Abstract
The management of the patellar articular surface at the time of primary total knee arthroplasty (TKA) is controversial. We used expected-value decision analysis to determine whether the patella should be resurfaced in TKA, and also whether secondary resurfacing on an unresurfaced patella is worthwhile. Outcome probabilities and utility values were derived from randomized controlled trials only. A decision tree was constructed and fold-back analysis was performed to ascertain the best treatment path. Sensitivity analyses were performed to determine the effect on decision-making of varying outcome probabilities and utilities. Our model showed patellar resurfacing is the best management strategy for the patella at the time of primary TKA. This decision is robust to changes in the specific data: the best path would remain the same as long as the incidence of persistent anterior knee pain (AKP) with resurfacing remains less than 29% (current mean, 12%) or the incidence of AKP after nonresurfacing falls below 12% (current mean, 26%). Delayed (ie, secondary) patellar resurfacing for ongoing patellar pain provides inferior results for the majority of patients.
Level of Evidence: Level II, decision analysis. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Total knee arthroplasty is one of the most commonly performed procedures in the field of adult reconstructive surgery and the number of procedures continues to increase [15]. In general, orthopaedic surgeons performing total knee replacements can be categorized into three groups as to how they address the patella: nonresurfacers, universal resurfacers, and selective resurfacers. Resurfacing is associated with good clinical results but is also associated with a small risk of patellar fracture or need for patellar revision in the future [9, 19, 21, 23]. Nonresurfacing of the patella may prevent such problems but is associated with a higher rate of anterior knee pain and reoperation [9, 19, 21, 23]. The decision to resurface the patella is subjective. The current literature on patellar resurfacing after TKA, including four recent meta-analyses, has failed to show clear superiority of patellar resurfacing or not resurfacing as judged by standard clinical outcome scores [1, 6–8, 19, 21–23, 30–32]. However, the authors concluded that patellar resurfacing could be considered a superior strategy with regard to less frequent anterior knee pain and need for reoperation [9, 19, 21, 23].
An unsolved problem for both resurfacing and nonresurfacing surgeons is how persistent anterior knee pain after surgery should be addressed. There are conflicting data concerning the efficacy of secondary resurfacing for anterior knee pain following unresurfaced TKA [1, 12, 17, 18]. The outcome after isolated secondary revision of a patellar component in patients who underwent resurfacing is also unclear [5, 14, 16, 24].
Expected-value decision analysis is a methodological tool that allows quantitative analysis of decision making under conditions of uncertainty [13, 25, 33]. The “expected value” refers to the predicted consequences of a decision, which is determined from the probabilities of the outcomes and their utilities. The best decision is identified by calculating the expected value of each therapeutic option; the stability of this conclusion is tested by varying the values of the model inputs (sensitivity analysis). Utility is a subjective value that an individual places on a particular outcome of interest. Reports on outcomes and probabilities from the published literature, when used in a decision model, can provide a meaningful comparison of alternative management strategies.
The primary purpose of our decision analysis was to determine the best treatment pathway for the patella in patients who undergo primary TKA, with reference to patellar resurfacing. We also asked whether secondary resurfacing is indicated for patients with persistent anterior knee pain after knee arthroplasty, whether the patella has been resurfaced or not.
Materials and Methods
We developed a decision model based solely on the data of randomized controlled trials (RCTs) [1, 7, 8, 22, 30–32] (Table 1). The model quantified postoperative utilities after TKA with and without resurfacing and investigated the outcome after revision surgery in both groups. A decision tree categorized the data into five sequences of decision and outcome with multiple potential pathways (Fig. 1). The model, constructed using decision analysis software (TreeAge Pro 2006; TreeAge Software, Williamstown, MA), was established to determine (1) if primary patellar resurfacing is a superior option to nonresurfacing in TKA, with respect to the patient’s health utility outcome and (2) if it is beneficial for patients with postoperative anterior knee pain to undergo revision or secondary resurfacing in the unresurfaced patella.
Table 1.
Characteristics of eligible studies
| First author (year of publication) | Enrollment period | Followup (months) | Number of knees analyzed (patellar resurfacing/no patellar resurfacing) |
|---|---|---|---|
| Waters (2003) [31] | 1992–NR | 64 | 474 (243/231) |
| Wood (2002) [32] | 1992–1996 | 48 | 218 (91/127) |
| Partio (1995) [22] | 1990–1992 | 30 | 95 (47/48) |
| Barrack (2001) [1] | 1992–1993 | 70 | 93 (47/46) |
| Campbell (2006) [8] | 1991–1993 | 120 | 58 (30/28) |
| Waikakul (2000) [30] | NR | 24 | 47 (21/26) |
| Burnett (2004) [7] | 1991–NR | 130 | 39 (19/20) |
NR = not reported.
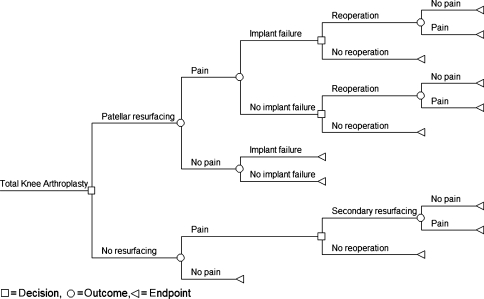
Fig. 1.
The schematic decision tree shows the decisions, outcomes and endpoints related to the patella in TKA.
The model evaluates these two strategic decisions as follows. Initially the surgeon has the possibility of performing a TKA with or without resurfacing the patella (Fig. 1, square pathways). Subsequently, two different outcomes are possible in both groups (Fig. 1, circular pathways). The patient is either pain-free (ie, reports minimal anterior knee pain) or has anterior knee pain (usually moderate or severe).
If a nonresurfaced patient is pain-free, no further treatment or measures are necessary as he or she already has the best outcome (Fig. 1, triangular endpoint). In the resurfaced group the ideal outcome may be jeopardized by a loose or worn implant, nevertheless the patient may not need any further treatment (Fig. 1, triangular endpoint). In a pain-free patient with a loose implant, the ideal outcome is not achieved, and this is represented by a lower utility, as described below. In both cases the decision tree is terminated at that point (Fig. 1, triangular endpoint).
If a patient in the resurfaced group has pain after surgery, two potential scenarios are possible. The implant is loose or the implant is stable. The patient, in discussion with the treating surgeon, has two possible options (Fig. 1, square): reoperation and revision of the implant or no further treatment. If the decision is no reoperation the decision tree ends (Fig. 1, triangle) and a certain value for the outcome (utility) is determined. If a revision surgery is performed two outcomes are possible (Fig. 1, circle). The patient may be pain-free or may still be in pain after the revision (Fig. 1, triangle). The corresponding utilities are valued.
The same options are available for the nonresurfaced group. The patient may complain of pain after surgery (Fig. 1, square). If the symptoms are severe enough, a secondary resurfacing may be performed (Fig. 1, circle). Subsequently, the patient can either be pain-free or may still experience anterior knee pain.
Probabilities (Table 2) were obtained using only data of randomized controlled trials in which patients were specifically asked about anterior knee pain. When there were multiple reports for the same patient group, we selected the most recent results. Seven reports providing relevant data with regard to anterior knee pain were identified [1, 7, 8, 22, 30–32]. The probabilities were calculated based on the absolute numbers for all trials combined.
Table 2.
Model parameters used in the decision tree
| Probabilities, utilities & disutilities | Absolute mean probability | Utility or disutility | Range of individual studies |
|---|---|---|---|
| Resurfaced patellae | |||
| Probability of AKP | 0.120 | 0.021–0.467 | |
| Probability of NO AKP | 0.880 | 0.533–0.970 | |
| Probability of AKP + Implant failure | 0.067 | 0–0.200 | |
| Probability of AKP + NO Implant failure | 0.933 | 0.800–1 | |
| Probability of AKP + Implant failure + Revision + NO Pain | 0.250 | 0–1 | |
| Probability of AKP + Implant failure + Revision + Pain | 0.750 | 0–1 | |
| Probability of AKP + NO Implant failure + Revision + NO Pain | 0.700 | 0–1 | |
| Probability of AKP + NO Implant failure + Revision + Pain | 0.300 | 0–1 | |
| Nonresurfaced patellae | |||
| Probability of AKP | 0.257 | 0.077–0.429 | |
| Probability of NO AKP | 0.743 | 0.571–0.923 | |
| Probability of AKP + Secondary resurfacing + NO Pain | 0.395 | 0.067–0.909 | |
| Probability of AKP + Secondary resurfacing + Pain | 0.605 | 0.091–0.933 | |
| Utilities and disutilities | |||
| Preoperative utility [3] | 0.52 | ||
| Expected postop utility, without pain, excluding disutility [3] | 0.79 | ||
| Expected postop utility, with AKP, excluding disutility | 0.62 | ||
| Disutility for total knee arthroplasty | 0.10 | ||
| Disutility for revision surgery after TKA | 0.10 | ||
| Disutility of implant failure | 0.02 | ||
| Calculated utilities | |||
| Pain-free after one operation | 0.69 | ||
| Pain-free after two operations | 0.59 | ||
| Persistent pain after one operation | 0.52 | ||
| Persistent pain after two operations | 0.42 | ||
Utilities used in this model (Table 2) are based on health state utilities intended for use with knee replacement surgery. The McKnee modified health utility index [3] provides a standardized, objective statement associated with osteoarthritis (OA) of the knee.
Utility theory bases decision making on the subjective worth that a patient places on the specific outcome. Robust and valid estimates of patient-derived utilities are derived from complex qualitative methods, such as the standard reference gamble or time trade-offs in which patients are asked to gamble or choose between health states usually referenced to death. The perfect health state is by definition 1.0. Utility values using the McKnee system described for the clinical marker health states in the patients with OA showed preoperative values of 0.59 for moderate pain and 0.44 for severe pain. For our study we used the mean of these values giving a preoperative value of 0.515 [3]. We assumed TKA increases the quality of life to a level corresponding to the health state of patients with mild preoperative pain in the McKnee system with a utility score of 0.79. If the patient had persistent pain after TKA, a utility value of 0.615 was assigned resulting in the identical utility as for the preoperative status once the negative experience of the operation is included, as described below.
For negative phenomena, such as the disadvantage of an operation or of implant failure and subsequent surgery, the concept of disutility is used and its value is subtracted (Table 2). The disutility of having TKA was set at 0.1 as reported and validated previously [27]. Secondary resurfacing was likewise assessed a disutility of 0.1. While secondary resurfacing might not be as invasive as the primary procedure, we consider secondary resurfacing as revision surgery and therefore not as benign as the index procedure, especially when taking into account the major impact a reoperation may impose on a patient [27]. A disutility of 0.1 for secondary resurfacing is less than would be associated with a full revision and greater than has been used for unicompartmental TKA (0.06) [27]. While we consider this value appropriate, we nevertheless evaluated the effect of a lower disutility by repeating the decision analysis with a disutility of 0.06 for secondary resurfacing.
Given the expected health utility in a patient after TKA is 0.79 and the intervention itself imposes a disutility of 0.1, the maximum achievable postoperative utility is 0.69. The lowest expected utility, 0.42, corresponds to persistent pain after two operations (Table 2).
After the construction of the decision tree, a sensitivity analysis was performed. By varying the probabilities and utilities, it is possible to determine to which point one clinical decision is superior to another. Sensitivity analysis also allows a threshold value to be determined at which the clinical decision of two competing strategies is equivocal.
Results
Our decision tree analysis was designed to answer two questions. The first question was whether to routinely resurface the patella or not in a primary total knee arthroplasty. Based on the decision tree, the highest expected value for the patient is achieved by resurfacing the patella at the time of the index operation (Fig. 2). Our second question was whether or not to resurface a painful patella secondarily. Based on the utilities derived from our decision tree model, secondary resurfacing is not seen as the best strategy in patients with a painful primary unresurfaced patella (Fig. 2).
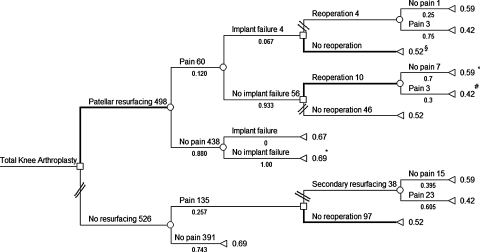
Fig. 2.
The completed decision tree shows the probabilities as calculated from RCT trials and the utilities based on the McKnee modified health utility index. The path probabilities on the optimal pathway are as follows: §path probability = 0.008; °path probability = 0.078; #path probability = 0.034; *path probability = 0.880. The remaining path probabilities were not calculated as they are not on the optimal pathway.
The probability of having anterior knee pain after primary surgery in patients with a resurfaced patella, for all studies combined, was 12% compared to a probability of 26% for patients without patellar resurfacing. All patients with implant failure reported pain. The probability of a patella-related second operation was 2.8% for the resurfaced group and 7.2% in the nonresurfaced group for the trials studied. Based on the higher probability of pain relief in the primarily resurfaced group compared with the unresurfaced group, primary patellar resurfacing is preferable to not resurfacing the patella.
The maximum achievable health utility (0.69) was achieved in 88% of patients with a resurfaced patella, making it the highest calculated probability path, and is the preferred approach according to the decision tree. The corresponding utility was achieved in only 74% of patients with a nonresurfaced patella.
The maximum achievable health utility for patients undergoing a second operation such as secondary resurfacing or revision of the patellar component is 0.59 due to the disutility of the second operation. In patients with secondary resurfacing, the expected utility improved for 39% of patients from 0.52 to 0.59. However, for the remaining 61% who experienced the second operation without relief of pain, the expected utility dropped from 0.52 to 0.42. Altogether, 89% of patients with primary resurfacing were free of anterior knee pain when the second operation was included versus 77% of patients with primary nonresurfacing, showing relatively little change from the primary results. The results of the decision analysis therefore do not favor secondary resurfacing.
In patients with a resurfaced patella who have persistent pain and associated implant failure, the calculated path probability unexpectedly showed superiority for the path with no reoperation. Although true from a model-based calculation (since pain remained in the majority of cases, thus making it an undesirable path), reoperation will still practically be required, as described below.
In patients with persistent pain and no implant failure of the patellar component, reoperation usually led to a reduction in pain, suggesting a different and identifiable cause to the pain. In this setting a revision is recommended. Reoperation most often involved lateral release. Other reasons were patellar implant position, arthroscopy for AKP, or patellectomy.
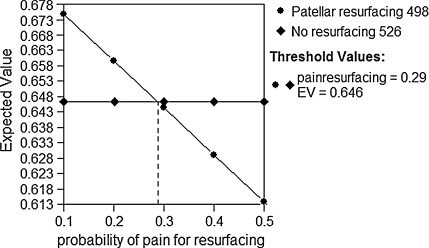
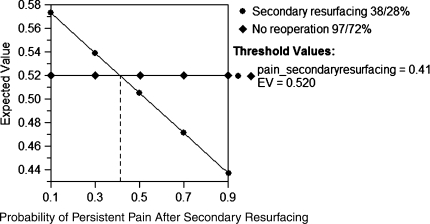
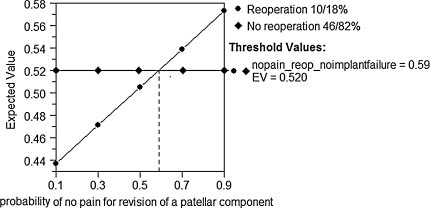
One-way sensitivity analysis indicated resurfacing the patella would continue to be the preferred option provided the incidence of AKP after resurfacing remains below 29% (currently 12%) (Fig. 3) or the incidence of AKP after nonresurfacing falls below 12% (currently 26%). The one-way sensitivity analysis of persistent pain after secondary resurfacing showed a threshold value of 41%, indicating secondary resurfacing would become beneficial only if the probability of pain drops below that value (currently 61%) (Fig. 4). One-way sensitivity analysis for the probability of persistent pain after revision for anterior knee pain without implant failure calculated a threshold value of 59% (Fig. 5), indicating revision surgery will continue to be recommended as long as the probability of having no pain is higher than 59% (currently 70%). Changing the disutility of secondary resurfacing from 0.1 to 0.06 did not change the optimal pathways.
Fig. 3.
One-way sensitivity analysis is shown for the probability of persistent pain after primary resurfacing. The probability of having pain after resurfacing is varied on the x axis. The lines represent the expected value (EV) for the decision to resurface and the decision not to resurface. The expected value is a weighted average of the expected value for each outcome (eg, pain or no pain) times the probability of its occurrence. Below the threshold value (a probability of 0.29), resurfacing is favored. The current estimate of 0.12 is well within this preferred region.
Fig. 4.
One-way sensitivity analysis is shown for the probability of persistent pain after secondary resurfacing. The lines represent the expected value (EV) for the decision to perform a secondary resurfacing or not. Above the threshold value (a probability of 0.41), secondary resurfacing is not favored. The current probability of persistent pain after secondary resurfacing (0.61) is well above this value, explaining the recommended decision to avoid secondary resurfacing.
Fig. 5.
One-way sensitivity analysis is shown for the probability of no pain after revision in resurfacing. The lines represent the expected value (EV) for the decision to revise and the decision not to revise for anterior knee pain. Above the threshold value (a probability of 0.59), revision should be performed. The current estimate of 0.70 is close to the threshold, indicating that the recommended decision to reoperate in the presence of AKP in the resurfaced patella may change as more data become available, or may depend on the specifics of each patient’s case.
Discussion
When performing primary TKA, the surgeon must decide on the best management path for the patellar articular surface since the best management in the published literature remains controversial. The primary advantages of resurfacing the patella are that it preempts future concerns of symptomatic arthritis of the patellar surface and may provide for lower rates of anterior knee pain and reoperation [9, 19, 21, 23]. The primary advantages of nonresurfacing are that it avoids future patellar prosthetic failure, may minimize future patellar fracture risk, and usually maintains reasonable patellar function. The question of best management of the patella lends itself well to expected-value decision analysis because of well-defined treatment options and relatively discrete outcomes. In this decision analysis we found patellar resurfacing is the best decision path, given the outcome probabilities and utilities typical of knee arthroplasty patients in the published literature. Based on the sensitivity analyses performed, this decision is robust to large changes in the incidence of pain after resurfacing or nonresurfacing.
We note several limitations. First, mechanisms of implant failure (eg, infection, metal-back implant, polyethylene wear) could not be addressed in this analysis as there is a lack of available data in the literature in this special subgroup of patients. It is also unclear in the reported RCTs as to what proportion of those cases with “anterior knee pain” also have associated abnormal rotational placement of their femoral and tibial components, as this information was not available. Our use of sensitivity analyses demonstrates a robust margin of superiority for patellar resurfacing, which should remain stable regardless of variations in degrees of femoral or tibial component malrotation providing that the rates and magnitude of component malrotation do not differ substantially from that which is likely to have occurred across these RCTs. Second, we were unable to use a Markov model to further investigate the timeline of the appearance of anterior knee pain due to limitations in the available literature. The studies included in our analysis represented a time frame from 2 years [30] up to 11 years [7], with the results normally being reported for the most recent followup. While we are unaware of any large-scale natural history studies to document time-to-event rates for anterior knee pain following primary knee arthroplasty, the majority of cases occurred relatively soon after the index operation. Waters and Bentley reported that, in all cases, anterior knee pain appeared within 18 months [31]. Wood et al. indicated anterior knee pain became apparent as early as 3 months, with the largest proportion of patients reporting their first symptoms within 6 months of the operation [32]. Burnett et al. [6] reported secondary resurfacing due to AKP was performed at a mean of 3.3 years (range, 1–5 years). Similarly Barrack et al. [1] reported six of seven secondary resurfacings were performed before the 2- to 4-year followup examination. After secondary resurfacing, they reported an initial decrease in AKP, followed by deterioration by the 5- to 7-year followup. Campbell et al. [8] reported the rate of AKP at 4 years, 8 years, and 10 years; the rate fluctuated slightly, but was greater at 10 years than at 4 or 8 years. Given the strong tendency for anterior knee pain to present early and receive reoperation early (within 2 years) following the primary knee arthroplasty, we believe a decision analytic model is an appropriate method to evaluate for the best path. This may appear a relatively simplistic approach to the problem, but is likely the most appropriate given the published literature available on this topic at this point in time: while the Markov model is a superior method to evaluate changes over time and competing events over time, large-scale randomized trials are lacking from which to extract utilities, events, costs, and consequences at different time points following the primary knee arthroplasty. As the goal of our study was not to investigate the arthroplasty survival rates but the overall incidence of anterior knee pain in patellar resurfacing, we believe our model gives the orthopaedic surgeon an additional tool for the treatment of patients with anterior knee pain after an index procedure.
We used only randomized controlled trials in the current medical literature in which anterior knee pain was specifically investigated [1, 7, 8, 22, 30–32]. Using only the probabilities reported in RCTs enhances the reliability of this model, which is greatly influenced by the quality of the data available. For example, a previous study that recommended decision tree analysis as a tool for patellar resurfacing recognized the limitations of the quality of the data available at that time, and was therefore unable to draw distinct conclusions and did not address secondary resurfacing [33]. Another strength of our study is that we used the McKnee modified health utility index which is a validated outcome instrument for the determination of health utilities [3] in patients with OA of the knee. Contrary to the EQ-5D index scores recently published [28] or other index scores based on the quality of well being [10, 27], the McKnee specifically addresses the question of clinical marker health state scores in the TKA patient group, further substantiating our results. The results obtained from decision tree analyses depend on the accuracy of the available data in the literature; with the inclusion of randomized controlled trials only, we have minimized this potential confounding factor. The results may not be applicable to individual patients, but provide guidance for overall patterns of patellar management.
Currently there is little information to guide the surgeon with regard to management of the patient presenting with late development of anterior knee pain after knee arthroplasty [9]. We were able to use our decision model to demonstrate the varying outcomes associated with treating the patient presenting with late anterior knee pain following knee arthroplasty whether or not they were resurfaced at the time of the index procedure. The following discusses the outcomes, options and explanations for each decision. In the resurfacing group, in the presence of an implant failure of the patellar component, revision surgery was associated with a lower health utility compared to no revision. This is explained due to the fact that there is a disutility (−0.1) of the second operation and an unpredictable outcome after the revision. The probability of being pain-free in this scenario was 25% and therefore did not represent the best path. In theory the decision tree consequently indicates the best path would be no additional surgery, but practically and ethically revision might be the correct decision. Furthermore, the potential mechanisms of implant failure (eg, infection, metal-back implant, polyethylene wear) could not be addressed in this analysis. Our results are in accordance, however, with other studies, where secondary revisions of loose patellar components were associated with poor outcomes [4, 16]. In contrast, the decision tree indicates a revision would be beneficial in patients where no failure due to loosening of the patellar component can be detected. In the reported studies, there was often an identifiable, mechanical cause that was corrected in the second operation. While the reported numbers included only patella-related revisions (such as lateral retinacular release), malpositioning of the femoral or tibial component can also produce anterior knee pain [2, 11, 26, 29] and revision of these components may be warranted. Lateral retinacular release or repositioning of the patellar component could potentially be more successful in comparison to replacing a loose implant, as the associated bone loss is less. This may not be valid when newer implants for patellar revision, such as a trabecular metal patellar augment is used, as none of the RCTs used such devices. The sensitivity analysis for reoperation due to AKP but without implant failure (Fig. 5) showed the results for this question are close to the decision threshold. Given this fact and the fact that a low number of patients presented with this condition, this decision pathway may change once more data become available.
On the other arm of the decision tree, with nonresurfacing of the patella, the sensitivity analysis showed that unless the probability of having persistent pain is less than 41% (currently 61%) secondary resurfacing is not in the best path. This result is mainly explained by the probability of reoccurring pain in long-term followup after secondary resurfacing. In addition, the disutility of the second operation influences the final utility. In recent studies, the results of secondary resurfacing were very favorable in the short term but tended to deteriorate with longer followup [1, 17, 18], resulting in an inferior outcome to primary resurfacing. Based on the current literature and the decision tree model, secondary resurfacing seems not to be beneficial for patients in the long term, and has the further disadvantage of a second operation.
The results of our study are in keeping with the published evidence of reduced prevalence of anterior knee pain and reoperation in patients with a resurfaced patella, as indicated by the previous meta-analyses [9, 19, 21, 23]. Given the average incidence of anterior knee pain for the nonresurfaced patients was 26%, compared to an average incidence of 12% for the resurfaced patients, resurfacing the patella would prevent one case of postoperative anterior knee pain for every seven patellae resurfaced. Under these circumstances, if all 526 nonresurfaced patients in this decision analysis had received a resurfaced patella at the index operation, 72 patients would have avoided experiencing postoperative anterior knee pain.
Because the average reoperation rate for nonresurfaced patients was 7.2% compared to 2.8% for the resurfaced patients, resurfacing the patella would prevent one reoperation for every 23 patellae resurfaced within the timeframe studied. In the past, the revision rate for resurfaced patellae was high due to the failure of metal-backed prostheses with wear, non-patella-friendly femoral component designs, and poor surgical technique leading to patellar fracture and/or instability. This explains the preference of some for not resurfacing; however, the current reoperation rate appears quite low. Given that the cost of a revision surgery is typically over $11,000 [20, 27], and that less than half of patients benefit from secondary resurfacing, primary resurfacing appears to offer both cost and health utility advantages.
Our model suggests, based on the best evidence currently available, that primary resurfacing of the patella is a superior strategy to nonresurfacing, and that secondary resurfacing for AKP is not recommended. Reoperating may be warranted in the case of a failed patellar implant or where a mechanical cause for pain can be identified. Our decision analysis model has, for the first time, tabulated the range of possible outcomes not only of primary replacement, but also after revision patellar surgery based on a meta-analysis of randomized controlled trials. This model may be of assistance to surgeons and patients when decisions need to be made pertaining to patellar management at the time of primary TKA.
Footnotes
Investigation performed at the Department of Orthopaedics and the Department of Mechanical Engineering, University of British Columbia, Vancouver, BC, Canada.
AO International, Davos, Switzerland (NH), the Canadian Arthritis Network (CA), and Praxim SA, Grenoble, France (CA) provided funding during the preparation of this manuscript.
References
- 1.Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am. 2001;83:1376–1381. [PubMed]
- 2.Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:46–55. [DOI] [PubMed]
- 3.Bennett KJ, Torrance GW, Moran LA, Smith F, Goldsmith CH. Health state utilities in knee replacement surgery: the development and evaluation of McKnee. J Rheumatol. 1997;24:1796–1805. [PubMed]
- 4.Berry DJ, Rand JA. Isolated patellar component revision of total knee arthroplasty. Clin Orthop Relat Res. 1993;286:110–115. [PubMed]
- 5.Burke WV, Ammeen DJ, Engh GA. Isolated revision of failed metal-backed patellar components: outcome with minimum 4-year follow-up. J Arthroplasty. 2005;20:998–1001. [DOI] [PubMed]
- 6.Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65–72. [DOI] [PubMed]
- 7.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res. 2004;428:12–25. [DOI] [PubMed]
- 8.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88:734–739. [DOI] [PubMed]
- 9.Forster MC. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a systematic review. Knee. 2004;11:427–430. [DOI] [PubMed]
- 10.Fryback DG, Dasbach EJ, Klein R, Klein BE, Dorn N, Peterson K, Martin PA. The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making. 1993;13:89–102. [DOI] [PubMed]
- 11.Hofmann S, Romero J, Roth-Schiffl E, Albrecht T. Rotational malalignment of the components may cause chronic pain or early failure in total knee arthroplasty [in German]. Orthopade. 2003;32:469–476. [DOI] [PubMed]
- 12.Karnezis IA, Vossinakis IC, Rex C, Fragkiadakis EG, Newman JH. Secondary patellar resurfacing in total knee arthroplasty: results of multivariate analysis in two case-matched groups. J Arthroplasty. 2003;18:993–998. [DOI] [PubMed]
- 13.Kocher MS, Bishop JA, Hresko MT, Millis MB, Kim YJ, Kasser JR. Prophylactic pinning of the contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2004;86:2658–2665. [DOI] [PubMed]
- 14.Koh JS, Yeo SJ, Lo NN, Tan SK, Tay BK, Seow KH. Isolated patellar revisions for failed metal-backed components: 2- to 9-year follow-up. J Arthroplasty. 2004;19:880–886. [DOI] [PubMed]
- 15.Kozak LJ, DeFrances CJ, Hall MJ. National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2006;162:1–209. [PubMed]
- 16.Leopold SS, Silverton CD, Barden RM, Rosenberg AG. Isolated revision of the patellar component in total knee arthroplasty. J Bone Joint Surg Am. 2003;85:41–47. [DOI] [PubMed]
- 17.Mockford BJ, Beverland DE. Secondary resurfacing of the patella in mobile-bearing total knee arthroplasty. J Arthroplasty. 2005;20:898–902. [DOI] [PubMed]
- 18.Muoneke HE, Khan AM, Giannikas KA, Hagglund E, Dunningham TH. Secondary resurfacing of the patella for persistent anterior knee pain after primary knee arthroplasty. J Bone Joint Surg Br. 2003;85:675–678. [PubMed]
- 19.Nizard RS, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, Sedel L. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432:196–203. [DOI] [PubMed]
- 20.Novak EJ, Silverstein MD, Bozic KJ. The cost-effectiveness of computer-assisted navigation in total knee arthroplasty. J Bone Joint Surg Am. 2007;89:2389–2397. [DOI] [PubMed]
- 21.Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005;87:1438–1445. [DOI] [PubMed]
- 22.Partio E, Wirta J. Comparison of patellar resurfacing and nonresurfacing in total knee arthroplasty: a prospective randomized study. J Orthop Rheum. 1995;8:69–74.
- 23.Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005;438:191–196. [DOI] [PubMed]
- 24.Parvizi J, Seel MJ, Hanssen AD, Berry DJ, Morrey BF. Patellar component resection arthroplasty for the severely compromised patella. Clin Orthop Relat Res. 2002;397:356–361. [DOI] [PubMed]
- 25.Pauker SG, Kassirer JP. Decision analysis. N Engl J Med. 1987;316:250–258. [DOI] [PubMed]
- 26.Romero J, Stahelin T, Wyss T, Hofmann S. Significance of axial rotation alignment of components of knee prostheses [in German]. Orthopade. 2003;32:461–468. [DOI] [PubMed]
- 27.Slover J, Espehaug B, Havelin LI, Engesaeter LB, Furnes O, Tomek I, Tosteson A. Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J Bone Joint Surg Am. 2006;88:2348–2355. [DOI] [PubMed]
- 28.Sullivan PW, Ghushchyan V. Preference-Based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2006;26:410–420. [DOI] [PMC free article] [PubMed]
- 29.Torga-Spak R, Parikh SN, Stuchin SA. Anterior knee pain due to biplanar rotatory malalignment of the femoral component in total knee arthroplasty. Case report. J Knee Surg. 2004;17:113–116. [DOI] [PubMed]
- 30.Waikakul S, Vanadurongwan V, Bintachitt P. The effects of patellar resurfacing in total knee arthroplasty on position sense: a prospective randomized study. J Med Assoc Thai. 2000;83:975–982. [PubMed]
- 31.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85:212–217. [DOI] [PubMed]
- 32.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84:187–193. [DOI] [PubMed]
- 33.Zangger P, Detsky A. Computer-assisted decision analysis in orthopedics: resurfacing the patella in total knee arthroplasty as an example. J Arthroplasty. 2000;15:283–288. [DOI] [PubMed]