Abstract
Objective
To examine the development of smoking behaviour among adolescents who, at age 11, had tried cigarettes just once.
Design
A five‐year prospective study.
Setting
36 schools in South London, England.
Subjects
A socioeconomically and ethnically diverse sample of students completed questionnaires annually from age 11–16. A total of 5863 students took part, with an annual response rate ranging from 74–85%. 2041 (35%) provided smoking status data every year.
Main outcome measures
Current smoking (smoking sometimes or more often) for the first time. Cotinine assays provided biochemical verification of smoking status.
Results
Students who at age 11 reported having tried smoking cigarettes just once (n = 260), but were not smoking at the time, were more likely to take‐up smoking at a later age than those that had not tried smoking (n = 1719), even after a gap of up to three years of not smoking. The odds of starting to smoke at age 14 were 2.1 times greater (95% confidence interval 1.2 to 3.5) in the age 11 “one time triers” than the “non‐triers”, even once sex, ethnicity, deprivation, parental smoking and conduct disorder were adjusted for.
Conclusions
This is the first clear demonstration of a “sleeper effect” or period of dormant vulnerability. Our findings have implications for understanding the development of cigarette use and for policies to reduce smoking in young people. Preventing children from trying even one cigarette may be important, and the design of interventions should recognise adolescents who have smoked just once, several years previously, as potentially vulnerable to later smoking uptake.
Keywords: smoking, adolescence, longitudinal studies
Cigarette use is typically initiated in adolescence.1 In 2004 in England 14% of 11 year olds and 62% of 15 year olds reported ever having tried cigarettes,2 a large number of whom will go on to smoke for many years.3 The damage to health caused by these years of smoking is well known, therefore understanding the process of progression from non‐smoking to smoking uptake is of considerable importance.
Cross‐sectional and retrospective studies have suggested that the progression from early trying to regular cigarette use can take several years.4,5,6 Similarly, a number of longitudinal studies have tracked adolescent smoking behaviour over time and shown that the development of cigarette use can occur at different rates and intensities.7,8,9,10,11,12,13 For example Audrain‐McGovern et al7 distinguished early/fast adopters, late/slow adopters, experimenters and never smokers, while Chassin et al11 differentiated between early stable smokers, late stable smokers, experimenters and quitters. These subgroups of cigarette users can often, although not always,13 be distinguished in terms of risk factors for smoking, such as attitudes to smoking,9 parental and friend smoking,11 reported grades7,10 and coping style.12 This heterogeneity suggests that smoking prevention programmes need to be tailored and varied in order to reach all groups of potential cigarette smokers.
The aim of this paper is to focus on one particular group of cigarette users, those who have tried just one cigarette at age 11, to establish the probability of, and time taken to progress to, later current smoking. Previous prospective research has shown that early cigarette experience is strongly linked to later behaviour.14,15,16 Patton et al16 found that occasional cigarette use was associated with an eight‐fold increase in the probability of being a daily cigarette smoker three years later, while Jackson et al14 showed even minimal childhood use of cigarettes to be predictive of smoking at age 17. However, limited follow‐up after periods of several years mean these studies are unable to track the progression of smoking uptake in a continuous fashion.
The present study uses data from the HABITS (Health and Behaviour in Teenagers) project, a five year prospective study in a socioeconomically and ethnically diverse population, with annual assessments of smoking status, to examine in detail the process of becoming a cigarette smoker from age 11 years to age 16 years. Our methodology provided an opportunity to give a clear picture concerning the risk of taking up smoking later in adolescence in children who had reported a single exposure to smoking at an earlier age.
METHODS
A total of 5863 students from 36 London schools took part in the HABITS study, a five year cohort study with annual waves of data collection between 1999 and 2003. Each year across the five years of secondary schooling, from year 7 (age 11–12, US grade 6) to year 11 (age 15–16, US grade 10), students completed a questionnaire in the classroom and provided a saliva sample for cotinine assay (a sensitive measure of nicotine intake). Schools were selected from a sampling frame designed to produce a socioeconomically and ethnically diverse sample. Parents were given the option to withdraw their child, and students could withdraw themselves from the study, which was approved by University College London/University College London Hospital Ethics Committee. At baseline 84% of those registered at the 36 schools took part; 10% were absent on the day of data collection and 5.5% opted out. Response proportions ranged from 74–85% throughout the study.
Participants were asked to indicate which of the following best described them: “I have never smoked”, “I have only ever tried smoking once”, “I used to smoke sometimes but I never smoke cigarettes now”, “I sometimes smoke cigarettes now but I don't smoke as many as one a week”, “I usually smoke between one and six cigarettes a week”, and “I usually smoke more than six cigarettes a week”. For these analyses we have defined current smoking as reporting smoking cigarettes sometimes or more frequently, “one time triers” describes those reporting having only ever tried smoking once, and non‐current smokers include never smokers, one time triers and ex‐smokers. Non‐current smokers whose cotinine value was above a cut point of 15 ng/ml were reclassified as current smokers. Other measures included in the analyses were: sex, area level socioeconomic deprivation (Townsend scores derived from postcode data17), ethnicity, parental smoking, and conduct problems.18 More details of the sampling method and procedures used are described elsewhere.19
Data analysis
At each year the probability of becoming a new current smoker (smoking cigarettes sometimes or more frequently for the first time) was calculated for those who had never tried cigarettes at year 7 (age 11–12) and who had tried cigarettes just once at year 7 (year 7 “one time triers”). New current cigarette use was calculated at each year as the percentage of previously non‐current smokers who became current cigarette smokers for the first time that year, as opposed to remaining a non‐current smoker. In order to establish when students first reported current smoking, only data from participants who provided smoking status data at each year were included in the analyses.
To establish the magnitude of the association between being a “one time trier” and onset of current smoking, a series of logistic regressions were performed using SPSS version 13, with smoking status at age 11–12 as the independent variable and new uptake of current smoking at each study year as the dependent variables. By looking at new uptake of current smoking, participants were excluded from analyses if they had already progressed to current smoking. This methodology therefore describes the longitudinal development of current smoking across the five years of the study. Sex, deprivation, ethnicity, parental smoking and conduct problems were then added to the model as covariates in order to examine the persistence of any effect once common variables known to influence vulnerability to smoking uptake were included.
RESULTS
Of those with full smoking data at each year (n = 2041, 34% of the whole sample), 56.4% (1151) were boys and 43.6% (890) were girls. The sample was ethnically diverse with 64.1% (1309) white, 22.6% (461) black/mixed black, 11.1% (227) Asian/mixed Asian, and 2.2% (44) of other ethnic origin. 84.3% (1720) of year 7 participants described themselves as having never smoked at age 11–12. After re‐classifying a single individual with a high level of cotinine as a current smoker, this figure dropped to 84.2% (1719). 12.7% (260) of year 7 participants reported having tried smoking just once at age 11–12, with no responses discrepant with cotinine values. Both self‐reported and cotinine adjusted current smokers at each year are displayed in table 1, as well as the percentage of all participants who reported current smoking for the first time at each year.
Table 1 Percentage (n) of self‐reported and cotinine adjusted current smoking (smoking sometimes or more often) and new current smoking (current smoking for the first time) at each study year.
| Year 7 | Year 8 | Year 9 | Year 10 | Year 11 | |
|---|---|---|---|---|---|
| Self‐reported current smoking | 1.1 (23) | 5.1 (104) | 12.4 (253) | 22.8 (465) | 28.6 (584) |
| Cotinine‐adjusted current smoking | 1.3 (26) | 5.1 (105) | 12.5 (255) | 23.0 (469) | 29.3 (597) |
| Cotinine‐adjusted new current smoking | – | 3.9 (80) | 6.8 (139) | 8.2 (168) | 6.9 (141) |
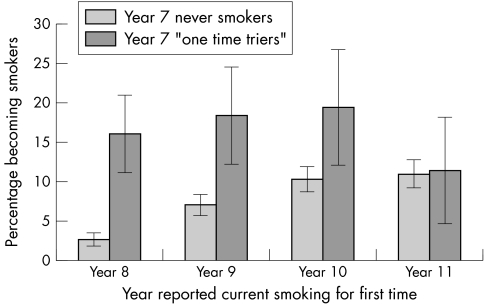
Figure 1 shows that 16% (35) of year 7 “one time triers” became current smokers for the first time in year 8 (age 12–13) compared with only 3% (45) of year 7 never smokers. Similarly 18% (28) of year 7 “one time triers” became current smokers for the first time in year 9 (age 13–14) compared with only 7% (111) of year 7 never smokers, and 20% (22) became current smokers in year 10 (age 14–15) compared with 10% (146) of year 7 never smokers. In these respondents, no further smoking, beyond the initial cigarette, had been reported in the intervening years and therefore current cigarette use was not reported until several years after the first cigarette. It was only in year 11 (age 15–16) that new current cigarette use finally equalised across the year 7 “one time triers”, 12% (10) and never smokers, 11% (131).
Figure 1 Percentage of year 7 never smokers and “one time triers” becoming current smokers for the first time as they progress through each school year.
The results of the logistic regression analyses are shown in table 2. Being a year 7 “one time trier” placed students at an increased risk, compared with those who had never smoked at this age, of reporting current smoking in the future. The relationship was strongest one year later (odds ratio (OR) 6.3) and, although the odds ratios decrease at each subsequent year, being a “one time trier” at year 7 was still predictive of starting to smoke for the first time up to year 10 (OR 2.1), several years after the first cigarette was smoked. The adjusted results show that the addition of sex, ethnicity, deprivation score, parental smoking and conduct problems to the model did not alter these results and that being a year 7 “one time trier” was a stronger predictor of new current smoking than these common covariates.
Table 2 Unadjusted and adjusted odds ratios of starting current smoking for the first time at year 8, year 9, year 10 and year 11 as a function of being a year 7 “one time trier” in relation to never smoking.
| Unadjusted odds OR (95% CI) | Year 8 (n = 1900) | Year 9 (n = 1721) | Year 10 (n = 1514) | Year 11 (n = 1283) |
|---|---|---|---|---|
| Year 7 Smoking | ||||
| Never tried | 1 | 1 | 1 | 1 |
| Tried just once | 7.0*** (4.36 to 11.10) | 3.0*** (1.89 to 4.67) | 2.1** (1.27 to 3.41) | 1.1 (0.53 to 2.09) |
| Adjusted odds OR (95% CI) | Year 8 (n = 1888) | Year 9 (n = 1709) | Year 10 (n = 1503) | Year 11 (n = 1273) |
|---|---|---|---|---|
| Year 7 smoking | ||||
| Never tried | 1 | 1 | 1 | 1 |
| Tried just once | 6.3*** (3.80 to 10.53) | 2.9*** (1.79 to 4.73) | 2.1** (1.22 to 3.51) | 1.0 (0.49 to 2.02) |
| Covariates | ||||
| Sex | ||||
| Boys | 1 | 1 | 1 | 1 |
| Girls | 2.8*** (1.68 to 4.59) | 2.0*** (1.37 to 2.85) | 1.4 (0.97 to 1.90) | 1.2 (0.83 to 1.71) |
| Deprivation | 0.94 (0.78 to 1.14) | 1.0 (0.86 to 1.15) | 0.90 (0.79 to 1.03) | 1.1 (0.96 to 1.28) |
| Ethnicity | ||||
| White | 1 | 1 | 1 | 1 |
| Black | 1.0 (0.54 to 1.87) | 0.41** (0.24 to 0.73) | 0.45** (0.26 to 0.77) | 0.40*** (0.21 to 0.65) |
| Asian | 0.91 (0.37 to 2.23) | 0.41* (0.20 to 0.83) | 0.62 (0.35 to 1.09) | 0.60 (0.32 to 1.03) |
| Other | 0.96 (0.20 to 4.52) | 0.46 (0.11 to 2.00) | 0.40 (0.09 to 1.72) | 0.65 (0.19 to 2.23) |
| Parental smoking | ||||
| Neither smoke | 1 | 1 | 1 | 1 |
| Father smokes | 0.96 (0.48 to 1.90) | 1.3 (0.81 to 2.06) | 1.4 (0.95 to 2.21) | 1.3 (0.83 to 2.07) |
| Mother smokes | 2.1 (1.00 to 4.22) | 1.8* (1.00 to 3.18) | 1.5 (0.81 to 2.72) | 1.3 (0.69 to 2.63) |
| Both smoke | 2.9** (1.52 to 5.42) | 1.2 (0.61 to 2.17) | 1.8* (1.06 to 3.19) | 0.73 (0.35 to 1.54) |
| Conduct problems score | 1.1 (0.94 to 1.22) | 1.1 (0.98 to 1.21) | 1.1* (1.00 to 1.22) | 1.1** (1.04 to 1.27) |
*p<0.05; **p<0.01; ***p<0.0005.
In order to identify the year current smoking was first reported, only participants who provided complete smoking data at every year were included in the above analyses (n = 2041, 34% of the whole sample). Table 3 shows how those with complete smoking data differ from those who were absent at one or more years. Most notably those with complete data are less likely to be smokers. However, when analyses were re‐run using all available data for the required years (that is, years 7 and 8 when predicting new year 8 current smoking and years 7, 8 and 9 when predicting new year 9 current smoking), findings remained the same; being a “one time trier” at year 7 was associated with a higher risk of new uptake of current smoking compared to year 7 never smokers, even after three years of non‐current smoking (year 8 (n = 3229), OR 8.7, 95% CI 6.47 to 11.68; year 9 (n = 2320), OR 3.1, 95% CI 2.17 to 4.41; year 10 (n = 1731), OR 2.3, 95% CI 1.45 to 3.50; year 11 (n = 1283), OR 1.1, 95% CI 0.53 to 2.09).
Table 3 Sociodemographic and smoking differences between those providing full smoking data and those absent for one or more years, percentage/mean (n).
| Full data | Incomplete data | Significance | |
|---|---|---|---|
| Sex | |||
| Boys | 56.4 (1151) | 60.4 (2308) | p = 0.003 |
| Girls | 43.6 (890) | 39.6 (1513) | |
| Deprivation (mean score) | 2.9 (2037) | 3.2 (3599) | p<0.001 |
| Ethnicity | |||
| White | 64.1 (1309) | 55.0 (2015) | p<0.001 |
| Black | 22.6 (461) | 27.9 (1021) | |
| Asian | 11.1 (227) | 10.9 (400) | |
| Other | 2.2 (44) | 6.2 (227) | |
| Conduct problems (mean score) | 2.6 (2034) | 3.0 (2252) | p<0.001 |
| Parental smoking | |||
| Neither smoke | 62.5 (1274) | 46.6 (1049) | p<0.001 |
| Father smokes | 18.5 (378) | 21.0 (472) | |
| Mother smokes | 8.6 (176) | 12.4 (279) | |
| Both smoke | 10.3 (210) | 20.0 (450) | |
| Smoking | |||
| Year 7 one time trier | 12.7 (260) | 20.7 (462) | p<0.001 |
| Year 8 current smoker | 5.1 (105) | 11.4 (256) | p<0.001 |
| Year 9 current smoker | 12.5 (255) | 18.4 (387) | p<0.001 |
| Year 10 current smoker | 23.0 (469) | 26.3 (551) | p = 0.013 |
| Year 11 current smoker | 29.3 (597) | 33.6 (562) | p = 0.004 |
DISCUSSION
In line with past research suggesting that progression to current smoking uptake can take several years,4,5,6 our results show that progression from experimenting with one cigarette (being a “one time trier”) to current smoking can take up to three years. However, we have also shown that, between trying an early cigarette and regular smoking uptake, there may be a protracted period of dormancy when no reported smoking occurs; what may be termed a “sleeper effect”, a personal propensity or vulnerability to smoke that may not become manifest without additional triggers.
There are several potential explanations for the mechanism of this “sleeper effect”. From a neurobiological viewpoint, neural reward pathways might be changed as a consequence of a single exposure to nicotine,20 thus potentially increasing vulnerability to later smoking uptake. Changes in the environment are likely to trigger a repeated experience with cigarettes among those vulnerable—for example, through changing protective and risk factors such as peer smoking, stress, depression, religiosity and school environment.21,22 Alternatively, from a social cognition perspective,23 an early experience with cigarettes might break down barriers that would otherwise prevent or delay smoking, such as fear of adverse reactions to smoking or insecurities regarding how to smoke. If these potential concerns have been overcome in the past, the likelihood of accepting a cigarette at a later time point may be raised in relation to those who have not had this experience, resulting in the expression of a behaviour which has been dormant. Finally, from a constitutional vulnerability viewpoint, past research suggests that individuals with a particular social and psychological profile are more likely to become smokers.21,22,24 The personal traits that lead to early experience of smoking could contribute an underlying increase in risk of smoking that is not triggered until environmental conditions are right.
What this paper adds
Progression from early trying to regular smoking can take several years, and various “trajectories” of progression of smoking from initial experimentation have been described. No previous prospective study has as yet assessed the extent to which children who have experimented with smoking show a pattern of dormant vulnerability.
This study provides the first prospective evidence that a single experience with cigarettes reported at age 11 places adolescents at significantly greater risk of becoming a current smoker even after up to three years of non‐smoking in the intervening years.
Whatever the explanation, there are important practical and policy implications. Our results show that young adolescents enter secondary school with a smoking history which represents a lasting predisposition to be at risk of becoming a later current smoker. It may be that preventing children from trying even one cigarette is an important goal, and prevention efforts could usefully be focused at the earliest ages. Secondly, these results suggest that previous experimentation is a strong predictor of later smoking uptake and the finding of a “sleeper effect” indicates that general practitioners, other health care providers, and those designing targeted interventions should pay particular attention to adolescents who report having tried cigarettes just once in the past.
The study has a number of limitations. Smoking behaviour was self‐reported and although the ability to validate smoking responses with cotinine assays is one strength of the study, this method does not give any indication as to the smoking behaviour of participants in the past. However, given previous evidence that self‐reported smoking by adolescents is generally reliable,25 and the small number of participants re‐classified as smokers on the basis of cotinine results in the current study, it is likely that pupils' statements are accurate. A second limitation is the attrition of pupils across the five years of the study. The analyses in the current paper are restricted to those participants providing smoking data at each year of the study. However, when we repeated the analyses using all the available data, findings were little changed. The low numbers of new smokers in year 11 may reflect inadequate statistical power or alternatively a ceiling effect in smoking uptake. Either way, caution should be taken in concluding that the non‐significant result in year 11 signifies that the “sleeper effect” does not extend for more than three years. Thirdly, there may be concerns regarding the generalisability of our results; however, the schools included in our sampling frame were selected to be both socioeconomically and ethnically diverse. Finally, the extent of smoking experimentation by age 11 in this sample suggests that the story actually starts at a much earlier time point and although the development of smoking behaviour is largely captured in examination of those aged 11 to 16, extension of research to both younger children and older teenagers and young adults would enable a fuller understanding of this progression.
ACKNOWLEDGEMENTS
The participation of the 36 schools and all students is gratefully acknowledged, as is the work of all those involved in the collection of data. We also thank David Boniface, who advised on the analysis of the data and Dr Jane Bradbury who commented on draft versions of the paper.
Footnotes
Funding: This study was funded by Cancer Research UK and the Department of Health for England who had no involvement in any aspect of the design, collection, analysis and interpretation of data, the writing of the report or the decision to submit the paper for publication.
Conflict of interest: Robert West undertakes research and consultancy for developers and manufacturers of smoking cessation treatments such as nicotine replacement products. No other authors have any conflicts of interest.
Ethics approval: This study was approved by the University College London/University College London Hospital Ethics Committee
Contribution of authors: JAF, JW, NHB, MJJ and RW participated in the conception, analysis and interpretation of the above paper. JAF and RW wrote the manuscript and JW, MJJ and NHB were involved in revisions of the original manuscript.
References
- 1.Royal College of Physicians Nicotine addiction in Britain. A report of the tobacco advisory group of the Royal College of Physicians. London, Royal College of Physicians of London 2000
- 2.Fuller E.Smoking, drinking and drug use among young people in England in 2004. Health and Social Care Information Centre 2005
- 3.Pierce J P, Gilpin E. How long will today's new adolescent smoker be addicted to cigarettes? Am J Public Health 199686253–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leventhal H, Cleary P D. The smoking problem: a review of the research and theory in behavioral risk modification. Psychol Bull 198088370–405. [DOI] [PubMed] [Google Scholar]
- 5.Robinson M L, Berlin I, Moolchan E T. Tobacco smoking trajectory and associated ethnic differences among adolescent smokers seeking cessation treatment. J Adolesc Health 200435217–224. [DOI] [PubMed] [Google Scholar]
- 6.Stallings M C, Hewitt J K, Beresford T.et al A twin study of drinking and smoking onset and latencies from first use to regular use. Behav Genet 199929409–421. [DOI] [PubMed] [Google Scholar]
- 7.Audrain‐McGovern J, Rodriguez D, Tercyak K P.et al Identifying and characterizing adolescent smoking trajectories. Cancer Epidemiol Biomarkers Prev 2004132023–2034. [PubMed] [Google Scholar]
- 8.Orlando M, Tucker J S, Ellickson P L.et al Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. J Consult Clin Psychol 200472400–410. [DOI] [PubMed] [Google Scholar]
- 9.Soldz S, Cui X. Pathways through adolescent smoking: a 7‐year longitudinal grouping analysis. Health Psychol 200221495–504. [PubMed] [Google Scholar]
- 10.White H R, Pandina R J, Chen P H. Developmental trajectories of cigarette use from early adolescence into young adulthood. Drug Alcohol Depend 200265167–178. [DOI] [PubMed] [Google Scholar]
- 11.Chassin L, Presson C C, Pitts S C.et al The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol 200019223–231. [PubMed] [Google Scholar]
- 12.Wills T A, Vaccaro D, McNamara G.et al Escalated substance use: a longitudinal grouping analysis from early to middle adolescence. J Abnorm Psychol 1996105166–180. [DOI] [PubMed] [Google Scholar]
- 13.Abroms L, Simons‐Morton B, Haynie D L.et al Psychosocial predictors of smoking trajectories during middle and high school. Addiction 2005100852–861. [DOI] [PubMed] [Google Scholar]
- 14.Jackson C, Dickinson D. Cigarette consumption during childhood and persistence of smoking through adolescence. Arch Pediatr Adolesc Med 20041581050–1056. [DOI] [PubMed] [Google Scholar]
- 15.Choi W S, Gilpin E A, Farkas A J.et al Determining the probability of future smoking among adolescents. Addiction 200196313–323. [DOI] [PubMed] [Google Scholar]
- 16.Patton G, Carlin J, Coffey C.et al The course of early smoking: a population‐based cohort study over three years. Addiction 1998931251–1260. [DOI] [PubMed] [Google Scholar]
- 17.Townsend P, Phillimore P, Beattie A.Health and deprivation: inequalities and the North. London: Croom Helm, 1998
- 18.Goodman R, Meltzer H, Bailey V. The strengths and difficulties questionnaire: a pilot study on the validity of the self‐report version. Eur Child Adolesc Psychiatry 19987125–130. [DOI] [PubMed] [Google Scholar]
- 19.Wardle J, Jarvis M J, Steggles N.et al Socioeconomic disparities in cancer‐risk behaviors in adolescence: baseline results from the Health And Behaviour In Teenagers Study (HABITS). Prev Med 200336721–730. [DOI] [PubMed] [Google Scholar]
- 20.Fagen Z M, Mansvelder H D, Russel K J.et al Short‐ and long‐term modulation of synaptic inputs to brain reward areas by nicotine. Ann N Y Acad Sci 20031003185–195. [DOI] [PubMed] [Google Scholar]
- 21.Schepis T S, Rao U. Epidemiology and etiology of adolescent smoking. Curr Opin Pediatr 200517607–612. [DOI] [PubMed] [Google Scholar]
- 22.Tyas S L, Pederson L L. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control 19987409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bandura A.Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, New Jersey: Prentice‐Hall, 1986
- 24.Burt R D, Dinh K T, Peterson A V.et al Predicting adolescent smoking: a prospective study of personality variables. Prev Med 200030115–125. [DOI] [PubMed] [Google Scholar]
- 25.Dolcini M M, Adler N E, Lee P.et al An assessment of the validity of adolescent self‐reported smoking using three biological indicators. Nicotine Tob Res 20035473–483. [PubMed] [Google Scholar]