Abstract
Computer-navigated and minimally invasive TKAs are emerging technologies that have distinct strengths and weaknesses. We compared duration of surgery, length of hospitalization, Knee Society scores, radiographic alignments, and complications in two unselected groups of 81 consecutive knees that underwent TKA using either a minimally invasive approach or computer navigation. The two groups were operated on by two different surgeons over differing timeframes. The mean surgical time was longer in the navigated group by 63 minutes. The Knee Society scores and lengths of hospitalization of the two groups were similar. The postoperative component alignments of the two groups were similar; the mean femoral valgus and tibial varus angles of the navigation group changed from 96° and 88° preoperatively to 95° and 89° postoperatively, respectively, and in the minimally invasive group, the mean femoral valgus angles and tibial varus angles changed from 97° and 88° preoperatively to 95° and 89° postoperatively, respectively. There were 11 major and three minor complications in the navigation group, including one revision, two femoral shaft fractures, four reoperations for knee stiffness, and four instances of bleeding from tracker sites. We believe the higher incidence of complications in addition to the longer operative time in the navigated group may outweigh any potential radiographic benefits.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Various minimally invasive techniques have been developed for TKA in an effort to decrease early morbidity and to aid rehabilitative efforts. Minimally invasive TKA has been associated with less pain (15% fewer patients reported pain at 6 weeks in one study and 15% less epidural pain medication was used in another) [1, 5, 16]; reduced mean length of hospitalization (2.2 versus 2.7 days) in one study [16]; a higher mean arc of motion on Day 1 (by 25°) at 6 weeks (by 5°–15°) and 1 year (by 4°–9°) postoperatively in various studies [11, 12, 16]; and better early quadriceps muscle strength (81% versus 29% could perform a straight-leg raise on the first postoperative day in one study and mean time to performance of a straight-leg raise was 2 versus 5 days in another study) [12, 23]. One multicenter report demonstrated no differences in the results of minimally invasive and conventional approaches [15]. However, another study reported higher rates of varus malalignment (13% versus 0%) using a minimally invasive approach [5].
Computer-assisted navigation surgery has also been developed to aid the surgeon in achieving improved alignment, presumably leading to better short- and long-term outcomes. Some studies have reported navigation techniques are associated with more precise component alignment (specifically, fewer outliers of more than 3°) when compared with standard techniques for TKA [4, 8, 18, 19]. Other reports document disadvantages, including increased operative time and more complications [2, 3, 22]. Many surgeons view minimally invasive and navigation techniques as becoming standard in the future. Some believe in the possibility of combining the two methods, although both are new technologies of still unproven benefit over conventional methods. Several studies have compared minimally invasive TKA using navigation with conventional TKA [7, 19], but the two new approaches have not been individually compared.
Because the literature is mixed on the benefits and disadvantages of the two procedures, we compared perioperative parameters (surgical time and estimated blood loss), clinical variables (Knee Society knee scores as well as range of motion at last followup), radiographic data (radiolucencies and tibiofemoral axis alignment), and complication rates in a group of patients who underwent minimally invasive TKA with those in a group treated with navigation.
Materials and Methods
We compared the clinical and radiographic outcomes of two groups of 81 TKAs performed between January 1, 2004, and January 1, 2006. As a control, we obtained similar data from 50 consecutive cases performed by each surgeon with standard TKA approaches performed just before the techniques used in this study and at a followup time similar to that of the two primary study groups. One author (DD) used computer-assisted navigation for all TKAs. Another author (PMB) used a minimally invasive approach without navigation. However, the navigation surgeon had less volume so the cases were completed over a 2-year timespan, whereas the minimally invasive surgeon finished the 81 cases in approximately 4 months. We included all patients in both groups in which the procedures were used during the timeframe; that is, no patients were excluded. Patients in both groups were followed for a minimum of 2 years (mean, 3 years; range, 2–4 years). No patients were lost to followup. We compared perioperative parameters (surgical time and estimated blood loss), clinical variables (Knee Society knee scores and ranges of motion at last followup), radiographic data (radiolucencies and tibiofemoral axis alignment), and complication rates. Institutional Review Board approval was obtained to enroll these patients in the study.
All patients in both groups had been diagnosed with osteoarthritis of the knee that had failed nonoperative treatment. In the navigation group, there were 33 women (52 knees) and 22 men (29 knees) who had a mean age of 64 years (range, 39–100 years). In the minimally invasive group, there were 37 women (53 knees) and 18 men (28 knees) who had a mean age of 71 years (range, 47–88 years). Other demographic variables such as body mass index and preoperative alignment variables were similar between the two groups (Table 1).
Table 1.
Demographic and preoperative data of the navigation and minimally invasive groups
| Demographic information | Navigation group | Minimally invasive group |
|---|---|---|
| Number of patients (knees) | 55 (81) | 55 (81) |
| Men | 22 (29) | 18 (28) |
| Women | 33 (52) | 37 (53) |
| Age in years, mean (range) | 64 (39–90) | 71 (47–88) |
| Body mass index, mean (range) | 34 (23–53) | 32 (19–56) |
| Preoperative alignment in degrees (range) | ||
| Anatomic axis of the knee* | 1 (−9–20) | 2 (−8–13) |
| Femoral valgus angle | 96 (81–101) | 97 (83–101) |
| Tibial varus angle | 88 (76–100) | 88 (79–97) |
| Knee Society scores in points, mean (range) | ||
| Knee | 39 (0–65) | 31 (12–40) |
| Functional | 46 (0–70) | 34 (0–65) |
* Negative values indicate varus alignment.
The minimally invasive technique was performed with a medial patellar incision, typically less than 10 cm long, which represented no more than twice the length of the patella. A modified vastus medialis obliquus muscle snip approach was made, which allowed for exposure of the knee without everting the patella. Using downsized instrumentation, all knees had a Scorpio™ Total Knee System (Stryker Orthopaedics, Mahwah, NJ) implanted. All components (femoral, tibial, and patellar) were cemented in all cases.
The patients in the navigation group underwent TKA using a conventional midvastus approach with an incision approximately 15 cm in length. A modified vastus medialis obliquus snip was performed, but the patella was everted and the tibiofemoral joint was dislocated as part of each procedure. The navigation system used a variable number of tracker pins (4.5-mm pins placed bicortically in the diaphysis of the femur and tibia) using the Stryker Navigation System (Stryker Orthopaedics). The navigation system was used to guide the bone cuts in both the coronal and sagittal planes as well as to verify the final bone cuts and the seating of the components.
The patients were evaluated independently by a registered nurse (MM) preoperatively, 6 weeks after the procedure, and at annual followup visits using the Knee Society clinical scoring system [13]. From the medical records, we obtained the duration of the procedure, the length of hospital stay, and the perioperative complications. We searched the records for any major or minor complications both perioperatively and at followup visits.
Anteroposterior and lateral weightbearing radiographs were taken preoperatively, within 6 weeks postoperatively, and afterward as needed by the same radiology technicians. Two research staff members and one author (LR, MM, PMB) evaluated all radiographs independently, and if there was disagreement, the radiograph was reexamined until a unanimous decision was made. Collection of radiographic data did not begin until investigators had performed an analysis of intra- and interobserver agreement with regard to radiographic alignment. Radiographs were not assessed for the study until the evaluators agreed, within 1° or less, with themselves on different days and with each other more than 90% of the time. The anatomic axis alignment as well as the alignment of the femoral and tibial components were determined in the anteroposterior and lateral projections. In addition, the femoral, tibial, and patellar components were divided into zones and evaluated for radiolucencies according to the method described by the Knee Society [9]. The width of each radiolucency was measured, all widths for each component were added, and any sums greater than 10 mm or progression of radiolucencies were considered signs of component loosening.
A chart review was conducted to collect data and evaluate 50 consecutive TKAs performed by each surgeon with standard approaches just before the techniques used in this study and at a followup time similar to the two primary study groups. The conventional TKAs that were performed by one author (PMB) occurred over a 6-month period during 2002 (which was the last time this author performed conventional TKAs) and the TKAs that were performed by the other author occurred over a 6-month period during 2004 and 2005, which directly preceded the navigation study group. The clinical evaluations of these patients were performed at the same followup times as those in the current groups of study patients (mean, 3 years; range, 2–4 years). The TKAs were all performed using a conventional midvastus approach with an incision of 15 to 20 cm. Navigation was not used. The perioperative variables (surgery duration and estimated blood loss) and postoperative variables (Knee Society knee score, range of motion, and tibiofemoral axis) were examined to assess the comparability of the two surgeons as well as to compare the conventional methods with the techniques used in the present study.
We compared the various clinical and radiographic parameters of the two study groups. In addition, to lessen the chance of surgeon bias, we compared the parameters of each surgeon’s study group with his historical conventional group, and we compared the parameters of the two conventional groups with each other. We determined differences in perioperative variables (surgical time and estimated blood loss), clinical scores (Knee Society knee scores as well as ranges of motion at last followup), and radiographic data (radiolucencies and tibiofemoral axis alignment). A repeated-measures analysis of variance was used to compare the variables, and the Holm-Sidak method of multiple pairwise comparisons was used when major differences were found among the groups. In addition, the number of major and minor complications was compared among the previously mentioned groups. We used SPSS version 13.0 (SPSS Inc, Chicago, IL) for all analyses.
Results
The perioperative variables of the navigation and minimally invasive groups were similar, except the mean duration of surgery was longer (p = 0.001) in the navigated group (mean, 121 minutes; range, 60–202 minutes) than in the minimally invasive group (mean, 58 minutes; range, 37–134 minutes). The other values were similar between the two study groups. In examining the perioperative variables of the two control groups, the surgeon who used navigation in the current study had a longer (p = 0.001) mean surgical time than the surgeon who used a minimally invasive approach in the current study. The estimated mean blood loss was similar between the two treatment groups as well as between the two control groups, but the mean blood loss was higher (p = 0.02) in the control groups compared with the treatment groups. There were no differences in duration of hospitalization among the four groups. Table 2 shows the perioperative parameters of all of the control and study groups.
Table 2.
Perioperative and postoperative results of navigation and minimally invasive total knee arthroplasty
| Variable | Navigation group | Minimally invasive group | Conventional group (DAD)* | Conventional group (PMB)* | p value |
|---|---|---|---|---|---|
| Mean operative time in minutes (range) | 121 (59–202) | 58 (37–137) | 87 (63–118) | 71 (50–111) | 0.0001 |
| Estimated blood loss in milliliters (range) | 66 (0–300) | 55 (0–200) | 98 (50–350) | 115 (50–200) | 0.020 |
| Mean duration of hospitalization in days (range) | 4 (3–8) | 4 (3–7) | 4 (3–8) | 4 (3–8) | 0.791 |
| Knee Society knee score in points (range) | 91 (40–100) | 93 (64–100) | 93 (72–100) | 95 (87–100) | 0.075 |
| Range of motion in degrees (range) | 114 (90–120) | 117 (95–120) | 113 (80–130) | 116 (90–130) | 0.030 |
* Initials in parentheses are authors who were the surgeons performing these operations.
We found no differences between the navigation and the minimally invasive surgery groups in the clinical scores at last followup (Table 2). The Knee Society knee scores for the navigation and minimally invasive groups improved from means of 39 and 31 points to 91 and 93 points, respectively. The control groups had similar (p = 0.075) postoperative clinical scores. The mean range of motion of the navigation group was higher by 2° (p = 0.026) than for the other three groups, but this is not likely a clinically important difference.
Mean postoperative alignment was similar between the two study groups in the coronal and sagittal planes and had a narrower range than the preoperative values. In the navigation group, the mean postoperative femoral valgus angle was 95° (range, 91°–100°) and the mean tibial varus angle was 89° (range, 86°–98°). In the minimally invasive group, the mean postoperative femoral valgus angle was 95° (range, 90°–100°) and the mean tibial varus angle was 89° (range, 86°–92°). Assessment of radiolucencies revealed no progressive radiolucencies, and there were no radiographs in which the total width of radiolucencies was greater than 5 mm. The mean anatomic axis angles of the knees of the conventional groups were similar.
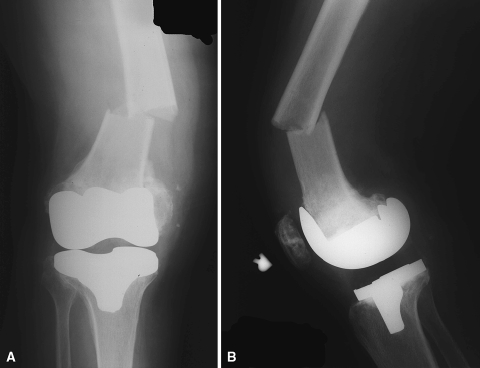
There were 11 major complications in the navigation group, including one revision; four reoperations for knee stiffness; two femoral neck fractures at the sites of tracker pin insertions, which both required open reduction and internal fixation (Fig. 1); and four bleeding complications, which required aspiration. There were also three minor complications, including a deep venous thrombosis, a peroneal nerve palsy, and a wound infection, each of which resolved with anticoagulation medication, physical therapy, and antibiotics, respectively. In comparison, there were six major complications in the minimally invasive surgery group, including one revision and five reoperations for knee stiffness. There was also one deep venous thrombosis, which resolved with anticoagulation medication. The conventional groups that were performed by the navigation author and the minimally invasive author had reoperation rates of 10% and 4%, respectively, consisting of one revision in each group as well as arthroscopic contracture releases for knee stiffness. We have provided details of the complications of all four groups (Table 3).
Fig. 1A–B.
A 71-year-old woman experienced a femoral fracture associated with the tracker pin site after her navigation-assisted TKA as can be seen in (A) anteroposterior and (B) lateral radiographs.
Table 3.
Summary of complications
| Complications | Navigated group | Minimally invasive group | Conventional group (DAD)* | Conventional group (PMB)* |
|---|---|---|---|---|
| Femoral shaft fracture | 2 | 0 | 0 | 0 |
| Revision | 1 | 1 | 1 | 1 |
| Deep venous thrombosis | 1 | 1 | 0 | 0 |
| MUA | 3 | 3 | 0 | 0 |
| Nerve lesion | 1 | 0 | 0 | 0 |
| Hematoma (tracker site) | 3 | 0 | 0 | 0 |
| Hemarthrosis | 1 | 0 | 0 | 0 |
| Infection | 1 | 0 | 0 | 0 |
| Arthroscopic contracture release | 1 | 2 | 4 | 1 |
| Total | 14 | 7 | 5 | 2 |
* Initials in parentheses are authors who were the surgeons performing these operations; MUA = manipulation under anesthesia.
Discussion
Computer-assisted navigation and minimally invasive TKA are both emerging technologies that have distinct strengths and weaknesses. Navigation reportedly improves alignment of components [4, 8, 18, 19], although some studies report greater operative times and more complications than TKA without navigation [2, 3, 22]. Minimally invasive TKA may decrease postoperative pain [1, 5, 16], shorten recovery time [1, 16], and improve function [1, 11, 12, 16, 23], but it has also been associated with a higher number of complications and failures [5]. As a result, we compared perioperative variables (surgical time and estimated blood loss), clinical scores (Knee Society knee scores as well as range of motion at last followup), radiographic data (radiolucencies and tibiofemoral axis alignment), and complications of a group of patients who were treated with minimally invasive surgery with a group of patients who were treated with navigation.
There were several limitations of this study. First, two surgeons performed the surgeries over varying lengths of time, and some of the differences might be explained by differences in surgical technique. However, both surgeons are partners who operate in the same hospital with similar patient populations, indications, anesthesia, pain management, venous thromboembolism prophylaxis, and rehabilitation. In addition, we used each surgeon’s historical data of 50 TKAs performed with standard approaches as an internal control, which showed the two surgeons had different surgical times in the conventional groups but otherwise similar results. This may mean the differences in surgical times of the two study groups might be attributable to differences between the surgeons, but the surgical times for the navigation study group were considerably longer than the surgical times for the conventional group performed by the same author. Another potential limitation is the navigation surgeon might have been early on the learning curve, although the femur fractures were Cases 62 and 75 in the series. Finally, the mean followup time was only 3 years. Nevertheless, we believe the increased complications with navigation have implications for how to perform these surgeries in the future (ie, without diaphyseal-placed tracker pins).
A number of studies suggest navigation can increase the accuracy of component alignment, although it can also increase operative time and complications (Table 4) [6, 8, 10, 17, 18, 20–22]. A prospective, randomized study compared 60 conventional with 60 navigated TKAs and found the percentage of knees in which the mechanical axes deviated more than 3° was 20% and 1.7% in the two groups, respectively [8]. However, a case-control study that compared navigation with conventional TKAs found navigation was associated with a greater mean estimated blood loss as well as a longer mean surgical time by 27 minutes, whereas the alignment and Knee Society scores were similar [22]. Another study reported an increased risk of complications using navigation, including fractures and nerve lesions [20]. These studies corroborate the present study, which found slight improvement in accuracy of alignment, but also a higher rate of complications, especially femur fractures, with the navigation technique.
Table 4.
Comparison studies of navigation versus conventional total knee arthroplasty
| Author | Year | Type of study | Number of knees | Results of navigation versus conventional procedure |
|---|---|---|---|---|
| Ensini et al. [8] | 2007 | Level I randomized, prospective | 60 versus 60 | Similar clinical outcomes; fewer radiographic outliers |
| Matziolis et al. [18] | 2007 | Level I randomized, prospective | 32 versus 28 | Improved alignment of the femoral component and mechanical axis;similar blood loss and surgical time |
| Martin and von Strempel [17] | 2006 | Level II prospective comparative | 21 versus 21 | Increased operative time;similar radiographic measurements and percentage of outliers |
| Chin et al. [4] | 2005 | Level I randomized, prospective | 30 versus 30 | Improved accuracy, fewer outliers in coronal and sagittal axis |
| Decking et al. [6] | 2005 | Level I randomized, prospective | 27 versus 25 | Fewer radiographic outliers |
| Haaker et al. [10] | 2005 | Level II retrospective comparative | 100 versus 100 | Improved precision of tibial and femoral components with fewer outliers |
| Stockl et al. [21] | 2004 | Level I prospective comparative | 32 versus 32 | Improved mechanical axis, posterior tibial slope, and rotational alignment as well as flexion angle of femoral component |
| Chauhan et al. [3] | 2004 | Level I randomized, prospective | 35 versus 35 | Improved alignment; less blood loss, worse surgical time |
Studies of minimally invasive TKA have reported mixed outcomes (Table 5) [5, 14, 19, 21, 23, 24]. A comparison of minimally invasive TKA with navigation with a group of conventional TKAs found the minimally invasive group had better pain scores and a shorter time to achieve 90° of flexion and straight-leg raises [19]. Another report found four of 30 patients who underwent TKA using a minimidvastus approach had tibial components placed in 3° or more of varus malalignment, which was not found in a conventional group [5]. The present study found no differences between the two approaches at a followup time of 3 years.
Table 5.
Comparison studies of minimally invasive versus conventional total knee arthroplasty
| Author | Year | Type of study | Number of knees | Results of minimally invasive versus conventional surgery |
|---|---|---|---|---|
| King et al. [14] | 2007 | Level III, retrospective comparative | 100 versus 50 | Significantly longer operative time; worse patellar alignment, but improvement over learning curve; shorter hospital stay, less narcotic use, faster return to function |
| Tashiro et al. [23] | 2007 | Level III retrospective comparative | 24 versus 25 | Longer operative time; faster return to function; no complications |
| Dalury and Dennis [5] | 2005 | Level III retrospective comparative | 30 versus 30 | Less epidural pain medication use; four of 30 patients had varus malalignment (zero of 30 in control group) |
| Bonutti et al. [1] | 2004 | Level II prospective comparative | 32 versus 29 | Similar Knee Society scores |
| Haas et al. [11] | 2004 | Level III prospective comparative | 40 versus 40 | Longer operative time; improved range of motion at 6 weeks, 12 weeks, and 1 year; improved Knee Society knee score (97 points versus 91 points) |
| Tria and Coon [24] | 2003 | Level III case-control | 60 versus 60 | Lower blood loss, shorter hospital stay, improved motion; improved pain score on first postoperative visit |
New developments might decrease the rate of fractures and hematomas associated with navigation. The use of thinner tracking pins placed in the metaphysis rather than the diaphysis might help reduce long bone fractures. Pinless navigation systems that use skin or bone mapping might be useful in the future.
The cost to obtain a navigation system was $193,000 in 2004 with an additional upgrade cost of $146,712 in 2007. The additional costs per procedure associated with navigation were calculated as $409 for disposable navigation instruments, $400 for the additional time in the operating room, and $116 for the additional anesthesia. This does not include additional trained personnel who may be needed if a representative is not available.
Additional operating time was required for navigation with added costs for purchasing and maintaining the system. We also found a larger number of major complications in this group, particularly femoral shaft fractures and hematomas. Clinical results were similar at a minimum followup of 2 years. Future changes to the navigation systems might improve the results, but at present, the complications combined with the costs may outweigh any potential radiographic benefits.
Acknowledgments
We thank Lindsay Rudert, Margo McMahon, Gina Zerrusen, and Colleen Kazmarek for collecting data and assisting with the preparation of the manuscript.
Footnotes
One or more of the authors (PMB, DAD, MAM) are consultants for and receive funding from Stryker.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bonutti PM, Mont MA, McMahon M, Ragland PS, Kester M. Minimally invasive total knee arthroplasty. J Bone Joint Surg Am. 2004;86(Suppl 2):26–32. [DOI] [PubMed]
- 2.Chang CW, Yang CY. Kinematic navigation in total knee replacement—experience from the first 50 cases. J Formos Med Assoc. 2006;105:468–474. [DOI] [PubMed]
- 3.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004;86:372–377. [DOI] [PubMed]
- 4.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618–626. [DOI] [PubMed]
- 5.Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res. 2005;440:77–81. [DOI] [PubMed]
- 6.Decking R, Markmann Y, Fuchs J, Puhl W, Scharf HP. Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282–288. [DOI] [PubMed]
- 7.Dutton AQ, Yeo SJ, Yang KY, Lo NN, Chia KU, Chong HC. Computer-assisted minimally invasive total knee arthroplasty compared with standard total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2008;90:2–9. [DOI] [PubMed]
- 8.Ensini A, Catani F, Leardini A, Romagnoli M, Giannini S. Alignments and clinical results in conventional and navigated total knee arthroplasty. Clin Orthop Relat Res. 2007;457:156–162. [DOI] [PubMed]
- 9.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed]
- 10.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. [DOI] [PubMed]
- 11.Haas SB, Manitta MA, Burdick P. Minimally invasive total knee arthroplasty: the mini midvastus approach. Clin Orthop Relat Res. 2006;452:112–116. [DOI] [PubMed]
- 12.Huang HT, Su JY, Chang JK, Chen CH, Wang GJ. The early clinical outcome of minimally invasive quadriceps-sparing total knee arthroplasty: report of a 2-year follow-up. J Arthroplasty. 2007;22:1007–1012. [DOI] [PubMed]
- 13.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 14.King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am. 2007;89:1497–1503. [DOI] [PubMed]
- 15.Kolisek FR, Bonutti PM, Hozack WJ, Purtill J, Sharkey PF, Zelicof SB, Ragland PS, Kester M, Mont MA, Rothman RH. Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. J Arthroplasty. 2007;22:8–13. [DOI] [PubMed]
- 16.Lombardi AV Jr, Viacava AJ, Berend KR. Rapid recovery protocols and minimally invasive surgery help achieve high knee flexion. Clin Orthop Relat Res. 2006;452:117–122. [DOI] [PubMed]
- 17.Martin A, von Strempel A. Two-year outcomes of computed tomography-based and computed tomography free navigation for total knee arthroplasties. Clin Orthop Relat Res. 2006;449:275–282. [DOI] [PubMed]
- 18.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. [DOI] [PubMed]
- 19.Seon JK, Song EK. Navigation-assisted less invasive total knee arthroplasty compared with conventional total knee arthroplasty: a randomized prospective trial. J Arthroplasty. 2006;21:777–782. [DOI] [PubMed]
- 20.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br. 2003;85:830–835. [PubMed]
- 21.Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;426:180–186. [DOI] [PubMed]
- 22.Stulberg SD, Yaffe MA, Koo SS. Computer-assisted surgery versus manual total knee arthroplasty: a case-controlled study. J Bone Joint Surg Am. 2006;88(Suppl 4):47–54. [DOI] [PubMed]
- 23.Tashiro Y, Miura H, Matsuda S, Okazaki K, Iwamoto Y. Minimally invasive versus standard approach in total knee arthroplasty. Clin Orthop Relat Res. 2007;463:144–150. [PubMed]
- 24.Tria AJ Jr, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res. 2003;416:185–190. [DOI] [PubMed]