donation readiness between older and younger donors. Those who were willing to donate organs after death were significantly more likely to agree to donation of living liver, kidney and lung (Pearson's χ2, p<0.05). The participants in a stable relationship were more willing to donate a part of their liver than those living singly (Pearson's χ2, p<0.05).
Figure 1 General readiness for living organ donation and postmortal organ donation and acceptance. The participants were asked if they possess a valid organ donor card (bar 1) and whether they would donate after death (bar 2). The participants were then asked if they could generally imagine being a living organ donor for several organs (bars 3–5). The willingness to accept a cadaveric organ and a live liver donation are depicted in bars 6 and 7. Possible answers for bars 3–7 were “yes, of course”, “probably yes”, “undecided”, “probably no” and “absolutely not”. Numbers in the bars indicate the percentage of participants stating “yes, of course” and “probably yes”, respectively. *The answer “probably yes” was not possible for these questions.
Of the participants assessed, 35.1% would generally accept an organ from a live donor; in an urgent life‐threatening situation this fraction increased to 56.6%, whereas 3.2% would categorically reject a live organ and 2.8% would refuse it even in a life‐threatening situation. To shorten the time on a waiting list, 34.7% would agree to receive an organ from a live donor. If the outcome would be inferior to that of cadaveric donation, 6.6% would still consider receiving the organ—compared with 9.4% who would categorically reject the organ in that particular situation. If the donor would take a substantial risk, 2.4% would accept and 23.8% would categorically reject a living organ donation. When asked for cadaveric grafts, 43.4% would principally accept and 2.8% would categorically reject this kind of graft. The participants with a higher education would accept a graft from a brain‐dead donor significantly more often (Pearson's χ2, p<0.05).
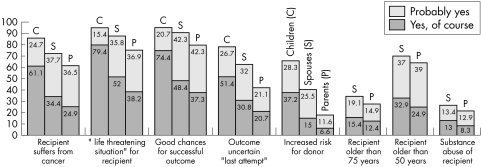
Donation for children
In a second block of questions, the participants were asked under which circumstances they would donate a part of their liver for their own children. If the disease of the child would be curable by live liver transplantation, the donation readiness was very high (80.2%). Postulating that the child had liver cancer resulted in a lower donation readiness (60.4%; fig 2), whereas the subgroup of the participants with a higher education stated significantly more often that they would donate in that case (Pearson's χ2, p<0.05). When asked for willingness to donate in case of an urgent life‐threatening situation for the recipient, values were similar (79.4%) to results obtained after postulating curable disease (80.2%) or good chances of successful outcome for the recipient (74.4%). In the cases with curable disease or good chances of successful outcome, the participants with a higher education again considered to donate an organ more often (Pearson's χ2, p<0.05). If the potential outcome of the recipient was uncertain and transplantation was performed as a last attempt, willingness to donate was significantly lower (51.4%), although not as low as if the risk of the donor was increased (37.2%). In all aspects, except in the case of increased donor risk, women were significantly more motivated than men to donate for their children.
Figure 2 Living liver donation readiness for children, for spouses or partners and for parents in different situations. Data are given for different questions, each hypothesising a defined situation. The first bar in each row shows the answers in the case of donating for children, the second for spouses or partners and the third for parents. Answers could be given on a 5‐point scale; only the positive answers “yes, of course” and “probably yes” are indicated for overview purposes. Inside the bars, percentages of stated answers are shown if >5%. The last three questions could be assessed only in the case of donating for spouses or partners and for parents.
Donation for spouses or partners and for parents
In a third block of questions, the participants were asked under which circumstances they would be willing to donate a part of their liver to their partners or spouses. Here, the willingness decreased with increase in age of the potential recipient (32.9% if the partner was >50 years compared with 15.4% if the partner was >75 years; fig 2). When it was hypothesised that the potential recipient had liver cancer, donation willingness was higher (34.4%) than when it was postulated that the recipient's addiction to drugs resulted in liver failure (13.0%). In case of an urgent life‐threatening situation, the donation readiness was high (52.0%). The same was true when hypothesising that the postoperative outcome would be good (48.4%). When postulating that the procedure would be a last attempt with an uncertain outcome, however, the motivation was markedly lower (30.8%). When asked for donations in case of increased risk for oneself (the donor), the willingness was extremely low (15.0%).
In the fourth set of questions, the participants were asked under which circumstances they could be a living liver donor for their parents. Willingness was low when the recipient's disease was caused by substance misuse (8.3%; fig 2) or when the risk for the donor was high (6.6%). Donation for younger parents (age >50 years, 24.9%) was considered to be more attractive than for recipients aged >75 years(12.4%). When subgrouping the participants, women and the participants with a higher education were significantly more willing to donate for younger parents and parents in an urgent life‐threatening situation than men and the participants with a lower degree of education, respectively (Pearson's χ2, p<0.05 for each relationship). Transplantation in case of liver cancer was accepted by 24.9% of the participants, although in case of a life‐threatening situation the willingness to donate was higher (38.2%). The participants with a full‐time job showed more motivation for donation than participants who were unemployed. Highest results were documented when the outcome after transplantation was considered to be good (46.0%). A fraction of 20.7% of the participants still considered a donation when live liver transplantation would be carried out as a last attempt with an uncertain outcome.
Factors underlying decision making
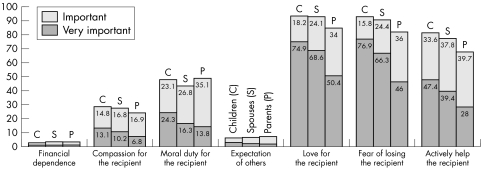
For each scenario, the participants were asked for the reasons underlying their decision. These questions were provided in two sets, one for potential arguments for (fig 3) and one for arguments against live liver donation (fig 4). Here, financial dependence was never an aspect in favour of donation. Love for the potential recipient was considered to be the most important reason of action; this was most apparent in transplantation for children, especially in the subgroup of the participants with a higher education. Women stated love as a rationale considerably more often than did men when donating a part of the liver for their parents. The fear of losing the potential recipient was another important motivation to donate. The participants with a full‐time job stated this argument significantly more often when asked for donation for parents (Pearson's χ2, p = 0.001). Compassion and the moral duty for the recipient was not rated an important feature for all potential donors, except that Christians stated compassion significantly more often as a reason to donate to children (Pearson's χ2, p<0.05). People with a higher education stated moral duty more often than those with lower education as a reason for donating part of the liver to their parents and children (Pearson's χ2, p<0.05). The expectation of others was denied being an important aspect. An important argument for living organ donation was the possibility to actively help the recipient, which was considered to be significantly more important by the participants with a higher education (Pearson's χ2, p<0.05).
Figure 3 Potential factors reasoning in favour of living liver donation. The participants were asked which factors would reason in favour of living liver donation to elucidate the motivation to donate for a certain group of recipients. Answers could be given on a 5‐point scale; only the positive answers “very important” and “important” are indicated. Inside the bars, percentages of stated answers are shown when >5%. The first bar in each row shows the answers in the case of donating for children, the second for spouses or partners and the third for parents.
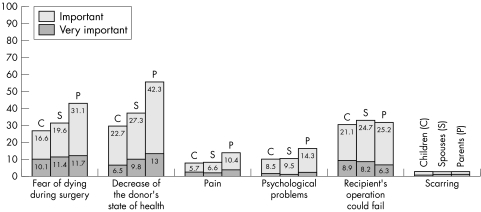
Figure 4 Potential factors reasoning against living liver donation. The participants were asked which factors reasoned against living liver donation to elucidate the motivation not to donate for a certain group of recipients. Answers could be given on a 5‐point scale; only the positive answers “very important” and “important” are shown. Inside the bars, percentages of stated answers are shown when >5%. The first bar in each row shows the answers in the case of donating for children, the second for spouses or partners and the third for parents.
Reviewing arguments against living liver donation, scarring after the operation was considered to be the aspect with least importance. The fear of dying during surgery was central to potential donors, with a lesser extent when solely Christians were assessed (Pearson's χ2, p<0.05). A decrease in the donor's state of health after the operation was another strong argument against living organ donation. Pain and psychological problems after the operation were considered to be minor problems. The fear that the recipient's operation would fail was not considered to be a strong argument against living liver donation (for all potential recipients).
Discussion
In this study we describe for the first time the attitude towards living organ donation of 250 people selected from the general German population. The study was focused on living liver donation and compared the will to be a live donor for people with different relationships to the donor. No specific educational material was handed out to the participants of the study to imitate the situation in which most potential living organ donors find themselves when confronted with living organ donation for the first time. A complex set of questions was sent to the attending people by a mail questionnaire.17,18,19 We believe that our study gives an important overview of the relevance that the personal situation and demographic background have on decision making in living organ donation. On comparing the readiness to be a live donor for varying organs, we found the overall values for kidney and liver donation to be similar, whereas potential living lung donation was rated lower. This is remarkable as the risk for donor mortality in living liver donation was estimated to be 0.2–0.6% as reported by donor deaths,20,21 whereas the risk for kidney donation is considered to be <0.1%. The nominal risk of living organ donation, however, does not seem to be the most important issue for the potential donor, which may be due to a low information level of the donors about the risks and possible complications of the procedure. About postmortal organ donation, 46.8% of our participants expressed the will to donate an organ after death. This was lower than in a Swedish survey, in which 61% of the participants asked wanted to donate after death.22
When the social relationship between live donors and recipients was analysed, donation for children was the strongest positive motivator.23 Women considered donating for children considerably more often than men, which is probably caused by the unique relationship between mothers and their infants. Donation readiness for partners or spouses as potential recipients was higher than that for parents. In living organ donation for adults, the circumstances that make the transplantation necessary also seem relevant. The age of the recipient is one key aspect and donation for a particularly old recipient was considered to be less acceptable. The same is true when the cause of the recipient's disease was considered: transplantation in case of substance misuse was rated lower than living organ donation in the case of cancer, obviously not taking into account that transplantation in case of liver cancer reveals specific problems.24,25 The outcome after a potential transplantation was important for all donors. A higher will to donate was generally expressed when the outcome was hypothesised to be good. When the outcome was described as uncertain, the will to donate was lower, although not as low as one may have expected, expressing the will to help even in case of an uncertain result. High scores were observed in an urgent life‐threatening situation. This is in basic contrast with the policy that is outlined by most of live donor programmes, which carry out liver transplantation only when careful evaluation of the recipient and donor is performed in an elective situation.26 The participants denied pain to be an argument against living liver donation, but presumably the participants underestimated the postoperative pain, as Trotter et al27 showed in their report.
The sex of the donor seemed not of particular importance when the general motivation to donate a part of the liver was assessed. This is somewhat in contrast with the fact that a majority of live liver and also kidney donors are currently women. Motivation in women, however, was greater when asked to donate for children. When subgrouping the general population, an influence of age on the overall motivation for living donation could not be outlined. The participants with a higher education were considerably more willing to donate for parents. This subgroup was also more prepared to receive an organ from a brain‐dead donor, reflecting a better status of information about the procedure of organ transplantation and its medical background. Additionally, the participants with a full‐time job were more afraid of losing a parent and would more likely donate for their parents. This may be the case because these people depend on the parents' support (eg, to care for their children). This is in contrast with the idea that employees may not be willing to donate, fearing losing their jobs due to complications. The marital status did play a part, as people in a stable relationship were considerably more willing to donate a part of their liver, but not a kidney or a part of the lung. Here, we did not distinguish between married and unmarried couples. This study shows coherence between the stated willingness for postmortal and living organ donation, pointing out that postmortal organ donors may also participate in living organ donor programmes. No relationship, however, existed between the possession of an organ donor card and the willingness to donate a live organ.
In December 2000, more than 100 members from all specialties of the Transplantation Society published their Consensus Statement on the Live Organ Donor.28 This report summarises standard procedures for donor evaluation, informed consent, as well as psychosocial and medical suitability. It was generally agreed that related and directed unrelated transplantation would be equally acceptable, when performed for altruistic reasons. The exchange of kidney donors between two recipients (paired exchange) because of immunological incompatibility was also considered to be appropriate. About donation to strangers and financial benefits, no consensus could be obtained. Several other reports discuss the problem of monetary compensation for living organ donation.29,30,31,32 A final conclusion has not yet been drawn and monetary benefit for live organ donors remains illegal in most countries.
In their report, Crouch and Elliott33 conclude that living organ donation for related family members, especially children, can never be considered to be an autonomous decision, as the family represents a social structure that does not leave its members without responsibility. Donation for own children, therefore, is always coercive. In our report highest readiness for living liver donation for own children was observed, giving further evidence to this concept. Crouch and Elliott33 conclusively point out that the type of coercion that may result from the relation of children and parents is, if at all, decreasing one's independence but not freedom. Parental donation in this situation is therefore considered to be ethically acceptable, although donor autonomy may be lost.
In the survey, care was taken to reduce potential pressure from the participants (neutral questions, anonymous telephone inquiry, 5‐point scale), because the participants generally tend to answer questions in a socially accepted way. It cannot be excluded that this bias, however, played some part in the results. Our study therefore concentrated on differences between subgroups rather than on overall values, as it can be assumed that all participants are affected by the same bias. One indicator for this potential bias is the difference between the stated will to donate after death (46.8%) and the actual possession of an organ donor card (16.9%).
Conclusions
This study showed that sex, religion, state of health and age of the donor were not major predictors for general donation readiness. Women were more willing to donate for their children in nearly every hypothesised situation. More participants were willing to receive a live organ than to donate one, reflecting the status quo in cadaveric organ transplantation. Nevertheless, live liver transplantation can provide more organs in the future, although ethical issues need to be discussed further. The general willingness for living liver donation was similar to that of living kidney donation, whereas the risks and complication rates are different. As participants tend to refuse living liver donation if an increased risk for the donor is postulated, it seems that informed consent is a key issue in living organ donation to allow potential donors to make a decision in full awareness of the consequences.
Acknowledgements
This work was financed by a generous grant by Roche Deutschland, Grenzach. It was also financed by Novartis Pharma GmbH, Nürnberg and Fujisawa Deutschland GmbH, München.
We thank all the participants for their contribution. We also thank Ms Irina Kucuk for her work on the database.
References
- 1.Wiesinger G F, Quittan M, Zimmermann K.et al Physical performance and health‐related quality of life in men on a liver transplantation waiting list. J Rehabil Med 200133260–265. [DOI] [PubMed] [Google Scholar]
- 2.Starzl T E. History of clinical transplantation. World J Surg 200024759–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keown P. Improving quality of life–the new target for transplantation. Transplantation 200172(12 Suppl)S67–S74. [PubMed] [Google Scholar]
- 4.Meier‐Kriesche H U, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation 2002741377–1381. [DOI] [PubMed] [Google Scholar]
- 5.Bismuth H, Houssin D. Reduced‐sized orthotopic liver graft in hepatic transplantation in children. Surgery 198495367–370. [PubMed] [Google Scholar]
- 6.Ringe B, Burdelski M, Rodeck B.et al Experience with partial liver transplantation in Hannover. Clin Transplant 1990135–144. [PubMed]
- 7.Broelsch C E, Whitington P F, Emond J C.et al Liver transplantation in children from living related donors. Surgical techniques and results. Ann Surg 1991214428–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raia S, Nery J R, Mies S. Liver transplantation from live donors. Lancet 19892497. [DOI] [PubMed] [Google Scholar]
- 9.Samstein B, Emond J. Liver transplants from living related donors. Annu Rev Med 200152147–160. [DOI] [PubMed] [Google Scholar]
- 10.Liu C L, Fan S T, Lo C M.et al Living‐donor liver transplantation for high‐urgency situations. Transplantation 200375(3 Suppl)S33–S36. [DOI] [PubMed] [Google Scholar]
- 11.Williams R S, Alisa A A, Karani J B.et al Adult‐to‐adult living donor liver transplant: UK experience. Eur J Gastroenterol Hepatol 2003157–14. [DOI] [PubMed] [Google Scholar]
- 12.Brown R S, Jr, Russo M W, Lai M.et al A survey of liver transplantation from living adult donors in the United States. N Engl J Med 2003348818–825. [DOI] [PubMed] [Google Scholar]
- 13.Broering D C, Wilms C, Bok P.et al Evolution of donor morbidity in living related liver transplantation: a single‐center analysis of 165 cases. Ann Surg 20042401013–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y S, Cheng Y F, De V V.et al Evaluation of living liver donors. Transplantation 200375(3 Suppl)S16–S19. [DOI] [PubMed] [Google Scholar]
- 15.De V V, Lo C M, Chen C L. Ethics and rationale of living‐donor liver transplantation in Asia. Transplantation 200375(3 Suppl)S2–S5. [DOI] [PubMed] [Google Scholar]
- 16.Russo M W, Brown R S., Jr Ethical issues in living donor liver transplantation. Curr Gastroenterol Rep 2003526–30. [DOI] [PubMed] [Google Scholar]
- 17.Boulware L E, Ratner L E, Sosa J A.et al Determinants of willingness to donate living related and cadaveric organs: identifying opportunities for intervention. Transplantation 2002731683–1691. [DOI] [PubMed] [Google Scholar]
- 18.Pascher A, Sauer I M, Walter M.et al Donor evaluation, donor risks, donor outcome, and donor quality of life in adult‐to‐adult living donor liver transplantation. Liver Transplant 20028829–837. [DOI] [PubMed] [Google Scholar]
- 19.Spital A. The ethics of unconventional living organ donation. Clin Transplant 19915322–326. [PubMed] [Google Scholar]
- 20.Brown R S, Jr, Russo M W, Lai M.et al A survey of liver transplantation from living adult donors in the United States. N Engl J Med 2003348818–825. [DOI] [PubMed] [Google Scholar]
- 21.Wiederkehr J C, Pereira J C, Ekermann M.et al Results of 132 hepatectomies for living donor liver transplantation: report of one death. Transplant Proc 2005371079–1080. [DOI] [PubMed] [Google Scholar]
- 22.Sanner M A. Giving and taking–to whom and from whom? People's attitudes toward transplantation of organs and tissue from different sources. Clin Transplant 199812530–537. [PubMed] [Google Scholar]
- 23.Biller‐Andorno N, Schauenburg H. It's only love? Some pitfalls in emotionally related organ donation. J Med Ethics 200127162–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gondolesi G, Munoz L, Matsumoto C.et al Hepatocellular carcinoma: a prime indication for living donor liver transplantation. J Gastrointest Surg 20026102–107. [DOI] [PubMed] [Google Scholar]
- 25.Mak K S, Tan K C. Liver transplantation for hepatocellular carcinoma: an Asian perspective. Asian J Surg 200225271–276. [DOI] [PubMed] [Google Scholar]
- 26.Liu C L, Fan S T, Lo C M.et al Living‐donor liver transplantation for high‐urgency situations. Transplantation. 2003 15 75(3 Suppl)S33–S36. [DOI] [PubMed] [Google Scholar]
- 27.Trotter J F, Talamantes M, McClure M.et al Right hepatic lobe donation for living donor liver transplantation: impact on donor quality of life. Liver Transplant 20017485–493. [DOI] [PubMed] [Google Scholar]
- 28.Hudson J N. Computer‐aided learning in the real world of medical education: does the quality of interaction with the computer affect student learning? Med Educ 200438887–895. [DOI] [PubMed] [Google Scholar]
- 29.Cameron J S, Hoffenberg R. The ethics of organ transplantation reconsidered: paid organ donation and the use of executed prisoners as donors. Kidney Int 199955724–732. [DOI] [PubMed] [Google Scholar]
- 30.Miller R B. Ethics of paid organ donation and the use of executed prisoners as donors: a dialectic with professors Cameron and Hoffenberg. Kidney Int 199955733–737. [DOI] [PubMed] [Google Scholar]
- 31.Schlitt H J. Paid non‐related living organ donation: horn of Plenty or Pandora's box? Lancet 2002359906–907. [DOI] [PubMed] [Google Scholar]
- 32.Soper C. Organ donation and kidney sales. Lancet 1998352484–485. [DOI] [PubMed] [Google Scholar]
- 33.Crouch R A, Elliott C. Moral agency and the family: the case of living related organ transplantation. Camb Q Healthcare Ethics 19998275–287. [DOI] [PubMed] [Google Scholar]