Abstract
Precise pre- and postoperative anatomic measurements are necessary to plan, perform, and evaluate total knee arthroplasty (TKA). We evaluated the relationship between radiographic and navigation alignment measurements, identified sources of error in radiographic and navigated alignment assessment, and determined the differences between desired and clinically accepted alignment. Fifty-eight computer-assisted TKAs were performed and limb alignment measurements were recorded both pre- and postoperatively with standard radiographs and with an intraoperative navigation system. Intraoperative navigation produced consistent navigation-generated alignment results that were within 1° of the desired alignment. The difference between preoperative radiographic and navigation measurements varied by as much as 12° and the difference between postoperative radiographic and navigation measurements varied by as much as 8°. This discrepancy depended on the degree of limb deformity. Postoperative radiographic measurements have inherent limitations. Navigation can generate precise, accurate, and reproducible alignment measurements. This technology can function as an effective tool for assessing pre- and postoperative limb alignment and relating intraoperative alignment measurements to clinical and functional outcomes.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Precise pre- and postoperative measurements of limb alignment are necessary to plan, perform, and evaluate the success of TKA. Standard radiographs, computed tomography, MRI, or intraoperative navigation systems can be used to perform these measurements. Standard radiographs can, in a controlled setting and in normal patients with minimal deformity, be quite accurate [8, 9]. However, these required conditions are difficult to achieve and are not applicable to patients with extremity-deforming osteoarthritis. The use of an intraoperative navigation system, which has a technical accuracy previously validated to within 1° [14, 23, 25], may allow for an objective assessment of the accuracy and reproducibility of radiographic measurement of TKA components and alignment. This type of relationship is important to examine given that numerous previous studies have used standard radiographs to evaluate and relate TKA limb and implant alignment to clinical and functional outcome measures [1–3, 6, 10, 13, 16, 21, 24, 30, 33–35].
Our objectives were: (1) to evaluate the strength of the association between standard pre- and postoperative radiographic and intraoperative navigation alignment measurements; (2) to determine the potential sources of error inherent to the process of radiographic and navigated alignment assessment; and (3) to examine the subtle differences that exist between desired alignment (anteroposterior [AP] mechanical axis and sagittal tibial and femoral axes of 0°) and clinically accepted alignment (final alignment after the bone cuts were made and implants placed) as assessed through an intraoperative navigation system.
Materials and Methods
Fifty-eight consecutive computer-assisted (CAS) TKAs were performed on 51 patients by a surgeon with extensive prior experience in CAS TKA. Of these patients, 30 underwent unilateral CAS TKA, seven underwent bilateral CAS TKA, and 14 underwent bilateral TKA with one side performed using CAS. For each TKA, we obtained weightbearing full-length AP and short film lateral radiographs. The AP mechanical axis and sagittal femoral and tibial axis measurements were recorded both intraoperatively using the navigation system and with standard 4-week (short-term) and 2-year (long-term) postoperative radiographs. Six patients (all unilateral) were lost to followup as a result of relocation, unwillingness to continue participation in the study, or lack of intraoperative measurements. These patients were excluded from the final analysis of the data.
Radiographs were performed with patients positioned in a method based on the recommendations described by Cooke et al. [8, 9]. For the weightbearing AP radiograph, the patient was placed in the standing position with their backside against the gridded 14 × 50-inch cassette. The feet were positioned together, touching if possible; we allowed patients to slightly separate the feet to provide good balance. The central ray was directed perpendicular to the joint space in between the patella and femoral condyles. The lateral views were performed with the patient supine lying on the affected side. The opposite leg was positioned over and in front of the knee in question to allow the affected knee to fully rest on the radiographic cassette. The central ray was directed perpendicular to the film.
We made intraoperative navigation measurements preoperatively before any cuts were made and again postoperatively after cuts were made and implants placed. We used the Aesculap OrthoPilot™ (Aesculap, Tuttlingen, Germany) navigation system for computer-assisted TKA and to generate navigation alignment measurements.
We used the EFilm Workstation™ (Merge Healthcare, Milwaukee, WI) to evaluate digitized radiographs and limb alignment according to the Knee Society Roentgenographic Evaluation System [12]. Two observers (MAY, SSK) performed these measurements and the correlation between these measurements was determined. The observers had no knowledge of the navigation measurements at the time the measurements were performed.
The senior author (SDS) made the final determination of any discrepancies between the readings of the two observers. We evaluated the difference and degree of variation between the measurements achieved using short- and long-term standard radiographs and intraoperative navigation measurements. The desired or targeted alignment, defined as a mechanical axis, femoral flexion, and tibial slope of 0°, was compared with the accepted intraoperative alignment as measured by the navigation system.
We used a two-tailed bivariate Pearson correlation to evaluate the strength of the association between pre- and postoperative radiographic and navigation alignment measurements as well as the association of interobserver measurements. An analysis was performed on pre- and postoperative radiographic and navigation measurements as well as desired and clinically accepted intraoperative measurements to determine mean values, standard deviation, minimum, and maximum discrepancy. All statistical analyses were performed using a commercial statistical software package (SPSS version 14.0; SPSS Inc, Chicago, IL).
Results
Radiographic results exhibited a greater range and variability than the navigation data in each of the three measurement criteria (Table 1). Radiographs had a tendency to overestimate the degree of varus in the AP mechanical axis, the degree of femoral flexion in the sagittal axis, and degree of posterior tibial slope in the sagittal axis relative to navigation measurements (Table 1). The radiographic and navigation measurements of the mechanical axis correlated preoperatively (r = 0.885, p = 0.01) but not postoperatively (r = 0.081, p = 0.587) (Tables 1, 2). Short-term and long-term radiographic measurements were correlated (r = 0.840, p = 0.01) (Table 1). The discrepancy between preoperative radiographs and navigation measurements increased with the degree of preoperative limb deformity (Figs. 1, 2; Table 3).
Table 1.
An analysis of radiographic and navigation measurement of limb and implant alignment
| Axis of measurement | Measurement of interest | Mean | Minimum | Maximum | Standard deviation |
|---|---|---|---|---|---|
| Mechanical axis (anteroposterior) (varus +) | Preoperative radiograph | 8.76 | −12 | 22 | 8.24 |
| Preoperative navigation | 5.62 | −12 | 16 | 5.20 | |
| Discrepancy between radiograph and navigation (preoperative) | 4.66 | −10.00 | 12.00 | 2.89 | |
| Postoperative (1-month) radiograph | 1.91 | −4 | 8 | 2.89 | |
| Postoperative (2-year) radiograph | 1.43 | −2 | 4 | 1.910 | |
| Postoperative navigation | 0.56 | −1 | 3 | 1.00 | |
| Discrepancy between radiograph and navigation (1 month) | 2.73 | −5.00 | 8.00 | 1.81 | |
| Femoral axis (sagittal) (flexion +) | Postoperative (1-month) radiograph | 2.05 | −4 | 7 | 2.46 |
| Postoperative (2-year) radiograph | 1.73 | 0 | 4 | 0.961 | |
| Postoperative navigation | −0.24 | −2 | 2 | 0.847 | |
| Discrepancy between radiograph and navigation | 3.00 | −4.00 | 7.00 | 1.76 | |
| Tibial axis (sagittal) (posterior slope −) | Postoperative (1-month) radiograph | −2.10 | −7 | 2 | 1.80 |
| Postoperative (2-year) radiograph | −2.93 | −8 | 0 | 2.219 | |
| Postoperative navigation | −0.76 | −6 | 1 | 1.33 | |
| Discrepancy between radiograph and navigation | 2.21 | −7.00 | 2.00 | 1.66 |
Table 2.
An analysis of radiograph to navigation correlation and interobserver correlation of limb and implant alignment measurements
| Alignment measurement | Radiograph:navigation Pearson correlation coefficient (two-tailed significance) | Observer 1:observer 2 Pearson correlation coefficient (two-tailed significance) |
|---|---|---|
| Mechanical axis (AP) preoperative | 0.885* | 0.762* |
| Mechanical axis (AP) postoperative | 0.081 (0.587) | 0.873* |
| Femoral cut (sagittal) postoperative | 0.027 (0.854) | 0.693* |
| Tibial cut (sagittal) postoperative | 0.200 (0.168) | 0.664* |
* Correlation is significant at the 0.01 level (two-tailed); AP = anteroposterior.
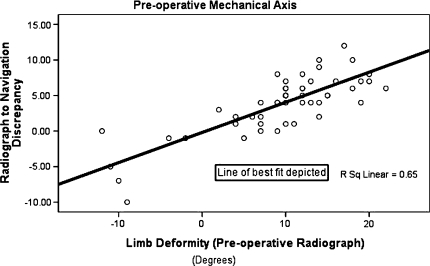
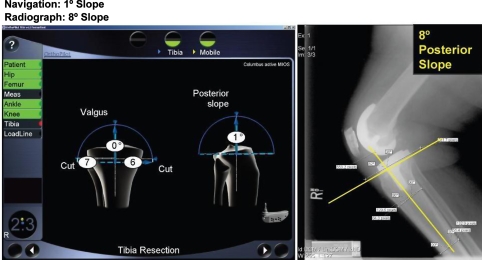
Fig. 1.
A comparison was made of radiograph and navigation measurement discrepancy with limb deformity. We observed a linear relationship between the two.
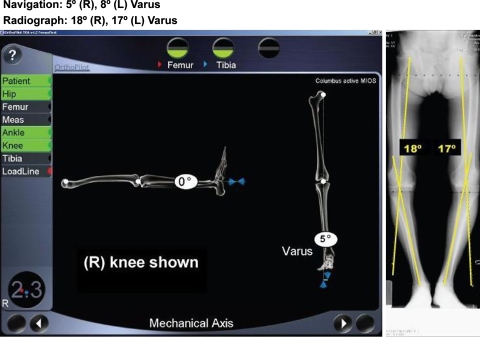
Fig. 2.
A case of extreme preoperative radiograph and navigation alignment discrepancy in the mechanical axis is seen.
Table 3.
An analysis of preoperative radiograph to navigation discrepancy*
| Discrepancy | Number | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|---|
| Mechanical axis greater than 15° | 9 | 4.00 | 12.00 | 7.4444 | 2.35112 |
| Mechanical axis 11° to 14° | 14 | 1.00 | 10.00 | 5.4286 | 2.50275 |
| Mechanical axis 6° to 10° | 19 | .00 | 8.00 | 3.8421 | 2.29161 |
| Mechanical axis −5° to 5° | 6 | 1.00 | 3.00 | 1.5000 | .83666 |
| Mechanical axis −10 to −6 | 2 | 7.00 | 10.00 | 8.5000 | 2.12132 |
| Mechanical axis −15° to −11° | 2 | 0 | 5.00 | 2.5000 | 3.53553 |
| Mechanical axis less than −15° | 0 | — | — | — | — |
* Defined by preoperative radiograph mechanical axis measurements.
The strength of interobserver radiographic measurement correlation depended on the ability of the observer to accurately and reproducibly demarcate anatomic landmarks. The interobserver measurement correlation was greatest for assessment of the mechanical axis (r = 0.873) and weakest for the tibial axis (r = 0.664) (Table 2).
Whereas the desired intraoperative mechanical, femoral, and tibial axis alignments were 0°, the accepted alignment was 0.56° varus ± 1.0° (−1° to 3°), 0.24° flexion ± 0.84° (−2° to 2°), and 0.76° posterior slope ± 1.3° (−6° to 1°), respectively (Table 4).
Table 4.
The deviation from desired limb alignment with the use of a navigation system
| Measurement | Mean deviation | Minimum | Maximum | Standard deviation |
|---|---|---|---|---|
| Mechanical axis (anteroposterior) (varus +) | 0.56 | −1 | 3 | 1.00 |
| Femoral axis (sagittal) (flexion −) | −0.24 | −2 | 2 | 0.847 |
| Tibial axis (sagittal) (posterior slope −) | −0.76 | −6 | 1 | 1.33 |
Discussion
Precise pre- and postoperative measurements of limb alignment are necessary to plan, perform, and evaluate the outcomes of TKA. Under ideal circumstances standard radiographs can in normal patients with minimal deformity be accurate [8, 9]. However, these required conditions are difficult to achieve and are not applicable to patients with extremity-deforming osteoarthritis. Intraoperative navigation has an accuracy to within 1° [14, 23, 25], and may allow objective assessment of the accuracy and reproducibility of radiographic measurement of TKA components and alignment. The purpose of our study, therefore, was to develop a more complete understanding of the relationship that exists between measurements performed using standard radiographs and those obtained with an intraoperative navigation system.
An appreciation of the limitations and potential sources of error inherent to each of these measurement modalities is warranted. We did not attempt to suggest navigation can or should be considered a “gold standard” tool for alignment assessment. Navigation is, however, a validated measurement tool capable of generating accurate and reproducible alignment measurements, which can assist the surgeon in achieving his or her desired and targeted alignment goals. The information generated by the navigation system grants the surgeon a unique opportunity to assess the subtle differences that exist between the desired or targeted alignment and the alignment that was deemed clinically acceptable in the operating room. Understanding these relationships can help guide the degree of confidence and caution one should maintain when using radiographs to plan preoperatively or draw firm conclusions from studies using this type of imaging modality for limb and implant assessment.
The two additional major limitations in this study include: (1) that alignment measurements using navigation are obtained on extremities that are nonweightbearing; and (2) an acceptance that according to published evidence, navigation is an accurate measurement tool if used appropriately. There is no clear consensus regarding the effect of weightbearing status on mechanical axis measurement. Kendoff et al. found the effect of weightbearing of one-half body weight will cause mechanical axis deviation of 0.4° [18], whereas Specogna et al. notes an average axis deviation of 1.6° in supine versus double-limb standing radiographs [32]. Still, other studies have found no effect of weightbearing on the apparent mechanical axis [29]. It is not unreasonable to conclude that weightbearing may contribute to the lack of radiograph to navigation correlation seen in this study; however, we believe the magnitude of the effect of weightbearing status is dependent on whether proper soft tissue balance can be achieved intraoperatively. In a previous study involving the same patient cohort, we established average medial-lateral laxity was 2.8° ± 1.1° with more than 70% of knees balanced within 1° of equal varus and valgus laxity [36]. We believe the narrow range of total laxity and balance of soft tissues would likely reduce or dampen the potential impact of weightbearing on radiographic assessment of the mechanical axis. The second major limitation was the assumption that the intraoperative navigation system is capable of generating accurate alignment measurements if used appropriately. An appreciation for the error inherent to the navigation system as well as an evaluation of published studies that have assessed the accuracy and reproducibility of navigation is warranted. Although the navigation system increases accuracy and precision of TKA [2, 5, 6, 10, 13, 16, 30, 33], there are several points during the acquisition of alignment measurements in which subtle error may be inadvertently introduced. These points include: (1) the registration process by which visually selected anatomic landmarks are selected and kinematic registration of the hip, knee, and ankle are performed; (2) the measurement process by which the image-free navigation system generates limb and implant alignment measurements based on data acquired from the registration process; and (3) intraoperative changes in the navigation environment (eg, inadvertent movement of pins or rigid bodies).
The hardware component of the navigation system, including the optical localizer, rigid bodies containing light-emitting diodes, and hardware and software components of the computer system is highly developed and capable of producing measurements accurate to 1 to 2 mm or less than 1° [14, 23, 25]. The registration process, however, is subject to intra- and interobserver errors in landmark registration capable of producing errors of 0.1° to 1.3° [11, 17, 28, 38]. The combined effect of these errors is demonstrated in two studies by Pitto et al. [26] and Yau et al. [39], who used validated precision calipers and computed tomography, respectively, to assess the accuracy of navigation measurements. Maximum discrepancies of 0.5° to 1.0° and up to 3.3°, respectively, were demonstrated in assessment of navigation-generated measurements of the mechanical axis. The errors in the registration process can be minimized through experience with the navigation system and developing a consistent and reliable registration technique [34]. In addition, safeguards inherent to the OrthoPilot™ navigation system used in this study help to ensure accurate evaluation of the mechanical axis in the frontal and sagittal planes. The system is redundant in that both surface registration as well as kinematic registration are performed to help identify the mechanical axis. If a discrepancy between these measurements is identified by the navigation system, the surgeon is prompted to repeat the registration process before proceeding.
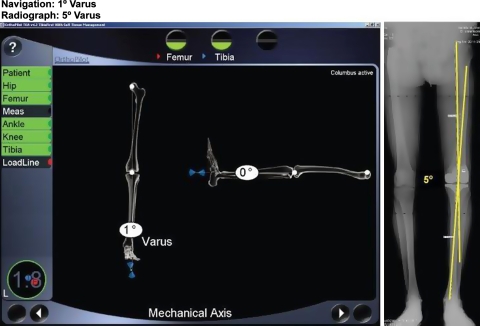
When compared with previous studies by Cooke et al. [7, 9] in which a standardized patient positioning system was used to radiographically evaluate the mechanical axis of “normal” patients in the population (0.97° to 1.0° varus ± 2.0° to 2.86°), our postoperative radiographic mechanical axis measurements were relatively similar in both average alignment and standard deviation (1.9° varus ± 2.8°). However, the standard deviation of the radiographic mechanical axis exhibited in Cooke et al.’s studies [7, 9] and the present study are greater than the standard deviation noted in the navigation-generated measurements (0.56° ± 1.0°). This degree of radiographic variability would make it difficult to draw firm conclusions from small differences between radiographic and navigation measurements. We found no correlation between intraoperative navigation measurements obtained at the conclusion of the procedure and postoperative radiographs (Table 2). In addition, we found the magnitude of preoperative radiograph to navigation discrepancy had a tendency to increase with the degree of preoperative limb deformity (Table 3; Fig. 1). These results are similar to previous studies that have noted statistical differences between mean radiographic and navigation measurements as well as a greater discrepancy in the preoperative period [28, 34]. A particularly noteworthy trend was identified, namely increasing radiograph to navigation measurement discrepancy as the degree of limb deformity increased. It is likely limbs with greater deformity are more prone to error introduced through the effects of weightbearing, flexion contracture, and rotation than limbs with less severe disease. Surgeons should recognize that not only is a major perceived deformity on a radiograph likely overestimating the degree of deformity relative to the corresponding navigation measurement generated in the operating room, but also the discrepancy between these measurements has a tendency to increase with the degree of deformity. Surgeons should thus be conservative with regard to initial soft tissue releases and bone cuts early in the performance of TKA and be careful not to overcorrect what appears to be a major deformity on the radiograph.
There is an interplay of several additional factors that limit the association and correlation between radiographs and navigation seen in this study. These factors include soft tissue conditions and patient positioning, human variability and error in alignment measurement, and difficulty in radiographic landmark demarcation. Radiographic assessment is prone to measurement error as a result of soft tissue conditions such as flexion contractures and inconsistencies in patient positioning. Previous studies by Lonner et al. [20], Brower et al. [4], and Hunt et al. [15] have noted variation in radiographic alignment measurements by up to 4° with varying combinations of knee flexion and internal or external rotation. Physiological rotation of the foot with respect to the tibia may also introduce error. Yoshioka et al. [40] notes most individuals have a natural foot rotation with respect to the tibia with men typically internally rotating and women typically externally rotating. Radiographers may also have difficulty in correctly and reproducibly positioning the limb and may only be able to accurately place the limb within 10° of the neutral position in the majority of clinical settings [37]. Correct positioning is particularly difficult to judge in specific subsets of patients such as those who are obese or those with severe flexion deformities [8, 9]. Even with consistent positioning, the error associated with radiographic assessment is reportedly about 0.75° [31]. The use of a standardized radiographic bilateral standing approach, as described by Cooke et al. [7] and Siu et al. [29], may still only provide angle reproducibility of ± 1.3°. Thus, even with a standardized approach to patient positioning in a controlled environment, the degree of variability in radiographic assessment may be noteworthy. Variability of this magnitude has the potential to dampen the validity of studies using radiographic assessment to attempt to identify small changes or differences in limb alignment. To avoid many of the aforementioned errors associated with flexion contractures and inconstant positioning, it may be advantageous to delay radiographs until full or near full knee extension is achieved [22]. In addition, standardization of limb positioning should be achieved using a standardized radiographic technique or frame-positioning system [7–9, 22, 29, 31].
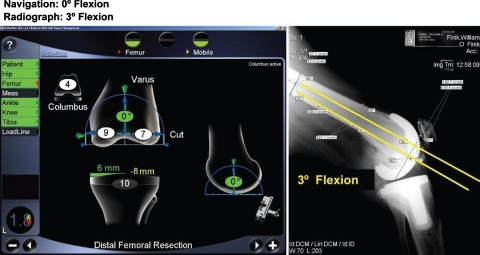
Human error during the process of alignment evaluation is a potential source of measurement variability. Intra- and interobserver measurement of the mechanical axis on standard radiographs can vary by more than 1° in 50% to 70% of cases and by more than 3° in 10% to 14% of cases [19, 27]. We believe the magnitude of intra- and interobserver variability is dependent on the degree of difficulty in demarcating anatomic landmarks on radiographs. The correlation of interobserver alignment measurements was much stronger for the AP mechanical axis than for the sagittal femoral and tibial axes in this study (Table 2); thus, we believe radiographic measurements of the AP mechanical axis can be performed more accurately than measurements of the sagittal femoral and tibial axes. This is attributable to the fact that measurement of the mechanical axis can be made using the intersection of lines connecting single points. These points include the center of the femoral head, proximal point of the femoral intercondylar notch, center of the proximal tibial spine, and center of the proximal talus (Figs. 2, 3). There is a high degree of interobserver consistency in demarcating these anatomic points and consequently interobserver measurement correlation of the mechanical axis is relatively high [28]. In contrast, measurement of the sagittal femoral and tibial axes cannot be performed with the same degree of precision. To determine the sagittal femoral component axis, one must find the intersection of one line parallel to the slope of the femoral component pegs (perpendicular to the distal femoral cut) with a second line parallel to the center of the femoral shaft (Fig. 4). The measurement of the axis of the peg is prone to error as a result of the small size of the pegs relative to the length of the shaft of the femur and resolution of these structures on plain radiograph is usually less than optimal. Any rotation of the limb inadvertently introduced will alter the apparent slope of the pegs. The measurement of the line parallel to the midpoint of the femoral shaft is subject to variability as a result of asymmetric expansion of the distal femoral metaphysis, bowing of the femoral shaft, and blurring of the precise borders of the cortex of the femoral shaft. Assessment of the sagittal tibial axis is made by determining the intersection of a line parallel to the base of the tibial component with a line parallel to the center of the tibial shaft (Fig. 5). Measurement of the tibial axis shares many of the same problems as the femur, in which asymmetric expansion of the tibial metaphysis, bowing of the tibial shaft, and blurring of the tibial cortex affect the accuracy and precision of landmark demarcation. Limb deviation in the coronal plane will also profoundly affect the ability to accurately place a line parallel to the base of the tibial component.
Fig. 3.
A case of extreme postoperative radiograph and navigation alignment discrepancy in the mechanical axis is seen.
Fig. 4.
A case of extreme postoperative radiograph and navigation alignment discrepancy in the femoral axis is seen.
Fig. 5.
A case of extreme postoperative radiograph and navigation alignment discrepancy in the tibial axis is seen.
The small deviation of accepted intraoperative alignment from desired or targeted alignment indicates it is possible to generate consistent alignment results through the use of a navigation system. In this study, we maintained a target implant alignment of 0° in the AP mechanical and sagittal femoral and tibial axes. We cannot claim this is the “correct” target alignment or even that it represents the alignment most likely to yield positive clinical and functional outcomes, but simply that it represented our target or “desired” alignment, which CAS effectively helped to achieve. Although there may be a small inherent degree of error associated with navigation-generated measurements, this tool is highly effective at generating precise and accurate alignment outcomes in TKA and may function as a valuable supplement for measurement of TKA limb alignment.
Precise pre- and postoperative measurements of limb alignment are necessary to plan and evaluate the success of TKA. There is a wealth of published literature attesting to the precision of intraoperative navigation systems; however, the vast majority of published studies use radiographic measurements as “the gold standard” for TKA alignment evaluation [1–3, 6, 10, 13, 16, 21, 24, 30, 33–35]. Radiographic measurements have inherent limitations and do not possess the precision, accuracy, or reproducibility necessary to function as the primary measure of limb and implant alignment in TKA. Factors including soft tissue conditions and patient positioning, human error in alignment measurements, and imprecise landmark demarcation contribute to the imprecision of this imaging modality. A degree of caution should be exercised when attempting to draw firm conclusions from clinical studies using plain radiographs to evaluate small differences or changes in alignment. Navigation offers the potential to function as a highly effective tool for measuring limb and implant alignment, because we believe the error inherent to the use of a navigation system is considerably less and more controllable than the error inherent to standard radiographs. Although we believe navigation is currently capable of generating precise, accurate, and reproducible alignment measurements, there is a major need for additional study in this area. It is still unclear to exactly what degree navigation is capable of accurately determining alignment measurements in the hands of an experienced user and in a clinical setting. A high-quality study comparing computed tomography, navigation, and radiographic limb and implant alignment measurements would provide great value. A study of this type could further assist in the adoption and validation of navigation as a technology capable of effectively assessing limb and implant alignment. This has the potential to open the door to a better understanding of the relationship that exists between intraoperative navigation measurements and long-term clinical and functional outcomes.
Acknowledgments
We thank Joseph Feinglass, PhD, Steven Gondek, MD, and Emily Martin, MD, for their valued contributions to this study.
Footnotes
One or more of the authors (SDS) has received funding from Aesculap.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bathis H, Perlick L, Tingart M, Luring C, Perlick C, Grifka J. Radiological results of image-based and non-image-based computer-assisted total knee arthroplasty. Int Orthop. 2004;28:87–90. [DOI] [PMC free article] [PubMed]
- 2.Bathis H, Perlick L, Tingart M, Luring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–687. [DOI] [PubMed]
- 3.Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D. Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am. 2007;89:261–269. [DOI] [PubMed]
- 4.Brouwer RW, Jakma TS, Brouwer KH, Verhaar JA. Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg. 2007;20:210–215. [DOI] [PubMed]
- 5.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004;86:372–377. [DOI] [PubMed]
- 6.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618–626. [DOI] [PubMed]
- 7.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39–47. [DOI] [PubMed]
- 8.Cooke TD, Scudamore RA, Bryant JT, Sorbie C, Siu D, Fisher B. A quantitative approach to radiography of the lower limb. Principles and applications. J Bone Joint Surg Br. 1991;73:715–720. [DOI] [PubMed]
- 9.Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34:1796–1801. [PubMed]
- 10.Decking R, Markmann Y, Fuchs J, Puhl W, Scharf HP. Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282–288. [DOI] [PubMed]
- 11.Delp SL, Stulberg SD, Davies B, Picard F, Leitner F. Computer assisted knee replacement. Clin Orthop Relat Res. 1998;354:49–56. [DOI] [PubMed]
- 12.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed]
- 13.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. [DOI] [PubMed]
- 14.Hauser R. Computer-aided 3D-navigation systems: a plea for an error model. HNO. 2000;2:71–74. [DOI] [PubMed]
- 15.Hunt MA, Fowler PJ, Birmingham TB, Jenkyn TR, Giffin JR. Foot rotational effects on radiographic measures of lower limb alignment. Can J Surg. 2006;49:401–406. [PMC free article] [PubMed]
- 16.Jenny JY, Boeri C. Computer-assisted implantation of a total knee arthroplasty: a case-controlled study in comparison with classical instrumentation [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:645–652. [PubMed]
- 17.Jenny JY, Boeri C, Picard F, Leitner F. Reproducibility of intra-operative measurement of the mechanical axes of the lower limb during total knee replacement with a non-image-based navigation system. Comput Aided Surg. 2004;9:161–165. [DOI] [PubMed]
- 18.Kendoff D, Board TN, Citak M, Gardner MJ, Hankemeier S, Ostermeier S, Krettek C, Hufner T. Navigated lower limb axis measurements: influence of mechanical weight-bearing simulation. J Orthop Res. 2008;26:553–561. [DOI] [PubMed]
- 19.Laskin R. Alignment in total knee components. Orthopedics. 1984;7:62–72. [DOI] [PubMed]
- 20.Lonner JH, Laird MT, Stuchin SA. Effect of rotation and knee flexion on radiographic alignment in total knee arthroplasties. Clin Orthop Relat Res. 1996;331:102–106. [DOI] [PubMed]
- 21.Mahaluxmivala J, Bankes MJ, Nicolai P, Aldam CH, Allen PW. The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty. 2001;16:635–640. [DOI] [PubMed]
- 22.McGrory JE, Trousdale RT, Pagnano MW, Nigbur M. Preoperative hip to ankle radiographs in total knee arthroplasty. Clin Orthop Relat Res. 2002;404:196–202. [DOI] [PubMed]
- 23.Oberst M, Bertsch C, Lahm A, Wuerstlin S, Holz U. Regression and correlation analysis of preoperative versus intraoperative assessment of axes during navigated total knee arthroplasty. Comput Aided Surg. 2006;11:87–91. [DOI] [PubMed]
- 24.Perlick L, Bathis H, Perlick C, Luring C, Tingart M, Grifka J. Revision total knee arthroplasty: a comparison of postoperative leg alignment after computer-assisted implantation versus the conventional technique. Knee Surg Sports Traumatol Arthrosc. 2005;13:167–173. [DOI] [PubMed]
- 25.Picard F, Gregori A, Leitner F. Computer Assisted Total Knee Arthroplasty: Validation of the Image Free Concept. Berlin, Germany: Pro Business; 2007.
- 26.Pitto RP, Graydon AJ, Bradley L, Malak SF, Walker CG, Anderson IA. Accuracy of a computer-assisted navigation system for total knee replacement. J Bone Joint Surg Br. 2006;88:601–605. [DOI] [PubMed]
- 27.Prakash U, Wigderowitz CA, McGurty DW, Rowley DI. Computerised measurement of tibiofemoral alignment. J Bone Joint Surg Br. 2001;83:819–824. [DOI] [PubMed]
- 28.Rauh MA, Boyle J, Mihalko WM, Phillips MJ, Bayers-Thering M, Krackow KA. Reliability of measuring long-standing lower extremity radiographs. Orthopedics. 2007;30:299–303. [DOI] [PubMed]
- 29.Siu D, Cooke TD, Broekhoven LD, Lam M, Fisher B, Saunders G, Challis TW. A standardized technique for lower limb radiography. Practice, applications, and error analysis. Invest Radiol. 1991;26:71–77. [DOI] [PubMed]
- 30.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br. 2003;85:830–835. [PubMed]
- 31.Specogna AV, Birmingham TB, DaSilva JJ, Milner JS, Kerr J, Hunt MA, Jones IC, Jenkyn TR, Fowler PJ, Giffin JR. Reliability of lower limb frontal plane alignment measurements using plain radiographs and digitized images. J Knee Surg. 2004;17:203–210. [DOI] [PubMed]
- 32.Specogna AV, Birmingham TB, Hunt MA, Jones IC, Jenkyn TR, Fowler PJ, Giffin JR. Radiographic measures of knee alignment in patients with varus gonarthrosis: effect of weightbearing status and associations with dynamic joint load. Am J Sports Med. 2007;35:65–70. [DOI] [PubMed]
- 33.Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;426:180–186. [DOI] [PubMed]
- 34.Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84(Suppl 2):90–98. [PubMed]
- 35.Stulberg SD, Yaffe MA, Koo SS. Computer-assisted surgery versus manual total knee arthroplasty: a case-controlled study. J Bone Joint Surg Am. 2006;88(Suppl 4):47–54. [DOI] [PubMed]
- 36.Stulberg SD, Yaffe MA, Koo SS. Navigation improves accuracy and reproducibility of soft tissue balance in TKA. Poster presentation: International Society for Computer Assisted Orthopedic Surgery 7th Annual Meeting. Heidelberg, Germany, June 20–23, 2007. http://www.caos-international.org/2007/FinalProgram.pdf.
- 37.Wright JG, Treble N, Feinstein AR. Measurement of lower limb alignment using long radiographs. J Bone Joint Surg Br. 1991;73:721–723. [DOI] [PubMed]
- 38.Yau WP, Leung A, Chiu KY, Tang WM, Ng TP. Intraobserver errors in obtaining visually selected anatomic landmarks during registration process in nonimage-based navigation-assisted total knee arthroplasty: a cadaveric experiment. J Arthroplasty. 2005;20:591–601. [DOI] [PubMed]
- 39.Yau WP, Leung A, Liu KG, Yan CH, Wong LL, Chiu KY. Interobserver and intra-observer errors in obtaining visually selected anatomical landmarks during registration process in non-image-based navigation-assisted total knee arthroplasty. J Arthroplasty. 2007;22:1150–1161. [DOI] [PubMed]
- 40.Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989;7:132–137. [DOI] [PubMed]