Abstract
Cellular metabolism generates the cytotoxic superoxide free radical, O2·–, and a family of enzymes called superoxide dismutases (SOD) protects us from O2·– by catalyzing its conversion to O2 and H2O2. Superoxide production increases in a wide variety of pathological states, especially those involving inflammation or ischemic injury. Most of the literature has described systems wherein added or over expressed SOD produced beneficial effects, yet in some circumstances SOD provided no benefit, or was clearly detrimental, exacerbating cell injury or death. When broad dose-response studies were finally possible in models of reperfusion injury in the isolated heart, hormesis became clear. We propose that the mechanisms underlying the hormesis are related to the paradoxical abilities of the superoxide radical to serve as both an initiator and a terminator of the free radical-mediated chain reaction that results in lipid peroxidation. Lipid peroxidation is a universal feature of oxidative stress, causing loss of cellular structure and function. Under any given conditions, the optimal concentration of SOD is that which decreases chain initiation without elimination of the chain termination properties of the radical, resulting in a minimum of net lipid peroxidation. Mathematical modeling of this hypothesis yields predictions fully consistent with observed laboratory data.
Keywords: superoxide dismutase, lipid peroxidation, dose-response, reperfusion injury, free radical, hormesis
INTRODUCTION
The increased production of the superoxide free radical has come to occupy a remarkably central role in a wide variety of diseases, as documented by thousands of published studies (McCord, 2000). Superoxide is not, as first thought, just a toxic but unavoidable byproduct of oxygen metabolism. Rather, we now appreciate that it is a carefully regulated metabolite capable of signaling and communicating important information to the cell’s genetic machinery. Redox regulation of gene expression by superoxide and other related oxidants and antioxidants has become a mechanism of great interest in health and disease (Rushmore and Kong, 2002).
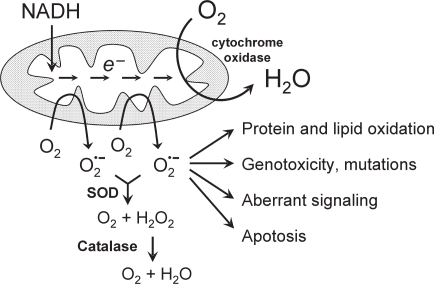
Surprisingly, about 98% of the oxygen we metabolize is handled by a single enzyme—the cytochrome oxidase in our mitochondria, which transfers four electrons to oxygen in a concerted reaction to produce two molecules of water as the product. The probable reason for this near monopoly in the reduction of oxygen is the chemical difficulty of carrying out this combustion reaction in a safe and controlled manner. If oxygen receives less than the full complement of four electrons, the result is the production of active oxygen species O2·− and H2O2. Even in a healthy cell approximately 1 or 2% of all oxygen metabolized might be converted directly to superoxide and/or hydrogen peroxide (Chance et al., 1979), reflecting the ability of molecular oxygen to “steal” electrons from a variety of cellular reductants via spontaneous (non-enzyme-catalyzed) oxidation. Thus, even though our electron-conducting metabolic circuits are generally well-insulated by evolutionary design to prevent the accidental development of short-circuits, our insulation is not perfect. At least two sites have been identified in the electron-transport chain (Complex I and ubisemiquinone) where electrons may leak out to oxygen molecules, resulting in the formation of superoxide (McCord and Turrens, 1994). These sites are shown in Fig. 1 as the primary sources of intracellular superoxide generation. In a healthy cell, the superoxide produced is detoxified by the antioxidant enzyme SOD (McCord and Fridovich, 1969), which catalyzes the reaction:
FIGURE 1.
A schematic diagram of the mitochondrial electron transport system illustrating that at least two specific “leakage sites” exist in injured mitochondrial allowing electrons to prematurely reach oxygen molecules, giving rise to the superoxide radical. SOD and catalase normally detoxify the radical. If superoxide concentration rises too high, oxidation of proteins, lipids, and DNA may occur and various signalling pathways may be triggered.
This dismutation or disproportionation reaction makes use of the fact that the superoxide radical can react either as an oxidant or a reductant, eager to get rid of its extra electron or to take on another. The enzyme uses one superoxide radical to oxidize another. Catalases work in much the same way to detoxify the resulting H2O2, because hydrogen peroxide can be a weak reductant as well as a fairly strong oxidant:
Thus, SOD and catalase working together convert superoxide to the innocuous products O2 and H2O (Fig. 1).
Working myocardium consumes oxygen at about 8 mM/min, and therefore the rate of superoxide production in a healthy cell might reach 0.1 mM/min. During exposure to hyperoxia, the rates of leakage from these sites in lung mitochondria are believed to increase in direct proportion to the increased oxygen tension. Healthy adult rats die after about 72 hours in an atmosphere of 100% oxygen—only five times the normal concentration at sea level (Crapo and Tierney, 1974). This accounts for the hormesis observed with increasing oxygen concentrations.
ISCHEMIA/REPERFUSION INJURY
In 1981 intravenously administered SOD was first shown to be protective in a model of feline intestinal partial ischemia/reperfusion injury (Granger et al., 1981), implying that increased superoxide production might be responsible in large part for the post-ischemic destruction of tissues as occurs, for example, in stroke and myocardial infarction. In the intestine, the major source of superoxide was concluded to be from the enzyme xanthine dehydrogenase, normally an innocuous NAD+-reducing enzyme involved in the catabolism of purines. During ischemia, however, tissues are unable to maintain ATP levels, allowing Ca++ to enter the cytosol as there is too little energy available to power the divalent cation pump at the cell membrane. This intracellular Ca++ can activate proteases such as calpain, which in turn can partially proteolyze xanthine dehy-drogenase converting it into xanthine oxidase. Xanthine oxidase no longer reduces NAD+, but rather transfers electrons to molecular oxygen to produce the superoxide radical:
During ischemia, an abundant amount of hypoxanthine builds up as AMP is catabolized. Upon reoxygenation of the tissue the missing substrate, O2, is supplied, allowing a burst of superoxide production (McCord, 1985). In tissues rich in xanthine dehydrogenase such as the intestine, this seems to be the major source of reoxygenation injury. In myocardial reperfusion injury of rodents and dogs, this also appears to be the predominant mechanism of injury. Hearts of humans (Eddy et al., 1987) and rabbits (Terada et al., 1991), however, contain only traces of xanthine oxidase activity, and this mechanism appears to make a much smaller contribution to reoxygenation injury, but one that may still be significant (Terada et al., 1991; Zhao et al., 2008).
In tissues or species that contain little xanthine dehydrogenase, SOD is still dramatically protective against reoxygenation injury (Nelson et al., 1994), implying that another damaging source of superoxide exists. This alternate source appears to be much more basic—the resumption of mitochondrial respiration itself (Ambrosio et al., 1993). As intracellular calcium levels rise in energy-compromised ischemia tissues, the calcium is avidly taken up by the mitochondria leading to uncoupling, futile cycling, and increase production of superoxide (Paraidathathu et al., 1992). This mechanism of reoxygenation-induced superoxide production is likely common to all mammalian cells.
CONTROVERSY AND HORMESIS
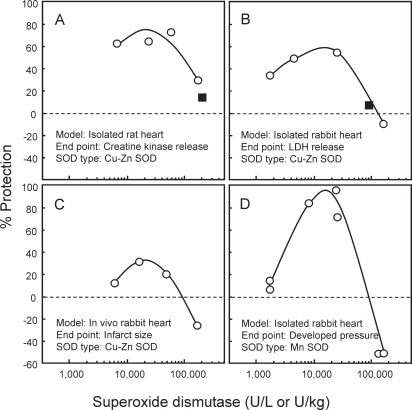
The possibility that reoxygenated tissues might be significantly protected by SOD quickly captured the interest of experimental cardiologists and myocardial physiologists. As various laboratories began studying various models, controversy soon appeared in the literature. There was little agreement as to whether SOD did (Ambrosio et al., 1986; Aoki et al., 1988; Burton, 1985; Chambers et al., 1985; Gardner et al., 1983; McCord et al., 1989; Tamura et al., 1988; Werns et al., 1985; Woodward and Zakaria, 1985) or did not (Buchwald et al., 1989; Menasche et al., 1986; Myers et al., 1985; Uraizee et al., 1987) protect the reoxygenated heart. There were many differences among the many models, including in vitro versus in vivo, global versus regional ischemia, partial versus complete ischemia, buffer perfused versus blood perfused, and, importantly, the concentration of SOD used. Because of the expense and labor-intensity of the models, none of these cited studies examined dose-response relationships. One of the first studies to vary the dose of SOD was quite illuminating, as U-shaped curves were apparent when SOD was used to prevent the occurrence of reperfusion-induced arrhythmias (ventricular fibrillation and tachycardia) following 10 min of coronary artery occlusion in isolated rat hearts (Bernier et al., 1989). We soon reported similarly shaped curves with regard to creatine kinase release from hypoxic/reoxygenated isolated rat hearts (Fig. 2A) and lactate dehydrogenase release from globally ischemic/reperfused rabbit hearts (Fig. 2B), or area of infarct in an in vivo model of coronary artery ligation in rabbits (Fig. 2C) (Omar et al., 1990). It is remarkable to note the consistent loss of protection at higher doses of SOD, even though the models differ considerably with respect to species (rat versus rabbit), end point measured (infarct size, enzyme release, arrhythmogenesis, or recovery of developed ventricular pressure), source of the SOD used (yeast in the rat and human recombinant in the rabbit) and its schedule of administration (continuous versus a single bolus). Furthermore, our curves could clearly have predicted the outcomes of some reported negative studies in the literature using the isolated rat (Menasche et al., 1986) (see Fig. 2A) and rabbit (Myers et al., 1985) hearts (see Fig. 2B).
FIGURE 2.
Bell-shaped dose-response curves have been reported in various models reflecting the ability of SOD to protect or exacerbate injury to the post-hypoxic heart. Data are re-plotted from Omar et al. (1990) and Omar and McCord (1990). In Panel A, the black square represents data from Menasche et al. (1986) using a similar model. Similarly, in Panel B the black square represents data from Myers et al. (1985) using a similar model. Both of these studies reported no significant protection from SOD at these single doses.
HOW CAN TOO MUCH SOD BE DAMAGING?
Several potential explanations have been offered to explain the hormetic behavior of SOD. The most common explanation is that since SOD produces H2O2 as a product, more SOD would produce more H2O2, which is toxic to cells (Kedziora and Bartosz, 1988; Mao et al., 1993; Norris and Hornsby, 1990). This explanation does not hold when the SOD-catalyzed reaction is competing for superoxide with spontaneous (uncatalyzed) dismutation, for the net reaction rates are identical in the steady-state. The molar rate of H2O2 production is exactly one-half the molar rate of O2·− production, regardless of the concentration of SOD (McCord and Fridovich, 1969). SOD will dramatically lower the steady-state concentration of superoxide, but obviously cannot alter the steady-state rate of its coversion to H2O2, as this is limited by the rate of superoxide production. It has also been suggested numerous times that the toxicity of high-dose SOD might be due to a weak peroxidase activity of Cu,Zn-SOD (Hodgson and Fridovich, 1975). As seen in Fig. 2D, however, Mn-SOD shows the same bell-shaped dose-response (Omar and McCord, 1990) as those produced by Cu,Zn-SOD (Fig. 2A, 2B, and 2C) (Omar et al., 1990), despite its lack of such a peroxidase activity (Hodgson and Fridovich, 1975).
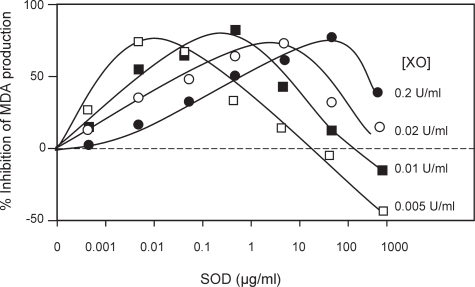
We hypothesized an alternate explanation based not upon the properties of SOD per se, but rather upon a major physiological process being modulated by changes in the concentration of superoxide in a cell—lipid peroxidation. Even in a very simple chemically defined system, SOD displays bell-shaped dose-response curves if that system involves lipid peroxidation. An example is the oxidation of pure linolenic acid by xanthine/ xanthine oxidase plus ferric iron (Lazzarino et al., 1994). Fig. 3 shows a series of hormetic curves as the concentration of SOD is varied together with the rate of O2·− generation in such a system. At each higher rate of O2·− generation a new optimally protective concentration is defined. This optimally protective SOD concentration varies linearly with rate of O2·− production over several orders of magnitude. In simple systems that do not involve lipid peroxidation such as the inactivation of creatine kinase by xanthine/xanthine oxidase, SOD shows nearly complete protection with no indication of hormesis (McCord and Russell, 1988).
FIGURE 3.
Bell-shaped dose-response curves produced by SOD in a simple system consisting of 3 mM linolenic acid in the presence of 4.65 μM FeCl3 and 1 mM xanthine. Superoxide was generated by the indicated concentrations of xanthine oxidase, and inhibition of malondialdehyde formation was noted at the indicated concentrations of SOD. Data are re-plotted from Lazzarino et al. (1994).
SUPEROXIDE RADICAL INITIATES AND TERMINATES LIPID PEROXIDATION
Like all other free radical chain reactions, lipid peroxidation must be initiated by a free radical, (i.e., by a one-electron oxidation) in this case abstracting an allylic hydrogen from a polyunsaturated side chain to create a lipid radical (L·). The protonated form of superoxide, the hydroperoxyl radical (HO2·), can serve as an initiating radical due to its lipophilicity and redox potential:
The lipid radical L· adds molecular oxygen extremely rapidly to produce a lipid dioxyl radical, which is a sufficiently good oxidant to abstract an allylic hydrogen from another unsaturated side chain, producing a lipid hydroperoxide (LOOH) and propagating the chain:
Typically in vivo these two reactions cycle about 15 times, such that each initiating event results in the oxidation of about 15 polyunsaturated fatty acid molecules. (The LOO· radical may alternatively rearrange and break down to produce malondialdehyde and other radical products, rather than yielding exclusively a lipid hydroperoxide product, but these options do not affect the present discussion.) Hence, it is well-established that superoxide can initiate lipid peroxidation. Ironically, the only way to eliminate a radical is by reacting it with another radical. (Because radicals have an odd number of electrons, any reaction with a non-radical must yield a product that is another radical.) Thus, from a teleological perspective, it would be useful if a cell had available a continuous supply of a relatively unreactive free radical for the purpose of promoting a radical-radical annihilation to eliminate the very dangerous chain-propagating lipid dioxyl radicals. We have suggested that superoxide meets these criteria (Nelson et al., 1994). It is produced as a by-product of oxygen metabolism, and is therefore continuously available in all cells. As free radicals go, it is relatively unreactive. Its concentration is maintained at a very low, but non-zero value by the cellular SOD content. If lipid dioxyl radicals were scavenged by O2·−, then entire chains of reactions would be prevented or terminated:
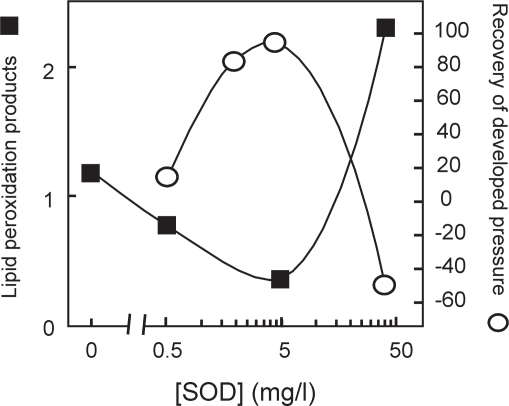
Therefore, it was hypothesized that O2·−, in addition to being able to liberate iron and to initiate lipid peroxidation, may also serve as a terminator of lipid peroxidation, such that over scavenging the radical may increase net lipid peroxidation (Nelson et al., 1994; Omar et al., 1990). A functionally similar termination reaction was proposed by Thom and Elbuken (Thom and Elbuken, 1991) whereby the protonated form of superoxide, HO2·, reacts with LOO· to produce water, oxygen, and a carbonyl containing lipid peroxidation product. If either hypothesis is correct, then indices of lipid peroxidation should be high at both low concentrations of SOD (where initiation would be high) and at high concentrations of SOD (where termination would be low). At some intermediate SOD concentration, initiation by superoxide would be largely suppressed, but termination by superoxide would still be making a contribution, and net lipid peroxidation would be at a minimum. We found these predictions to be true (Nelson et al., 1994), and experimental verification is shown in Fig. 4. In this model of the isolated perfused rabbit heart, 60 min of no-flow ischemia followed by reperfusion results in serious oxidative stress. As the concentration of SOD in the perfusate is increased, a new balance is restored when the concentration reaches 5 mg/l. Note that maximal recovery of preischemic function (developed pressure) occurs when lipid peroxidation is reduced to the minimum. These results suggest that for any given level of oxidative stress, a single optimal concentration of SOD exists that will restore the superoxide level to yield the best combination of initiation and termination (i.e., the one producing minimal net lipid peroxidation). Any concentration of SOD other than the optimal leads to increased lipid peroxidation and therefore to increased oxidative stress.
FIGURE 4.
Relationships of net lipid peroxidation and functional recovery of isolated rabbit hearts to administered dosages of SOD following ischemia-reperfusion. Recovery of developed pressure correlates inversely with net lipid peroxidation as assessed by thiobarbituric acid-reactive substances in the coronary effluent. Maximal recovery of developed pressures was seen at a dosage of 5 mg SOD/L in the coronary perfusate. Data are re-plotted from (Nelson et al., 1994).
THEORETICAL PREDICTIONS
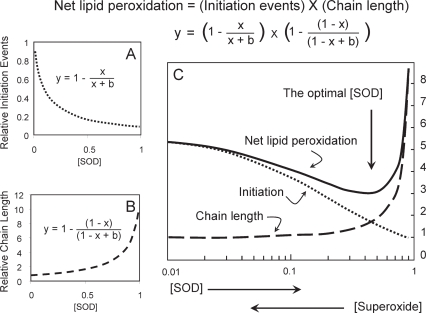
Fig. 5 presents the expected mathematical relationships between SOD concentration (which is inversely related to superoxide concentration) and initiation, termination, and net lipid peroxidation. Panel A shows that as SOD concentration increases (and O2·− decreases) initiation (at least that fraction dependent upon superoxide) would decrease according to an inverse rectangular hyperbola, asymptotically approaching zero initiating events at infinite SOD. Panel B shows the expected effect on chain length. At the highest concentration of O2·− (no SOD) the chain length would approach unity, reflecting complete suppression of propagation reactions. At the lowest concentration of the radical (high SOD) the chain length would be maximal (limited only by other terminators such as vitamin E, or by the mutual annihilation of propagating radicals). This produces another inverse rectangular hyperbolic function in the opposite direction. Net lipid peroxidation, shown in Panel C, is represented by the product of initiation events times chain length. Panel C shows the curves from Panels A and B replotted on a semilog coordinate, along with the curve produced by multiplying initiation by chain length. Note that the net amount of lipid peroxidation displays a minimum at a specific, optimal concentration of SOD. It is an inverted bell-shaped curve. Fig. 5 shows the remarkable similarity in shape of this theoretically predicted curve for net lipid peroxidation and that obtained experimentally by monitoring lipid peroxidation products generated by an isolated perfused heart (Fig. 4). This convinces us that the superoxide radical can act both as initiator of lipid peroxidation and terminator of lipid peroxidation. This realization provides a rational basis for the bell-shaped dose-response curves observed for SOD in systems involving lipid peroxidation, and argues that, for any specific set of conditions, there is a single, optimally protective concentration of SOD. It underscores the importance of balance between oxidants and antioxidants.
FIGURE 5.
The predicted mathematical relationships between SOD concentration (which is inversely related to superoxide concentration) and lipid peroxidation. Panel A shows the relationship between SOD and initiation events, while Panel B shows the relationship between SOD and termination events (in terms of chain length). The equations for the rectangular hyperbolic functions are shown in the respective panels. As net lipid peroxidation is reflected by the product of initiation events times chain length, that resulting equation is plotted in Panel C, showing the predicted minimum at a certain concentration of SOD.
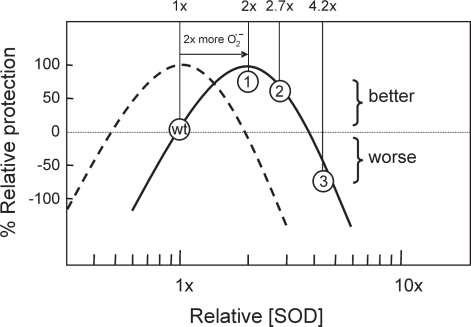
An understanding of hormetic behavior has allowed us to reconcile seemingly contradictory early studies using single doses of exogenous SOD in isolated organ preparations as pointed out in Figs. 2A and 2B. We can also use this understanding to reconcile seemingly contradictory studies of transgenic (Tg) mice, where varying but fixed levels of endogenous SOD expression have been achieved in Tg mouse lines depending on gene copy number and promoter efficiency. Fig. 6 examines results from three such published studies of Tg mice overexpressing SOD1 to different degrees, superimposed on our own empirical dose-response curve (from the data in Fig. 2D, seen here as the dashed curve in Fig 6). This curve assumes that in a healthy wild-type mouse, the normal 1X expression level of SOD1 provides near optimal biological outcome. If we further assume that a pathological stress such as ischemia followed by reperfusion might double the rate of superoxide production in a tissue, then we can imagine that the dose-response curve would be shifted to the right (solid curve in Fig. 6), such that the optimal biological outcome would require twice as much SOD expression. Let us first look at the results of a study examining intestinal reperfusion injury in a Tg mouse line overexpressing SOD1 by 2-fold (Deshmukh et al., 1997). These authors observed that the Tg mice showed only 26% as much increase in lipid peroxidation as their wild-type counterparts. These data are normalized to wild-type and plotted as the point labeled “1” in Fig. 6, falling close to its predicted position on the solid curve. Another study of a Tg mouse line overexpressing SOD1 by 2.7-fold examined myocardial ischemia-reperfusion in isolated hearts, measuring lactate dehydrogenase release as a marker of tissue damage (Chen et al., 2000). Here the Tg mice showed only 40% as much enzyme release as their wild-type counterparts. These data are normalized to wild-type and plotted as the point labeled “2” in Fig. 6, again falling at its predicted position on the solid curve. In a third study of a Tg mouse line, this time overexpressing SOD1 by 4.2-fold, transient in utero ischemia-reperfusion was produced in pregnant mothers. After 24 h of reperfusion in utero the fetal brains were analyzed for lipid peroxidation products (Levy et al., 2002). Here the Tg mice showed 76% more lipid peroxidation than their wild-type counterparts. These data are normalized to wild-type and plotted as the point labeled “3” in Fig. 6, again falling near the predicted position on the solid curve. Remarkably, very similar and predictable results are obtained whether is SOD dosed in vivo by transgenic manipulation or ex vivo in isolated organs perfused with purified exogenous SOD at various concentrations.
FIGURE 6.
Reconciliation of literature reports describing transgenic mice overexpressing SOD1 to different degrees. Our empirical dose-response curve from the data in Fig. 2D is seen here as the dashed curve. If pathological stress doubles the rate of superoxide production, then the curve would shift to the right (solid curve), such that optimal protection requires twice as much SOD, and 1x wild-type (wt) expression becomes inadequate. Results from three published studies of Tg-mice are shown: Point “1”, a 2-fold overexpressing mouse (Deshmukh et al., 1997); Point “2”, a 2.7-fold over-expressing mouse (Chen et al., 2000); and Point “3”, a 4.2-fold overexpressing mouse (Levy et al., 2002). The data are normalized to their respective wild-types.
CONCLUSIONS AND PRACTICAL IMPLICATIONS
An obvious and far-reaching conclusion to draw from these observations is that the optimally protective concentration of SOD under any set of circumstances is at the top of the bell-shaped curve, but that the curve is not static. Rather, the curve will shift to the right as the flux of superoxide production increases due to a variety of pathophysiological conditions, including ischemia-reperfusion, inflammation, redox-cycling drugs or xenobiotics, hyperoxia, and even normal aging. Adding to the complexity is the likelihood that the curve may shift to the right in one particular organ if the pathology is organ-specific, as would be the case following a heart attack or stroke. It is precisely these bell-shaped curves, we believe, that have made clinical applications of SOD1 or SOD2 so problematic. To maintain plasma concentrations of therapeutically administered enzymes in a range that varies by no more than two- or three-fold becomes clinically difficult with proteins that are rapidly cleared by the kidneys. It might be pointed out here that the apparent toxicity of high-dose SOD appears to be manifest only in injured tissues where lipid peroxidation is increased, and superoxide may not be the exclusive initiator. If lipid peroxidation is not ongoing, elevated concentrations of SOD appear to do no harm to tissues until they reach 5- or 6-fold above wild type.
A genetically-engineered chimeric recombinant human SOD (SOD2/3) has been produced by combining portions of the SOD2 and SOD3 genes (Gao et al., 2003). This chimeric molecule has better pharmacological properties than any of the naturally occurring enzymes, and may eliminate some of the dose-response problems that have been described here (Hernandez-Saavedra et al., 2005). A comparison of the effects of SOD2/3 in a variety of in vivo models at varying dosages produced a dramatically flattened bell curve. This may reflect the unusual properties of SOD2/3 regarding its subcellular location (on the outer surfaces of cells or bound to intracellular matrix), its size (small enough to extravasate easily), and its near-neutral charge (which facilitates both both extravasation and binding). If these factors are considered with regard to the three natural forms of SOD (SOD1 in the cytosol, SOD2 in the mitochondrial matrix, SOD3 in the extracellular and nuclear compartments) one realizes that changes in the activities of the isozymes may not produce equivalent effects with regard to hormetic behavior. That is, changing the SOD activity in any given subcellular compartment and/or binding location within a compartment may affect the shape or magnitude of the resulting hormetic curve.
While this review has focused on hormetic behavior that is strictly related to the dual effects of superoxide as initiator and terminator of lipid peroxidation, it is interesting to consider other data suggesting that hormetic behavior might also result from the signal transducing roles of the radical. As primitive life forms evolved in an increasingly aerobic environment, living with the unavoidable production of superoxide became a fact of life. The concentration of this omnipresent yet evanescent free radical afforded the cell with a realtime indicator of such important information as the availability of a food supply, reflected by mitochondrial oxidative activity. An abundance of food signals a good time for a cell to divide. Not surprisingly, cells learned to undergo mitosis when mild oxidative stress signaled an abundance of energy. One might wonder what would happen to this signaling system if the cell produced so much SOD that this signal to divide might be extinguished. One possibility is that the cell would simply cease to divide. When scientists began to produce SOD-transfected cell lines and SOD-transgenic mice it became apparent that there was an upper limit of perhaps eight- to ten-fold to the amount of SOD over expression that could be tolerated (Norris and Hornsby, 1990). There is a growing appreciation of the roles played by superoxide and its dismutation product hydrogen peroxide in the regulation of cell growth (Burdon, 1995), while other signal transduction pathways seem to generate superoxide specifically for signaling purposes. A family of NADPH oxidases, activated by such stimuli as angiotensin II, tumor necrosis factor-α, and insulin, regulate the activation of distinct protein kinases (Anilkumar et al., 2008) that have the potential to affect vascular smooth muscle and cardiac hypertrophy, endothelial activation, angiogenesis, and atherosclerosis. Hence, the aberrant regulation of these signals by too much or too little SOD activity could, in theory, give rise to many additional instances of hormetic behavior.
An exciting alternative approach to the therapeutic use of exogenous SODs is the controlled induction of the family of antioxidant enzymes regulated directly or indirectly by the Antioxidant Response Element (ARE). The ARE is a promoter element activated by the transcription factor Nrf2. A number of phytochemicals long known to traditional medicine appear to be a safe and effective means of upregulating these enzymes in humans via Nrf2-dependent mechanisms (Chen and Kong, 2004; Nelson et al., 2006). Interestingly, these phytochemicals themselves display strong hormetic effects which reflect their abilities to stimulate or inhibit multiple signaling pathways, with different effects occurring at different ED50 concentrations of the phytochemical. Unfortunately, much of the literature in this area has not utilized dose-response curves, but rather has examined fixed, high concentrations of the phytochemicals. The concentrations examined are often not pharmacologically achievable and therefore of questionable physiological relevance. The studies have often overlooked dramatic ARE activation at lower concentrations that disappears at the higher concentrations. An awareness of hormesis is essential for studies involving signal transduction pathways.
Finally, it should be noted that the antioxidant enzymes are largely coordinately regulated, directly or secondarily, by ARE-regulated promoters. It may be highly artificial to manipulate the concentration of SOD alone, observing effects on net lipid peroxidation, when in vivo the entire network of antioxidant enzymes would more likely be induced in concert. This means that glutathione levels would be raised via increased synthesis, glutathione reductase and peroxidases would be induced to eliminate lipid hydroperoxides, and various peroxiredoxins would also be induced. All of these actions would serve to limit lipid peroxidation. Hence, an animal’s natural response to oxidative stress might be much less likely to produce hormetic effects than laboratory experiments that manipulate any single antioxidant enzyme such as SOD.
REFERENCES
- Ambrosio G, Becker LC, Hutchins GM, Weisman HF, Weisfeldt ML. Reduction in Experimental Infarct Size by Recombinant Human Superoxide Dismutase: Insights into the Pathophysiology of Reperfusion Injury. Circulation. 1986;74:1424–1433. doi: 10.1161/01.cir.74.6.1424. [DOI] [PubMed] [Google Scholar]
- Ambrosio G, Zweier JL, Duilio C, Kuppusamy P, Santoro G, Elia PP, Tritto I, Cirillo P, Condorelli M, Chiariello M, Flaherty JT. Evidence That Mitochondrial Respiration Is a Source of Potentially Toxic Oxygen Free Radicals in Intact Rabbit Hearts Subjected to Ischemia and Reflow. J Biol Chem. 1993;268:18532–18541. [PubMed] [Google Scholar]
- Anilkumar N, Weber R, Zhang M, Brewer A, Shah AM. Nox4 and Nox2 NADPH Oxidases Mediate Distinct Cellular Redox Signaling Responses to Agonist Stimulation. Arterioscler Thromb Vasc Biol. 2008;28:1347–1354. doi: 10.1161/ATVBAHA.108.164277. [DOI] [PubMed] [Google Scholar]
- Aoki N, Bitterman H, Brezinski ME, Lefer AM. Cardioprotective Actions of Human Superoxide Dismutase in Two Reperfusion Models of Myocardial Ischaemia in the Rat. Br J Pharmacol. 1988;95:735–740. doi: 10.1111/j.1476-5381.1988.tb11699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier M, Manning AS, Hearse DJ. Reperfusion Arrhythmias: Dose-Related Protection by Anti- Free Radical Interventions. Am J Physiol. 1989;256:H1344–H1352. doi: 10.1152/ajpheart.1989.256.5.H1344. [DOI] [PubMed] [Google Scholar]
- Buchwald A, Klein HH, Lindert S, Pich S, Nebendahl K, Wiegand V, Kreuzer H. Effect of Intracoronary Superoxide Dismutase on Regional Function in Stunned Myocardium. J Cardiovasc Pharmacol. 1989;13:258–264. doi: 10.1097/00005344-198902000-00013. [DOI] [PubMed] [Google Scholar]
- Burdon RH. Superoxide and Hydrogen Peroxide in Relation to Mammalian Cell Proliferation. Free Radic Biol Med. 1995;18:775–794. doi: 10.1016/0891-5849(94)00198-s. [DOI] [PubMed] [Google Scholar]
- Burton KP. Superoxide Dismutase Enhances Recovery Following Myocardial Ischemia. Am J Physiol. 1985;248:H637–H643. doi: 10.1152/ajpheart.1985.248.5.H637. [DOI] [PubMed] [Google Scholar]
- Chambers DE, Parks DA, Patterson G, Roy RS, McCord JM, Yoshida S, Parmley L, Downey JM. Xanthine Oxidase As a Source of Free Radical in Myocardial Ischemia. J Mol Cell Cardiol. 1985;17:145–152. doi: 10.1016/s0022-2828(85)80017-1. [DOI] [PubMed] [Google Scholar]
- Chance B, Sies H, Boveris A. Hydroperoxide Metabolism in Mammalian Organs. Physiol Rev. 1979;59:527–605. doi: 10.1152/physrev.1979.59.3.527. [DOI] [PubMed] [Google Scholar]
- Chen C, Kong AN. Dietary Chemopreventive Compounds and ARE/EpRE Signaling. Free Radic Biol Med. 2004;36:1505–1516. doi: 10.1016/j.freeradbiomed.2004.03.015. [DOI] [PubMed] [Google Scholar]
- Chen Z, Oberley TD, Ho Y, Chua CC, Siu B, Hamdy RC, Epstein CJ, Chua BH. Overexpression of CuZnSOD in Coronary Vascular Cells Attenuates Myocardial Ischemia/Reperfusion Injury. Free Radic Biol Med. 2000;29:589–596. doi: 10.1016/s0891-5849(00)00363-4. [DOI] [PubMed] [Google Scholar]
- Crapo JD, Tierney DF. Superoxide Dismutase and Pulmonary Oxygen Toxicity. Am J Physiol. 1974;226:1401–1407. doi: 10.1152/ajplegacy.1974.226.6.1401. [DOI] [PubMed] [Google Scholar]
- Deshmukh DR, Mirochnitchenko O, Ghole VS, Agnese D, Shah PC, Reddell M, Brolin RE, Inouye M. Intestinal Ischemia and Reperfusion Injury in Transgenic Mice Overexpressing Copper-Zinc Superoxide Dismutase. Am J Physiol. 1997;273:C1130–C1135. doi: 10.1152/ajpcell.1997.273.4.C1130. [DOI] [PubMed] [Google Scholar]
- Eddy LJ, Stewart JR, Jones HP, Engerson TD, McCord JM, Downey JM. Free Radical-Producing Enzyme, Xanthine Oxidase, Is Undetectable in Human Hearts. Am J Physiol. 1987;253 (Heart 22):H709–H711. doi: 10.1152/ajpheart.1987.253.3.H709. [DOI] [PubMed] [Google Scholar]
- Gao B, Flores SC, Leff JA, Bose SK, McCord JM. Synthesis and Anti-Inflammatory Activity of a Chimeric Recombinant Superoxide Dismutase: SOD2/3. Am J Physiol Lung Cell Mol Physiol. 2003;284:L917–L925. doi: 10.1152/ajplung.00374.2002. [DOI] [PubMed] [Google Scholar]
- Gardner TJ, Stewart JR, Casale AS, Downey JM, Chambers DE. Reduction of Myocardial Ischemic Injury With Oxygen-Derived Free Radical Scavengers. Surgery. 1983;94:423–427. [PubMed] [Google Scholar]
- Granger DN, Rutili G, McCord JM. Superoxide Radicals in Feline Intestinal Ischemia. Gastroenterology. 1981;81:22–29. [PubMed] [Google Scholar]
- Hernandez-Saavedra D, Zhou H, McCord JM. Anti-Inflammatory Properties of a Chimeric Recombinant Superoxide Dismutase: SOD2/3. Biomed Pharmacother. 2005;59:204–208. doi: 10.1016/j.biopha.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Hodgson EK, Fridovich I. The Interaction of Bovine Erythrocyte Superoxide Dismutase With Hydrogen Peroxide: Chemiluminescence and Peroxidation. Biochem. 1975;14:5299–5303. doi: 10.1021/bi00695a011. [DOI] [PubMed] [Google Scholar]
- Kedziora J, Bartosz G. Down’s Syndrome: a Pathology Involving the Lack of Balance of Reactive Oxygen Species. Free Radical Biol Med. 1988;4:317–330. doi: 10.1016/0891-5849(88)90052-4. [DOI] [PubMed] [Google Scholar]
- Lazzarino G, Tavazzi B, Di Pierro D, Giardina B, McCord JM. Superoxide radical as both initiator and terminator of lipid peroxidation: the importance of oxidative balance. In: Asada K, Yoshikawa T, editors. Frontiers of Reactive Oxygen Species in Biology and Medicine. Elsevier Sciences B.V.; 1994. pp. 523–524. [Google Scholar]
- Levy R, Glozman S, Milman D, Seruty C, Hagay Z, Yavin E, Groner Y. Ischemic Reperfusion Brain Injury in Fetal Transgenic Mice With Elevated Levels of Copper-Zinc Superoxide Dismutase. J Perinat Med. 2002;30:158–165. doi: 10.1515/JPM.2002.020. [DOI] [PubMed] [Google Scholar]
- Mao GD, Thomas PD, Lopaschuk GD, Poznansky MJ. Superoxide Dismutase (SOD)-Catalase Conjugates - Role of Hydrogen Peroxide and the Fenton Reaction in SOD Toxicity. J Biol Chem. 1993;268:416–420. [PubMed] [Google Scholar]
- McCord JM. Oxygen-Derived Free Radicals in Post-Ischemic Tissue Injury. N Engl J Med. 1985;312:159–163. doi: 10.1056/NEJM198501173120305. [DOI] [PubMed] [Google Scholar]
- McCord JM. The Evolution of Free Radicals and Oxidative Stress. Am J Med. 2000;108:652–659. doi: 10.1016/s0002-9343(00)00412-5. [DOI] [PubMed] [Google Scholar]
- McCord JM, Fridovich I. Superoxide Dismutase: an Enzymic Function for Erythrocuprein (Hemocuprein) J Biol Chem. 1969;244:6049–6055. [PubMed] [Google Scholar]
- McCord JM, Omar BA, Russell WJ. Sources of oxygen-derived radicals in ischemia-reper-fusion. In: Hayaishi O, Niki E, Kondo M, Yoshikawa T, editors. Medical, Biochemical, and Chemical Aspects of Free Radicals. Elsevier Science; Amsterdam: 1989. pp. 1113–1118. [Google Scholar]
- McCord JM, Russell WJ. Inactivation of Creatine Phosphokinase by Superoxide During Reperfusion Injury. Basic Life Sci. 1988;49:869–873. doi: 10.1007/978-1-4684-5568-7_141. [DOI] [PubMed] [Google Scholar]
- McCord JM, Turrens JF. Mitochondrial Injury by Ischemia and Reperfusion. Curr Topics Bioenerg. 1994;17:173–195. [Google Scholar]
- Menasche P, Grousset C, Gauduel Y, Mouas C, Piwnica A. Enhancement of Cardioplegic Protection With the Free-Radical Scavenger Peroxidase. Circulation. 1986;74:III138–III144. [PubMed] [Google Scholar]
- Myers CL, Weiss SJ, Kirsh MM, Shlafer M. Involvement of Hydrogen Peroxide and Hydroxyl Radical in the ‘Oxygen Paradox’: Reduction of Creatine Kinase Release by Catalase, Allopurinol or Deferoxamine, but Not by Superoxide Dismutase. J Mol Cell Cardiol. 1985;17:675–684. doi: 10.1016/s0022-2828(85)80067-5. [DOI] [PubMed] [Google Scholar]
- Nelson SK, Bose SK, Grunwald GK, Myhill P, McCord JM. The Induction of Human Superoxide Dismutase and Catalase in Vivo: A Fundamentally New Approach to Antioxidant Therapy. Free Radic Biol Med. 2006;40:341–347. doi: 10.1016/j.freeradbiomed.2005.08.043. [DOI] [PubMed] [Google Scholar]
- Nelson SK, Bose SK, McCord JM. The Toxicity of High-Dose Superoxide Dismutase Suggests That Superoxide Can Both Initiate and Terminate Lipid Peroxidation in the Reperfused Heart. Free Radical Biol Med. 1994;16:195–200. doi: 10.1016/0891-5849(94)90143-0. [DOI] [PubMed] [Google Scholar]
- Norris KH, Hornsby PJ. Cytotoxic Effects of Expression of Human Superoxide Dismutase in Bovine Adrenocortical Cells. Mutat Res. 1990;237:95–106. doi: 10.1016/0921-8734(90)90015-j. [DOI] [PubMed] [Google Scholar]
- Omar BA, Gad NM, Jordan MC, Striplin SP, Russell WJ, Downey JM, McCord JM. Cardioprotection by Cu,Zn-Superoxide Dismutase Is Lost at High Doses in the Reoxygenated Heart. Free Radical Biol Med. 1990;9:465–471. doi: 10.1016/0891-5849(90)90123-z. [DOI] [PubMed] [Google Scholar]
- Omar BA, McCord JM. The Cardioprotective Effect of Mn-Superoxide Dismutase Is Lost at High Doses in the Postischemic Isolated Rabbit Heart. Free Radical Biol Med. 1990;9:473–478. doi: 10.1016/0891-5849(90)90124-2. [DOI] [PubMed] [Google Scholar]
- Paraidathathu T, Degroot H, Kehrer JP. Production of Reactive Oxygen by Mitochondria From Normoxic and Hypoxic Rat Heart Tissue. Free Radical Biol Med. 1992;13:289–297. doi: 10.1016/0891-5849(92)90176-h. [DOI] [PubMed] [Google Scholar]
- Rushmore TH, Kong AN. Pharmacogenomics, Regulation and Signaling Pathways of Phase I and II Drug Metabolizing Enzymes. Curr Drug Metab. 2002;3:481–490. doi: 10.2174/1389200023337171. [DOI] [PubMed] [Google Scholar]
- Tamura Y, Chi L, Driscoll EM, Jr, Hoff PT, Freeman BA, Gallagher KP, Lucchesi BR. Superoxide Dismutase Conjugated to Polyethylene Glycol Provides Sustained Protection Against Myocardial Ischemia/Reperfusion Injury in Canine Heart. Circ Res. 1988;63:944–959. doi: 10.1161/01.res.63.5.944. [DOI] [PubMed] [Google Scholar]
- Terada LS, Rubinstein JD, Lesnefsky EJ, Horwitz LD, Leff JA, Repine JE. Existence and Participation of Xanthine Oxidase in Reperfusion Injury of Ischemic Rabbit Myocardium. Am J Physiol Heart Circ Physiol. 1991;260:H805–H810. doi: 10.1152/ajpheart.1991.260.3.H805. [DOI] [PubMed] [Google Scholar]
- Thom SR, Elbuken ME. Oxygen-Dependent Antagonism of Lipid Peroxidation. Free Radical Biol Med. 1991;10:413–426. doi: 10.1016/0891-5849(91)90050-d. [DOI] [PubMed] [Google Scholar]
- Uraizee A, Reimer KA, Murry CE, Jennings RB. Failure of Superoxide Dismutase to Limit Size of Myocardial Infarction After 40 Minutes of Ischemia and 4 Days of Reperfusion in Dogs. Circulation. 1987;75:1237–1248. doi: 10.1161/01.cir.75.6.1237. [DOI] [PubMed] [Google Scholar]
- Werns SW, Shea MJ, Driscoll EM, Cohen C, Abrams GD, Pitt B, Lucchesi BR. The Independent Effects of Oxygen Radical Scavengers on Canine Infarct Size. Reduction by Superoxide Dismutase but Not Catalase. Circ Res. 1985;56:895–898. doi: 10.1161/01.res.56.6.895. [DOI] [PubMed] [Google Scholar]
- Woodward B, Zakaria MN. Effect of Some Free Radical Scavengers on Reperfusion Induced Arrhythmias in the Isolated Rat Heart. J Mol Cell Cardiol. 1985;17:485–493. doi: 10.1016/s0022-2828(85)80053-5. [DOI] [PubMed] [Google Scholar]
- Zhao L, Roche BM, Wessale JL, Kijtawornrat A, Lolly JL, Shemanski D, Hamlin RL. Chronic Xanthine Oxidase Inhibition Following Myocardial Infarction in Rabbits: Effects of Early Versus Delayed Treatment. Life Sci. 2008;82:495–502. doi: 10.1016/j.lfs.2007.12.010. [DOI] [PubMed] [Google Scholar]