Abstract
While the literature suggests lateral unicondylar knee arthroplasty (UKA) improves function in the short- and medium-term, it is less clear on longer-term function. We asked (1) whether lateral UKA improved longer-term Knee Society scores and return to previous activity level); (2) whether there were any concerning longer-term radiographic findings (the Knee Society roentgenographic evaluation and scoring system); and (3) whether lateral UKA was durable as measured by survivorship to revision at 10 and 16 years. We retrospectively reviewed 39 patients with 40 lateral cemented metal-backed UKA. The patients had a mean age of 61 years at surgery. The etiologies were primary osteoarthritis in 24 knees, posttraumatic in 12 cases, and osteonecrosis in four cases. We performed clinical and radiographic evaluations at a minimum followup of 3 years (mean, 12.6 years; range, 3–23 years). Prostheses survivorship was 92% at 10 years and 84% at 16 years. Despite the limited number of indications and technical considerations, our data suggest lateral UKA is a reasonable alternative for isolated lateral femorotibial compartment disease.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Unicompartmental femorotibial osteoarthritis usually affects the medial compartment of the knee and more rarely the lateral compartment [24]. The lateral compartment is involved in 5% to 10% of unicompartmental femorotibial arthroplasty cases [32, 33]. The surgical options for lateral femorotibial osteoarthritis include osteotomy for correction of a valgus deformity and arthroplasty, either total (TKA) or unicompartmental (UKA) [17]. Various tibial or femoral osteotomies have been advocated to correct valgus deformities with a partial loss of cartilage thickness [17]. The results of these different types of osteotomy remain controversial [17]. When there is full loss of cartilage in the affected compartment, osteotomy is usually no longer considered and UKA offers an alternative to TKA when the other compartments are preserved [12, 13, 17, 32, 33]. UKA has several potential advantages compared with TKA such as reduced morbidity, quicker recovery, the preservation of bone stock, and a more physiological knee function [2–4, 32]. Midterm and long-term studies suggest reasonable outcome at 10 years with survivorship greater than 95% of UKA performed for medial osteoarthritis or osteonecrosis [2, 29], but limited long-term followup data are available for lateral UKA in the literature [5, 14, 17, 30, 32]. The authors of one small series of UKA in the lateral compartment reported only one failure out of 19 patients at 89 months of followup [22]. Recently, two other series reported high functional scores without revision at 5.2 years for one and at 12.4 years for another [30, 32].
Both the anatomic and biomechanical characteristics are different in each of the knee femorotibial compartments [5, 32], and similar surgical treatment may not provide reproducible results when applied to a different compartment [5, 32]. Furthermore, UKA in the lateral compartment has been described as technically more challenging and 10 times less performed than medial UKA, thus representing less than 1% of all knee arthroplasty procedures [33]. These facts may explain the limited data available concerning outcomes of lateral UKA [33].
We therefore asked (1) whether lateral UKA improved longer-term Knee Society scores and return to previous activity level; (2) whether there were any concerning longer-term radiographic findings (the Knee Society roentgenographic evaluation and scoring system); and (3) whether lateral UKA was durable as measured by survivorship to revision at 10 and 16 years for the patients operated on before or after 1989.
Materials and Methods
We retrospectively reviewed all 39 patients treated with isolated lateral UKA (40 knees) with a diagnosis of lateral unicompartmental osteoarthritis of the knee or idiopathic osteonecrosis between February 1982 and December 2004. The indication for the procedure was isolated lateral osteoarthritis or osteonecrosis associated with loss of articular cartilage in the involved compartment of at least Grade 2 according to the Ahlback classification [1]. The inclusion criteria were a minimum clinical followup of 3 years, a confirmed diagnosis of isolated lateral unicompartmental osteoarthritis (Ahlback [1] Grade 2 or greater), or osteonecrosis with a full thickness of the articular cartilage in the medial compartment and preserved status of the patellofemoral joint (based on clinical evaluation and skyview radiographs), a preoperative range of knee flexion greater than 100° associated with a full range of knee extension, and a knee clinically stable in the frontal and sagittal planes. The absence of valgus deformity was not an exclusion criterion. After 1989, varus and valgus stress radiographs were also performed to evaluate the opposite femorotibial compartment and the correction of the deformity [15]. A full loss of cartilage on the opposite compartment or a fixed deformity observed on the stress radiograph was considered exclusion criteria after 1989 [15]. During the study period on a total number of 881 UKAs performed at our institution, 40 (4.5%) of them were performed as isolated lateral UKA, whereas 703 (80%) were performed as isolated medial UKA and 138 (15.5%) as an association of a lateral UKA with a medial UKA (115 knees), a patellofemoral arthroplasty (four knees), or a medial UKA and a patellofemoral arthroplasty (19 knees). There were 24 women and 15 men in the series with 22 right knees and 18 left knees. The mean age of the patients at the time of surgery was 61 ± 7 years (range, 34–79 years). The mean body mass index of the patients was 26 ± 5 kg/m2 (range, 18–43 kg/m2). According to the Ahlback classification [1], two knees (5%) were Grade 2, seven (17%) were Grade 3, and 31 (78%) were Grade 4. The etiologies of the lateral osteoarthritis were primary osteoarthritis in 24 knees (60%), posttraumatic (after a tibial plateau fracture) in 12 cases (30%), and secondary to osteonecrosis in four cases (10%). In this series, 31 (77%) patients were engaged in labor or sporting activities. Three of the 39 patients died before this review (at 12 years for one patient and at 13 years for two other patients), but data were available from the last followup before their death (1 year before) and we used these data for the final analysis. Two patients were lost to followup. Thus, 38 knees in 37 patients were available for final analysis. Approval of the local ethical committee was obtained.
All surgery was performed by the two senior authors (JNA, JMA). The surgical approach was a standard medial parapatellar approach until 2000 for 34 cases (85%) and then a so-called minimally invasive lateral approach [4] with lateral arthrotomy for six cases (15%). All components were cemented on the tibial and femoral side. Between 1982 and 1989, 15 Marmor-like (Zimmer, Warsaw, IN) (two patients lost to followup had a Marmor-like UKA, leaving 13 Marmor-like for the final evaluation) and one Alpina (Biomet, Bridgend, UK) were implanted. After 1989, UKAs were performed with new dedicated instrumentation and modern ancillaries, including tibial and femoral cutting guides. Then, 24 UKAs were performed with these ancillaries, including 20 Miller-Galante and four ZUK (Zimmer). In the series, mean polyethylene thickness of the tibial insert was 9 mm (range, 6–17 mm). Postoperative rehabilitation protocols included immediate weightbearing protected by crutches during the first 2 or 3 weeks according to patient tolerance and exercises were focused on passive flexion immediately and then active recuperation of flexion and extension. All patients in the present study received routine prophylaxis with low-molecular-weight heparin pre- and postoperatively for 21 days.
All patients were evaluated clinically preoperatively, at 3 months postoperatively, at yearly intervals postoperatively, and at last followup by an independent observer (YCB) using the Knee Society knee and function score [18]. The arc of knee flexion was recorded preoperatively, during followup, and at the final evaluation. For the patients operated on in the 1980s, the data collected on the standardized knee sheet used in the department during this period were used to calculate the Knee Society score [18]. Patient satisfaction regarding the procedure was assessed using a four-level scale (enthusiastic, satisfied, no change, not satisfied) previously used for evaluation of outcomes after UKA [2, 29]. At last clinical followup, patients were also asked whether they were back to their previous level of activity [29].
Radiographic evaluation was performed by one independent observer (SP) on long-leg radiographs and on anteroposterior (AP), lateral, and skyline radiographs of the knee at last followup. The lower limb alignment was assessed on long-leg radiographs performed using a standardized protocol in which the patient stood with the patella facing anteriorly. On these long-leg radiographs, pre- and postoperatively, the femoral angle (CH = condylar axis to hip center), the tibial angle (PA = plateau axis to ankle), and the articular deformation (CP = condylar axis and plateau axis) were calculated. Then the hip-knee-ankle angle was calculated as the sum of the three previously defined angles (HKA = CH + PA + CP) considering CP as positive in case of lateral convergence [8, 9]. Postoperative alignments of the femoral and tibial components as well as the postoperative alignment of the limb were assessed using the same method on long-leg radiographs performed using the same standardized protocol as preoperatively [8, 9]. The presence, extent, or progression of femoral or tibial radiolucencies according to the Knee Society roentgenographic score was evaluated on full tangential AP and lateral radiographs [18]. Furthermore, progression of osteoarthritis was evaluated in the medial compartment on AP radiographs and in the patellofemoral joint on skyline radiographs performed according to the same protocol as preoperatively. The Ahlback classification was used to evaluate the osteoarthritis progression in the medial or femoropatellar compartment [1].
Patient demographics were described using means and standard deviations or medians and ranges for continuous variables and counts (percent) for categorical variables. Clinical improvement between the pre- and postoperative evaluation as described by the mean Knee Society knee and function score was analyzed using a t test for paired comparisons. We compared the pre- and postoperative alignment. Finally, 10-year and 16-year survival analysis was performed using the Kaplan-Meier technique (with 95% confidence intervals) for all patients considering revision for any reason or radiographic loosening as the endpoint [19]. We performed a log rank survivorship comparison to compare the results of the patients operated on before or after 1989 [14]. Analysis was performed using SPSS software (version 12; SPSS Inc, Chicago, IL). All calculations assumed two-tailed tests.
Results
The Knee Society knee and function scores [18] improved (p = 0.000134 and p = 0.00023) after lateral UKA between the preoperative and the final evaluation at a minimum followup of 3 years (mean, 12.6 ± 4.2 years; range, 3–23 years) for the 38 knees available (Table 1). Preoperatively, the mean active knee flexion was 115° ± 8° (range, 100°–135°) and 134° ± 7° (range, 122°–153°) at final followup. All but 10 patients returned to their preoperative activity level (63%). At the time of the final followup, 23 patients (62.3%) were enthusiastic regarding the procedure, nine patients (24.3%) were satisfied, one patient (2.7%) reported no change, and four patients (10.7%) were not satisfied. One was not satisfied with the lateral UKA result because of a patellar fracture with remaining pain and three others because they required early revision of the lateral UKA (two knees for osteoarthritis progression at 1 year and 2.8 years and the last one for tibial loosening after a tibial plateau fracture requiring revision to a TKA 11 months after the lateral UKA).
Table 1.
Pre- and postoperative values of Knee Society knee and function scores
| Knee Society score type | Preoperative mean ± SD (range) | Postoperative mean ± SD (range) | p Value |
|---|---|---|---|
| Knee | 57 ± 10 (35–75) | 88 ± 5 (40–100) | 0.000134 |
| Function | 46 ± 5 (10–89) | 78 ± 3 (20–100) | 0.00023 |
SD = standard deviation.
The mean preoperative HKA angle was 188° (range, 184°–195°). Postoperatively, the mean HKA angle was 183° ± 2° (range, 181°–186°). The mean AP axis of the tibial component was 90° ± 3° (range, 87°–92°) and the mean tibial slope was 3° ± 4° (range, 0°–8°). The mean AP femoral axis was 91° ± 5° (range, 88°–94°). Four knees (10%) showed radiolucencies (less than 1 mm) at the tibial bone-cement interface without any sign of progression after 5 years of followup. No femoral radiolucencies were observed. Four knees underwent revision for symptomatic osteoarthritis (OA) progression at 1 year, 2.8 years, 9.8 years, and 13.7 years. At final followup, six knees presented isolated asymptomatic (without any change in the clinical score) OA progression in the medial compartment (Fig. 1) (from normal at the time of surgery to Ahlback Grade 1 at the last evaluation [1]) and five knees presented isolated asymptomatic OA progression in both the medial and patellofemoral compartments (from normal at the time of surgery to Ahlback Grade 1 at the last evaluation) [1].
Fig. 1.

This anteroposterior radiograph of the knee shows asymptomatic osteoarthritis progression in the medial compartment.
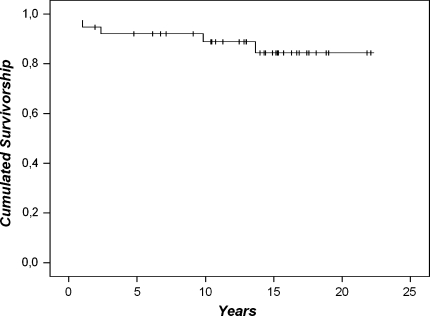
Considering revision for any reason as the endpoint, the 10-year survivorship was 92% (95% confidence interval, 0.79–0.99) and the 16-year survivorship was 84% (95% confidence interval, 0.71–0.97) (Fig. 2).
Fig. 2.
A Kaplan-Meier survivorship analysis curve with revision for any reason as the endpoint is shown. The 10-year survivorship was 92% (95% confidence interval, 0.79–0.99) and the 16-year survivorship was 84% (95% confidence interval, 0.71–0.97).
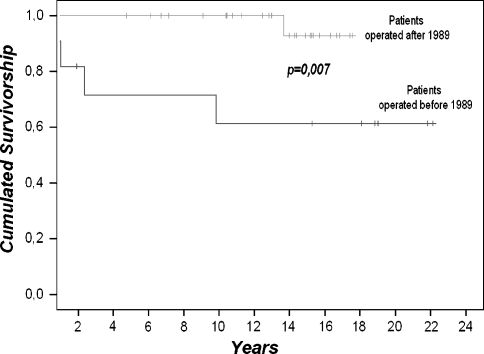
We observed no intraoperative complications. Three patients had postoperative deep venous thromboses and were treated with a therapeutic dose of low-molecular-weight heparin. Five knees required a revision and two knees were reoperated on without implant removal, one for traumatic patellar fracture at 10 years on a well-functioning knee treated with open reduction and internal fixation with a poor result and a remaining painful patella. One knee had limited motion after 2 years as a result of arthrofibrosis and was arthroscopically treated with a satisfactory outcome. Four knees were revised for substantial and painful progression of OA in the medial compartment in three cases and in the patellofemoral compartment in one case. For two of these four knees, a bicompartmental arthroplasty was performed in one case at 1 year by adding a medial UKA and in the other case by adding a patellofemoral arthroplasty at 2.4 years. At final followup, 10 years for the patient with the lateral and medial UKAs and 12 years for the patient with the medial UKA and the patellofemoral arthroplasty, the Knee Society knee score was, respectively, 80 and 85 and the Knee Society function score, respectively, 75 and 80. Radiographic evaluation showed no sign of implant loosening or OA progression in the remaining nonresurfaced compartment. The two remaining knees presenting with painful OA progression were revised using a TKA at 9.8 years and 13.7 years. Finally, one knee was revised with a standard posterostabilized TKA for tibial loosening at 11 months secondary to a tibial plateau fracture with a satisfactory outcome at final followup. Four of these five knees were in the group operated on before 1989 and one was in the group operated on after 1989. The group operated on after 1989 had a higher (p = 0.007) survival than the group operated on before 1989 (Fig. 3).
Fig. 3.
Kaplan-Meier survivorship using revision as an endpoint in the group of patients operated on before 1989 and for the patients operated on after 1989 are shown. The log rank test demonstrated a difference in survivorship between the two groups (p = 0.007).
Discussion
Besides osteotomy for correction of a valgus deformity [17], surgical treatment of lateral femorotibial OA includes either total or unicompartmental arthroplasty [5, 11, 13, 17, 21]. When there is full loss of cartilage in the affected compartment, UKA may offer an alternative to TKA when the other compartments are preserved with the potential advantage of reduced morbidity and preservation of bone stock [2, 12]. Limited long-term followup data are available for lateral UKA in the literature [13, 22, 27, 32, 33] compared with the well-known functional outcomes reported for medial UKA [2, 10]. We therefore asked (1) whether lateral UKA improved longer-term Knee Society scores and return to previous activity level); (2) whether there were any concerning longer-term radiographic findings (the Knee Society roentgenographic evaluation and scoring system); and (3) whether lateral UKA was durable as measured by survivorship to revision at 10 and 16 years for the patients operated on before or after 1989.
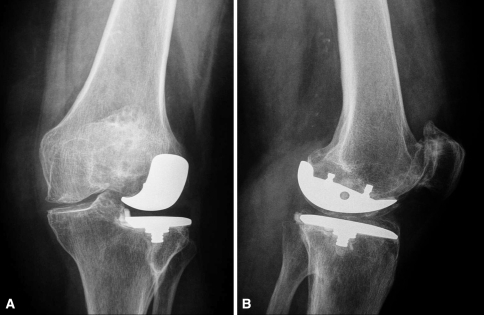
Some limitations should be noted. First, we included different types of implants performed during a long time period with a major evolution in both the ancillaries and the implants over that time. Second, we did not match our patients with patients operated on for a medial UKA during the study period to directly compare the results of medial and lateral UKA. As a result of the relatively small number of patients, we were unable to determine any influence of potentially confounding factors such as age, gender, body mass index, and activity. We were also unable to use any knee-specific quality-of-life score to describe the functional results of the patients such as the Knee Osteoarthritis Outcomes Score [28]. Despite these limitations, we report a relatively homogenous and continuous series of patients operated on in the same department for a lateral UKA by the two senior authors (JNA, JMA) using a cemented fixed-bearing, metal-backed implant. Furthermore, the mean followup (12.6 ± 4.2 years) is one of the longest reported in the literature with patients followed over 23 years (Fig. 4A–B) [5, 13, 17, 22, 27, 30, 32, 33]. Finally, to consider the changes concerning the implants and the indications over time, we performed a direct comparison of the survivorship between the group of patients operated on before 1989 and the group of patients operated on after 1989.
Fig. 4A–B.
These radiographs show a well-functioning lateral unicondylar knee arthroplasty 23 years after implantation from (A) the anteroposterior view and (B) the mediolateral view.
Our data demonstrate lateral UKA can provide reasonable clinical and radiographic results, and the survivorship at 10 and 16 years is comparable to the survivorship obtained for medial UKA in the literature (Table 2) [2, 5, 6, 10, 16, 17, 22, 23, 25–27, 30–32, 34]. Our results at a maximum followup of 23 years ranged between the results of the old and recent studies of lateral UKA reported in the literature [5, 13, 17, 22, 27, 30, 32, 33]. Recent studies reported a very low failure rate, whereas the results of older series were more controversial [5, 13, 17, 22, 27, 30, 32, 33]. Comparing the earlier with the later operated patients, we observed an improvement in the results. This improvement may relate to several factors. First is an improvement of patient selection as illustrated by the two cases revised before 3 years for arthritis progression in the 1980s (group of patients operated on before 1989). The routine use of stress radiographs in varus and valgus to evaluate the opposite femorotibial compartment and the correction of the deformity as well as the contraindications of UKA in case of full loss of patellofemoral cartilage on the skyline views may have played an important role for better patient selection [2, 4, 29]. Second, during the 1980s, very limited instrumentation was available and most of the cuts were handmade based on a resurfacing concept. Our case of early tibial implant migration was consecutive to a tibial plateau fracture probably linked to a technical error resulting from this limited instrumentation. Gunther et al. [17] reported a 21% failure rate using the mobile-bearing Oxford unicompartmental prosthesis in the lateral compartment with a 10% rate of bearing dislocation. This difference with the commonly reported high functioning long-term outcomes using the same implant for the medial compartment may be explained by the amount of femoral translation of the lateral condyle while the medial one remains fairly stationary [17]. When studying the in vivo kinematics of patients implanted with either a medial or lateral UKA, we showed an important posterior femoral translation of the lateral condyle during flexion compared with the medial one [3]. According to these results and as a result of the biomechanical properties of the lateral compartment, fixed-bearing implants seem more appropriate [3]. Thus, two recent studies report more favorable results using fixed-bearing UKA at mid- or long-term followup [30, 32]. Sah and Scott [32] reported no revision at 5 years in a group of 49 knees implanted with lateral UKA, as did Pennington et al. [30] in a group of 29 knees at 12 years followup. The rate of radiolucencies observed in our series (10% of nonprogressive tibial radiolucencies) is comparable with those observed in previous series of lateral UKA at the same followup [27, 30, 32]. Although original reports comparing medial and lateral UKA were conflicting, the results of our series concerning the group of patients operated on after 1989 were comparable with those reported by Pennington et al. [30] and by Sah and Scott [32] and compares favorably with the results of medial UKA [2, 5, 13, 17, 22, 27].
Table 2.
Results of the different series of medial and lateral UKA in the literature
| Authors | Date of publication | Number of evaluated UKAs | Type of implant | Number of surgeons | Mean followup (years)* | Survivorship (number of revisions) |
|---|---|---|---|---|---|---|
| Medial UKA | ||||||
| Marmor [23] | 1986 | 53 | Cemented all poly tibia | 1 | 11 (10–13) | 70% at 10 years (20) |
| Squire et al. [34] | 1999 | 48 | Cemented all poly tibia | 1 | 18 (15.8–21.8) | 84% at 22 years (5) |
| Argenson et al. [2] | 2002 | 145 | Cemented, metal-backed, fixed-bearing | 2 | 5.5 (3–9.33) | 94% at 10 years (5) |
| Perkins and Gunckle [31] | 2002 | 40 | Cemented, metal-backed (60%); all poly (40%) | 1 | 6 (3–10) | 74% at 10 years (6) |
| Gioe et al. [16] | 2003 | 474 | Nine different designs | 23 | NA | 88.6% at 10 years (36) |
| Naudie et al. [25] | 2004 | 113 | Cemented, metal-backed, fixed-bearing | NA | 10 (2–14) | 86 % at 10 years (11) |
| Berger et al. [6] | 2005 | 62 | Cemented, metal-backed, fixed-bearing | 3 | 12 (10–13) | 95.7 % at 13years (2) |
| O’Rourke et al. [26] | 2005 | 122 | Cemented all poly tibia | 1 | 24 (17–28) | 72% at 25 years (17) |
| Eickmann et al. [10] | 2006 | 411 | 12 different designs | 1 | 9 (0.1–19.3) | 80% at 9 years (96) |
| Lateral UKA | ||||||
| Marmor [22] | 1983 | 14 | Cemented all poly tibia | 1 | 7.4 (2.5–9.83) | NA (2) |
| Gunther et al. [17] | 1996 | 53 | Cemented, metal-backed, mobile-bearing | 2 | 5 (2.5–9.83) | 82% at 5 years (11) |
| Ohdera et al. [27] | 2001 | 18 | Four different designs | NA | 8.25 (5–15.75) | NA (2) |
| Ashraf et al. [5] | 2002 | 83 | Cemented all poly tibia | 4 | 9 (2–21) | 74% at 15years (15) |
| O’Rourke et al. [26] | 2005 | 14 | Cemented all poly tibia | 1 | 24 (17–28) | 72% at 25 years (2) |
| Pennington et al. [30] | 2006 | 29 | Cemented, metal-backed (75%); all poly tibia (25%) | NA | 12.4 (3.1–15.6) | 100% at 12.4 years (0) |
| Sah and Scott [32] | 2007 | 49 | Three different designs | 1 | 5.2 (2–14) | 100% at 5.4 years (0) |
| Our series | 38 | Four different designs | 2 | 12.6 (3–23) | 84% at 16 years (5) | |
* Ranges in parentheses; UKA = unicondylar knee arthroplasty; NA = not available.
Because both the anatomic and the biomechanical characteristics are different in each of the knee’s femorotibial compartments, some surgical considerations may be outlined for the lateral compartment [3, 7, 35]. The rule of undercorrection of the deformity should be strictly applied to lateral UKA [27] to avoid medial OA progression. Furthermore, the positioning of the femoral component should accommodate the femoral divergence of the lateral condyle when the knee is flexed to avoid impingement with the tibial spines when brought into extension [7]. The mediolateral positioning of the femoral component should also avoid the excessive lateral placement in extension, which may lead to an overload of the lateral part of the tibial plateau when the knee is flexed 30° [7]. Additionally, internal rotation of the tibial component when performing lateral UKA accommodates the typical “screw-home” mechanism occurring during knee flexion, and this should be included when performing the sagittal tibial cut [30]. Most of the cases in the present series of lateral UKA were performed through a medial arthrotomy, like in the experience of Sah and Scott [32]. However, since the introduction of minimally invasive surgery with dedicated cutting guides, the surgical approach is now realized through a lateral arthrotomy without subluxation of the patella [4]. The results reported in this study for the most recent cases look fairly reproducible, but longer followup for these cases operated on through a so-called minimally invasive lateral approach is mandatory [4].
Our mid- and long-term data of lateral UKA suggest reasonable clinical and radiographic results [2, 10, 20]. The specific anatomic and biomechanical characteristics of the lateral compartment should be accommodated at the time of surgery when performing lateral UKA [3, 5, 32, 35]. Improvements in patient selection and surgical ancillaries over time have decreased the failure rate. Despite the limited number of indications resulting from the preponderance of medial osteoarthritis [33, 35], lateral UKA may represent a reasonable alternative to TKA when a single femorotibial compartment of the knee is affected.
Acknowledgments
We thank Yamina Chevrol-Benkeddache, MD, for the clinical review of the patients and Vanessa Pauly, MS, for the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277:7–72. [PubMed]
- 2.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002;84:2235–2239. [PubMed]
- 3.Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson DT, Agostini S. In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty. 2002;17:1049–1054. [DOI] [PubMed]
- 4.Argenson JN, Parratte S, Flecher X, Aubaniac JM. Unicompartmental knee arthroplasty: technique through a mini-incision. Clin Orthop Relat Res. 2007;464:32–36. [DOI] [PubMed]
- 5.Ashraf T, Newman JH, Evans RL, Ackroyd CE. Lateral unicompartmental knee replacement survivorship and clinical experience over 21 years. J Bone Joint Surg Br. 2002;84:1126–1130. [DOI] [PubMed]
- 6.Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006. [DOI] [PubMed]
- 7.Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty. 1996;11:782–788. [DOI] [PubMed]
- 8.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39–47. [DOI] [PubMed]
- 9.Cooke TD, Scudamore RA, Bryant JT, Sorbie C, Siu D, Fisher B. A quantitative approach to radiography of the lower limb. Principles and applications. J Bone Joint Surg Br. 1991;73:715–720. [DOI] [PubMed]
- 10.Eickmann TH, Collier MB, Sukezaki F, McAuley JP, Engh GA. Survival of medial unicondylar arthroplasties placed by one surgeon 1984–1998. Clin Orthop Relat Res. 2006;452:143–149. [DOI] [PubMed]
- 11.Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Joint Surg Am. 2004;86:2671–2676. [DOI] [PubMed]
- 12.Engh GA. Orthopaedic crossfire—can we justify unicondylar arthroplasty as a temporizing procedure? In the affirmative. J Arthroplasty. 2002;17:54–55. [DOI] [PubMed]
- 13.Engh GA. The lateral unicompartmental replacement: a road less traveled. Orthopedics. 2006;29:825–826. [DOI] [PubMed]
- 14.Flecher X, Parratte S, Aubaniac JM, Argenson JN. A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res. 2006;452:91–96. [DOI] [PubMed]
- 15.Gibson PH, Goodfellow JW. Stress radiography in degenerative arthritis of the knee. J Bone Joint Surg Br. 1986;68:608–609. [DOI] [PubMed]
- 16.Gioe TJ, Killeen KK, Hoeffel DP, Bert JM, Comfort TK, Scheltema K, Mehle S, Grimm K. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003;416:111–119. [DOI] [PubMed]
- 17.Gunther T, Murray D, Miller R. Lateral unicompartmental knee arthroplasty with Oxford meniscal knee. The Knee. 1996;3:33–39. [DOI]
- 18.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 19.Kaplan E, Meier P. Nonparametric observation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [DOI]
- 20.Laskin RS. Unicompartmental knee replacement: some unanswered questions. Clin Orthop Relat Res. 2001;392:267–271. [DOI] [PubMed]
- 21.Maquet P. The treatment of choice in osteoarthritis of the knee. Clin Orthop Relat Res. 1985;192:108–112. [PubMed]
- 22.Marmor L. Lateral compartment arthroplasty of the knee. Clin Orthop Relat Res. 1984;186:115–121. [PubMed]
- 23.Marmor L. Unicompartmental arthroplasty of the knee with a minimum ten-year follow-up period. Clin Orthop Relat Res. 1988;228:171–177. [PubMed]
- 24.McAlindon TE, Snow S, Cooper C, Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis. 1992;51:844–849. [DOI] [PMC free article] [PubMed]
- 25.Naudie D, Guerin J, Parker DA, Bourne RB, Rorabeck CH. Medial unicompartmental knee arthroplasty with the Miller-Galante prosthesis. J Bone Joint Surg Am. 2004;86:1931–1935. [DOI] [PubMed]
- 26.O'Rourke MR, Gardner JJ, Callaghan JJ, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC. The John Insall Award: unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27–37. [DOI] [PubMed]
- 27.Ohdera T, Tokunaga J, Kobayashi A. Unicompartmental knee arthroplasty for lateral gonarthrosis: midterm results. J Arthroplasty. 2001;16:196–200. [DOI] [PubMed]
- 28.Ornetti P, Parratte S, Gossec L, Tavernier C, Argenson JN, Roos EM, Guillemin F, Maillefert JF. Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthritis Cartilage. 2007;16:423–428. [DOI] [PubMed]
- 29.Parratte S, Argenson JN, Dumas J, Aubaniac JM. Unicompartmental knee arthroplasty for avascular osteonecrosis. Clin Orthop Relat Res. 2007;464:37–42. [DOI] [PubMed]
- 30.Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2003;85:1968–1973. [DOI] [PubMed]
- 31.Perkins TR, Gunckle W. Unicompartmental knee arthroplasty: 3- to 10-year results in a community hospital setting. J Arthroplasty. 2002;17:293–297. [DOI] [PubMed]
- 32.Sah AP, Scott RD. Lateral unicompartmental knee arthroplasty through a medial approach. Study with an average five-year follow-up. J Bone Joint Surg Am. 2007;89:1948–1954. [DOI] [PubMed]
- 33.Scott RD. Lateral unicompartmental replacement: a road less traveled. Orthopedics. 2005;28:983–984. [DOI] [PubMed]
- 34.Squire MW, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Unicompartmental knee replacement. A minimum 15 year followup study. Clin Orthop Relat Res. 1999;61–72. [PubMed]
- 35.Weidow J. Lateral osteoarthritis of the knee. Etiology based on morphological, anatomical, kinematic and kinetic observations. Acta Orthop Suppl. 2006;77:3–44. [PubMed]