Abstract
Proper femoral and tibial component rotational positioning in TKA is critical for outcomes. Several rotational landmarks are frequently used with different advantages and limitations. We wondered whether coronal axes in the tibia and femur based on the transepicondylar axis in the femur would correlate with anteroposterior deformity. We obtained computed tomography scans of 100 patients with arthritis before they underwent TKA. We measured the posterior condylar angle on the femoral side and the angle between Akagi’s line and perpendicular to the projection of the femoral transepicondylar axis on the tibial side. On the femoral side, we found a linear relationship between the posterior condylar angle and coronal deformity with valgus knees having a larger angle than varus knees, ie, gradual external rotation increased with increased coronal deformity from varus to valgus. On the tibial side, the angle between Akagi’s line and the perpendicular line to the femoral transepicondylar axis was on average approximately 0°, but we observed substantial interindividual variability without any relationship to gender or deformity. A preoperative computed tomography scan was a useful, simple, and relatively inexpensive tool to identify relevant anatomy and to adjust rotational positioning. We do not, however, recommend routine use because on the femoral side, we found a relationship between rotational landmarks and coronal deformity.
Introduction
Rotational positioning of femoral and tibial components has emerged as a critical aspect of TKA because the consequences of malrotation may produce patellofemoral problems, flexion instability, ultrahigh-molecular-weight polyethylene or post wear, stiffness, and abnormal gait patterns. Achieving correct rotation is difficult using traditional methods and with navigation [17] for the femur and the tibia. For the femur, at least four methods have been reported: (1) flexion gap balancing (tibial cut or shaft axis) [9, 20]; (2) posterior condylar line plus a few degrees of fixed external rotation [12]; (3) Whiteside’s anteroposterior axis (trochlear line) [4, 25]; and (4) transepicondylar axis (TEA) [5, 10, 19]. Each method has its advantages and disadvantages, but most of them show low interindividual reproducibility [15, 18, 23].
Traditional methods on the tibial side include the “classic” medial one-third of the tibial tubercle [7] or self-alignment of a conforming mobile tibial insert in extension (range of motion with a “floating insert”) [17]. Comparative studies [7] demonstrate the difficulties in achieving the desired rotation, relative to the TEA, typically showing outliers with abnormal external or internal rotation. Recently, Ikeuchi et al. [13] reported a greater likelihood of tibial component internal rotation when using the self-aligning method. A rotational mismatch with TEA of more than 10° was found by Uehara et al. [24] using different methods on postoperative computed tomography (CT) scans in 12% of the cases. In another study, the neutral point of the rotating insert in extension, relative to the medial one-third of the tibial tubercle, was more than 10° in 5% of the cases [18]. Recently, preoperative CT scanning methods have been introduced for the femur by Yoshino et al. [26] and Akagi et al. [3]. In the tibia, Akagi et al. described a new anteroposterior axis [1, 2], which is the line connecting the midposterior cruciate ligament attachment to the medial border of the tibial plateau. This axis is perpendicular to the femoral TEA. Therefore, the axis reference of Akagi et al. [1, 2] on the tibia should take into account also the femoral TEA. However, it is unclear whether routine preoperative CT scanning is a useful tool to improve positioning.
The purpose of our study was to (1) ascertain whether a reference system to determine rotational deformity using the femoral TEA on both bones correlated with anteroposterior tibiofemoral angulation; we specifically used the angle of the TEA with the posterior condylar line (posterior condylar angle) on the femur and the angle between the perpendicular line to the TEA and the line of Akagi et al. [1, 2] on the tibia; and (2) determine if there were gender differences in any relationship.
Materials and Methods
We obtained preoperative knee CT scans on all 100 patients with primary osteoarthritis undergoing TKA between January 2007 and July 2007. The mean age was 72 years (range, 59–83 years). There were 73 women and 27 men. The mechanical axis on standing long anteroposterior films (obtained under fluoroscopic control with the patella facing the radiographic source) ranged from 20° of valgus to 23° of varus. Five patients had an axis of 0° ± 2° (neutral), 79 greater than 2° varus, and 16 greater than 2° valgus from the mechanical axis. All patients signed informed consent for the procedure; informed consent for participation in the study was not required by our ethics board.
We used a Siemens Somatom Emotion CT scanner (Siemens Medical Solutions USA, Malvern, PA) for all scans. The patient was placed in the supine position on the scanning table with the affected leg in full extension. Twelve patients with a flexion contracture greater than 10° were not included in the study because this would have resulted in an altered reciprocal rotational position between the femur and tibia. A scout view was obtained. To take scans perpendicular to the long axis of the leg, the scanner’s gantry was tilted based on the lateral scout view. CT images 2 mm in thickness and 2 mm in Recon increment were taken from the femoral distal metaphysis to the tibial tubercle. The reconstruction was obtained using both bone and soft tissue filters. Field parameters were not changed during reconstruction to allow image superimposition.
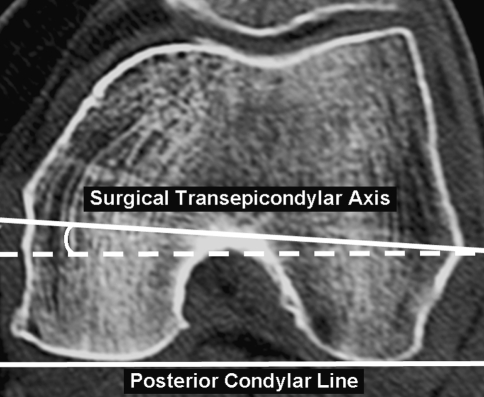
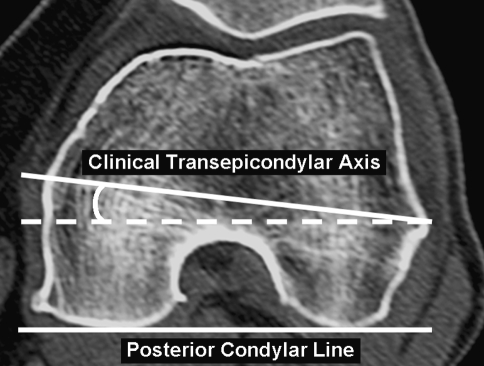
For the femur, we concentrated on the TEA, the line connecting the tip of the lateral epicondyle to the medial epicondylar ridge (clinical TEA) or the medial epicondylar sulcus (surgical TEA) as described by Berger et al. [5]. This allowed us to calculate two angles: (1) the posterior condylar angle (PCA), which is the angle formed by the posterior condylar line and the surgical TEA (Fig. 1); and (2) the condylar twist angle (CTA), which is the angle formed by the posterior condylar line and the clinical TEA, useful when the sulcus is not detectable (Fig. 2). With patience and choosing the best CT slice for sulcus identification, usually 30 mm from the joint line [21], the sulcus was detected in 80% of our patients.
Fig. 1.
The posterior condylar angle is formed by the posterior condylar line and the surgical transepicondylar axis.
Fig. 2.
The condylar twist angle is formed by the posterior condylar line and the clinical transepicondylar axis. This is used when the sulcus is absent on the medial side.
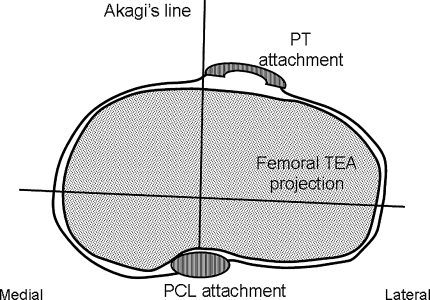
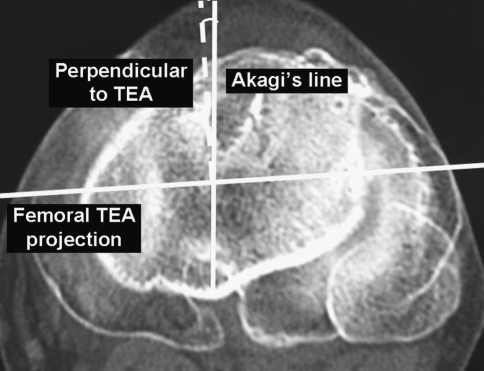
For the tibial side, Akagi et al.’s [1, 2] concept is a line perpendicular to the projection of the femoral TEA and passing through the midposterior cruciate ligament attachment is tangent to the medial patellar tendon (PT) attachment (Fig. 3). To verify this, two tibial cuts were superimposed on the computer, one passing through the midposterior cruciate ligament attachment and the other passing through the PT insertion. In this manner, the angle between the perpendicular line to the TEA and Akagi’s line was measured (tibial rotation angle [TRA]) (Fig. 4). All measurements were performed twice by a radiologist (GD) and an orthopaedic consultant (LS). We computed the intra- and interobserver variability by Pearson coefficient calculation. The intraobserver variability was 0.9 and the interobserver variability was 0.8.
Fig. 3.
The Akagi’s anteroposterior line, perpendicular to the projection of the femoral transepicondylar axis (TEA) and passing through the midposterior cruciate ligament attachment, is tangent to the medial patellar tendon attachment. PT = patellar tendon; PCL = posterior cruciate ligament.
Fig. 4.
The tibial rotation angle is the angle formed by the line perpendicular to the femoral transepicondylar axis (TEA; dotted line) and the Akagi’s anteroposterior line.
We used the Pearson correlation coefficient to determine any relationship between coronal deformity and PCA or TRA for the entire population and individually for each gender.
Results
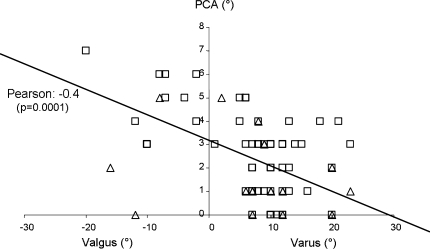
We observed a linear relationship (p = 0.0001) between the PCA and anteroposterior mechanical axis (Fig. 5). From varus to valgus for approximately every 10° increment of coronal deformity, a 1° PCA increment was observed. The PCA was greater (p = 0.001) in the valgus than in the varus knees (mean, 4.1° ± 1.9° versus 1.9° ± 1.4°, respectively). The CTA was also greater (p = 0.001) in valgus than in varus knees (mean, 8.4 ± 1.3 versus 5.6 ± 1.7, respectively). Women and men had similar PCAs (mean, 2.8 ± 1.7 for women and 2.1 ± 1.6 for men). The difference between PCA and CTA was greater (p = 0.01) in men than in women (3.0 ± 1.1 versus 3.8 ± 1 in women, respectively); women had, on average, a wider medial sulcus.
Fig. 5.
Scatterplot of posterior condylar angle (PCA) versus frontal plane deformity with men (triangles) and women (boxes). We observed a linear relationship between PCA and preoperative coronal deformity.
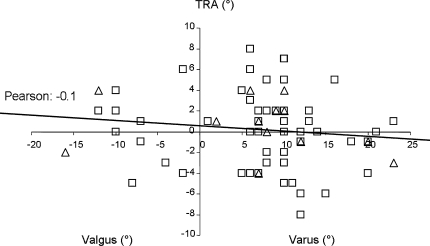
On the tibial side, the TRA was 0.1° ± 3.3° in men and 0.0° ± 3.9° in women, respectively. The TRA did not correlate (r = − 0.1) with the anteroposterior mechanical axis angle (Fig. 6).
Fig. 6.
Scatterplot of tibial rotation angle (TRA) versus frontal plane deformity with men (triangles) and women (boxes). We observed no relationship between TRA and preoperative coronal deformity.
Discussion
Component rotational positioning in TKA is critical and malpositioning impairs outcomes. The purpose of our study was to (1) ascertain whether a reference system using the femoral TEA on both bones to determine coronal angulation correlated with tibiofemoral angulation; and (2) determine if there were gender differences in any relationship.
This study has several limitations. First, it was performed on arthritic knees and this could have an influence on the results attributable particularly to cartilage erosion, especially in the posterior condyles. Matsuda et al. [16] performed a study to compare normal and osteoarthritic knees and found the latter knees differ from normal only in the valgus deformity population, whereas there was no major difference in patients with varus deformity. The increased external rotation observed in valgus knees is likely the consequence of lateral femoral condyle erosion or hypoplasia in valgus knees. However, the usefulness of the approach would be in this study population, not a normal population. Furthermore, the arthritic process can affect the reciprocal relationship between the femur and tibia in the extension position at which the CT scan was performed. To partially limit this bias, knees with a flexion contracture were not included in the series; this is not enough to bypass the altered femorotibial relative position in arthritic knees. This should not affect our femoral findings, whereas tibial measurements can be influenced by an altered femorotibial relative position in extension and may result in interindividual variability as we observed.
Other studies from different groups found similar results using different methods. The difference in distal femur rotation between valgus and varus knees has been reported [10], although not a linear relationship (ie, gradual external rotation increase with increasing coronal deformity from varus to valgus). On the tibia, other authors have reported on the superiority of the femoral TEA reference when compared with other landmarks [14].
The TEA is a valid reference for both the femur and tibia probably because it approximates the flexion-extension axis of the knee and the femoral collateral ligaments’ origin [6, 8, 11, 22, 24, 26]. Our data confirm this concept. In the femur, rotational alignment is based on coronal deformity. In the tibia, we observed high interindividual variability and no relationship either to gender or deformity.
As a consequence, in the femur, we were able to develop a simplified formula, which increases the PCA by 1° per 10° of coronal deformity increments from varus to valgus, resulting for instance in 2° external rotation for a 20° varus knee and 5° external rotation for a 20° valgus knee. Based on this concept and without the use of the preoperative CT scan, rotational accuracy is within ± 2° of TEA in 80% of the cases. Nevertheless, in patients with severe deformities (particularly in valgus) with posttraumatic arthritis or with unusual extraarticular deformities, we believe a preoperative femoral CT scan is useful. Other authors have described a larger posterior condylar angle in valgus knees than in varus [10]. This reflects the lateral femoral condyle hypoplasia, which is present in valgus knees, whereas varus knee distal femur anatomy does not differ from normal [16].
For the tibia, given the high interindividual variability with large standard deviations, the TRA is greater than +2° in 52% of the cases. Therefore, if the surgeon wants more precision, he or she should customize tibial rotation at surgery based on the preoperative CT scan and make appropriate corrections. There are other well-known methods of choosing the rotational position of the tibial component such as aligning the component with the medial third of the tibial tubercle [14] or letting a mobile tibial insert align itself with the femoral component in extension [17]. In comparative studies, these methods showed substantial variability and may require a CT scan for more precision [13]. The concept of trying to align the tibial baseplate to the femoral TEA should be retained because it was a reproducible landmark also in other studies [14].
Based on our data, in routine surgery on the femoral side, we now externally rotate the femoral component referencing off the posterior condyles using a dedicated instrument with posterior paddles that allows single-degree increments of external rotation. When performing the rotational adjustment, the surgeon should take into consideration the amount of worn posterior cartilage. This was not included in the CT measurements and failure to account for worn posterior cartilage at surgery can result in improper alignment. If cartilage wear exists, the reference paddle must be set a little apart from the posterior condyle. On the tibia, we routinely draw the Akagi’s line on the resected tibial surface with the patella reduced and then rotate the component the same amount of TRA measured on the preoperative CT scan.
Component rotational positioning is critical and malrotation has several negative consequences. Implant design features such as insert mobility can help minimize the negative effects of malrotation. On the femoral side, we found a linear relationship between coronal deformity and rotational alignment, which allows us to consistently refer off the posterior condyles and adjust rotation to deformity. On the tibial side, the Akagi’s line is a simple and useful method but with considerable interindividual variability and without any relationship to gender or deformity. Therefore, alternative landmarks should be investigated unless a preoperative CT scan is routinely performed with increased costs and ionizing radiation.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res. 2005;436:172–176. [DOI] [PubMed]
- 2.Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res. 2004;420:213–219. [DOI] [PubMed]
- 3.Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T. Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res. 2001;388:147–156. [DOI] [PubMed]
- 4.Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am. 1995;77:1331–1334. [DOI] [PubMed]
- 5.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed]
- 6.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;356:111–118. [DOI] [PubMed]
- 7.Eckhoff DG, Metzger RG, Vandewalle MV. Malrotation associated with implant alignment technique in total knee arthroplasty. Clin Orthop Relat Res. 1995;321:28–31. [PubMed]
- 8.Elias SG, Freeman MA, Gokcay EI. A correlative study of the geometry and anatomy of the distal femur. Clin Orthop Relat Res. 1990;260:98–103. [PubMed]
- 9.Fehring TK. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000;380:72–79. [DOI] [PubMed]
- 10.Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees. J Arthroplasty. 1998;13:812–815. [DOI] [PubMed]
- 11.Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res. 1993;290:259–268. [PubMed]
- 12.Hungerford DS, Krackow KA. Total joint arthroplasty of the knee. Clin Orthop Relat Res. 1985;192:23–33. [PubMed]
- 13.Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T. Determining the rotational alignment of the tibial component at total knee replacement. J Bone Joint Surg Br. 2007;89:45–49. [DOI] [PubMed]
- 14.Incavo SJ, Coughlin KM, Pappas C, Beynnon BD. Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty. J Arthroplasty. 2003;18:643–648. [DOI] [PubMed]
- 15.Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc. 2002;10:194–197. [DOI] [PubMed]
- 16.Matsuda S, Miura H, Nagamine R, Mawatari T, Tokunaga M, Nabeyama R, Iwamoto Y. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res. 2004;22:104–109. [DOI] [PubMed]
- 17.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. [DOI] [PubMed]
- 18.Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:49–64. [PubMed]
- 19.Olcott CW, Scott RD. The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res. 1999;367:39–42. [DOI] [PubMed]
- 20.Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:35–46. [DOI] [PubMed]
- 21.Stiehl JB, Abbott BD. Morphology of the transepicondylar axis and its application in primary and revision total knee arthroplasty. J Arthroplasty. 1995;10:785–789. [DOI] [PubMed]
- 22.Stiehl JB, Cherveny PM. Femoral rotational alignment using the tibial shaft axis in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:47–55. [DOI] [PubMed]
- 23.Suter T, Zanetti M, Schmid M, Romero J. Reproducibility of measurement of femoral component rotation after total knee arthroplasty using computer tomography. J Arthroplasty. 2006;21:744–748. [DOI] [PubMed]
- 24.Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y. Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2002;402:196–201. [DOI] [PubMed]
- 25.Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995;321:168–172. [PubMed]
- 26.Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty. 2001;16:493–497. [DOI] [PubMed]