Abstract
It has often been assumed rotational kinematics are improved with mobile-bearing TKA designs as the terms mobile-bearing and rotating platform imply. We tested this assumption by assessing the in vivo axial rotation magnitudes and patterns of 527 knees implanted with 12 different mobile-bearing TKA designs. Implants were grouped and compared by type—posterior stabilized (PS), posterior cruciate retaining (PCR), and posterior cruciate sacrificing (PCS)—and by specific design. We hypothesized all three mobile-bearing types (PS, PCR, and PCS) would achieve greater than 10° average axial rotation and we would find no differences in axial rotation between types. Only 14% of PS knees, 3% of PCS knees, and 17% of PCR knees attained greater than 10° axial rotation when measured from 0° to 90°. The percentage of PCS knees with greater than 10° axial rotation was less compared with the other two groups. Axial rotation averaged 4.3°, 2.5°, and 3.8° for the PS, PCS, and PCR knees, respectively. Incidences of reverse rotation were observed in 17% of PS knees, 32% of PCS knees, and 28% of PCR knees. Compared with the PCS group, the PS group achieved greater average axial rotation and had a lower percentage of knees displaying incidences of reverse rotation. The data refuted the hypotheses.
Introduction
In the normal knee, the tibia internally rotates relative to the femur during flexion and externally rotates during extension (ie, screw home mechanism). Kinematic analyses of normal knees have reported mean axial rotation magnitudes between 16° and 23° [1, 8, 12] during deep knee bend (DKB) to 90° and mean axial rotation magnitudes close to 24° [1, 9, 14] during DKB to 120°. After TKA, magnitudes and patterns of axial femorotibial rotation are more variable owing to ligamentous, design, and surgical influences [2, 5, 10, 22]. Reported average magnitudes after TKA range from −1° to 13.4° during DKB [3, 5–7, 18, 23, 24]. To replicate tibial internal rotation, fixed-bearing knees must rotate at the insert-femoral articulation. Mobile-bearing knee implants were designed to accommodate this rotation at the tibial-insert articulation, potentially allowing greater rotation. A variety of kinematic studies has been performed on mobile-bearing knees [2, 3, 6–8, 10, 11, 15–24], yet the kinematic rotational advantage is still debated.
In 1991, Nilsson and colleagues [16] reported fixed-bearing knees (MG) provided superior rotation over their mobile-bearing counterparts (LCS), although neither approximated normal rotation. Mobile-bearing designs have advanced since Nilsson’s early study. More recent studies suggest improved axial rotation performance by mobile-bearing knees [7, 11, 18, 24]. To our knowledge, the literature lacks a large multidesign analysis solely focused on magnitudes and patterns of axial rotation after mobile-bearing TKA.
We presumed three major implant types (PS, PCR, and PCS mobile-bearing) would achieve, on average, greater than 10° axial rotation and that the three types would display similar axial rotation magnitudes and patterns. We therefore asked whether contemporary mobile-bearing TKA designs provided the anticipated in vivo axial rotation magnitudes and patterns. We also asked whether differences in magnitudes and patterns of rotation were displayed by posterior stabilized (PS) mobile-bearing, posterior cruciate retaining (PCR) mobile-bearing, and posterior cruciate sacrificing (PCS) mobile-bearing knees or by knees implanted with different prosthetic designs.
Materials and Methods
We analyzed the in vivo axial rotation magnitudes and patterns of 527 knees that had TKA with a mobile-bearing prosthesis. Of these 527 knees, data from 340 have been reported previously [8]. The knees composed 42 patient cohorts; each cohort consisted of patients who had TKA performed by the same surgeon and received the same mobile-bearing implant design. The surgeries were performed from 1994 to 2007 at multiple centers. Twelve implant designs by three different manufacturers were analyzed (Table 1). Implants were grouped by type: PS mobile-bearing, PCR mobile-bearing, and PCS mobile-bearing (Table 2). We conducted a posthoc power analysis, which revealed the data have a power of nearly 1 to measure an effect size greater than 0.2° of rotation. This was deemed adequate because we found no literature attributing any clinical relevance to rotation changes less than 0.2° (much larger differences may also be clinically unimportant).
Table 1.
Axial rotation details for the 12 implant designs
| Implant | Number of knees | Average rotation 0°–90° | Negative (reverse) rotation (%) | Normal rotation (%) | Less than 3° rotation (%) | Less than 5° rotation (%) | Less than 10° rotation (%) | Greater than 10° rotation (%) |
|---|---|---|---|---|---|---|---|---|
| LCS RP PS | 81 | 2.7 | 31 | 69 | 49 | 62 | 88 | 11 |
| LCS RP PCS | 106 | 2.5 | 32 | 68 | 58 | 79 | 97 | 3 |
| LCS APG | 49 | 2.7 | 29 | 71 | 51 | 57 | 86 | 14 |
| LCS MB | 23 | 5.2 | 22 | 78 | 39 | 57 | 74 | 26 |
| Sigma RP PS | 75 | 4.8 | 11 | 89 | 39 | 52 | 87 | 13 |
| Sigma RP-F PS | 48 | 5.6 | 10 | 90 | 33 | 46 | 88 | 12 |
| Sigma RP PCR | 15 | 5.2 | 20 | 80 | 27 | 40 | 80 | 20 |
| Legacy HF PS | 51 | 4.6 | 12 | 88 | 33 | 53 | 86 | 14 |
| Legacy PS | 28 | 2.9 | 25 | 75 | 39 | 57 | 86 | 14 |
| Ceragyr MP | 17 | 6.3 | 6 | 94 | 24 | 35 | 77 | 23 |
| SROM | 7 | 5.9 | 0 | 100 | 14 | 57 | 86 | 14 |
| MBKIII PCR | 27 | 2.3 | 37 | 63 | 56 | 70 | 89 | 11 |
PS = posterior stabilized; PCS = posterior cruciate sacrificing; PCR = posterior cruciate retaining.
Table 2.
Axial rotation details for the three mobile-bearing implant types
| Implant | Number of knees | Average rotation 0°–90° | Negative (reverse) rotation (%) | Normal rotation (%) | Less than 3° rotation (%) | Less than 5° rotation (%) | Less than 10° rotation (%) | Greater than 10° rotation (%) |
|---|---|---|---|---|---|---|---|---|
| Posterior stabilized RP (PS) | 307 | 4.3 | 17 | 83 | 38 | 53 | 86 | 14 |
| Posterior cruciate sacrificing RP (PCS) | 106 | 2.5 | 32 | 68 | 58 | 79 | 97 | 3 |
| Posterior cruciate retaining RP (PCR) | 114 | 3.8 | 28 | 72 | 47 | 58 | 83 | 17 |
All TKAs were performed by experienced surgeons using the standard surgical technique for each prosthesis. To qualify for fluoroscopic analysis, subjects had to be at least 6 months post-TKA and their TKAs had to be considered clinically successful (Hospital for Special Surgery score greater than 90) with no measurable ligamentous laxity or pain.
Each knee was evaluated during DKB using video fluoroscopy and a two- to three-dimensional image registration technique. Fluoroscopic images were captured at each center and downloaded to a workstation computer for analysis. Three-dimensional kinematics were recovered from the two-dimensional fluoroscopic images using a previously described automated registration technique that determines the in vivo orientation of the femoral component relative to the tibial component [4]. Extensive error analyses of the registration technique demonstrate a translational three-dimensional error of less than 0.5 mm and rotational out-of-plane rotational error of less than 0.5° [13].
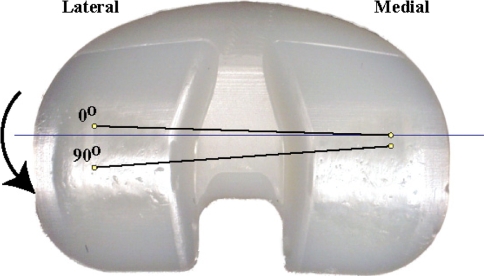
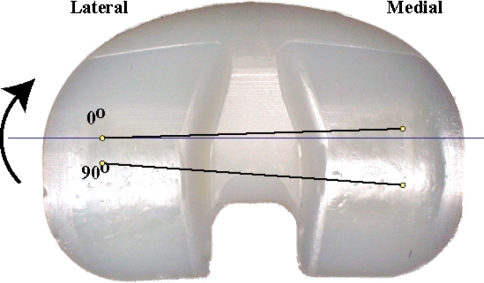
During the DKB activity, knee rotation was assessed at 0°, 30°, 60°, and 90°. Femorotibial contact positions for the medial and lateral condyles were determined for each selected video frame during the DKB maneuver. For each frame, the lowest point on each condyle was determined and taken as the contact point for that condyle. A line was created from the medial condylar contact point to the lateral condylar contact point. A second line was constructed bisecting the center of the tibial plateau in the coronal plane. The angle created between these two lines represented the axial rotation angle and thus was measured (Figs. 1, 2). If the lateral condylar contact position was more anterior than the medial condylar contact position, the axial rotation angle was labeled negative (reverse rotation). If the medial condylar contact position was more anterior than the lateral condylar contact position, the axial rotation angle was labeled positive (normal rotation).
Fig. 1.
An example of normal axial rotation in which the lateral femoral condyle rotates more posteriorly than the medial condyle (ie, internal tibial rotation) during flexion is shown. (Reprinted with permission from Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;428:180–189.)
Fig. 2.
An example of negative (reverse) axial rotation in which the medial femoral condyle rotates more posteriorly than the lateral condyle (ie, external tibial rotation) during flexion is shown. (Reprinted with permission from Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;428:180–189.)
For this study, axial rotation measurements were gathered from the starting point (0°) to the final flexion position (90°). This is different from a previous study that used the maximally internally rotated position and the maximally externally rotated position regardless of where in the range of motion these values occurred [8]. Measuring rotation from the start of the arc of motion to the end corresponds to what happens in the normal knee.
A Tukey-Kramer honestly significant difference comparison was used to identify differences in axial rotation; we used this test owing to the multiple comparisons and unequal group sizes. We used JMP software (SAS Institute, Cary, NC) for all analyses.
Results
During DKB to 90°, axial rotation greater than 10° was attained by only 14% of knees in the PS group, 3% of knees in the PCS group, and 17% of knees in the PCR group (Table 2). The percentage of PCS mobile-bearing knees with greater than 10° of axial rotation was less compared with the PS (p = 0.0012) and PCR (p = 0.0004) mobile-bearing knees. Approximately half of the PCS and PCR knees (58% and 47%, respectively) experienced less than 3° of axial rotation, and more than half of all three types (53% of PS, 79% of PCS, and 58% of PCR knees) (Table 2) and of all patient cohorts (26 of 42) experienced less than 5° of rotation (Tables 3, 4, 5). A patient cohort comprised of 10 LCS RP PS implants achieved the greatest average magnitude (8.2°). The same implant design performed poorly in other patient cohorts, averaging as low as −1.5°, −1.3°, and 0.5° (Table 3).
Table 3.
Details for patient cohorts with PS mobile-bearing implants
| Implant/surgeon | Number of knees | Average rotation 0°–90° | Negative (reverse) rotation (%) | Normal rotation (%) | Less than 3° rotation (%) | Less than 5° rotation (%) | Less than 10° rotation (%) | Greater than 10° rotation (%) |
|---|---|---|---|---|---|---|---|---|
| Sigma RP PS #1 | 9 | 5.3 | 0 | 100 | 22 | 44 | 89 | 11 |
| Sigma RP PS #2 | 9 | 2.2 | 22 | 78 | 67 | 78 | 89 | 11 |
| Sigma RP PS #3 | 12 | 5.3 | 8 | 92 | 42 | 58 | 75 | 25 |
| Sigma RP PS #4 | 10 | 4 | 0 | 100 | 50 | 60 | 100 | 0 |
| Sigma RP PS #5 | 20 | 7.3 | 10 | 90 | 25 | 30 | 80 | 20 |
| Sigma RP PS #6 | 15 | 3 | 20 | 80 | 40 | 60 | 93 | 7 |
| Sigma RP-F PS #1 | 12 | 4.9 | 17 | 83 | 33 | 50 | 100 | 0 |
| Sigma RP-F PS #2 | 20 | 5.5 | 15 | 85 | 35 | 45 | 85 | 15 |
| Sigma RP-F PS #3 | 16 | 6.4 | 0 | 100 | 31 | 44 | 81 | 19 |
| LCS RP PS #1 | 10 | 8.2 | 10 | 90 | 30 | 40 | 70 | 30 |
| LCS RP PS #2 | 10 | 4.3 | 20 | 80 | 40 | 40 | 90 | 10 |
| LCS RP PS #3 | 6 | −1.5 | 50 | 50 | 67 | 67 | 83 | 17 |
| LCS RP PS #4 | 5 | 5.2 | 40 | 60 | 40 | 60 | 60 | 40 |
| LCS RP PS #5 | 10 | 2.7 | 30 | 70 | 50 | 60 | 80 | 20 |
| LCS RP PS #6 | 10 | −1.3 | 70 | 30 | 80 | 100 | 100 | 0 |
| LCS RP PS #7 | 20 | 0.5 | 35 | 65 | 55 | 70 | 100 | 0 |
| LCS RP PS #8 | 10 | 5.5 | 0 | 100 | 30 | 50 | 90 | 10 |
| LPS HF #1 | 20 | 5.4 | 15 | 85 | 25 | 50 | 75 | 25 |
| LPS HF #2 | 21 | 4.6 | 10 | 90 | 38 | 57 | 95 | 5 |
| LPS HF #3 | 10 | 4.6 | 10 | 90 | 40 | 50 | 90 | 10 |
| LPS #1 | 28 | 2.9 | 25 | 75 | 39 | 57 | 86 | 14 |
| Ceragry MP #1 | 17 | 6.3 | 6 | 94 | 24 | 35 | 77 | 23 |
| SROM | 7 | 5.9 | 0 | 100 | 14 | 57 | 86 | 14 |
| Total | 307 | 4.3 | 17 | 83 | 38 | 53 | 86 | 14 |
PS = posterior stabilized.
Table 4.
Details for patient cohorts with PCR mobile-bearing implants
| Implant/surgeon | Number of knees | Average rotation 0°–90° | Negative (reverse) rotation (%) | Normal rotation (%) | Less than 3° rotation (%) | Less than 5° rotation (%) | Less than 10° rotation (%) | Greater than 10° rotation (%) |
|---|---|---|---|---|---|---|---|---|
| Sigma RP PCR #1 | 15 | 5.2 | 20 | 80 | 27 | 40 | 80 | 20 |
| MBKIII PCR #1 | 7 | 7.6 | 0 | 100 | 14 | 23 | 86 | 14 |
| MBKIII PCR #2 | 20 | 0.5 | 50 | 50 | 70 | 85 | 90 | 10 |
| LCS APG #1 | 20 | 6 | 15 | 85 | 35 | 35 | 75 | 25 |
| LCS APG #2 | 9 | 5.4 | 22 | 88 | 33 | 33 | 78 | 22 |
| LCS APG #3 | 10 | −1.1 | 50 | 50 | 80 | 100 | 100 | 0 |
| LCS APG #4 | 10 | 0.6 | 40 | 60 | 70 | 80 | 100 | 0 |
| LCS MB#1 | 10 | 3.5 | 30 | 70 | 50 | 60 | 90 | 10 |
| LCS MB#2 | 13 | 7 | 15 | 85 | 31 | 54 | 62 | 38 |
| Total | 114 | 3.8 | 28 | 72 | 47 | 58 | 83 | 17 |
PCR = posterior cruciate retaining.
Table 5.
Details for patient cohorts with PCS mobile-bearing implants
| Implant/surgeon | Number of knees | Average rotation 0°–90° | Negative (reverse) rotation (%) | Normal rotation (%) | Less than 3° rotation (%) | Less than 5° rotation (%) | Less than 10° rotation (%) | Greater than 10° rotation (%) |
|---|---|---|---|---|---|---|---|---|
| LCS RP PCS #1 | 10 | 3.7 | 10 | 90 | 30 | 70 | 100 | 0 |
| LCS RP PCS #2 | 8 | 4.4 | 13 | 87 | 50 | 75 | 88 | 12 |
| LCS RP PCS #3 | 8 | 1.7 | 25 | 75 | 75 | 88 | 100 | 0 |
| LCS RP PCS #4 | 12 | 2.4 | 25 | 75 | 50 | 75 | 100 | 0 |
| LCS RP PCS #5 | 10 | 2.9 | 30 | 70 | 40 | 60 | 100 | 0 |
| LCS RP PCS #6 | 8 | 0.6 | 50 | 50 | 63 | 88 | 100 | 0 |
| LCS RP PCS #7 | 16 | 2.4 | 19 | 81 | 75 | 94 | 94 | 6 |
| LCS RP PCS #8 | 9 | 4.2 | 11 | 89 | 22 | 67 | 89 | 11 |
| LCS RP PCS #9 | 5 | 3.4 | 40 | 60 | 60 | 60 | 100 | 0 |
| LCS RP PCS #10 | 20 | −0.8 | 70 | 30 | 85 | 90 | 100 | 0 |
| Total | 106 | 2.5 | 32 | 68 | 58 | 79 | 97 | 3 |
PCS = posterior cruciate sacrificing.
The PS-type knees experienced a greater (p = 0.0004) average magnitude of axial rotation compared with the PCS-type knees. During DKB to 90°, axial rotation averaged 4.3°, 2.5°, and 3.8° for the PS, PCS, and PCR mobile-bearing knee groups, respectively (Table 2). Every patient cohort in the PCS group (all composed of LCS RP PCS implants [DePuy Orthopaedics, Warsaw, IN]) experienced less than 5° of axial rotation (Table 5).
The incidence of reverse rotation was less (p = 0.0001) for the PS group compared with the PCS group. All three mobile-bearing implant groups exhibited incidences of reverse rotation: 17% of PS knees, 32% of PCS knees, and 28% of PCR knees (Table 2).
Discussion
Because mobile-bearing TKA inserts were designed to rotate relative to the tibial component, it has often been assumed that patients having mobile-bearing TKA will experience rotational kinematics similar to the normal knee and superior to fixed-bearing knees. We tested this assumption by analyzing the axial rotation data of a large group of knees implanted with a variety of mobile-bearing TKA designs. We expected to find average axial rotation magnitudes greater than 10° and only rare occurrences of reverse rotation. We therefore asked whether contemporary mobile-bearing TKA designs provided the anticipated in vivo axial rotation magnitudes and patterns. We also asked whether differences in magnitudes and patterns of rotation were displayed by posterior stabilized (PS) mobile-bearing, posterior cruciate retaining (PCR) mobile-bearing, and posterior cruciate sacrificing (PCS) mobile-bearing knees or by knees implanted with different prosthetic designs.
This study contains limitations that warrant mention. One limitation is a lack of patient demographic information such as weight and age, which could influence kinematics. The likelihood that patient demographics varied among the groups is lessened by the large number of subjects and the criterion that subjects had to have Hospital for Special Surgery scores greater than 90 (excellent rating). Another limitation is that although our kinematic results revealed mobile-bearing knees did not approximate normal axial rotation, these data cannot justly be used to infer implant longevity or outcome. It should also be noted that our measurements were made through 90° of flexion. If rotation was measured to 120°, greater rotation values may have been found. It is possible mobile-bearing knees achieve more rotation from 90° to 120° than from 0° to 90°, although this would be opposite of the normal knee.
This study’s mobile-bearing knees experienced less axial rotation compared with normal knees in published reports [1, 8, 9, 12, 14]. Average magnitudes for normal knees range between 16° and 23° when measured during DKB to 90° [1, 8, 12]. We used a more conservative value of normal axial rotation, 10°. Only 65 of 527 knees (12%) exceeded this 10° value. Over half of the PCS knees and nearly half of the PCR knees did not attain even 3° of rotation. Although the majority of PS knees achieved minimum 3° of rotation, not quite half of PS knees achieved minimum 5°. These data suggest contemporary mobile-bearing implant designs have not achieved markedly improved axial rotation magnitudes.
The use of multiple surgeons exposed the strong influence of surgical factors on kinematic success after mobile-bearing TKA. Looking at the Sigma RP PS patient cohorts, one surgeon’s mean rotation was 7.3°, whereas another surgeon’s mean was only 2.2°. For the LCS RP PS patient cohorts, one surgeon’s cohort averaged 8.2° of rotation, whereas another surgeon’s cohort averaged −1.5° (Table 3). Both designs of high-flex implants (LPS High Flex [Zimmer, Warsaw, IN] and Sigma RP-F PS [DePuy Orthopaedics]) seemed to perform more consistently compared with the other mobile-bearing implants (Table 3). These variable results suggest that although certain designs may be more surgeon-friendly, the surgeon factors affecting femorotibial rotation need to be more fully understood.
Wasielewski et al. [23] studied the influence of surgical factors on knee kinematics using an intraoperative pressure-measuring device on the insert trial. In 16 patients with well-balanced knees, they reported only three occurrences of major condylar liftoff (defined as condylar tibial separation 1 mm or greater) but poor translation and axial rotation (average, 2.4°). Only four knees internally rotated more than 4° with knee flexion, and three of 16 experienced reverse axial rotation. Only one patient had normal axial rotation (14.4°), and incidentally, this patient had 1 mm of liftoff. These data suggest variables other than just compartment balance are needed to achieve normal rotation patterns.
An average reverse axial rotation pattern was demonstrated by four patient cohorts (Tables 3–5). When rotation was assessed at individual flexion angles, reverse rotation was even more prevalent. Some knees alternated between internal and external rotation as the knee was flexed, a phenomenon not observed in the normal knee.
In their roentgen stereophotogrammetric analysis study, Nilsson and colleagues [16] reported PCR fixed-bearing TKA (MG) subjects averaged 3° of axial rotation, whereas PCR mobile-bearing TKA (LCS) subjects averaged only 1.5° of axial rotation while performing a stepup maneuver. Nonetheless, neither group approached the 7° of axial rotation achieved by normal, nonreplaced knees. Other studies have reported similar axial rotation between fixed- and mobile-bearing knees [8, 11, 15]. Two more recent studies reported greater axial rotation with mobile-bearing over fixed-bearing knees [3, 18]. Delport and colleagues [3], using a single implant system (Performance; Biomet, Warsaw, IN), found at maximum flexion, PS mobile-bearing knees displayed more axial rotation (mean, 7.46°) compared with PS (mean, 2.36°) and PCR fixed-bearing knees (mean, 5.89°). The mobile-bearing knees in our study, which is the largest to date, did not achieve better axial rotation magnitudes compared with fixed-bearing knees in published reports [5, 8, 18].
In this large analysis of mobile-bearing knee implants of differing designs, we found none attained the expected magnitudes or patterns of axial rotation. From our data, it is evident implant type and design and surgeon factors interact to create suboptimal mobile-bearing rotational kinematics. Nonetheless, the contribution of the insert undersurface and main articular still needs to be delineated.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Asano T, Akagi M, Tanaka K, Tamura J, Nakamura T. In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clin Orthop Relat Res. 2001;388:157–166. [DOI] [PubMed]
- 2.Banks SA, Hodge WA. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res. 2004;426:187–193. [DOI] [PubMed]
- 3.Delport HP, Banks SA, De Schepper J, Bellemans J. A kinematic comparison of fixed- and mobile-bearing knee replacements. J Bone Joint Surg Br. 2006;88:1016–1021. [DOI] [PubMed]
- 4.Dennis DA, Komistek RD, Hoff WA, Gabriel SM. In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res. 1996;331:107–117. [DOI] [PubMed]
- 5.Dennis DA, Komistek RD, Mahfouz MR. In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res. 2003;410:114–130. [DOI] [PubMed]
- 6.Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. [DOI] [PubMed]
- 7.Dennis DA, Komistek RD, Mahfouz MR, Outten JT, Sharma A. Mobile-bearing total knee arthroplasty: do the polyethylene bearings rotate? Clin Orthop Relat Res. 2005;440:88–95. [DOI] [PubMed]
- 8.Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;428:180–189. [DOI] [PubMed]
- 9.Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38:241–253. [DOI] [PubMed]
- 10.D’Lima DD, Trice M, Urquhart AG, Colwell CW Jr. Comparison between the kinematics of fixed and rotating bearing knee prostheses. Clin Orthop Relat Res. 2000;380:151–157. [DOI] [PubMed]
- 11.Elias JJ, Kumagai M, Mitchell I, Mizuno Y, Mattessich SM, Webb JD, Chao EY. In vitro kinematic patterns are similar for a fixed platform and a mobile-bearing prosthesis. J Arthroplasty. 2002;17:467–474. [DOI] [PubMed]
- 12.Komistek RD, Dennis DA, Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res. 2003;410:69–81. [DOI] [PubMed]
- 13.Mahfouz MR, Hoff WA, Komistek RD, Dennis DA. A robust method for registration of three-dimensional knee implant models to two-dimensional fluoroscopy images. IEEE Trans Med Imaging. 2003;22:1561–1574. [DOI] [PubMed]
- 14.Mahfouz MR, Komistek RD, Dennis DA, Hoff WA. In vivo assessment of the kinematics in normal and anterior cruciate ligament-deficient knees. J Bone Joint Surg Am. 2004;86(Suppl 2):56–61. [DOI] [PubMed]
- 15.Most E, Li G, Schule S, Sultan P, Park SE, Zayontz S, Rubash HE. The kinematics of fixed- and mobile-bearing total knee arthroplasty. Clin Orthop Relat Res. 2003;416:197–207. [DOI] [PubMed]
- 16.Nilsson KG, Karrholm J, Gadegaard P. Abnormal kinematics of the artificial knee. Roentgen stereophotogrammetric analysis of 10 Miller-Galante and five New Jersey LCS knees. Acta Orthop Scand. 1991;62:440–446. [DOI] [PubMed]
- 17.Oakeshott R, Stiehl JB, Komistek RA, Anderson DT, Haas BD. Kinematic analysis of a posterior cruciate retaining mobile-bearing total knee arthroplasty. J Arthroplasty. 2003;18:1029–1037. [DOI] [PubMed]
- 18.Ranawat CS, Komistek RD, Rodriguez JA, Dennis DA, Anderle M. In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res. 2004;418:184–190. [DOI] [PubMed]
- 19.Russo A, Montagna L, Bragonzoni L, Visani A, Marcacci M. Changes in knee motion over the first 3 years with a mobile-bearing prosthesis. Knee. 2006;13:301–306. [DOI] [PubMed]
- 20.Saari T, Uvehammer J, Carlsson LV, Herberts P, Regner L, Karrholm J. Kinematics of three variations of the Freeman-Samuelson total knee prosthesis. Clin Orthop Relat Res. 2003;410:235–247. [DOI] [PubMed]
- 21.Stiehl JB, Dennis DA, Komistek RD, Keblish PA. In vivo kinematic analysis of a mobile-bearing total knee prosthesis. Clin Orthop Relat Res. 1997;345:60–66. [DOI] [PubMed]
- 22.Sugita T, Sato K, Komistek RD, Mahfouz MR, Maeda I, Sano T. In vivo determination of knee kinematics for Japanese subjects having either a low contact stress rotating platform or an anteroposterior glide total knee arthroplasty. J Arthroplasty. 2005;20:154–161. [DOI] [PubMed]
- 23.Wasielewski RC, Galat DD, Komistek RD. An intraoperative pressure-measuring device used in total knee arthroplasties and its kinematic correlations. Clin Orthop Relat Res. 2004;427:171–178. [DOI] [PubMed]
- 24.Watanabe T, Yamazaki T, Sugamoto K, Tomita T, Hashimoto H, Maeda D, Tamura S, Ochi T, Yoshikawa H. In vivo kinematics of mobile-bearing knee arthroplasty in deep knee bending motion. J Orthop Res. 2004;22:1044–1049. [DOI] [PubMed]