Abstract
Objectives
To measure the coverage, gender distribution, and participants' prevalence of genital Chlamydia trachomatis infections using a new internet based self selective testing approach by means of home sampling in the general population in Sweden. To investigate factors associated with these measures.
Methods
Observational survey of people actively ordering coded testing packages, and checking their test results, from a known website. No personal invitations were sent out. All inhabitants (256 885 men and women) in a Swedish county were eligible to participate. A special interest was taken in coverage, gender distribution, participants' chlamydia prevalence, and determinants for infection.
Results
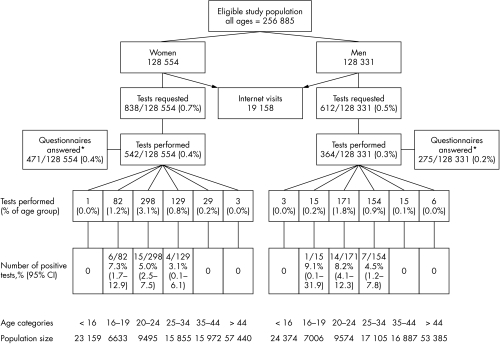
Testing was highest in the age group 20–24 years, where 298/9495 (3.1%) of all women and 171/9574 (1.8%) of all men in the population participated. The overall population participation (all ages) was 906/256 885 (0.4%). 40% (364/906) of the tests were from men and 60% (542/906) from women. The prevalence of Chlamydia trachomatis infection was 6.0% (95% CI: 3.6% to 8.4%) among male participants and 4.6% (95% CI: 2.8% to 6.4%) among female participants. Prevalence increased with decreasing age. Believing to be infected and having symptoms were the strongest determinants of infection.
Conclusion
Simplifying and increasing the accessibility of chlamydia testing by means of internet and home sampling proved feasible. Self risk assessment improves the chance of finding people infected by Chlamydia trachomatis, especially among men, if an accessible testing method is offered. This new method can serve as a supplement to regular preventive methods and might encourage young people to be tested.
Keywords: sexually transmitted infections, home sampling, internet, gender, Chlamydia trachomatis
Infections caused by Chlamydia trachomatis, being easily treated but mostly asymptomatic, have long posed a challenge to primary and secondary prevention. Despite current preventive measures chlamydia rates are increasing in Sweden and other European countries.1 With the advent of home sampling new possibilities for active screening have emerged but many posted testing kits are never used.2 All large scale chlamydia screening programmes have up till now consistently showed a lower male than female participation rate.3,4 It has been suggested that long term reduction in the prevalence of chlamydia infections seems improbable with the current screening programmes, unless men are included comprehensively and innovative strategies are developed to encourage young people to be screened.5,6 With an individualised self selective testing approach we wanted to investigate the feasibility of a simpler and more effective chlamydia testing method using home sampling and the internet. A special interest was taken in coverage, gender distribution, participants' C trachomatis prevalence, and factors associated with these measures.
Methods
Eligible people
The study was conducted from September 2004 to April 2005. All males and females with permanent addresses in the county of Västerbotten were eligible to participate. Västerbotten is a sparsely populated county in northern Sweden with 250 000 inhabitants (3% of the Swedish population), which compromises 13% of the Swedish total area.
Website content and design
The website contains information about chlamydia in Swedish and English (www.klamydia.se) and also relevant links to more information about other sexually transmitted infections (STI). All material was written and developed by a medical doctor with previous experience of internet related medical advice and by a sexual health educator. The website content was approved by a committee of doctors, nurses, and other public health professionals. Layout and design was done by a professional programmer.
Website testing procedure
The informative chlamydia website offered the opportunity to order a home chlamydia test package that is free. To receive a test package, participants needed to type in their civic registration number, postal address, and an optional email address. Orders were stored in a database and test packages were sent to the participants. The test package contained a cover letter, a personally coded urine specimen container, a laboratory requisition slip, and a questionnaire. The cover letter briefly described the study and gave instruction on how to obtain a first void urine specimen and to store the specimen in a refrigerator before mailing. Participants were informed that only four central research workers were aware of their identity. The participants could then send in their coded urine specimen, the laboratory slip, and the questionnaire in a prepaid preaddressed biological substance envelope to the local laboratory. The local medical ethics committee approved the study.
The questionnaire
The questionnaire was optional to answer. The questionnaire was coded so results were fed into a database anonymously and each code was related to its test result. It was a multiple choice questionnaire with 17 questions. The questions regarded reasons for testing, socioeconomic status of parents, sexual behaviour associated with increased risk of acquiring C trachomatis, and general internet usage. The questions have previously been validated.7,8,9
Sample analysis
Upon receipt, the urine specimens were analysed for C trachomatis DNA by means of a commercially available polymerase chain reaction (PCR) test (BDProbeTec ET system for detection of C trachomatis test, BD Biosciences, Madrid, Spain) according to the instructions of the manufacturer. For each specimen an internal control was included. A negative result was reported as negative only if the sample was negative for C trachomatis and the internal control was positive. A sample positive for C trachomatis was reanalysed and reported as positive if the reanalysis was also positive.
Obtaining the results
The laboratory test results were fed into the database as a simple text file. The participants could access their results by typing in their personal code on the website. If the urine sample was negative for C trachomatis a message appeared on the screen telling them that they were not infected with chlamydia but if they still had symptoms or worried about other STI they should contact their physician. If the urine specimen was positive for C trachomatis a message appeared on the screen instructing them to print out a physician referral sheet for treatment.
Treatment and control
Infected people who sought treatment also received counselling and participated in partner tracing. Partner tracing was performed by a specially trained social worker. Receiving a letter from the treating physician confirmed that the infected person had sought treatment. Participants who had not accessed their test results within 2 weeks after the test results were put into the database were automatically reminded first by three emails and then by phone. Participants who had accessed their test result but from whom we had not received a confirming letter, from a treating physician, within 4 weeks were automatically reminded by emails and then by phone.
Website database and security
Information entered online while ordering was stored in a database independent of other computer systems. In addition to saving the participants' names, civic registration numbers, and addresses the database also stored test results to be viewed with personal codes. The only place the names appeared with the personal code was on the laboratory slip and the doctor's referral sheet. The personal codes and their corresponding test results were recorded in the database. Personal data were stored according to the Swedish law on personal data.
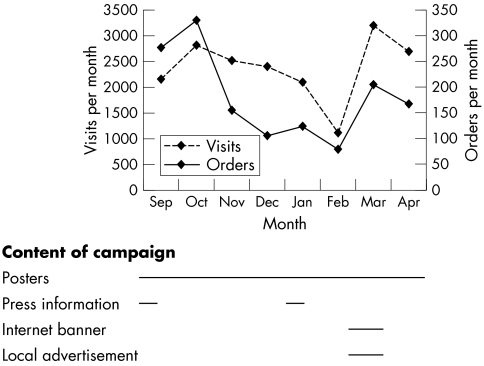
Website marketing
Marketing was mostly done by word of mouth. Except for a press conference at the start, a poster at each youth health centre, and one poster sent to each school in the county, no other campaign was done during the study period. During the last month of the study a banner was shown on a popular chat website and a video commercial was run at a local sporting arena.
Statistical analyses
Statistical analyses of coverage of chlamydia testing (proportion testing themselves) participation (proportion testing and submitting questionnaire) was performed using SPSS (SPSS Inc, Chicago, IL, USA) software for Windows. Differences in prevalence between sexes were analysed using two sided Pearson χ2 or Fisher's exact test. The association between chlamydia infection (dependent variable) and test reasons (independent variables) was investigated by multivariate logistic regression analysis.
Results
Test rate and prevalence
On average, the website received 85 visits per day with more visits and orders after the weekend. An average of 14 orders was made per day. Most visits and orders were done during the afternoon. Figure 1 portrays the number of tests requested and visit frequency during the study period related to the marketing campaign. The total number of tests requested, tests taken, questionnaires returned, and the C trachomatis prevalence according to age group and sex can be seen in figure 2. A total of 19 518 visits were made, a total of 1450 tests were requested, and a total of 906 tests were performed. The distribution of tests returned was 542/906 (60%) female and 364/906 (40%) male. The C trachomatis prevalence decreased with age but there was no statistically significant difference between the male and female prevalence. The overall male and female C trachomatis prevalence was 6.0% (95% CI: 3.6% to 8.4%) and 4.6% (95% CI: 2.8% to 6.4%), respectively. Most tests were done among 20–24 year olds and more than 3% of all the females in the county tested themselves with this method. The overall uptake (tests returned/tests requested) was 542/838 (65%) for females and 364/612 (59%) for males. An average of 4 days was needed for a person to check their results after they became accessible. An average of 21 days was needed to send in urine sample after ordering. The geographic coverage was good, with orders from all parts of the county. Most orders (93%) were made from the cities. Four infected people needed to be reminded by phone to check their test results and two of these people had lost their codes. One person did not seek treatment but after multiple phone calls and after missing two physician appointments the patient was referred to the county medical officer of Communicable Disease Control who fulfilled the necessary treatment and partner tracing.
Figure 1 Number of tests requested and visits related to content of marketing campaign during the study period. A total 19 518 visits were made and 1450 tests were requested. Note that the study period started in the middle of September and ended in the middle of April.
Figure 2 Flow diagram showing the activity of residents in Västerbotten County, Sweden. The figure shows web page visits, Chlamydia trachomatis tests requested and performed, questionnaires answered, and prevalences according to age group. The prevalence of C trachomatis infection was 6.0% (95% CI: 3.6% to 8.4%) among male participants and 4.6% (95% CI: 2.8% to 6.4%) among female participants. *Not all providing a test answered the questionnaire.
Characteristics of participants
A total of 471 women and 275 men answered the questionnaire. The characteristic of the participants who tested themselves and filled in the questionnaire is shown in table 1. There was no statistical significance between the sexes. Not comparing sexes within strata gives a global p value of 0.694. Believing to be infected with chlamydia and having symptoms were strongest factors correlated to being infected (table 2).
Table 1 Characteristics and chlamydia prevalence of participants answering the questionnaire according to age, civil status, and sexual behaviour.
| Women | Men | p Value | |||
|---|---|---|---|---|---|
| No of women | No (%) CT+ | No of men | No (%) CT+ | ||
| Age | 0.239 | ||||
| <16 | 1 | 0 | 3 | 0 | |
| 16–19 | 73 | 5 (6.8%) | 14 | 1 (7.1%) | |
| 20–24 | 264 | 12 (4.5%) | 120 | 7 (5.8%) | |
| 25–34 | 105 | 4 (3.8%) | 120 | 6 (5.0%) | |
| 35–44 | 23 | 0 | 10 | 0 | |
| >44 | 1 | 0 | 3 | 0 | |
| Unreported | 4 | – | 5 | – | |
| Civil status | 1.00 | ||||
| Single | 279 | 14 (5.0%) | 172 | 9 (5.2%) | |
| Steady partner | 188 | 6 (3.2%) | 103 | 5 (4.9%) | |
| Unreported | 4 | 1 (25%) | – | – | |
| Sex behaviour | |||||
| No of new sexual partners in past year | 0.135 | ||||
| 0 | 5 | 0 | 6 | 0 | |
| 1 | 43 | 3 (2.1%) | 74 | 6 (8.1%) | |
| 2–4 | 243 | 14 (5.8%) | 131 | 5 (3.8%) | |
| 5+ | 78 | 3 (3.8%) | 64 | 3 (4.7%) | |
| Unreported | 102 | 1 (1.0%) | – | – | |
| Intercourse (n) without condom in the last year | 0.311 | ||||
| 0 | 259 | 9 (3.5%) | 113 | 4 (3.5%) | |
| 1 | 89 | 2 (2.2%) | 60 | 4 (6.7%) | |
| 2+ | 57 | 3 (5.3%) | 56 | 4 (7.1%) | |
| Unreported | 66 | 7 (10.6%) | 46 | 2 (4.3%) | |
| Ever infected with chlamydia | 1.00 | ||||
| No | 383 | 19 (5.0%) | 237 | 12 (5.1%) | |
| Yes | 88 | 2 (2.3%) | 38 | 2 (5.3%) | |
| Unreported | – | – | – | – | |
| All | 471 | 21 (4.5%) | 275 | 14 (5.1%) | 0.694 |
CT+, Chlamydia trachomatis positive.
Table 2 Prevalence and odds ratios of infection according to test reason for men and women who tested themselves with the help of the internet.
| Reason to test | Total No of tests | Women | Men | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of tests | Number (%) CT+ | Unadjusted OR (95% CI) | p Value | Adjusted OR (95% CI)† | p Value | No of tests | Number (%) CT+ | Unadjusted OR (95% CI) | p Value | Adjusted OR (95% CI)† | p Value | ||
| Believe to be infected | |||||||||||||
| Yes | 130 | 78 | 4 (5.1%) | 1.20 (0.40 to 3.65) | 0.754 | 1.09 (0.34 to 3.42) | 0.889 | 52 | 9 (17.3%) | 9.13 (2.92 to 28.6) | 0.000 | 9.10 (2.80 to 29.5) | 0.000 |
| No | 616 | 393 | 17 (4.3%) | referent | Referent | 223 | 5 (2.2%) | referent | referent | ||||
| Symptoms | |||||||||||||
| Yes | 150 | 115 | 9 (7.8%) | 2.40 (1.00 to 5.90) | 0.050 | 2.94 (1.17 to 7.38) | 0.022 | 35 | 6 (17.1%) | 6.00 (1.95 to 18.5) | 0.002 | 6.90 (2.18 to 22.0) | 0.001 |
| No | 596 | 356 | 12 (3.4%) | referent | referent | 240 | 8 (3.3%) | referent | Referent | ||||
| Requested by sex partner | |||||||||||||
| Yes | 91 | 32 | 0 | 0 | 0 | 59 | 3 (5.1%) | 1.00 (0.27 to 3.70) | 0.998 | 0.96 (0.23 to 4.03) | 0.953 | ||
| No | 654 | 439 | 21 (4.8%) | referent | referent | 216 | 11 (5.1%) | referent | referent | ||||
| All | 756 | 471 | 21 (4.5%) | 275 | 14 (5.1%) | ||||||||
CT+, Chlamydia trachomatis positive; OR, odds ratio; CI, confidence interval.
†Adjusted for age and civil status.
Characteristics of non‐submitters
Less than 65% of the ordered test packages were returned (906/1450). Ordering but not submitting increased with decreased age. There were no multiple orders from individuals less than 16 years old or from individuals older than 44 years. Among 16–19 year olds there were eight multiple orders, among 20–24 year old 82 multiple orders, among 25–34 year old 36 multiple orders, and among 35–44 year old 11 multiple orders.
Discussion
In Sweden regular chlamydia testing is done at healthcare centres, STI clinics or youth health centres. Most of the young and sexually active visitors are women. In Sweden only 20–25% of the chlamydia tests are taken by men.10 Infected men are usually found through contact tracing or if symptomatic. In a previous study using the internet for C trachomatis screening we reached 39% of the male population aged 22 years.11
In this study we evaluated a new method simplifying C trachomatis testing and increasing its accessibility by offering participants to make their own risk assessment and confidentially order from home a chlamydia test and its result on the internet.
Strength and limitations
The methodological and design strength is that it is population based. With the help of the national registration an accurate denominator for the population size is known. The method allows requests and uptake to be calculated enabling a geographic, age, and sex comparison. The design also works preventively by educating website visitors about chlamydia.
The methodological and design weakness is that the number of infections is small so risk factor analysis is limited. A further limitation is that participation was not assessed according to social class. Even though in Sweden over 80% of the population aged 16–74 years have internet access at home12 we do not know if this strategy causes a health selection.
Comparison with other studies
Internationally, our participation rates are substantially lower than population based systematic postal screening such as the Danish in‐home sampling (women 30%, men 25%),13 the UK ClaSS population based studies (women 38%, men 28%),2 and the national population based study in the Netherlands (women 48%, men 33%).14 However, with a limited campaign, over 3% of all the females aged 20–24 in our study participated, which is good in comparison with a Danish study where 0.8% of the women aged 20–23 tested themselves for chlamydia after a large structured information campaign.15
The proportion of male tests returned (men 40%, women 60%) is higher than in opportunistic screening programmes4 (which reflect the health service use), but is comparable with previous population based screening efforts.2,13,14
The strength of this method was the participants' prevalence of infection. In the ages 16–24 years the female prevalence exceeded 5% and the male prevalence exceeded 8%. This compares favourably with a previous population screening, where female prevalence ranged from 2.3% to 8.0% and male prevalence from 1.5% to 5.9%.2,13,14 Our participants' prevalence is higher compared to a previous population based screening in the same region, achieving a 1% prevalence11 but lower than current regular testing in Sweden where 5% of the females and over 13% of the males are infected with chlamydia.10 The high male prevalence in the regular testing is caused by the fact that almost half (44%) of the men in Sweden are tested as a result of partner tracing.10 Increasing the accessibility and simplifying chlamydia testing gives increased opportunities for people at risk to be tested.
A weakness of this method was that it only tests for C trachomatis and clinical consultations are only done with infected individuals, which misses important preventive discussion opportunities. A limitation was that participation was low in the age group below 20 years, which is an important age group since it has recently been shown to have the largest increase in the number of chlamydia infections in Sweden.10 A further limitation was that more than one third of the ordered testing packages in the study were never returned with urine samples. This was more common among the younger age groups. The fact that it takes an average of 3 weeks from ordering to submitting indicates that people may keep their tests for future use but there is also the possibility that, especially among the young, some participants sent joke testing packages to each other that were never used. This non‐testing problem has been identified elsewhere, where 67% of the downloaded syphilis tests were never performed during an online syphilis testing study.16 Whatever the reason for not using the test packages, the non‐used packages are still fewer in comparison to systemic postal screening.2
Meaning of the study
Self risk assessment improves the chance of finding positive chlamydia test results, especially among men, if an accessible testing method is offered. In this study men who believed they had chlamydia were at a higher risk of being infected with C trachomatis. Having symptoms was associated with a higher chance of being infected in both men and women. The internet combined with a home sampling strategy has given the population a more convenient access to chlamydia testing. Future applications of this method may benefit from using a questionnaire containing questions regarding sexual risk behaviour and symptoms before ordering. Interested individuals may then perform their own risk assessment on the internet. Individuals with behaviours and symptoms associated with an increased risk of having an STI would then be recommended to order a test. Individuals with low risk behaviour may still order a home test and, as a preventive measure, individuals will learn what behaviours and symptoms are associated with STIs. The method could also benefit from sending out reminder letters to individuals who ordered a test but did not return it, to increase the participation rate.
In a screening programme an internet based method, as described here, could be a valuable adjunct to opportunistic screening by reaching and educating people not using the healthcare facilities. People tested during healthcare visits can also be encouraged to use the internet for regular testing.
Key messages
This study show that home based urine testing using the internet for both ordering and obtaining test results is feasible
Using the internet for chlamydia testing could be a valuable adjunct to other recruitment methods
Using the internet for chlamydia testing had a good geographical coverage and people aged 20–24 years were the most common users
Conclusion
Simplifying and increasing the accessibility of chlamydia testing by means of internet and home sampling proved feasible. The geographic coverage was good, participation rate highest among young people, and the chlamydia prevalence among men was 6.0% (95% CI: 3.6% to 8.4%) and among females 4.6 % (95% CI: 2.8% to 6.4%). Almost as many men as women tested themselves. Believing themselves to be infected and having symptoms were the strongest determinants of infection.
Success in controlling chlamydia transmission is likely to depend on achieving consistent and regular coverage of testing and partner notification in both women and men. This new method that encourages young people to be tested may be used as an adjunct to regular recruitment, but further research is needed to evaluate the internet based chlamydia testing upon sexual health inequalities.
Acknowledgements
This study was supported by grants from the Swedish National Institute for Public Health and the medical council of Västerbotten. We are also grateful for help with laboratory problems to Dr Ann‐Christine Edman, the county medical officer of Communicable Disease Control and Dr Jens Boman; and for computer assistance to Emil Edeholt.
Contributors
DPN was the project leader, involved in the conception, design, and organisation of the study, interpretation of the data, and writing the first draft of the report; RBK was involved in the conception, design, and organisation of the study, interpretation of the data, and drafting the final report.
Abbreviations
PCR - polymerase chain reaction
STI - sexually transmitted infections
Footnotes
Competing interests: The authors have no competing interests.
References
- 1.Low N. Current status of chlamydia screening in Europe. Eurosurveillance 20048(5) [Google Scholar]
- 2.Macleod J, Salisbury C, Low N.et al Coverage and uptake of systematic postal screening for genital Chlamydia trachomatis and prevalence of infection in the United Kingdom general population: cross sectional study. BMJ 2005330940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Low N, McCarthy A, Macleod J.et al The chlamydia screening studies: rationale and design. Sex Transm Infect 200480342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LaMontagne D S, Fenton K A, Randall S.et al Establishing the National Chlamydia Screening Programme in England: results from the first full year of screening. Sex Transm Infect 200480335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Low N, Egger M. What should we do about screening for genital chlamydia? Int J Epidemiol 200231891–893. [DOI] [PubMed] [Google Scholar]
- 6.Miller W C. Screening for chlamydial infection: are we doing enough? Lancet 2005365456–458. [DOI] [PubMed] [Google Scholar]
- 7.Fenton K A, Korovessis C, Johnson A M.et al Sexual behaviour in Britain: reported sexually transmitted infections and prevalent genital Chlamydia trachomatis infection. Lancet 20013581851–1854. [DOI] [PubMed] [Google Scholar]
- 8.Lewin B, Fugl‐Meyer K, Helmius G.et alSex in Sweden—on the Swedish sexual life. Stockholm: The National Institute of Public Health, 2000
- 9.Lundberg O, Diderichsen F, Yngwe M A. Changing health inequalities in a changing society? Sweden in the mid‐1980s and mid‐1990s. Scand J Public Health Suppl 20015531–39. [PubMed] [Google Scholar]
- 10.SIIDC Statistics on sexually transmitted infections in Sweden. Available at www.smittskyddsinstitutet.se [Swedish English summaries]. Stockholm: Swedish Institute for Infectious Disease Control, 2005
- 11.Novak D P, Edman A C, Jonsson M.et al The internet, a simple and convenient tool in Chlamydia trachomatis screening of young people. Euro Surveill 20038171–176. [DOI] [PubMed] [Google Scholar]
- 12.Hintze A, Skatt P.Use of computer and the internet by private persons in 2004. Stockholm: Statistics Sweden, 2004
- 13.Andersen B, Olesen F, Moller J K.et al Population‐based strategies for outreach screening of urogenital Chlamydia trachomatis infections: a randomized, controlled trial. J Infect Dis 2002185252–258. [DOI] [PubMed] [Google Scholar]
- 14.van Bergen J, Gotz H M, Richardus J H.et al Prevalence of urogenital Chlamydia trachomatis increases significantly with level of urbanisation and suggests targeted screening approaches: results from the first national population based study in the Netherlands. Sex Transm Infect 20058117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersen B, Ostergaard L, Moller J K.et al Effectiveness of a mass media campaign to recruit young adults for testing of Chlamydia trachomatis by use of home obtained and mailed samples. Sex Transm Infect 200177416–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levine D K, Scott K C, Klausner J D. Online syphilis testing—confidential and convenient. Sex Transm Dis 200532139–141. [DOI] [PubMed] [Google Scholar]