Abstract
We report a patient with severe obstructive sleep apnea syndrome, diabetes mellitus, and hypertension, with postoperative complications following tracheostomy. His stormy postoperative course is presented with emphasis on glycemic control and hypertension. We present a cautionary tale of a significant reduction in medications to control blood pressure and hyperglycemia following tracheostomy for severe OSA. The severe reduction in blood pressure and hypoglycemia could mimic sepsis and clinicans need to be vigilant to these dramatic effects following tracheostomy and appropriately adjust baseline medications.
Citations:
Bhimaraj A; Havaligi N; Ramachandran S. Rapid reduction of antihypertensive medications and insulin requirements after tracheostomy in a patient with severe obstructive sleep apnea syndrome. J Clin Sleep Med 2007;3(3):297–299
Keywords: Sleep apnea, insulin resistance, hypertension
Obstructive sleep apnea syndrome (OSA) affects 2–4% of the general population.1 Irrespective of the type of sleep apnea (central versus obstructive), epidemiologic studies have indicated its independent association with hypertension2 and cardiovascular disease.3 Also, there is emerging evidence suggesting that sleep disordered breathing (SDB) has an association with fasting hyperglycemia, insulin resistance, and type 2 diabetes mellitus.4,5 The impact of tracheostomy for severe obstructive sleep apnea syndrome on glycemic control has not been previously reported.
CASE REPORT
RR is a 58-year-old African American male with history of longstanding hypertension, obesity, type 2 diabetes mellitus, chronic kidney disease, congestive heart failure, sinus node dysfunction status post permanent pacemaker placement, coronary artery disease, and severe obstructive sleep apnea. He had a body mass index of 32. His baseline blood pressures were in the range of 140–160 mm Hg systolic and 70–90 mm Hg diastolic.
An overnight sleep study prior to admission documented severe OSA, with an apnea-hypopnea index (AHI) of 54/hr and oxygen desaturation to 66%. He failed continuous positive airway pressure titration and was subsequently titrated to a bilevel (BiPAP®) setting of 15/9 cms of H20 with 3 liters/minute of oxygen. Despite compliance with bilevel therapy, he continued to have clinical and echocardiographic evidence of cor pulmonale with an oxygen saturation of 82%. He was admitted for an elective tracheostomy for intractable obstructive sleep apnea syndrome.
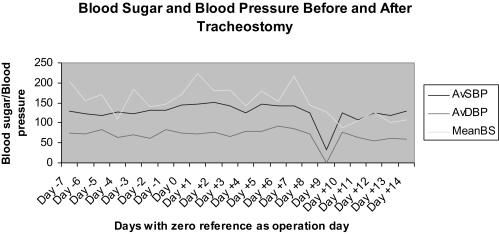
His outpatient medications included: insulin glargine, 60 U at bedtime: insulin NPH, 30 U before meals, carvedilol, 25 mg twice daily, hydrochlorthiazide, 25 mg daily, amlodipine 5mg daily, furosemide 80 mg in the morning and 40 mg in the evening; isosorbide mononitrate 60 mg daily, irbesartan 300 mg daily, and hydralazine 25 mg every 8 hours. On admission, his insulin dosage was reduced to 30 U insulin glargine due to anticipated decreased oral intake in the hospital. None of his other medications were changed. Post tracheostomy, the patient was monitored in the ICU as a routine protocol and transferred back to the floor on the third postoperative day. During his ICU stay, both his antihypertensive medications and insulin were held as the patient was kept nil per oral (patient had refused feeding through a nasogastric tube). After clearing a swallow evaluation, the patient was placed back on oral medications and food on postoperative day 7. As the patient was getting ready to be discharged, on day 9, he complained of dizziness and had a blood pressure measurement of 60/0 and blood sugar of 47 and was transferred to the ICU. As the patient was post tracheostomy, empiric antibiotics were initiated at the time of transfer to the ICU for possible hospital associated pneumonia. They were later discontinued once the chest radiograph and cultures were found to be negative. His blood pressure was stabilized by the next day. His antihypertensive medications were reduced to irbesartan, 150 mg daily, carvedilol, 12.5 mg twice daily, and furosemide 40mg daily. Amlodipine, isosorbide mononitrate, and hydralazine were discontinued. His insulin dosage was reduced to insulin glargine 20 U at bedtime and insulin aspart 7 U before meals. Figure 1 trends the changes in blood pressure and glycemic control before and after tracheostomy.
Figure 1.
Blood Sugar and Blood Pressure Before and After Tracheostomy. (AvSBP: Average systolic blood pressure; AvDBP: Average diastolic blood pressure; BS: Blood sugar)
He was finally discharged on furosemide, 40 mg daily, irbesartan, 150 mg daily; carvedilol, 12.5 mg twice daily; insulin glargine, 20 U at bedtime; and insulin aspart, 7 U before meals. He was also advised to closely monitor his blood sugar and blood pressure with the help of the visiting nurse and primary care physician.
DISCUSSION
Excess sympathetic activity is a consistent finding in patients with sleep apnea syndrome and is presumed to contribute to the high incidence of hypertension and altered glycemic control. The use of CPAP has been shown to improve insulin sensitivity and control of blood pressure in patients with OSA.6–10 There is some data exploring these relationships following tracheostomy.11–12 A significant correlation between urinary norepinephrine and the respiratory disturbance index has been reported.13 Fletcher and colleagues showed normalization of urinary catecholamine excretion after long-term use of CPAP and following tracheostomy for severe sleep apnea.10 This normalization of catecholamine surge following a definitive treatment for OSA is rapid, has an impact on glycemic control and on blood pressure and could mimic severe sepsis. A simple explanation for the reason this patient's blood pressure and sugar dropped on post operative day 9 could be that his antihypertensive and insulin medications were restarted on day 7 when he was able to tolerate oral feeding.
Hypoxia has also been known to cause activation of certain transcription factors such as hypoxia-inducible factor-1 and nuclear factor-kB; which in turn increase the expression of a number of genes such as those encoding endothelin-1, a potent vasoconstrictor with proinflammatory properties.14 Hypoxia also suppresses the transcriptional rate of endothelial nitric oxide synthase, resulting in decreased production of nitric oxide, which is vasodilatory and has anti-mitogenic properties.15 These effects have also been seen with intermittent hypoxia, and reoxygenation may contribute to oxidative stress by delivering oxygen molecules for production of oxygen free radicals.16 When the hypoxemia-reoxygenation stress is taken away by means of tracheostomy, one might see the immediate effects of the decreased sympathetic drive as a drop in blood pressure. In addition, we postulate that as a delayed effect one might see sustained decrease in blood pressure and glucose as a result of decrease in production of endothelin-1 and increase in nitric oxide levels.
We present a cautionary tale of a significant reduction in medications to control blood pressure and hyperglycemia following tracheostomy for severe OSA. Clinicans need to be vigilant for these dramatic effects.
Footnotes
Disclosure Statement
This is not an industry supported study. Drs. Bhimaraj, Havaligi, and Ramachandran have indicated no financial conflicts of interest.
REFERENCES
- 1.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstrucive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.Robinson GV, Stradling JR, Davies RJ. Obstructive sleep apnea/hypopnea syndrome and hypertension. Thorax. 2004;59:1089–94. doi: 10.1136/thx.2003.015875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton GS, Solin P, Naughton MT. Obstructive sleep apnea and cardiovascular disease. Intern Med J. 2004;34:420–6. doi: 10.1111/j.1445-5994.2004.00596.x. [DOI] [PubMed] [Google Scholar]
- 4.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O'Donnell CP. Sleep-disordered breathing, glucose intolerance and insulin resistance. Respir Physiol Neurobiol. 2003;136:167–78. doi: 10.1016/s1569-9048(03)00079-x. [DOI] [PubMed] [Google Scholar]
- 5.Punjabi NM. Shahar E. Redline S, Gottlieb DJ, Givelber R, Resnick; Sleep Heart Health Study Investigators. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am J Epidemiol. 2004;160:521–30. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 6.Brooks B, Cistulli PA, Borkman M, et al. Obstructive sleep apnea in obese noninsulin-dependent diabetic patients: effect of continuous positive airway pressure treatment on insulin responsiveness. J Clin Endocrinol Metab. 1994;79:1681–85. doi: 10.1210/jcem.79.6.7989475. [DOI] [PubMed] [Google Scholar]
- 7.Cooper BG, White JE, Ashworth LA, Alberti KG, Gibson GJ. Hormonal and metabolic profiles in subjects with obstructive sleep apnea syndrome and the acute effects of nasal continuous positive airway pressure (CPAP) treatment. Sleep. 1995;18:172–9. [PubMed] [Google Scholar]
- 8.Harsch IA, Schahin SP, Radespiel-Troger M, et al. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2004;169:156–62. doi: 10.1164/rccm.200302-206OC. [DOI] [PubMed] [Google Scholar]
- 9.Babu AR, Herdegen J, Fogelfeld L, Shott S, Mazzone T. Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch Intern Med. 2005;165:447–52. doi: 10.1001/archinte.165.4.447. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher EC, Miller J, Schaaf JW, Fletcher JG. Urinary catecholamines before and after tracheostomy in obstructive sleep apnea and hypertension. Sleep. 1987;10:35–44. doi: 10.1093/sleep/10.1.35. [DOI] [PubMed] [Google Scholar]
- 11.Guilleminault C, Simmons FB, Motta J, et al. Obstructive sleep apnea syndrome and tracheostomy:long term follow up experience. Arch Intern Med. 1981;141:985–8. [PubMed] [Google Scholar]
- 12.Sher AE. Upper airway surgery for obstructive sleep apnea. Sleep Med Rev. 2002;6:195–212. doi: 10.1053/smrv.2002.0242. [DOI] [PubMed] [Google Scholar]
- 13.Dimsdale JE, Coy T, Ziegler MG, et al. The effect of sleep apnea on plasma and urinary catecholamines. Sleep. 1995;18:377–81. [PubMed] [Google Scholar]
- 14.Aoki M, Nata T, Morishita R, et al. Endothelial apoptosis induced by oxidative stress through activation of NF-kB: Antiapoptotic effect of antioxidant agents on endothelial cells. Hypertension. 2001;38:48–55. doi: 10.1161/01.hyp.38.1.48. [DOI] [PubMed] [Google Scholar]
- 15.Phelan MW, Faller DV. Hypoxia decreases constitutive nitric oxide synthase transcript and protein in cultured endothelial cells. J Cell Physiol. 1996;167:469–76. doi: 10.1002/(SICI)1097-4652(199606)167:3<469::AID-JCP11>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 16.Kanagy NL, Walker BR, Nelin LD. Role of endothelin in intermittent hypoxia-induced hypertension. Hypertension. 2001;37:511–15. doi: 10.1161/01.hyp.37.2.511. [DOI] [PubMed] [Google Scholar]