Abstract
Background
Tobacco will soon be the biggest cause of death worldwide, with the greatest burden being borne by low and middle‐income countries where 8/10 smokers now live.
Objective
This study aimed to quantify the direct burden of smoking for cardiovascular diseases (CVD) by calculating the population attributable fractions (PAF) for fatal ischaemic heart disease (IHD) and stroke (haemorrhagic and ischaemic) for all 38 countries in the World Health Organization Western Pacific and South East Asian regions.
Design and subjects
Sex‐specific prevalence of smoking was obtained from existing data. Estimates of the hazard ratio (HR) for IHD and stroke with smoking as an independent risk factor were obtained from the ∼600 000 adult subjects in the Asia Pacific Cohort Studies Collaboration (APCSC). HR estimates and prevalence were then used to calculate sex‐specific PAF for IHD and stroke by country.
Results
The prevalence of smoking in the 33 countries, for which relevant data could be obtained, ranged from 28–82% in males and from 1–65% in females. The fraction of IHD attributable to smoking ranged from 13–33% in males and from <1–28% in females. The percentage of haemorrhagic stroke attributable to smoking ranged from 4–12% in males and from <1–9% in females. Corresponding figures for ischaemic stroke were 11–27% in males and <1–22% in females.
Conclusions
Up to 30% of some cardiovascular fatalities can be attributed to smoking. This is likely an underestimate of the current burden of smoking on CVD, given that the smoking epidemic has developed further since many of the studies were conducted.
Keywords: attributable fraction, ischaemic heart disease, stroke, smoking, Western‐Pacific, South‐East Asia
Worldwide, the only two major causes of death whose effects are increasing rapidly are HIV and tobacco use.1 By 2030, tobacco is expected to be the single biggest cause of death worldwide, accounting for about 10 million deaths per year, more than the total number of deaths from malaria, maternal and major childhood conditions, and tuberculosis combined. This burden will be borne largely by low and middle‐income countries (LMIC) where eight out of 10 smokers now live.1 It will further increase disparities in health and wealth in LMIC, as smoking is known to be increasing in poorer countries and even more so in poorer people in poor countries.2,3
The current high prevalence of smoking and its upward trend foreshadow challenges in the future, not only for population health and health care, but also economically. In LMIC, high tobacco use exerts well known direct effects in terms of increased morbidity and mortality from cardiovascular diseases (CVD), respiratory diseases and cancer, and also indirect health effects due to the decreased ability of a household to spend money on health care, education and healthy foods because of money spent on tobacco.4 Outside of the household, the indirect health effects of tobacco are felt in reduced productivity by removing people from the workforce.2 For example, of the expected nine million deaths from CVD in China in 2030, over half will occur in the prime working ages 35–64.5
In conjunction with rising the prevalence of smoking, many LMIC are in, or entering, what has been termed the epidemiologic transition and are experiencing an increase in CVD and other non‐communicable diseases.6 This has been well documented by the World Bank's Global Burden of Disease project, and by the World Health Organization MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) project.6,7 These demonstrate that LMIC currently contribute 80% of global CVD‐related deaths and 87% of CVD‐related disability.6 Notably, of all the countries included in the MONICA project, China (Beijing) demonstrated the greatest recent increase in heart disease.7 The impact of this increase cannot be understated in the Asia‐Pacific region, estimated to contain at least 65% of the world's population.8 Of all the major and modifiable risk factors for CVD (smoking, hypertension, diabetes, hyperlipidaemia, and lack of exercise), tobacco smoking is almost certainly the most important in LMIC due to its high prevalence as well as its unarguable negative impacts on health.
To the best of our knowledge, there are no published studies of the population attributable fraction of CVD caused by smoking in the Western Pacific or South East Asian regions. However, there have been studies of the overall risk of dying due to smoking in these regions. For instance, a large retrospective study in China, the world's largest producer and consumer of tobacco, revealed that one smoker in four in that country has already been killed by tobacco.9 Another study from Hong Kong estimates that about 33% of all male deaths and about 5% of all female deaths are caused by smoking.10 The proportion of all deaths caused by smoking in the region is still currently lower than in “the West”, mainly because the full effects of the large recent increases in male smoking are not yet evident.11 Yet, even at this early stage, because of the size of its population, China has more deaths from tobacco than the United States or Russia.11
Trends
Whereas current mortality from past smoking patterns can serve as an early warning, greater concern should be directed toward the much larger number of deaths that are expected in coming decades as a result of current smoking, especially for LMIC. Unfortunately, knowing what to expect is difficult as detailed age‐ and sex‐specific trends in smoking by country in the WHO Western Pacific and South East Asian regions are not consistently available. However, it is known that overall tobacco consumption increased in all LMIC in the past two decades by about 3.4% per year, compared with declines in consumption in high‐income countries.5 In selected countries in the Western Pacific and South East Asian regions, percentage increases in per capita cigarette consumption over the period 1970–1990 range from 30% for Thailand and Cambodia to more than 130% for Nepal, China and Indonesia.5 For example, the average consumption of cigarettes per Chinese man per day was 1 in 1952, 4 in 1972, 10 in 1992, and 11 in 1996.5 Cases of CVD are increasing simultaneously, with anticipated increases of 120% for women and 137% for men in LMIC between 1990 and 2020, compared with age‐related increases of between 30–60% in high‐income countries.2 These are conservative estimates, as they do not take into account the likely increase in the prevalence of other CVD risk factors over time.
Rationale
This paper addresses a major area of uncertainty, as indicated by the World Bank Report on Smoking, the lack of knowledge regarding the burden of tobacco‐attributable disease, as well as estimates for the prevalence and impact of smoking on women in LMIC.5 It quantifies the direct burden of smoking for cardiovascular diseases (CVD) by calculating the population attributable fractions (PAFs) for ischaemic heart disease (IHD) and stroke (haemorrhagic and ischaemic) for countries in the WHO Western Pacific and South‐East Asian regions. The PAF provides estimates of the proportion of heart disease and stroke cases in a country that could be avoided if smoking were eliminated.
METHODS AND POPULATIONS
Calculation of the PAFs required estimates of the prevalence of smoking by country, as well as estimates of hazard ratio (HR) for CVD associated with smoking.
Prevalence of smoking
Data on the prevalence of smoking for adult males and females were obtained for countries in the WHO Western Pacific and South‐East Asian regions. Although the WHO does not recognise them as separate countries, Hong Kong, Macau and Taiwan were considered separately from China because these regions have unique health, political and administrative bodies that may influence the prevalence of smoking. Data on prevalence were obtained from studies compiled by the WHO and supplemented by data from national surveys, available either through Medline or via national government or non‐governmental organisation websites. These other surveys were used only if they provided more recent data or where the WHO did not have sex‐specific data on smoking for a particular country. Only those studies compiled by the WHO and judged by the WHO to be “methodologically sound and to provide reasonable reliable and comparable results”, or those national surveys that used random sampling techniques to obtain representative population estimates from countries in the WHO Western Pacific and South‐East Asian regions, were used to obtain estimates of the prevalence of smoking.9
Relative risk of cardiovascular disease
Age‐adjusted estimates of the relative risk of smoking for cardiovascular death were obtained from the Asia Pacific Cohort Studies Collaboration (APCSC). The APCSC is an overview of cohort studies in the region. Details on the APCSC, including study identification, data collection, and event verification are described elsewhere.12 All studies included in APCSC were conducted prospectively in populations from the Asia‐Pacific region, had at least 5000 person years of follow‐up and recorded age, sex, and blood pressure at baseline and vital status at the end of the follow‐up. Studies were excluded from the APCSC if entry was dependent upon the individual having a particular condition or risk factor.
All data on current cigarette smoking (yes/no) were self‐reported at enrolment. Cardiovascular deaths were ascertained using monitoring, re‐surveying and/or record linkage, and classified according to the ninth revision of the International Classification of Diseases (ICD): IHD (ICD 410–414); stroke (430–438); haemorrhagic stroke (431.0–432.9); ischaemic stroke (433.0–434.9). Deaths were ascribed solely to their underlying cause. Analyses used individual participant data, and were restricted to individuals aged 20 years and over at the time of the baseline survey for whom smoking status was recorded.
Population attributable fraction
Using the estimates of prevalence obtained from the literature and the HR from APCSC, population attributable fractions (%) for fatal ischaemic heart disease, haemorrhagic and ischaemic stroke caused by smoking were calculated for each country, for both males and females, using the formula: PAF = [100 × prevalence × (HR−1)]/[100 + prevalence × (HR−1)], where prevalence is in %.
RESULTS
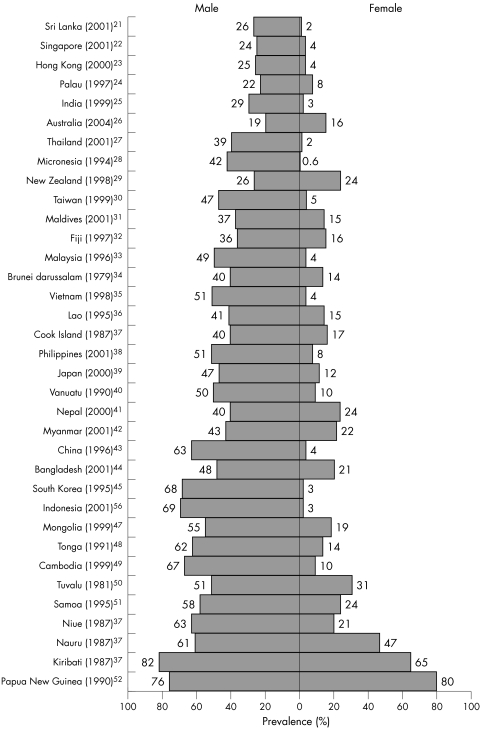
Nationally representative data on the sex‐specific prevalence of smoking were available for all 27 countries in the WHO Western Pacific Region except for the Marshall Islands and the Solomon Islands; and for all 11 countries in the WHO South‐East Asia Region except for Bhutan, North Korea and Timor‐Leste. Also, no data were available for Macau. For the Solomon Islands and Timor‐Leste, data were available only for female smoking prevalence, 33% and 1.1%, respectively, and the total prevalence of smoking (males and females) in Bhutan is reported to be 1%.13,14,15 The prevalence of smoking in the other 33 countries in the WHO Western Pacific and South‐East Asian regions (plus Hong Kong and Taiwan) ranged from 28–82% in males and from 1–65% in females (fig 1).
Figure 1 Prevalence of smoking in the Western Pacific and South East Asian Regions by sex.21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52
A previous individual participant data analysis of the 40 cohort studies from APCSC provided estimates of HR for CVD.16 In APCSC there are no significant differences (p > 0.05) in the relative effect of smoking on IHD or stroke between countries, between Asia and Australia/New Zealand (ANZ) or between women and men. The HRs (95% confidence intervals (CI)) comparing current smokers with non‐smokers are: 1.60 (95% CI 1.49 to 1.72) for ischaemic heart disease; 1.19 (95% CI 1.06 to 1.33) for haemorrhagic stroke; and 1.38 (95% CI 1.24 to 1.54) for ischaemic stroke.
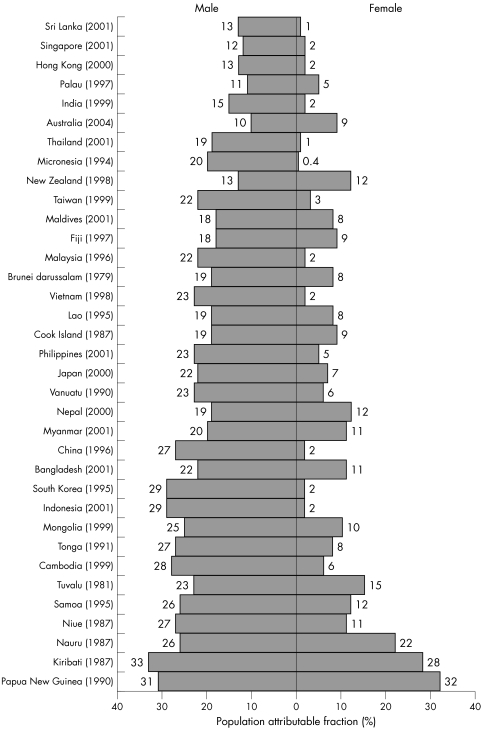
Figures 2–4 present the population attributable fractions for males and females for IHD, haemorrhagic and ischaemic stroke caused by smoking for each country in the WHO Western Pacific and South‐East Asian regions. Countries are ranked by the total prevalence of smoking in fig 1 and this ranking remains for figs 2–4. The fraction of IHD attributable to smoking ranged from 13–33% in males and from <1–28% in females (fig 2). The fraction of haemorrhagic stroke attributable to smoking ranged from 4–12% in males and from <1–9% in females (fig 3). The fraction of ischaemic stroke attributable to smoking ranged from 11–27% in males and from <1–22% in females (fig 4).
Figure 2 Population attributable fraction (%) of heart disease caused by smoking.
Figure 3 Population attributable fraction (%) of haemorrhagic stroke caused by smoking.
Figure 4 Population attributable fraction (%) of ischaemic stroke caused by smoking.
DISCUSSION
We have quantified the direct burden of smoking on cardiovascular diseases (CVD) in the WHO Western Pacific and South East Asian regions by calculating the PAFs for IHD and stroke. Results from this study suggest that up to ∼30% of fatal CVD in these populations can be attributed to smoking, depending on the outcome of interest. Much of the projected increase in mortality over the next 50 years could be avoided if adults quit smoking; however, quitting remains rare in LMIC.5
Interestingly, this study demonstrated that Australia and New Zealand, the two higher‐income countries in the WHO Western Pacific and South‐East Asian regions, with predominantly white populations, have relatively low smoking prevalence and therefore low PAFs for CVD. As expected, the attributable fractions for all outcomes are greater for males because their prevalence of smoking is currently higher. PAFs for CVD in women will almost certainly increase in the future because smoking by women in LMIC in these regions is expected to increase in the coming years.2 The attributable fractions for CVD for Australia and New Zealand from this study are similar to estimates previously published by Peto et al in their monograph providing PAFs for various outcomes caused by smoking in developed countries.17 However, the methods used here are more direct and robust.
While this paper addresses only the PAF for heart disease and stroke associated with smoking, not only is the prevalence of smoking increasing in the Western Pacific and South East Asian regions, but the countries in these regions are also experiencing increases in other risk factors for CVD, including overweight/obesity, diabetes, hypertension and dyslipidaemia.18 Ominously, these trends are likely to work together, further amplifying observed death and disability from IHD and stroke.
Strengths and limitations
This study has the strength of being able to calculate PAFs using HRs from the region based on the largest‐ever study of CVD in the Asia‐Pacific, and one of the largest anywhere in the world. The size of the APCSC means that the overall estimates of the relative effects of smoking are more precise than those employed in most previous calculations and offer an improvement over previous indirect methods for estimation.
However, the APCSC does have a number of disadvantages, particularly with respect to the assessment of smoking. First, this study needed to define smoking as a simple self‐reported, dichotomous variable (yes/no) reflecting status at baseline, since few variables on smoking habits are included in the Collaboration. Thus PAFs could not be calculated using duration of smoking, although duration is recognised as more important than daily consumption of cigarettes in determining the effects of smoking on some health outcomes such as cancer.16 However, the relative importance of duration versus daily consumption smoking measures is less clear for cardiovascular outcomes.19 If the measurement of the duration of smoking is important for CVD, as it is for cancer, then the inclusion of ex‐smokers in the reference group will have led to an underestimation of the RRs associated with current versus never smoking and a concomitant underestimation of PAFs.
A second limitation is that no objective measures of smoking status were available in the APCSC database, nor in studies used to estimate the prevalence of smoking. Any misclassification of current smokers as former or never‐smokers will have served to underestimate the HRs and hence the PAFs.
A third limitation is that, although there were no statistically significant differences in APCSC between countries in HR, for IHD or stroke, the same measure of HR has been used to calculate the PAFs for countries not represented in APCSC (for example, India). A fourth limitation is that although the estimates of risk were adjusted for age, data on prevalence of smoking were not. A final limitation is that the individual studies included in the APCSC used different methods to verify CVD outcomes, and the lack of standardisation could have some effect on the estimation of the HR. Of particular importance for the current study is that only 57% of fatal strokes were classified by subtype and, while pathological diagnoses were verified by imaging or autopsy, limited information was available from many studies.
In summary, all of the limitations in this study are likely to have resulted in conservative estimates of the PAFs. This only further underscores the impact of smoking on CVD in these regions.
Future
CVD and its risk factors are moving not only from high‐income to LMIC, but also from the more affluent in LMIC to the less affluent. Yet, a recent assessment by the WHO has indicated that the capacity of many countries to prevent and treat chronic diseases remains extremely weak.2 There is a need to develop integrated approaches to prevention, surveillance and control of chronic diseases. There is also a need to continue monitoring the state of smoking and CVD in order to ensure country‐specific policies and programmes for the prevention and treatment of CVD are appropriate, and to gauge the effectiveness of current interventions. The present study is a useful step, and future studies with country‐specific HRs are warranted.
Conclusion
There is convincing evidence that, even on conservative assumptions, tackling smoking could prevent millions of deaths over the next few decades. A decrease in the prevalence of smoking would not only address the increasing rates of CVDs and their risk factors but will also contribute substantially to reducing the incidence and impact of other chronic diseases, such as cancer and chronic respiratory diseases, that share smoking as a common risk factor. There are existing tobacco control policies that have been shown to be effective.20 Implementation of the Framework Convention on Tobacco Control and following through with its protocols is likely the best first step toward addressing the large fraction of cardiovascular disease that is attributable to smoking.
What this paper adds
The prevalence of smoking is high and growing in low and middle‐income countries including the WHO Western Pacific and South East Asian regions. More males than females currently smoke. There is less information on the prevalence of smoking in women. There is little information on the burden of disease caused by smoking in these regions. This study provides estimates for the population attributable fraction of cardiovascular diseases (heart disease and stroke) caused by smoking for men and women.
This study indicates that up to 30% of some cardiovascular fatalities are attributable to smoking in these regions. It provides information on the burden of CVD caused by smoking for both males and females by country. This is the first study to present information on tobacco attributable CVD in two large WHO regions. Information from this study may help inform country‐specific health policies regarding cardiovascular diseases and tobacco control in the Western Pacific and South East Asian regions.
Acknowledgements
This project has received grants from the National Health and Medical Research Council of Australia and an unrestricted educational grant from Pfizer Inc. Martiniuk received support from a Rotary International Ambassadorial Scholarship. The sponsors had no influence on design, analysis or interpretation of results.
Abbreviations
APCSC - Asia Pacific Cohort Studies Collaboration
CVD - cardiovascular disease
IHD - ischaemic heart disease
LMIC - low and middle‐income countries
PAF - population attributable fractions
HR - hazard ratio
WHO - World Health Organization
Footnotes
The authors declare no known competing interests.
References
- 1.Jha P, Chaloupka F J, Brown P.Tobacco control in developing countries: curbing the epidemic. (Chapter 1: Overview). World Bank: Economics of Tobacco Control, 2000. http://www1.worldbank.org/tobacco/tcdc.asp (Accessed March 31, 2005)
- 2.Leeder S, Raymond S, Greenberg H.et alA race against time: the challenge of cardiovascular disease in developing economies. New York: Columbia University, 2004
- 3.de Beyer J, Lovelace C, Yurekli A. Poverty and tobacco. Tob Control 200110210–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Efroymson D, Ahmed S, Townsend J.et al Hungry for tobacco: an analysis of the economic impact of tobacco consumption on the poor in Bangladesh. Tob Control 200110212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gajalakshmi C K, Jha P, Ranson K.et alTobacco control in developing countries: curbing the epidemic. (Chapter 2: Global patterns of smoking and smoking attributable mortality). World Bank: Economics of Tobacco Control, 2000. http://www1.worldbank.org/tobacco/tcdc.asp (Accessed March 31, 2005)
- 6.Murray C JL, Lopez A D. eds. Global health statistics: a compendium of incidence, prevalence and mortality for over 200 conditions. Global burden of disease. Cambridge, Massachusetts: Harvard University Press, 19961–900.
- 7.Tunstall‐Pedoe H. ed. MONICA Monograph and Multimedia Sourcebook. Geneva: World Health Organization, 20031–244.
- 8.Population Reference Bureau 2004 World Population Data Sheet. www.prb.org (Accessed June 29, 2005)
- 9.World Health Organization Tobacco or health: a global status report. Geneva: World Health Organization, 1997
- 10.Lam T H, Ho S Y, Hedley A J.et al Mortality and smoking in Hong Kong: casecontrol study of all adult deaths in 1998. BMJ 2001323361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu B Q, Peto R, Chen Z M.et al Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ 19983171411–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asia Pacific Cohort Studies Collaboration Determinants of cardiovascular disease in the Asian Pacific region: protocol for a collaborative overview of cohort studies. Cardiovascular Disease Prevention 19992281–289. [Google Scholar]
- 13.World Health Organization 1997 [Solomon Islands]. Tobacco or health: a global status report. Geneva, WHO http://www.cancer.org/downloads/TOB/Solomon_Islands.pdf (Accessed July 1, 2005)
- 14.Barraclough S. Women and tobacco in Indonesia. Tob Control 19998327–32 http://www.cancer.org/downloads/TOB/Timor_Leste.pdf (Accessed July 1, 2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ugen S. Bhutan: the world's most advanced tobacco control nation? Tob Control 200312431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woodward M, Lam T H, Barzi F. Asia Pacific Cohort Studies Collaboration. Smoking, quitting and the risk of cardiovascular disease among women and men in the Asia‐Pacific Region. Int J Epidemiol 2005341036–1045. [DOI] [PubMed] [Google Scholar]
- 17.Peto R, Lopez A D, Boreham J.et alMortality from smoking in developed countries 1950–2000: indirect estimates from national vital statistics. New York: Oxford University Press, 1994
- 18.Ghaffar A, Reddy K S, Singhi M. Burden of non‐communicable diseases in South Asia. BMJ 2004328807–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ezzati M, Lopez A D. Measuring the accumulated hazards of smoking: global and regional estimates for 2000. Tob Control 20031279–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jha P, Paccaud F, Nguyen S.Tobacco control in developing countries: curbing the epidemic. (Chapter 19: Strategic priorities in tobacco control for governments and international agencies) World Bank: Economics of Tobacco Control, 2000. http://www1.worldbank.org/tobacco/tcdc.asp (Accessed March 31, 2005)
- 21.Gunasekara O. Sri Lanka: Sentinel tobacco use prevalence survey 2001. In: Strong K, Bonita R, eds. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva: WHO, 2003. http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 22.Singapore Ministry of Health National Health Surveillance Survey 2001. In Strong K, Bonita R. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva: WHO, 2003. http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 23.Hong Kong Council on Smoking and Health Smoking prevalence in Hong Kong 2000. Wanchai, Hong Kong http://www.info.giv.hk/hkcosh/ (Accessed June 10, 2005)
- 24.Futterman A.Palau Ministry of Health: Palau substance abuse needs assessment (SANA) 1998. http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 25.International Institute for Population Services India National Family Health Survey (NFHS‐2) 2000. ORC Macro: Calverton, MD, http://www.nfhsindia.org/india.html (Accessed June 10, 2005)
- 26.Australian Institute of Health and Welfare 2004 National Drug Strategy Household Survey: State and territory supplement 2005. Canberra: Australian Institute of Health and Welfare, 2005. http://www.aihw.gov.au/publications/phe/ndshs04sts/ndsh04sts.pdf (Accessed June 10, 2005)
- 27.Thailand National Statistical Office The Survey of Cigarette Smoking 2001. http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 28.Shmulewitz D, Auerbach S B, Lehner T.et al Epidemiology and factor analysis of obesity, type II diabetes, hypertension, and dyslipidemia (syndrome X) on the Island of Kosrae, Federated States of Micronesia. Human Heredity 2001518 19 http://www.cancer.org/downloads/TOB/Micronesia.pdf (Accessed June 10, 2005). [DOI] [PubMed] [Google Scholar]
- 29.New Zealand Ministry of Health Males and Females ‐ Tobacco Facts 1998. http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 30.Yen L L, Pan L Y. Smoking prevalence and behaviours of adults in Taiwan: a national survey 1999. Chin J Public Health (Taipei) 200019423–36 http://ccms.ntu.edu.tw/˜ihpm/prospectus/teachers/lee2000‐1.PDF (Accessed June 10, 2005). [Google Scholar]
- 31.World Health Organization South‐East Asian Regional Office Maldives Ministry of Health National Survey 2001. http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 32.Maxwell J C. Davenport & Company LLC. The Maxwell Consumer Report: international tobacco report ‐ Part one and two. 1998 http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 33.Zain Z.Malaysia Ministry of Health Penang State Health Department's Second National Health and Morbidity Survey (NHMS2) 1996. http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 34.World Health Organization Smoking in Tutong, Brunei: a changing habit. Med J Malaysia 1979;XXXIV:3–5 http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005) [PubMed]
- 35.Southeast Asia Tobacco Control Alliance and ASH Thailand Smoking data from the Second Vietnam Living Standard Survey 1998. http://www.tobaccofreeasia.net (Accessed June 10, 2005)
- 36.World Health Organization Western Pacific Region Laos Country Profile Pilot study in Vientaine. Tobacco or Health 2000 http://www.cancer.org/downloads/TOB/Lao_PDR.pdf (Accessed June 10, 2005)
- 37.Li N. Prevalence of coronary heart disease indicated by electrocardiogram abnormalities and risk factors in developing countries. J Clin Epidemiol 199447599–611 http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005). [DOI] [PubMed] [Google Scholar]
- 38.Tiglao T V, Baquilod M M. Philippines Baseline Risk Factor Survey 2001. In: Strong K, Bonita R, eds. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva: WHO, 2003. http://www.cancer.org/downloads/TOB/Philippines.pdf (Accessed June 10, 2005)
- 39.Japan Ministry of Health, Labor and Welfare Kokumin‐eiyou no Genjo: Heisei 12‐nen Kokumineiyou chosa kekka. [Results of National Nutrition Survey 2000] Reported in Strong K and Bonita R. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva, 2003. WHO http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 40. WHO Western Pacific Regional Office [Vanuatu Smoking Prevalence] 1990. http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 41.Pande B, Karki Y, Plant K. A study on tobacco economics in Nepal. In Strong K, Bonita R. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva: WHO, 2003. http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 42.Kyaing N N.Myanmar Sentinel Tobacco Use Prevalence Study 2001. http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 43.Yang G. Smoking in China: findings of the 1996 National Prevalence Survey. JAMA 19992821247–1253 http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005). [DOI] [PubMed] [Google Scholar]
- 44.Yunus M. Craving for nicotine: a study on tobacco prevalence in Bangladesh 2000. In: Strong K, Bonita R, eds. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva: WHO, 2003. http://www.whoban.org/tobbacco.html (Accessed June 10, 2005)
- 45.World Bank [Smoking Prevalence in South Korea] 1995 http://www1.worldbank.org/tobacco/brieflist_db.asp (Accessed June 10, 2005)
- 46.Strong K, Bonita R. Current smoking data from the Indonesia Health Survey (SURKENAS) 2001. The SuRF Report 1. Surveillance of risk factors related to non‐communicable diseases: current status of global data. Geneva: WHO, http://w3.whosea.org/EN/Section1174/section1462/TFIMain.asp?pg = surveillance (Accessed June 10, 2005)
- 47.Sukhbat G. Medical University of Mongolia Health Sector Review 1999. http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 48.Woodward A. Smoking in the Kingdom of Tonga: report from a national survey. Tob Control 1994341–45. [Google Scholar]
- 49.Cambodia National Institute of Statistics Cambodian Socioeconomic Survey 1999. Phnom Penh http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005)
- 50.Stanton H, Tuomilehto J. Smoking rates in the Pacific Islands (Tuvalu). Bull World Health Organ 198664447–456 http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005). [PMC free article] [PubMed] [Google Scholar]
- 51.McGarvey S T.Current smoking in Samoa. International Health Institute, Brown University School of Medicine 1995 http://www.cancer.org/downloads/TOB/Samoa.pdf
- 52.Lindeberg S. Apparent absence of stroke and ischaemic heart disease in a traditional Melanesian Island: a clinical study in Kitava. J Intern Med 1993233269–75 http://tfi.wpro.who.int/prevalence.asp (Accessed June 10, 2005). [DOI] [PubMed] [Google Scholar]