Abstract
Objective
Assessment of HIV prevalence and associated risk behaviours among female commercial sex workers (FCSW) across major cities in South America.
Methods
Seroepidemiological, cross sectional studies of 13 600 FCSW were conducted in nine countries of South America during the years 1999–2002. Participants were recruited in brothels, massage parlours, hotels, and streets where anonymous questionnaires and blood samples were collected. HIV infection was determined by enzyme linked immunosorbent assay (ELISA) screening and western blot confirmatory tests.
Results
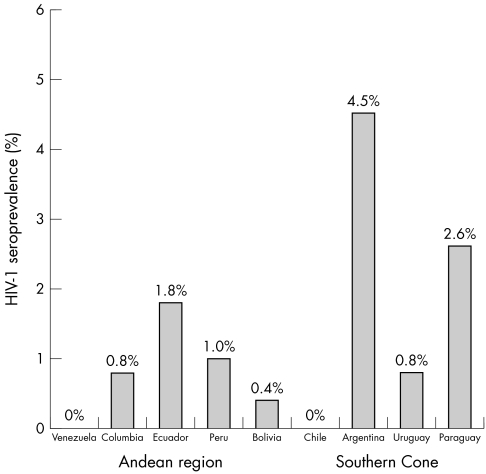
The overall HIV seroprevalence was 1.2% (range 0.0%–4.5%). The highest HIV seroprevalences were reported in Argentina (4.5%) and Paraguay (2.6%); no HIV infected FCSW were detected in Venezuela and Chile. Consistent predictors of HIV seropositivity were: (1) a previous history of sexually transmitted infections (STI, AORs = 3.8–8.3), and (2) 10 years or more in commercial sex work (AORs = 2.2–24.8). In addition, multiple (⩾3) sexual contacts (AOR = 5.0), sex with foreigners (AOR = 6.9), use of illegal drugs (AOR = 3.2), and marijuana use (AOR = 8.2) were associated with HIV seropositivity in Southern Cone countries.
Conclusions
Consistently low HIV seroprevalences were detected among FCSW in South America, particularly in the Andean region. Predictors of HIV infection across the continent were STI and length of commercial sex work; however, use of illegal drugs, especially marijuana, and sexual contacts with foreigners were also found to be associated risk factors in the Southern Cone region. Interventions for the control of HIV and other STI need to be region and country specific; drug use appears to have an ever increasing role in the spread of HIV among heterosexually active populations.
Keywords: HIV, prevalence, risk factors, South America, female, sex workers
The burden of infection with human immunodeficiency virus type 1 (HIV‐1) continues to increase worldwide.1 HIV prevalence varies widely among female commercial sex workers (FCSW) in different regions of the world.2 Higher prevalences have been reported in sub‐Saharan Africa (0.2% to 60.5%), followed by south and South East Asia (0.0% to 26.0%).3 In Latin America and the Caribbean, where data are available, overall rates are lower than in other regions (0.0% to 14.0%),3,4 and HIV transmission appears to prevail among other high risk groups such as men who have sex with men (MSM) and injecting drug users (IDU).
Sexually transmitted infections (STI) are widely recognised as major risk factors for HIV acquisition because they share the same modes of transmission, and because ulcerogenic STIs such as syphilis and herpes increase HIV associated susceptibility and infectiousness.5 Heterosexual promiscuity, unsafe sexual behaviour (that is, lack of consistent condom use) and increased number of clients represent important risk factors for FCSW. Reductions in HIV prevalence among FCSW may serve as an indicator of the success of early diagnosis, treatment, and/or preventive interventions for STI in heterosexually active populations.6,7
Information about HIV among FCSW in most South American countries is limited; recent UNAIDS estimates (2004) and a few studies have been published.8,9,10,11 The data presented in this report represent a summary of several cross sectional studies conducted among thousands of FCSW and complements a similar analysis among MSM populations in the same region.12 To our knowledge, this study represents the largest HIV prevalence database among FCSW in Latin America. Country specific assessments of HIV prevalence and determination of potential risk factors among FCSW in the region, are presented with particular attention paid to perceived differences in risk behaviour patterns between the countries of the Andean region (Venezuela, Colombia, Ecuador, Peru, and Bolivia) and those of the Southern Cone (Chile, Argentina, Uruguay, and Paraguay).
Methods
Study population
Seroepidemiological, cross sectional studies were performed among various FCSW high risk groups during the years 1999–2002. These studies were conducted in 32 cities in nine countries of South America. Sites included Isla Margarita in Venezuela; Bogota in Colombia; Quito and Guayaquil in Ecuador; Lima, Iquitos, Pucallpa, Trujillo, Arequipa, Tacna, and Sullana in Peru; Santa Cruz in Bolivia; Santiago in Chile; Buenos Aires, and seven other cities in Argentina; Montevideo and five border cities with Brazil in Uruguay; and Asuncion and four other cities in Paraguay.
Agreements were established with the local country's ministry of health (MoH) national AIDS control programmes and AIDS supporting non‐governmental organisations (NGO) in advance and approval for implementation of studies was obtained from the Pan American Health Organization (PAHO), the US Naval Medical Research Center Detachment Lima, Peru (NMRCD‐Lima), the Walter Reed Army Institute of Research (WRAIR), and the Henry M Jackson Foundation (HJF), Rockville, MD, as described elsewhere.12,13 Central funding, laboratory reference, and statistical analysis support was provided by the US Military HIV Research Program at the WRAIR. Study protocols were approved by human use, ethics, and institutional review boards in each country as well as by the US Naval Medical Research Center (NMRC), Silver Spring, MD, USA.
Participants were at least 18 years of age, agreed to participate in the study and were enrolled after providing written informed consent in accordance with human use study guidelines. FCSW participants were contacted at their working locations such as brothels, saunas, massage houses, parks, and streets. No records of potential (that is, subjects approached) versus actual participants were collected in these studies, thus, no assessment of the completeness or representativeness of FCSW participation could be achieved. Access to FCSW populations is often hard and limited in scope, even under the best of circumstances.
Baseline demographic and epidemiologic data that included information regarding sexual and other risk behaviour information were collected by trained staff with experience in HIV and STI prevention by use of a standardised questionnaire. Participants were queried regarding lifetime length of commercial sex work (CSW), numbers of sexual contacts per week, sexual contact with foreigners, frequency of condom use with clients, as well as history, length, and types of illegal drugs used. A venous blood sample was collected from each participant for HIV antibody testing as detailed below and as described previously.12,13 Participants received pretest and post‐test counselling, and were referred to appropriate medical and social services for follow up in accordance with local MoH guidelines.
Laboratory testing
Details of laboratory testing have been described in detail elsewhere.13,14,15 Briefly, serum samples were tested for antibodies against HIV‐1 by enzyme linked immunosorbent assay (ELISA) screening (Bio‐Rad, Hercules, CA, USA), and repeatedly reactive samples were subjected to western blot confirmation using FDA approved testing kits (Calypte Biomedical, Alameda, CA, USA).
Statistical analysis
HIV‐1 seroprevalences were expressed as percentages. χ2 and Fisher's exact tests were utilised to compare differences in categorical variables. Mann‐Whitney U and Kruskal‐Wallis H, non‐parametric tests were used to compare differences between continuous variables. Variables available in this analysis included age in years, number of sexual contacts per week (categorised as 0–2, and three or more), condom use, previous STI history, sexual contact with foreigners, past use of drugs (marijuana, cocaine, and/or heroin), alcohol use, and history of previous blood transfusions. Analysis of demographic and risk factor data was performed for FCSW from all but two countries (Venezuela and Chile).
Regional aggregate analysis was performed for two regions of South America, the Andean region and the Southern Cone region. To evaluate the association with HIV infection, odds ratios (ORs) and adjusted ORs (AORs) controlling for age were estimated for each region. Participants were grouped into strata, or risk sets, defined by the country in which they were enrolled. This matching strategy holds constant the potentially confounding effects of unmeasured characteristics within a single country.16 To correct for sparse and unbalanced data sets, the ORs and AORs were estimated based on fully conditional exact inference in univariate and multiple logistic regression analyses,17 as well as associated 95% confidence intervals (95% CI). All reported probability (p) values were two sided, and values of <0.05 were considered to be statistically significant. All analyses were carried out applying LogXact v.5.0 (Cytel Software Corporation, Cambridge, MA, USA) and Stata v 8.0 (Stata Corporation, College Station, TX, USA).
Results
A total of 13 600 FCSW participants were enrolled. Of these, 10 989 (80.8%) were enrolled in the Andean region and 2611 (19.2%) in Southern Cone countries. Given the high level of involvement by MoH and NGOs in pre‐existing collaborations with FCSW based studies in the past, Peru accounted for 8304 (75.6%) participants in the Andean region. The number of participants was equally distributed among countries of the Southern Cone. The median (mean) age of participants was 26 (28.3) years. Subjects from Argentina were found to be older (34.1 years) than from other countries (27.9 years, p<0.001). Most (59%) study participants were single and 13% were married. Thirty one per cent reported ever having sexual intercourse with foreign clients, and only six of the participants reported having ever used injecting drugs. The median (mean) weekly number of sexual contacts was four (13) and 5.6% reported at least one previous STI. Only 36% of the participants reported consistent use of condoms during their sexual contacts.
HIV seroprevalence
HIV seroprevalences by country and region are shown in table 1. The overall HIV seroprevalence was 1.2% (95% CI = 1.0% to 1.4%; range 0.0%–4.5%). Argentina (4.5%) and Paraguay (2.6%), two countries of the Southern Cone region reported significantly higher HIV seroprevalences (fig 1). In the Andean region, Ecuador (1.8%) and Peru (1.0%) reported the highest HIV seroprevalences. No HIV infected FCSW were detected among 652 and 626 participants in Venezuela and Chile, respectively. In addition, HIV prevalence was also higher, on average, in the Southern Cone than in the Andean region (2.0% v 1.0%, p<0.001). HIV infected subjects were found to be older (mean, 29.6 years) than HIV negative ones (mean 27.3 years) only in the country of Peru (p = 0.017). HIV seroprevalences by country and age groups (in years) among FCSW participants are shown in table 2.
Table 1 HIV‐1 seroprevalences among FCSW from nine countries in South America, 1999–2002.
| Region and country | Period | % | (n/No) |
|---|---|---|---|
| Total | 1999–2002 | 1.2 | (164/13 600) |
| Andean | 1.0 | (112/10 989) | |
| Venezuela | 2002 | 0.0 | (0/652) |
| Colombia | 2001–2 | 0.8 | (4/514) |
| Ecuador | 2000–1 | 1.8 | (23/1247) |
| Peru | 1999–2000 | 1.0 | (84/8304) |
| Bolivia | 2001–2 | 0.4 | (1/272) |
| Southern Cone | 2.0 | (52/2611) | |
| Chile | 2000 | 0.0 | (0/626) |
| Argentina | 2000–1 | 4.5 | (28/626) |
| Uruguay | 2000–2 | 0.8 | (5/616) |
| Paraguay | 2002 | 2.6 | (19/743) |
HIV‐1, human immunodeficiency virus type 1; FCSW, female commercial sex workers.
In parentheses is number of HIV‐1 positive (n)/total number participants tested (No).
Figure 1 HIV‐1 seroprevalences by region and country, South America, 1999–2002.
Table 2 HIV‐1 seroprevalences by country and age groups (in years) among FCSW participants from nine countries in South America, 1999–2002.
| Region | Aged 18–25 | Aged ⩾26 | Age | ||||
|---|---|---|---|---|---|---|---|
| % | (n/No)* | % | (n/No)* | p value | Mean | (SE) | |
| Andean | |||||||
| Colombia | 0.5 | (1/186) | 0.9 | (3/318) | 0.998 | 30.8 | (0.4) |
| Ecuador | 1.9 | (11/590) | 1.7 | (11/650) | 0.833 | 28.0 | (0.2) |
| Peru | 0.8 | (34/4114) | 1.1 | (45/3946) | 0.175 | 27.3 | (0.01) |
| Bolivia | 1.0 | (1/103) | 0.0 | (0/169) | 0.379 | 29.9 | (0.5) |
| Southern Cone | |||||||
| Argentina | 4.5 | (6/134) | 2.8 | (13/464) | 0.399 | 34.1 | (0.4) |
| Uruguay | 0.5 | (1/209) | 1.0 | (4/406) | 0.666 | 30.7 | (0.4) |
| Paraguay | 5.4 | (13/241) | 3.6 | (6/167) | 0.479 | 25.7 | (0.3) |
| Chile | 0.0 | (0/176) | 0.0 | (0/450) | NA | 32.1 | (0.4) |
HIV‐1, human immunodeficiency virus type 1; FCSW, female commercial sex workers; SE, standard error.
*Number of HIV‐1 positive (n)/total number participants tested (No). Denominator totals varied slightly owing to missing data.
In the Andean region, HIV seroprevalence was higher with an STI history (p<0.001) and length of CSW (10 years or more, p = 0.001). In the Southern Cone region, significantly higher HIV seroprevalences were seen with multiple (⩾3) sexual contacts (p<0.001), a previous STI history (p<0.001), any reported drug use (p = 0.001), marijuana consumption (p = 0.004) and alcohol consumption (p<0.05). HIV seroprevalences were not found to be different with other variables such as marital status, condom use, sexual contact with foreigners, use of heroine or cocaine, alcohol consumption, or previous blood transfusions (table 3).
Table 3 HIV‐1 seroprevalences by risk factor and region among FCSW participants in South America, 1999–2002.
| Risk factor | Andean | Southern Cone | ||
|---|---|---|---|---|
| % | (n/No)† | % | (n/No) | |
| Marital status | ||||
| Married, widow, divorced, others | 1.3 | (42/3320) | 1.5 | (13/850) |
| Single | 0.9 | (65/6916) | 2.8 | (20/702) |
| Sexual contacts per week | ||||
| None, one or two | 1.0 | (29/2985) | 1.2 | (20/1736) |
| Three or more | 1.2 | (77/6622) | 3.8* | (32/851) |
| Previous STI history | ||||
| No | 1.0 | (92/9453) | 1.2 | (30/2406) |
| Yes | 3.0* | (16/534) | 6.5* | (12/185) |
| Condom use | ||||
| Sometimes, rarely, never | 1.2 | (78/6714) | 2.5 | (30/1188) |
| Always | 1.0 | (32/3302) | 1.6 | (22/1358) |
| Sexual contact with foreigners | ||||
| No | 1.2 | (82/6818) | 1.8 | (32/1770) |
| Yes | 0.8 | (27/3181) | 2.2 | (18/821) |
| Time in CSW | ||||
| Less than 10 years | 0.7 | (30/4271) | 1.7 | (22/1332) |
| 10 years or more | 1.4* | (81/5863) | 2.3 | (29/1273) |
| Use of any illegal drugs | ||||
| No | 1.1 | (104/9673) | 1.1 | (20/1746) |
| Yes | 1.8 | (3/164) | 6.3* | (7/111) |
| Use of marijuana | ||||
| No | 1.1 | (110/10220) | 1.8 | (47/2558) |
| Yes | 1.0 | (1/101) | 9.4* | (5/53) |
| Use of cocaine | ||||
| No | 1.1 | (110/10245) | 1.9 | (49/2545) |
| Yes | 1.5 | (1/68) | 4.5 | (3/66) |
| Use of alcohol | ||||
| No | 1.0 | (91/8913) | 1.6 | (22/1347) |
| Yes | 1.3 | (17/1354) | 4.4* | (19/428) |
| Blood transfusion history | ||||
| No | 1.0 | (107/10099) | 1.9 | (47/2447) |
| Yes | 2.3 | (5/219) | 3.1 | (5/160) |
HIV‐1, human immunodeficiency virus type 1; FCSW, female commercial sex workers; STI, sexually transmitted infections; CSW, commercial sex work.
†Number of HIV‐1 positive (n)/total number participants tested (No). Denominator totals varied owing to missing data.
*p<0.05 by χ2 or Fisher's exact test.
Risk factor analysis
Logistic regression analysis of risk factors for HIV infection in the Andean region is shown in table 4. In univariate logistic regression analysis, previous STI history (OR = 4.43) and greater length (10 years or more) in CSW (OR = 1.94) were found to be associated. These same risk factors remained significantly associated after adjusting for age in the multiple logistic regression analysis (AORs of 3.77 and 2.19, respectively). By comparison, multiple (⩾3) sexual contacts (AOR = 5.03), previous STI history (AOR = 8.27), 10 years or more in CSW (AOR = 24.81), sexual contact with foreigners (AOR = 6.88), use of any illegal drugs (AOR = 3.15), and marijuana use (AOR = 8.18) were found to be associated with HIV seropositivity in Southern Cone region countries (table 5). We also noted that the magnitude of the associations for sexual risk factors was consistently higher than the associations for illegal drug use behaviours.
Table 4 Logistic regression analysis of risk factors for HIV‐1 infection among FCSW in the Andean region, 1999–2002.
| Risk factor | OR | (95% CI) | p Value | AOR | (95% CI) | p Value |
|---|---|---|---|---|---|---|
| Single marital status (others) | 0.79 | (0.52 to 1.22) | 0.306 | 0.88 | (0.59 to 1.32) | 0.528 |
| Sexual contacts per week (⩽two) | 1.19 | (0.77 to 1.91) | 0.486 | 1.26 | (0.79 to 1.99) | 0.330 |
| Previous STI history (no) | 4.43 | (1.64 to 11.28) | 0.002 | 3.77 | (1.59 to 8.94) | 0.003 |
| Time in CSW (<10 years) | 1.94 | (1.25 to 3.06) | 0.002 | 2.19 | (1.36 to 3.52) | 0.001 |
| Consistent condom use (sometimes or never) | 1.31 | (0.83 to 2.11) | 0.279 | 1.24 | (0.79 to 1.94) | 0.353 |
| Sexual contact with foreigners (no) | 0.68 | (0.42 to 1.07) | 0.100 | 0.76 | (0.49 to 1.19) | 0.227 |
| Use of any illegal drugs (no) | 1.55 | (0.17 to 6.63) | 0.789 | 1.60 | (0.37 to 6.99) | 0.533 |
| Use of marijuana (no) | 0.81 | (0.02 to 5.11) | 0.998 | 0.92 | (0.12 to 6.88) | 0.933 |
| Use of cocaine (no) | 1.63 | (0.04 to 10.97) | 0.956 | 1.68 | (0.22 to 12.94) | 0.618 |
| Use of alcohol (no) | 1.12 | (0.44 to 3.24) | 0.998 | 1.21 | (0.50 to 2.97) | 0.671 |
| Blood transfusion history (no) | 1.57 | (0.45 to 4.43) | 0.516 | 1.54 | (0.56 to 4.20) | 0.402 |
HIV‐1, human immunodeficiency virus type 1; FCSW, female commercial sex workers; STI, sexually transmitted infections; CSW, commercial sex work; OR, odds ratio; AOR, odds ratio adjusted by age in years; 95% CI, 95% confidence interval; categories in parentheses describe the reference group for odds calculation.
Statistically significant variables are shown in bold.
Table 5 Logistic regression analysis of risk factors for HIV‐1 infection among FCSW in the Southern Cone, 1999–2002.
| Risk factor | OR | (95% CI) | p Value | AOR | (95% CI) | p Value |
|---|---|---|---|---|---|---|
| Single marital status (others) | 0.74 | (0.21 to 2.36) | 0.757 | 0.80 | (0.28 to 2.31) | 0.685 |
| Sexual contacts per week (⩽two) | 9.35 | (4.00 to 23.15) | <0.001 | 5.03 | (2.51 to 10.05) | <0.001 |
| Previous STI history (no) | 10.04 | (4.31 to 22.43) | <0.001 | 8.27 | (3.94 to 17.33) | <0.001 |
| Time as CSW (<10 years) | 6.53 | (2.75 to 16.46) | <0.001 | 24.81 | (9.28 to 66.34) | <0.001 |
| Consistent condom use (sometimes or never) | 1.57 | (0.90 to 2.74) | 0.110 | 1.56 | (0.85 to 2.87) | 0.154 |
| Sexual contact with foreigners (no) | 4.46 | (2.07 to 9.41) | <0.001 | 6.88 | (3.24 to 14.58) | <0.001 |
| Use of any illegal drugs (no) | 2.90 | (0.69 to 9.26) | 0.145 | 3.15 | (1.02 to 9.78) | 0.046 |
| Use of marijuana (no) | 6.12 | (1.71 to 17.90) | 0.006 | 8.18 | (2.85 to 23.47) | <0.001 |
| Use of cocaine (no) | 2.34 | (0.44 to 8.15) | 0.328 | 3.32 | (0.94 to 11.66) | 0.061 |
| Use of alcohol (no) | 3.58 | (0.32 to 39.57) | 0.299 | 3.51 | (0.32 to 38.12) | 0.303 |
| Blood transfusion history (no) | 1.50 | (0.44 to 4.08) | 0.564 | 2.02 | (0.73 to 5.61) | 0.179 |
HIV‐1, human immunodeficiency virus type 1; FCSW, female commercial sex workers; STI, sexually transmitted infections; CSW, commercial sex work; OR, odds ratio; AOR, odds ratio adjusted by age in years; 95% CI, 95% confidence interval; categories in parentheses describe the reference group for odds calculation.
Statistically significant variables are shown in bold.
Discussion
This study provides insight into some regional characteristics of the HIV epidemic in South America where few studies have been published. Our findings suggest a low overall HIV‐1 seroprevalence of 1.2% (range 0.0% to 4.5%) for nine countries surveyed in South America, with significantly higher HIV seroprevalences in Argentina (4.5%) and Paraguay (2.6%). Previously published, population based, HIV seroprevalence studies among FCSW high risk groups have also reported similar low prevalences in other regions of the world, including Australia (0.2%) in 2001,18 Japan (1%–3%) in 1984–2000,19 and the Philippines (1%–2%) in 2003.20
The absence of HIV infection among FCSW in Venezuela and Chile confirms the very low HIV seroprevalences previously reported in these countries.11,21 In addition, the low HIV seroprevalences reported in Peru (1.0%), Colombia (0.8%), and Bolivia (0.4%) may be explained in part by existing, MoH mandated, periodic check ups of sex workers on a routine basis (at least every 3 months). A cross sectional study performed in La Paz among FCSW in 2002, for example, reported a prevalence of 0.2%.22 By contrast, Ecuador continues to report the highest HIV seroprevalence (1.8%) in the Andean region with higher seroprevalences in coastal areas such as Guayaquil and Esmeraldas.23 In Colombia and Peru, where the HIV epidemic appears to be concentrated among high risk groups of MSM, trends in HIV seroprevalences among FCSW appear to be stable at low levels. Previously published prevalences have been for Colombia (0.9% in 1994) and Peru (1.6% in 1998).3
Our data suggest consistently low HIV seroprevalences among FCSW in South America, particularly in the Andean region. This may be due in part to the low STI rates, as well as by a low contact rate between gay/bisexual men and FCSW, in this region. Future studies need to be conducted that address these factors, however, since we were not able to collect sufficient data regarding STI predisposing and gay/bisexual sexual risk practices.
In Argentina, more than 65% of HIV infections are concentrated in the metropolitan Buenos Aires area.3,24 Our results suggest a possible increase in HIV prevalence in from 2.6% in 199324 to 4.5% in 2000–1. Increases in HIV prevalences have also been noted to occur in Paraguay, from a low of 0.1% in 19873 to 2.6% in 2002, and in Uruguay from a low in 1997 of 0.5%3 to a slight increase of 0.8% in 2000–2 in our studies.
Different risk factors have been associated with HIV infection in the region. However, above all other factors, a previous history of STI and greater length (10 years or more) in CSW appear to constitute two common risk factors associated with HIV infection among FCSW across the continent. Elevated STI rates have been associated with elevated HIV prevalences in many countries of the world.25 This association between STI and HIV acquisition may be accounted for by increased transmissibility and/or increased susceptibility to HIV,4,5,6,26 as well as by a common association with types and numbers of sexual partnerships.27 The relatively important associations between STI and HIV seropositivity identified in this study highlights a need for renewed efforts in STI prevention28 and understanding predisposing behavioural and sexual health risk practices in order to try to stem the tide of the HIV epidemic among FCSW communities in the region.
We also noted distinct geographic differences in the patterns of drug use and sexual contact with foreigners, particularly in the Southern Cone. We believe that FCSW in the Southern Cone sustain more frequent and varied types of sexual contact across borders in this region. The relatively short geographic distances between major cities and the accessibility for travel between countries may contribute to this. The associations with non‐injecting drug use, particularly use of marijuana and cocaine, was worrying and points to a need for public health authorities to address as part of the evaluation and implementation of harm reduction programmes.
We recognise that these cross sectional studies have some inherent limitations because of potential non‐representativeness of the study population, as well as socioeconomic factors which were not assessed in areas where low socioeconomic status represents a risk factor for HIV and STI.29 It is well know that cross sectional studies make it impossible to determine the direction of the observed associations, and the non‐representativeness of the sample population may narrow the external validity of the findings, as well as the estimate of the mean effect (prevalence) may be rather imprecise, given the relatively small sample size. Therefore, the findings of this study may have systematic errors and not accurately represent the true situation among FCSW high risk groups across the region. Despite these limitations, it is noteworthy to mention that all study participants were asymptomatic at the time of enrolment. Thus, we feel strongly that we could estimate actual HIV seroprevalences and associated risk factors in a reliable manner, without a major possibility of including previously documented HIV infected individuals in our study.
Key messages
Seroepidemiological surveys of 13 600 FCSW were conducted in nine countries of South America during the years 1999–2002
The overall HIV‐1 seroprevalence was 1.2% (range 0.0%–4.5%). High seroprevalences were noted in Argentina (4.5%) and Paraguay (2.6%)
History of previous STI, 10 years or more in CSW, sexual contact with foreigners, and drug use were associated with increase risk of HIV‐1 infection among FCSW
In conclusion, we found that predictors of HIV infection across the continent were STI and length of CSW; however, use of illegal drugs, especially marijuana, and sexual contacts with foreigners were also found to be associated risk factors in the Southern Cone region. Interventions for the control of HIV and other STI need to be region and country specific. Our data also strongly suggest that illegal drug use appears to have an ever increasing role in the spread of HIV among heterosexually active populations. Effective, public health oriented, local education and intervention programmes must be tailored to this vulnerable portion of the population according to local prevailing sexual and social behavioural risk patterns, as well as continued surveillance among FCSW and their clients to monitor trends in HIV prevalences in these populations in the region.
Acknowledgments
We would like to acknowledge the assistance provided by Gloria Chauca, Gladys Carrion, Maria Ester Gamero, and Merly Sovero in sample processing; Pamela Limo, Claudia Oroya and Ruth Centeno in data management; Gloria Talledo in administrative assistance at NMRCD Lima, and Sebastian A for his technical assistance. We also appreciate the assistance of Steve Harvey.
Contributions
CTB and JLS conceived the idea for this manuscript, generated the initial working draft, conducted statistical analyses of the data, and coordinated collaborators' responses. LS, JS, and PC participated in the Peruvian study design, implementation, and data collection, as well as coordinated study protocol approval in Peru, and commented on initial manuscript draft and reviewer comments. CG, CM, MVdeB, NA, MMA, MW, ER, RC, MS, CA, AM, NV, and AG participated in the design, implementation, and data collection in their respective countries in South America; JLS, SMM, VAL‐T, NM, R KL, and JKC participated in the design, approval, and implementation of all study protocols. All authors listed were involved in the interpretation of the results of the different studies, as well as in the review and approval of the final version of this manuscript.
Abbreviations
AORs - adjusted ORs
ELISA - enzyme linked immunosorbent assay
FCSW - female commercial sex workers
IDU - injecting drug users
MSM - men who have sex with men
ORs - odds ratios
STI - sexually transmitted infections
Footnotes
Financial support: This study was supported by the US Military HIV Research Program at the Walter Reed Army Institute of Research, and by the US Naval Medical Research Center, Silver Spring, MD, Work Unit Number No 62787A S17 H B0002.
Disclaimer: The opinions and assertions expressed herein are those of the authors and do not necessarily reflect the official position of the US Departments of the Army or Navy, the US Department of Defense, the US Government, the Henry M Jackson Foundation for the Advancement of Military Medicine, Inc, or any other organization listed.
Human use statement: The study protocol was approved by the Naval Medical Research Center's Institutional Review Board under Protocol # NMRCD.2000.0002 (DoD 31523), Protocol # NMRCD.1999.0002 (DoD 30590), Protocol # (DoD 30583), Protocol # NMRCD.1999.0001 (DoD 30587), Protocol # NMRCD.2002.0006 (DoD 31590), Protocol # NMRCD.1998.0001 (DoD 30578), and Protocol (DoD 31513) in compliance with all federal regulations governing the protection of human subjects.
References
- 1.Grant A D, De Cock K M. The growing challenge of HIV/AIDS in developing countries. Br Med Bull 199854369–381. [DOI] [PubMed] [Google Scholar]
- 2.McKeganey N P. Prostitution and HIV: what do we know and where might research be targeted in the future? AIDS 199481215–1226. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization, UNAIDS, June 2004. Report on the global AIDS epidemic, 4th global report, table of country‐specific HIV/AIDS estimates and data, end 2003189–207.
- 4. The global HIV and AIDS epidemic, 2001. MMWR Morb Mortal Wkly Rep 200150434–439. [PubMed] [Google Scholar]
- 5.Cohen M. Sexually transmitted diseases enhance HIV transmission: no longer a hypothesis. Lancet 1998351(suppl III)5–7. [DOI] [PubMed] [Google Scholar]
- 6.Renton A M, Whitaker L, Riddlesdell M. Heterosexual HIV transmission and STD prevalence: predictions of a theoretical model. Sex Transm Infect 199874339–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayaudo P.et al Advances in control of sexually transmitted diseases in developing countries. Lancet 1998351(suppl 3)29–32. [DOI] [PubMed] [Google Scholar]
- 8.Zapiola I, Salomone S, Alvarez A.et al HIV‐1, HIV‐2, HTLV‐I/II and STD among female prostitutes in Buenos Aires, Argentina. Eur J Epidemiol 19961227–31. [DOI] [PubMed] [Google Scholar]
- 9.Levine W C, Revollo R, Kaune V.et al Decline in sexually transmitted disease prevalence in female Bolivian sex workers: impact of an HIV prevention project. AIDS 1998121899–1906. [DOI] [PubMed] [Google Scholar]
- 10.Trujillo L, Munoz D, Gotuzzo E.et al Sexual practices and prevalence of HIV, HTLV‐I/II, and Treponema pallidum among clandestine female sex workers in Lima, Peru. Sex Transm Dis 199926115–118. [DOI] [PubMed] [Google Scholar]
- 11.Camejo M I, Mata G, Diaz M. Prevalence of hepatitis B, hepatitis C and syphilis in female sex workers in Venezuela. Rev Saude Publica 200337339–344. [DOI] [PubMed] [Google Scholar]
- 12.Bautista C T, Sanchez J L, Montano S M.et al Seroprevalences of and risk factors for HIV‐1 infection among South American men who have sex with men. Sex Transm Infect 200480498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hierholzer J, Montano S, Hoelscher M.et al Molecular epidemiology of HIV type 1 in Ecuador, Peru, Bolivia, Uruguay, and Argentina. AIDS Res Hum Retroviruses 2002181339–1350. [DOI] [PubMed] [Google Scholar]
- 14.Russi J C, Serra M, Vinoles J.et al Sexual transmission of hepatitis B virus, hepatitis C virus, and human immunodeficiency virus type 1 infections among male transvestite commercial sex workers in Montevideo, Uruguay. Am J Trop Med Hyg 200368716–720. [PubMed] [Google Scholar]
- 15.Pando M A, Maulen S, Weissenbacher M.et al High human immunodeficiency virus type 1 seroprevalence in men who have sex with men in Buenos Aires, Argentina: risk factors for infection. Int J Epidemiol 200332735–740. [DOI] [PubMed] [Google Scholar]
- 16.Hosmer D W, Lemeshow S.Applied logistic regression. 2nd ed. New York: John Wiley, 2000
- 17.Mehta C R, Patel N R. Exact logistic regression: theory and examples. Stat Med 1995142143–2160. [DOI] [PubMed] [Google Scholar]
- 18.Kaldor J, McDonald A. HIV/AIDS surveillance systems in Australia. J Acquir Immune Defic Syndr. 2003;32Suppl 1S18–S23. [DOI] [PubMed]
- 19.Kihara M, Ono‐Kihara M, Feldman M D.et al HIV/AIDS surveillance in Japan, 1984–2000. J Acquir Immune Defic Syndr. 2003;32Suppl 1S55–S62. [PubMed]
- 20.Mateo R, Jr, Sarol J N, Jr, Poblete R. HIV/AIDS in the Philippines. AIDS Educ Prev 200416(Suppl A)43–52. [DOI] [PubMed] [Google Scholar]
- 21.Medina R, Mella L, Espoz H.et al Prostitutes of the east sector of Santiago: characteristics and pathology of sexual transmission. Rev Med Chil 19891171063–1067. [PubMed] [Google Scholar]
- 22.US Agency for International Development USAID/Bolivia, April 2003. Country Profile report (available at www.usaid.gov/pop_health/aids/Countries/lac/boliviabrief.pdf, last accessed on 24 September 2004)
- 23.UNAIDS UNICEF, WHO, September 2004. Ecuador, epidemiological fact sheets on HIV/AIDS and sexually transmitted infections (available at www.who.int/hiv/pub/epidemiology/pubfacts/en/, last accessed on 24 September 2004)
- 24.UNAIDS UNICEF, WHO, September 2004. Argentina, epidemiological fact sheets on HIV/AIDS and sexually transmitted infections (available at www.who.int/hiv/pub/epidemiology/pubfacts/en/, last accessed on 24 September 2004)
- 25.Kreiss J, Carael M, Meheus A. Role of sexually transmitted diseases in transmitting human immunodeficiency virus. Genitourin Med 1988641–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fleming D T, Wasserheit J N. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect 1999753–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.May R M, Anderson R M. Heterogeneities, co‐factors and other aspects of the transmission dynamics of HIV/AIDS. Curr Topics in AIDS 1989233–67. [Google Scholar]
- 28.Ghys P D, Diallo M O, Ettiegne‐Traore V.et al Effect of interventions to control sexually transmitted disease on the incidence of HIV infection in female sex workers. AIDS 2001151421–1431. [DOI] [PubMed] [Google Scholar]
- 29.Lamptey P R. Reducing heterosexual transmission of HIV in poor countries. BMJ 2002324207–211. [DOI] [PMC free article] [PubMed] [Google Scholar]