Abstract
Objectives:
To describe the growth in the use of state-funded (Medicare) polysomnography (PSG) in Australia since 1990 and to compare PSG growth to other common diagnostic procedures and growth in total Medicare payments.
Methods:
Interrogation of online database of historical census-level data routinely collected by Medicare.
Results:
There has been a steady rise in the number of PSGs performed in Australia since 1990; the growth has been faster than overall Medicare-spending growth and faster than growth in comparable diagnostic procedures. However, there are marked interstate differences in growth. Per capita data, available only for 1995 to 2004, shows that nationwide PSG provision has risen from 123 to 308 per 100,000 people enrolled in Medicare.
Conclusions:
The provision of PSG in Australia has been growing steadily since publicly funded reimbursement began in 1990. This growth has been faster than the overall population growth and faster than the growth in Medicare funding for other diagnostic procedures and classes of medical interventions. However, the provision of PSG might be expected to continue to increase because the per capita provision (308 per 100,000) is still less than recent estimates from Canada and the United States (370.4 and 427.0 per 100,000, respectively).
Citations:
Marshall N; Wilsmore B; McEnvoy D et al. Polysomnography in australia—Trends in provision. J Clin Sleep Med 2007;3(3):281–284
Keywords: Polysomnography, historical data, Australia, provision of service, Medicare
The prevalence of sleep-disordered breathing (which is defined as more than 5 respiratory disturbances per hour of sleep) in Australian men is 25%,1 with similar prevalence estimates being found in other counties.2 Increasingly, sleep-disordered breathing has been recognized as a medical disorder associated with substantial morbidity and mortality.3–7 Polysomnography (PSG) is currently considered the most appropriate method of diagnosing and quantifying the severity of sleep-disordered breathing.8 However, there are no published accounts of longitudinal PSG provision using census-level data from an entire country.
Since December 1989, a procedure fee for PSG has been reimbursed by the Australian national health insurance system, Medicare. Since inception, the procedure fee has included at least 8 channels of recording, including electroencephalography, and requires direct technical supervision and physician interpretation.9 The intent of the fee for PSG was to reimburse procedural fees primarily for inclusion and exclusion of sleep-related breathing disorders, though this has also been used for diagnosis of causes of sleepiness and parasomnias not related to sleep-disordered breathing. In Australia, the government fee covers the procedural cost (equipment, technologist salary, etc.) and medical interpretation of the PSG. If the patient elects to have the test performed in a private, and not a government hospital, a further bed charge can be claimed from the patient's private health fund.
In 1998 to 1999, a compulsory physician-accreditation process involving the Royal Australasian College of Physicians and the Australian Department of Health took place, and tests were subsequently only reimbursed when performed by accredited sleep medicine practitioners, who may be from any physician specialty. Medicare covers all Australians with either citizenship or residency and is responsible for administering payments to medical practitioners for consultations, tests related to medical diagnosis, and surgical procedures. The only exception to this is the payment of such services performed on patients admitted as inpatients to hospitals administered by the state and territory governments of Australia (public hospitals). Because the vast majority of PSG is performed in private centers or as outpatients in public hospitals, it is estimated that Medicare funds more than 85% to 90% of the total number of PSGs performed in Australia.10
Given the increasing awareness of sleep-related breathing disorders and interest in the cost utility of investigating these conditions, we investigated trends in Medicare-funded PSG by demographic and geographic groupings based on data adjusted for Medicare population growth (1995–2004) and also for total PSG since the procedure was first reimbursed in 1990. We also compared PSG growth to other commonly utilized Medicare-funded diagnostic procedures and total Medicare payments.
METHODS
Data on the Medicare Benefits Scheme were obtained from an electronic database (www.medicareaustralia.gov.au). The figures provided include only those services that are performed by a registered provider (post-1998 claims only) and for which a claim has been processed by Medicare. However, the figures do not include a minority of services provided by hospital doctors to public patients in public hospitals. In 2001, Medicare introduced new billing codes for pediatric PSG; however, children, younger than 16 years of age were still regularly classified as having received adult PSGs for 2 years after that date. Before 2001, pediatric PSGs are discernable via attached demographic data (age and sex). Figures given include all of the PSG billing item numbers used over the period 1994 to 2004 inclusive (adult item numbers 12203, 12207; pediatric item numbers 12210, 12213, 12215, 12217), unless otherwise stated. Data from 1990 to 1993 were supplied upon request directly by Medicare. The vast bulk of billing has been done under the 12203 and, since 2001, a supplemental number of pediatric studies under 12210. In 2005, Medicare funded either 75% or 85% (private hospital, government hospital, respectively) of AUD508.90 for an adult PSG and the same ratio for a pediatric PSG of AUD607.40.
Australia is a federation of self-governing states, with some similarities to the state-federal structure in the United States of America, and comprises the states of New South Wales, Victoria, Queensland, South Australia, Tasmania, and Western Australia, as well as 2 self-governing territories—the Australian Capital Territory and the Northern Territory. Within Medicare data, state or territory is determined according to the address (at the time of claiming) of the patient to whom the service was rendered. Services per capita (per 100,000 population) were calculated by dividing the number of services processed in a month by the number of people enrolled in Medicare at the end of that month.
Polysomnography was compared with other common Medicare-claimable procedures such as (1) respiratory function test (item number 11503), which refers to the measurement of respiratory system function performed under the supervision of a consultant physician or in the respiratory laboratory of a hospital and covers a wide variety of testing procedures, including spirometry, inhalation provocation tests, respiratory muscle strength measurement, and limited-channel sleep investigations that do not meet the description of full PSG; (2) 12-lead electrocardiogram (ECG) (item number 11700) refers to a full 12-lead ECG involving the attendance of a medical practitioner; (3) exercise/stress testing measured with ECG (item number 11712) and (4) nonambulatory, non–video-recorded prolonged electroencephalography (item number 11003). The last item number also includes claims made for Multiple Sleep Latency Tests. Diagnostic procedures are also grouped into medical subspecialties such as respiratory and cardiovascular. Total costs for these in 2004 were extracted for comparison of gross spending. The entire billing class covering all diagnostic procedures and investigations (excluding pathology testing and diagnostic imaging) and the overall growth in diagnostic imaging (but excluding magnetic resonance imaging), pathology, and total Medicare were also retrieved from this source.
Data were provided in age groups 0 to 4 years and then by decade to 75+ years. However, only data from 1995 onward were provided with adjustment for services per capita, and, thus, 1995 served as a baseline year for much of the presented data. Raw or gross expenditure and expenditure per capita for PSG were also available. Data were presented as means ± SD, unless otherwise noted.
At the time of submission 1 Australian dollar could buy approximately 75 United States cents. Thus, quick conversion to US dollars can be achieved by multiplying the Australian figures by three-quarters.
RESULTS
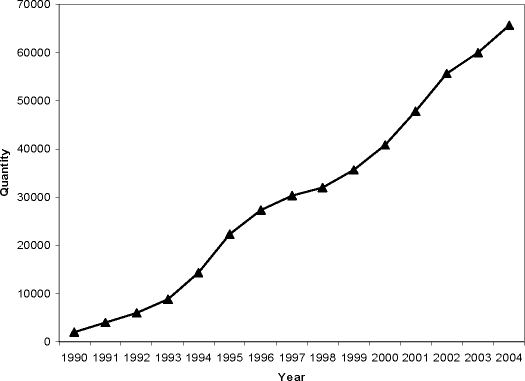
Over a 10-year period (1995–2004) Medicare has paid out AUD162.8 million for 417,533 PSGs (USD 122.1 million, where 1AUD= 0.75 USD). The annual cost of PSGs to the scheme has steadily risen from AUD9.2 million in 1995 to AUD26.7 million in 2004. Growth in supply of PSGs has been relatively consistent over this time period, rising by 4541 ± 2058 procedures per year (mean ± SD, see Figure 1). In 1995, PSG supply per 100,000 Medicare enrollees was 123 per year and increased to 308 per year in 2004, an increase of 150% above population growth.
Figure 1.
Gross number of polysomnography claims per year in Australia (1990–2004).
By comparison, the overall spending for Medicare has increased from AUD5.9 billion in total and AUD124.9 million on diagnostic procedures in 1995 to AUD9.2 billion, with AUD221.7 million spent on diagnostic procedures and investigations in 2004. Total Medicare spending has increased by 36.1% from 1995 above population growth. Spending in 2004 on common diagnostic procedures was as follows: 12-lead ECG (item number 11700 = AUD33.3 million), exercise/stress test ECG (item 11712= AUD33.7 million). Diagnostic procedures grouped according to subspecialty included cardiovascular (AUD88.4 million), respiratory (AUD18.3 million), ophthalmology (AUD23.8 million), otolaryngology (AUD15.1 million), and neurology (AUD20.0 million). PSGs are classed as miscellaneous diagnostic procedures and investigations.
Medicare payments for other common diagnostic procedures (Figure 2) have grown (respiratory function testing) or have remained relatively steady (12-lead ECG and 3-hour nonambulatory electroencephalogram). However, respiratory function testing has not grown as fast as PSG, despite a large component of the growth of the former being due to increasing use of limited-channel sleep studies. By further comparison to PSG, the overall number of diagnostic procedures (Medicare groups for reimbursement) performed per capita has grown by 13.0% over the period 1995 to 2004. Provision of service in other diagnostic categories such as Diagnostic Imaging and Pathology (both Medicare groups) has grown by 15.2% and 37.2% per capita, respectively, over the same period.
Figure 2.
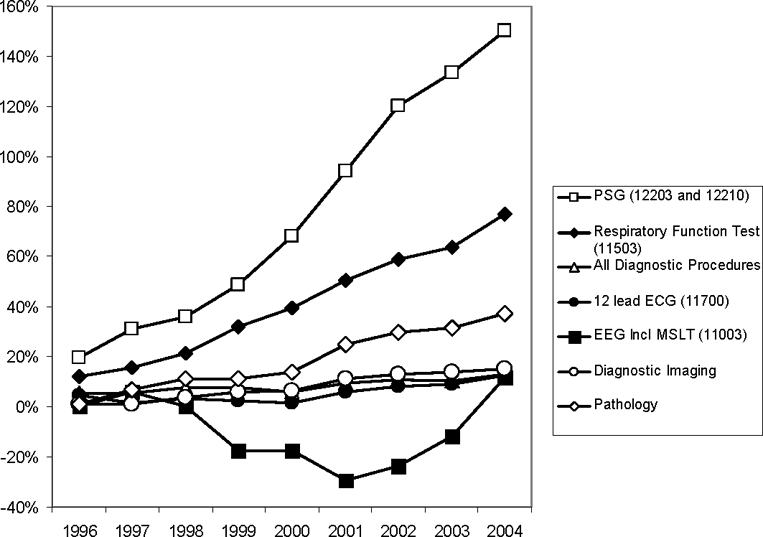
Relative per capita growth in provision of common diagnostic procedures and categories compared with 1995 baseline. PSG refers to polysomnography; ECG, electrocardiogram; EEG, electroencephalogram; MSLT, Multiple Sleep Latency Test.
In 1994, females accounted for 23.1% of PSGs, but, by 2004, this figure had risen to 30.6%. The age structure of people receiving adult PSG (item numbers 12203 and 12210 only) has remained relatively constant. In 1994, children aged 0–14 years accounted for approximately 6.0% of volume (item number 12203 only) whilst by 2004 they accounted for 5.4% (combined item numbers 12203 and 12210 only). Pediatric PSGs have fluctuated between 4.9% and 6.3% of total volume. Other age groups remain similar across the entire time period with middle-aged people (45–64 years) making up just over half of the population.
Nationwide aggregates hide the inter-state differences in the demand growth. Whilst New South Wales had the highest rate of polysomnography claims in 1995 (189 per capita,), Queensland has had the largest increase (from 76 to 398 p.c.), contributed 37% of the gross national growth in PSG (2003–2004 only), and subsequently now provides the most polysomnography studies per capita. Greater population size means that NSW is still the largest provider of PSG and while the PSG provision growth is relatively flat, NSW still accounts for 29% of the raw national growth. Victoria accounts for 26% of raw growth.
DISCUSSION
This is the first census-level description of longitudinal growth in the provision of polysomnography to an entire country. The use of government rebated polysomnography is growing steadily at about 4500 procedures per year or 18.7 ± 7.2 per 100,000 Medicare enrollees. This rate of growth exceeds the growth of the population each year, and exceeds that of other common diagnostic procedures and classes of procedures as well as the growth in Diagnostic Imaging and Pathology provision. Polysomnography cost the Medicare scheme over AUD26.7 million in 2004 (USD 20.0 million), approximately 0.29% of the Medicare budget. In addition, for the period 1994–2005, a total of 417,533 polysomnograms were reimbursed by Medicare. This figure does not include some publicly funded procedures in public hospitals but probably includes the vast majority of PSGs performed in Australia each year. Interestingly the increasing recent use of non-polysomnographic methods to diagnose sleep-disordered breathing (e.g. overnight oximetry) or titrate CPAP therapy (e.g. autotitrating CPAP devices) do not seem to have affected the growth in PSG to this point. Some of the growth in other costs such as bed charges billed by private hospitals for patients having sleep studies may have also increased during this period but these are not included in the figures.
The estimated population of Australia in March of 2005 was 20.4 million (www.abs.govt.au). Potentially this means that a maximum of 1.9% of the population have received Medicare funded polysomnography, although the true figure is probably only 50–66% of the 1.9%, as the major billing codes can include up to three PSGs on the same person in the same year and it is likely that about one third of procedures represent continuous positive airway pressure implementation/titration studies. The prevalence and incidence of treatable obstructive sleep apnoea in the Australian community is unknown, but is likely to be similar to the United States.1 Due to rising obesity levels, obstructive sleep apnea prevalence has been increasing in the USA.11 Similar changes in obstructive sleep apnea prevalence would be expected in Australia, where obesity is an increasing public health problem, particularly in younger people (for review see reference 12).
The 2004 provision of 308 procedures per 100,000 population can be compared to international estimates. Australian provision of PSG is higher than that estimated in the United Kingdom (42.5 per 100K) and Belgium (177.2 per 100K) but is still substantially lower than both Canada and the United States (370.4 and 427.0 per 100K, respectively).10 This suggests that the national growth in PSG services in Australia is likely to continue for some years to come, as there is still a substantial unmet need. Even in the US where service provision of PSG is the highest in the world there is still a high proportion of people with moderate-severe OSA who have not been diagnosed.2,13 Flemons and colleagues10 have calculated that 2310 PSGs per 100,000 people per year would be required to diagnose and treat the prevalence of moderate-severe OSA. This was calculated given an assumption that 50% of diagnostic PSGs would be negative for moderate-severe OSA and a further CPAP titration night would be required for those who did test positive.
It is difficult to estimate the numbers of non-PSG studies being performed for the diagnosis of SDB or implementation of CPAP. This is currently in a major state of flux in Australia though the reality is that Medicare is unlikely to reimburse non-PSG methods specifically unless there is evidence that this approach is associated with at least equivalence in treatment outcomes and reduced costs.
The age mix in those receiving PSG has remained relatively constant with middle aged people predominating. However, the traditional male to female PSG ratio has been decreasing since the mid-nineties and may soon approach the 2 men to 1 women ratio identified in overseas community dwelling populations.2
We observed marked interregional differences in provision of polysomnography. The higher rate of growth in one state (Queensland) may reflect lower threshold for referral, increased use of PSG for CPAP follow-up or possibly more service providers for PSG in that state. Such marked regional disparities in Australia might be instructive with regard to other countries with federal/state systems such as Canada and the United States.
Growth in other diagnostic procedures has been less than PSG, in which service provision has grown by 150% above population since 1995 (see Figure 2). Comparable diagnostic procedures such as 12 lead ECG (12.6%), 3 hour EEG (11.8%), and respiratory function testing (76.9%) have not grown as quickly, nor have the overall growth in diagnostic procedures, diagnostic imaging or pathology services grown as much over population growth (13.0%, 15.2% and 37.2% comparing 1995 to 2004, respectively). However the rapid growth in PSG has been from a low baseline, which tends to exaggerate the percentage increase, and the per capita provision of services and total expenditure in comparison to other diagnostic procedures may be a more valid measure. In addition, it is likely that primary health care recognition of sleep apnea is increasing due to greater undergraduate and postgraduate education.
Indeed, the overall burden on the health system is still small with approximately 0.29% of the Medicare budget spent on PSG in 2004. Medicare Australia generally adjusts fee levels annually by a factor related to the consumer price index but the increase over time has been lower than the CPI rate. For example, the fee for polysomnography in 2000 was 75 or 85% of AUD405.95 compared with 75 or 85% of AUD508.90 in 2005. However, the total cost of PSG is now approaching some common diagnostic procedures, such as 12 lead ECG (item number 11700 AUD33.3 million) and exercise/stress ECG testing (item number 11712 AUD33.7 million) and exceeds spending on all respiratory (AUD18.3 million), ophthalmologic (AUD23.8 million), and neurologic (AUD20.0 million) diagnostic procedures and investigations. These costs only cover the Medicare rebate amount for PSG but not some of the additional costs, including bed charges and the percentage of PSG costs that Medicare does not pay (15% or 25%). These additional charges are currently being met by either the patients' health insurance or directly by the patients themselves. However, data on these exact costs are unavailable but are likely to approximate AUD350 to AUD500 extra per night.10
Nationwide, Medicare PSG costs amounted to AUD26.7 million in 2004 and can be expected to grow by about AUD1.6 to AUD2.5 million per year (USD20.0 million and USD1.2 to 1.9 million per year, respectively). It is possible that some of the growth in PSG reflects increasing recognition of sleep disorders other than sleep apnea. Although PSG in Australia was originally funded to rule-in or rule-out sleep-related breathing disorders, PSG is being used in the diagnosis of narcolepsy or complex movement disorders during sleep.
These data clearly show a consistent pattern of growth of PSG in Australia over the past decade congruent with the increasing recognition of the importance of sleep disorders by physicians and the community. The rate of PSG provision is still well short of what would be expected given the number of PSGs estimated to be required to address the prevalence of treatable obstructive sleep apnea.10 Given the expected prevalence and incidence of sleep disorders, particularly sleep-related breathing disorders in Australia, our data support previous evidence suggesting that most cases of sleep-related breathing disorders remain undiagnosed.2
Footnotes
Disclosure Statement
This is not an industry supported study. Dr. John Wheatley has participated clinical trial research supported by Boehringer-Ingelheim, Pharmaxis-Mannitol, Cephalon, and ResMed. Drs. Marshall, Wilsmore, McEvoy, Michael Dodd, and Dr. Grunstein have indicated no financial conflicts of interest.
REFERENCES
- 1.Bearpark H, Elliot L, Grunstein R, et al. Snoring and sleep apnea: a population study in Australian men. Am J Respir Crit Care Med. 1995;151:1459–65. doi: 10.1164/ajrccm.151.5.7735600. [DOI] [PubMed] [Google Scholar]
- 2.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 3.Peppard P, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 4.Marti S, Sampol G, Munoz X, et al. Mortality in severe sleep apnoea/hypopnoea syndrome patients: impact of treatment. Eur Respir J. 2002;20:1511–8. doi: 10.1183/09031936.02.00306502. [DOI] [PubMed] [Google Scholar]
- 5.Marin J, Carrizo S, Vicente E, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 6.Shahar E, Whitney C, Redline S, et al. Sleep disordered breathing and cardiovascular diseases: cross sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 7.Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 8.Kushida C, Littner M, Morganthaler T, et al. Practice Parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499–521. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]
- 9.Medicare Benefits Schedule Book. Canberra: Commonwealth of Australia; 2005. [Google Scholar]
- 10.Flemons WW, Douglas NJ, Kuna ST, et al. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004;169:668–72. doi: 10.1164/rccm.200308-1124PP. [DOI] [PubMed] [Google Scholar]
- 11.Newman AB, Foster G, Givelber R, et al. Progression and regression of sleep-disordered breathing with changes in weight: the Sleep Heart Health Study. Arch Intern Med. 2005;165:2408–13. doi: 10.1001/archinte.165.20.2408. [DOI] [PubMed] [Google Scholar]
- 12.Thorburn AW. Prevalence of obesity in Australia. Obes Rev. 2005;6:187–9. doi: 10.1111/j.1467-789X.2005.00187.x. [DOI] [PubMed] [Google Scholar]
- 13.Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20:705–6. doi: 10.1093/sleep/20.9.705. [DOI] [PubMed] [Google Scholar]