Abstract
Objectives
To examine various models of integrated and/or one stop shop (OSS) sexual health services (including general practice, mainstream specialist services, and designated young people's services) and explore their relative strengths and weaknesses.
Methods
Literature review and interviews with key informants involved in developing the National Strategy for Sexual Health and HIV (n = 11).
Results
The paper focuses on five broad perspectives (logistics, public health, users, staff, and cost). Contraceptive and genitourinary medicine issues are closely related. However, there is no agreement about what is meant by having “integrated” services, about which services should be integrated, or where integration should happen. There are concerns that OSSs will result in over‐centralisation, to the disadvantage of stand alone and satellite services. OSS models are potentially more user focused, but the stigma that surrounds sexual health services may create an access barrier. From staff perspectives, the advantages are greater career opportunities and increased responsibility, while the disadvantages are concern that OSSs will result in loss of expertise and professional status. Cost effectiveness data are contradictory.
Conclusion
Although there is a policy commitment to look at how integrated services can be better developed, more evidence is required on the impact and appropriateness of this approach.
Keywords: integration, one stop shop, sexual health, contraception, sexually transmitted diseases
In 2001, the government launched the National Strategy for Sexual Health and HIV.1 An aim of this strategy is to develop sexual health services around patients' needs. A recommendation resulting from this is provision of comprehensive and integrated sexual health services. More recently, the white paper Making Healthier Choices Easier,2 stated that funding is to be made available to “support modernisation of the whole range of NHS sexual health services, ….and deliver these services in a different way.” Providing all sexual health services under one roof has been suggested as a model to ensure a more integrated approach to health care. There is no clear consensus as to what constitutes an integrated service. The white paper, The New NHS: Modern, Dependable, sets an agenda for the NHS to work towards integrated health services that provide for local communities.3 From an organisational perspective, this implies integrated management, planning and configuration of services, as well as common information technology support systems and surveillance. What is less clear is how integration would work.4,5 Should sexual health services be provided under one roof (that is, the one stop shop model) or is it best to maintain specialist services, but ensure good collaborative working or as described by Wilkinson “the supportive friendship” model?6 Where is the best setting and who should provide this integrated service?
The aims of this paper are to examine various approaches and models of integrated and/or one stop shop (OSS) sexual health services (within mainstream contraceptive and genitourinary medicine (GUM) clinics, designated young people's services and general practice), and to investigate strengths and weaknesses of these approaches.
Methods
Literature relating to the integration of contraceptive and GUM services (including OSSs) within primary and secondary care settings was identified through a search of Medline, Embase, and Popline (1990–January 2005). Relevant “grey” literature, such as government policy documents, was also sought. As the focus of this work was to inform the national evaluation of one stop shops in England, the literature reviewed was primarily from the United Kingdom.
The literature review informed the topic guide for in‐depth interviews. The guide included questions on definitions of integration, key characteristics of integrated services, and where they should be located; potential strengths and weaknesses of different approaches; and what could be the main outcomes of a policy promoting integration. Interviewees were purposely selected to represent different stakeholders/professions involved in the development of the national strategy for sexual health and HIV (n = 11) across England. Interviews were conducted over the telephone or face to face. Interviews were taped and transcribed. A thematic analysis was conducted, using the first stages of “framework.”7 Two researchers (RF and CC) analysed the transcripts to ensure reliability. A unique ID number was allocated to each interviewee.
The findings of the literature review and interviews were combined to identify potential benefits and pitfalls associated with integration.
Results
Five broad themes were identified through the analysis: logistics, public health, users, staff, and cost. These provide the structure for this paper and are summarised in table 1.
Table 1 Summary of strengths and weaknesses associated with a one stop shop approach.
| Strengths | Weaknesses | ||
|---|---|---|---|
| Logistics | Provides sexual health care under one roof | Lack of clarity about who should provide care and what levels of care should be providedDifferent ways of collecting data and monitoring | |
| Public health | Evidence of reduction in defaulting after referral to second serviceOpportunity to screen for other health problemsHealth issues are commonly related and some users may be unaware of the need for the alternative service | If target population for each service is different then utilisation is not increasedContraceptive clients are not at disproportionate risk of HIV/STIsCentralisation of services can reduce access and increase delays | |
| User | Many consumers appreciate advantages of OSSMove towards a “holistic” philosophy of care which is more sympathetic to real lifeProvides continuity of careReferral to a second service reduced | Reduced service in both areasEvidence of reduced information given to clientsSome users prefer separate specialist services which offers more choiceIncreased stigma associated with GUM speciality | |
| Staff | Potential to increase staff job satisfaction due to extended roleImprove career opportunitiesProviders are less likely to work in isolation—a more team approachGreater management flexibility | Staff lose specialist skillsResults in overloading of staffContradictory service cultures makes working together challengingStaff may prefer different employment conditions | |
| Cost | Avoid duplication of servicesReduced client/provider contactsOpportunity for cost sharingBoth client groups have similar needs | Costs increase if service offered is comprehensiveReduction in specified funding for services—eg, satellite contraceptive services | |
Logistics
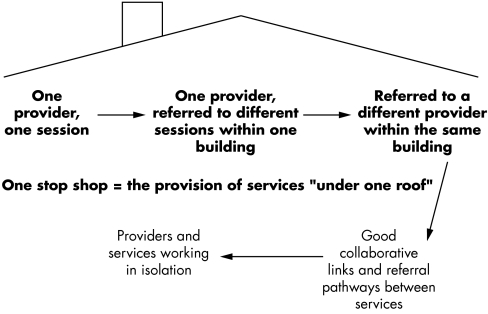
The “one stop shop” in its broadest sense refers to sexual health services on a single site (see fig 1).8,9
Figure 1 Levels of integration.
There is less agreement as to whether one provider should manage care (and who that provider should be) or whether different specialists should be housed in the same building. In practice, OSS services have evolved in different ways, dependent on setting, provider interest, and resources. More contraceptive services are offering chlamydial screening, GUM services supplying contraceptives, and general practitioners (GPs) leading on specialist sexual health services than in the past. However, whether these services should be described as OSSs is arguable.
“It isn't GU services providing three family planning clinics a week and saying that it's an integrated sexual health service.” (ID 5)
The new general medical services contract for GPs has the potential to expand current sexual health services within general practice. There is scope for local primary care organisations to negotiate with general practice providers to widen the remit of ‘essential' sexual health services. Although it was acknowledged by interviewees that there is not capacity to have a fully integrated service within this setting, it was thought that GPs are underused and there was little incentive to change.
Concerns were voiced that sexual health was often viewed as a low priority at local level and different targets for different disciplines of GUM, contraceptive services, and general practice further complicated a move towards integration.
GUM services are often located within acute trusts while GPs and mainstream contraceptive services are within primary care trusts. This can act as a barrier to integration. It has been argued that in order to have an integrated approach common aims need to be established at the development stage.10 Unfortunately, there is often considerable discrepancy between planned and executed actions in terms of integration.11 One of the logistical problems that has been described when integrating community contraceptive and GUM services is that users often end up having different case notes even if all the services are under one roof. There are usually different computer and monitoring systems.12,13 This demonstrates that simply placing two separate services in one building, without a commitment to structural change to bring the services together, does not necessarily lead to meaningful integration.
It is argued that local “managed” networks will provide a framework for planning and structuring services, as well as establishing integrated pathways for the user.14 Some of the interviewees felt it was more important (and realistic) to establish collaborative networks, with clear signposting and consistent messages between services, rather than focusing on OSSs.
“values rather than bricks and mortar.” (ID 11)
Public health perspective
Contraceptive and GUM services have developed along largely independent paths with health issues that are closely related. An interviewee described how the issues were inseparable, and explained how “not taking a sexual history when offering contraceptive care was like giving drugs to a diabetic without discussing diet.” (ID 9).
In the second National Survey of Sexual Attitudes and Lifestyles, 11% of men and 13% of women reported ever having an STI.15 Of these, 76% of men and 57% of women reported attending a GUM clinic. Women were more likely than men to attend their GP for STI treatment. Chlamydial infection is prevalent among users of community contraceptive clinics and general practice.1,16 Yet there is still insufficient STI screening and treatment in these services.17 A study of under 16s attending a GUM clinic in London found that 19% of all female attendees were pregnant, and 76% of those who were not pregnant were not using any contraception at the time.18 Over half of these women reported that they did not receive advice on contraception during their visit.
An OSS approach has the potential to reduce poor sexual health. It has been argued that combined services under one roof may be more successful at targeting clients who are not aware that they need the alternative service.19,20 The effect of different models of sexual health service delivery on STI detection and management or the uptake of contraception remains unknown.
A study in London found that the management of uncomplicated STIs in community clinics was a feasible and effective alternative to merging contraceptive and GUM services into one site.21 Concerns exist that OSS models of sexual health provision may result in centralisation of services and closure of satellite services. If there are too few trained staff to deal with extra capacity and longer consultations resulting from the complexity of the case mix, delays could increase and the public health crisis worsen. Rural services in particular may suffer. A reduced satellite community contraceptive service may mean that some women would use less effective “over the counter” methods or no method at all, rather than travel further to a clinic or go to their GP.22 Satellite and outreach services were seen as an important way of reaching young people and other vulnerable groups in settings such as youth centres and schools. These services act as a “sort of stepping stone into a more mainstream fuller service” (ID 1) and it is important to have local flexibility. One interviewee explained, “a move towards OSSs does not have to mean the end of satellite services; instead we should be looking at adopting a more ‘hub and spoke approach' increasing integration and access across the community” (ID 7).
The user perspective
Designated young people's services have led the development of OSS approaches in the United Kingdom,19 illustrating how changes in service delivery have been introduced to meet local and client specific demands rather than being purely driven by national policy.
Another argument for having contraceptive and STI services under one roof is to be more user focused. The traditional division between contraceptive and GUM services may not be so evident to those who use the services.23 User groups in sexual health are a rarity, and therefore users have no directly driven integration policy. In terms of the development of services there may be conflict between user and staff priorities.24 The benefits of OSSs for users include convenience, a more holistic approach, fewer provider contacts, greater continuity of care, and less referral to other services.25,26,27,28 Evidence suggests that people referred to GUM clinics from contraceptive services do not often attend.29,30 The OSS model has been described as particularly attractive to young people,21 as, for example, issues such as drug use and poor educational achievement can be addressed alongside sexual health. However, OSSs do not necessarily provide a “seamless approach.” An interviewee described how within one service “a patient can be unnecessarily ‘shunted' between different staff during one visit” (ID 10), and therefore the number of contacts with different professionals may not be reduced. There is evidence that users may receive less information in a OSS service compared to a dedicated service.11
Different services often have different target groups. People who use contraceptive clinics are more likely to be younger and single compared to GP users.31 A number of factors affecting service preference have been identified by users.32,33 In contraceptive clinics a wider range of methods may be available and there is a greater chance of seeing a female doctor. In one study just over half of GUM attendees (57%) said they would use a contraceptive service within the GUM clinic.34 Services in general practice may be preferred because they offer greater continuity of care and the reason for the visit is not obvious. There are concerns that, by having all services under one roof, consumer choice is greatly reduced.
The stigma of GUM clinics may act as a barrier to access.35 Contraceptive clinics may have a more “benign appeal” to women, but men are less likely to access these services.26 One of the interviewees felt the branding of sexual health services was one of the main challenges. Health professionals were seen as key in reducing any stigma around using sexual health services.
“The point about stigma is that it should not be perpetuated by the people providing the services.” (ID 4)
Staff perspective
Interviewees commented that the historical divide between general practice, GUM clinics, and contraceptive services still affects attitudes.
“I think the historical legacy is still quite strong and there is a little bit of rivalry.” (ID 1)
Concerns exist about restructuring service provision to an OSS model. From a provider perspective, this includes concerns about professional development, status, and adequacy of expertise.36 Many staff working in sexual health services are currently not trained in both contraception and GUM.37 Some interviewees felt that a move towards OSSs would not lead to the sacrifice of specialist skills:
“It's helpful for people's career development and their sense of professionalism to have specialisms, but … they could still be all generalists in sexual health.” (ID 11)
There is evidence that working within an integrated service maximises staff motivation.27 Most interviewees thought that the move towards integration would increase career opportunities, particularly for nurses. Other benefits include greater flexibility from the management perspective, as there is a dual trained workforce, and use of a team approach rather than staff working in isolation on a sessional basis.6,38 There is also the potential to increase the profile of those working within mainstream contraceptive services. One interviewee explained career opportunities are often lacking in this specialty.
A commitment to multisector and multidisciplinary training was seen as crucial to address attitudes on talking about sex.
“We were fanatically obsessed with taking blood pressure (of women wanting the pill) … but lots of people didn't talk about taking chlamydia swabs and using condoms.” (ID 9)
Cost
It has been argued that OSS models improve efficiency and cost effectiveness by avoiding duplication of service delivery functions and by delivering more services per client contact.11,12,26,27
The provision of parallel services is expensive and limited resources often mean that opening hours are reduced.39 Although it appears there will need to be additional costs to provide more integrated services (including the provision of OSSs), it has been argued that integration is not just about new buildings and more consultants; there is a need to be innovative and utilise the existing infrastructure.6 Concerns have been voiced that OSS models can result in a loss of focus on a particular health issue and hence lack of designated funds.40 Interviewees described how commissioning priorities around sexual health were often patchy:
“On the one hand we've got all the tools … you've got a strategy, action plan, guidance and at the same time you've got no levers in the system to make it happen … We're steering not rowing.” (ID 3)
Interviewees believed there is a lack of evidence that OSSs are more cost effective than separate services that work in collaboration.
Conclusion
There is increasing pressure on sexual health services as rates of infections and high risk sexual behaviour rise. As demand for services increases, it has become more difficult to provide high quality, open access services. In light of these factors there has been a need to rethink service delivery. The literature review and interviewees identified a number of issues that commissioners need to explore when making plans for sexual health services. Namely, the importance of being clear when defining integration and OSS approaches, where and how integration should take place, and what benefits are expected from the different approaches. Despite the government's policy and financial commitment to evaluating OSS approaches, there is currently no clear evidence to suggest that OSSs are any more or less effective in improving sexual health outcomes, acceptable (to both staff and users), accessible or cost effective than separate services that work collaboratively.
Acknowledgements
We would like to thank the individuals who agreed to be interviewed for this paper, and Wendy Chandler who helped prepare the manuscript. Members of the One‐Stop Shop Evaluation team not identified by name in the list of authors include Dr Jo Coast (University of Bristol), Dr Debra Gray (University of Bristol), Dr Sandra Hollinghurst (University of Bristol), Dr Catherine Mercer (UCL), Dr Kevin Miles (UCL), Dr Angela Robinson (UCL), and Dr Karen Rogstad (Royal Hallamshire Hospital). All members of the team provided comments to draft manuscripts.
Abbreviations
GUM - genitourinary medicine
OSS - one stop shop
Footnotes
Funding: The One‐Stop Shop Evaluation is supported by a grant from the Department of Health.
Competing interests: none.
Ethics: Ethical approval was gained via Trent Multi‐centre Research Ethics Committee.
This work was undertaken by the One‐Stop Shop Evaluation Team. The views expressed in this paper are those of the authors and not necessarily those of the Department of Health.
References
- 1.Department of Health The national strategy for sexual health and HIV. London: HMSO, 2001
- 2.Department of Health Making healthier choices easier. London: HMSO, 2004
- 3.Department of Health The new NHS: modern, dependable. London: HMSO, 1997
- 4.Caldwell J, Hardon A. Is integration the answer for Africa? Repro Health Matters 200228108–112. [Google Scholar]
- 5.Mayhew S. Integrating MCH/FP and STD/HIV services: current debates and future directions. Health Policy Plan 199611339–353. [DOI] [PubMed] [Google Scholar]
- 6.Wilkinson C. Keys to success in setting up an integrated sexual health service. Trends in Urology and Sexual Health . 2004;September/October30–34.
- 7.Ritchie J, Spenser L. Qualitative data analysis for applied policy research. In: Baymen A, Burgess RG, eds. Analyzing qualitative data . London: Routledge, 2002;Chapter 9,173–194.
- 8.Fox L J, Williamson N E, Cates W.et al Improving reproductive health: integrating STD and contraceptive services. J Am Med Womens Assoc 199550129–136. [PubMed] [Google Scholar]
- 9.Rogstad K, Ahmed‐Jushuf I H, Robinson A J. Standards for comprehensive sexual health services for young people under 25 years. UK national survey. Int J STDs AIDS 200213420–424. [DOI] [PubMed] [Google Scholar]
- 10.Mackie C M, Elliot L, Thomson D A M.et al Public and private collaboration in establishing a young person's sexual health clinic in a commercial setting. J Fam Plann Reprod Health Care 20024201–203. [DOI] [PubMed] [Google Scholar]
- 11.Schierhout G, Fonn S.The integration of primary health care services: a systematic literature review. Durban: Health Systems Trust, 1999
- 12.Dawson S G, Callander N, Roche C.et al Integrated sexual healthcare: the development and review of one model of service delivery.Int J STDs AIDS 200011428–434. [DOI] [PubMed] [Google Scholar]
- 13.Jones M. Integrating family planning with genitourinary medicine: developing a holistic sexual health clinic in Eastbourne. Br J Fam Plann 200026221–224. [DOI] [PubMed] [Google Scholar]
- 14.Medical Foundation for AIDS and Sexual Health Recommended standards for sexual health services. London: MedFASH, www.medfash.org 2005
- 15.Fenton K A, Korovessis C, Johnson A M.et al Sexual behaviour in Britain: reported sexually transmitted infections and prevalent genital Chlamydia trachomatis infection. Lancet 20023581851–1854. [DOI] [PubMed] [Google Scholar]
- 16.Low N, Slater W. Surveillance of sexually transmitted infections in primary care. Sex Transm Infect 200480152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dale A W, Wilkinson C, Forster G E.et al Provision of Chlamydia trachomatis screening in family planning clinics and emergency contraception in genitourinary medicine clinics: a collaborative cross‐speciality survey. J Fam Plann Reprod Health Care 200228185–188. [DOI] [PubMed] [Google Scholar]
- 18.Creighton S, Edwards S, Welsh J.et al News from the frontline: sexually transmitted infections in teenagers attending a genitourinary clinic in south east London. Sex Transm Infect 200278349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bloxham S, Capstick S, Greenwood A. Combining GUM and contraceptive services for young people: profile of an innovative clinic. Br J Fam Plann 19992518–21. [PubMed] [Google Scholar]
- 20.Beddard D, Chandiok S, James P.et al A 6‐month pilot of a collaborative clinic between genitourinary medicine services and a young person's sexual health service. J Fam Plann Reprod Health Care 20032940–42. [DOI] [PubMed] [Google Scholar]
- 21.Evans J, Baraitser P, Cross J.et al Managing genital infection in community family planning clinics: an alternative approach to holistic sexual health provision. Sex Trans Inf 200480142–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bardsley M, Newman M, Morgan D.et al Estimating the balance of general practice versus family planning coverage of contraceptive services in London. Br J Fam Plann 20002621–25. [PubMed] [Google Scholar]
- 23.Wilkinson C. The integration of family planning and genitourinary medicine services. Br J Fam Plann 200026187–189. [DOI] [PubMed] [Google Scholar]
- 24.Baraitser P, Blake G, Brown K C.et al Barriers to the involvement of clients in family planning service development: lessons learnt from experience. J Fam Plann Reprod Health Care 200329199–203. [DOI] [PubMed] [Google Scholar]
- 25.Hardon A. Reproductive health care in the Netherlands: would integration improve it? Repro Health Matters 20031159–73. [DOI] [PubMed] [Google Scholar]
- 26.Hardee K, Yount K M.From rhetoric to reality: delivering reproductive health promises through integrated services. US, Family Health International. Working Paper Series 1995
- 27.Fleischman Foreit K, Hardee K, Agarwal K. When does it make sense to consider integrating STI and HIV services with family planning services? Repro Health Matters 200228105–107. [Google Scholar]
- 28.Stirland A. Family planning up a gum tree‐the integration of family planning and genitourinary services in Australia and New Zealand. Br J Fam Plann 199520132–136. [Google Scholar]
- 29.Gunneberg N, Mann M C, Radcliffe K W. Access to genitourinary medicine services by women attending a family planning clinic. Int J STDs AIDS 19967102–105. [DOI] [PubMed] [Google Scholar]
- 30.Vanhagen G, Wedgwood A. Do you people attend genitourinary medicine clinics when referred by a community based Brook Advisory Centre? Br J Fam Plann 19992523–24. [Google Scholar]
- 31.Cooper P, Diamond I, High S.et al A comparison of family planning provision: general practice and family planning clinics. Br J Fam Plann 199419263–269. [Google Scholar]
- 32.Selman P, Calder J. Variations in the characteristics of attenders at community family planning clinics. Br J Fam Plann 199424123–127. [Google Scholar]
- 33.Coleman L, Philipps D R. Consumers' use of family planning services in the United Kingdom: a review of the current literature and findings from surveys 1985–1992. Occasional Paper No 21. University of Exeter: Institute of Population Studies, 1993
- 34.Kingston M A, White C, Carlin E M.et al Genitourinary medicine: an opportunity to reduce unwanted pregnancy. Int J STDs AIDS 200415192–194. [DOI] [PubMed] [Google Scholar]
- 35.Scoular A, Duncan B, Hart G. “That sort of place…where filthy men go…”: a qualitative study of women's perceptions of genitourinary medicine services. Sex Transm Infect 200177340–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kane R, Wellings K. Integrated sexual health services: the views of medical professionals. Cult Health Sex 19991131–145. [DOI] [PubMed] [Google Scholar]
- 37.Walsh J.Reviewing contraceptive services: research findings and framework. London: Contraception Education Service, 1999
- 38.Stedman Y, Elstein M. Rethinking sexual health clinics. BMJ 1995310342–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baraitser P, Fettiplace R, Dolan F.et al Quality, mainstream services with proactive and targeted outreach: a model of contraceptive service provision for young people. J Fam Plann Reprod Health Care 20022890–94. [DOI] [PubMed] [Google Scholar]
- 40.Berer M. Integration of sexual and reproductive health services: a health sector priority. Repro Health Matters 2003116–15. [DOI] [PubMed] [Google Scholar]