Abstract
Patients undergoing bilateral total knee arthroplasty (BTKA) may have higher complication rates and mortality than those undergoing a unilateral procedure (UTKA). To evaluate this hypothesis, we analyzed nationally representative data collected for the National Hospital Discharge Survey on discharges after BTKA, UTKA, and revision TKA (RTKA) between 1990 and 2004. The demographics, comorbidities, in-hospital stay, complications, and mortality of each procedure were compared. An estimate of 4,159,661 discharges (153,259 BTKAs; 3,672,247 UTKAs; 334,155 RTKAs) were included. Patients undergoing BTKA were younger (1.5 years) and had a lower prevalence of comorbidities for hypertension (versus UTKA), diabetes, pulmonary disease, and coronary artery disease (versus UTKA and RTKA). The length of hospitalization was 5.8 days for BTKA, 5.3 for UTKA, and 5.4 for RTKA. Despite similar length of hospitalization, the prevalence of procedure-related complications was higher for BTKA (12.2%) compared with UTKA (8.2%) and RTKA (8.7%). In-hospital mortality was highest for patients undergoing BTKA (BTKA, 0.5%; UTKA, 0.3%; RTKA, 0.3%). Patients undergoing BTKA had a 1.6 times higher rate of procedure-related complications and mortality compared with those undergoing UTKA. Outcomes for patients undergoing RTKA for most variables were similar to those for UTKA. BTKA, advanced age, and male gender were independent risk factors for complications and mortality after TKA.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Total joint arthroplasty remains the most successful treatment for end-stage osteoarthritis of the knee, improving pain and function [13, 14, 25, 37, 58, 77]. The number of primary unilateral (UTKA), bilateral (BTKA), and revision TKAs (RTKA) has increased substantially over the last two decades [68, 78] and is projected to surpass a half million per year by 2030 in the United States [31, 37, 38, 46, 58, 76].
With the confidence that is associated with advancements in anesthesia, surgical technique, and perioperative care of patients undergoing UTKA, those with severe bilateral osteoarthritis of the knee are increasingly being offered bilateral, single-stage TKA [41, 56]. Single-stage BTKA has gained popularity among surgeons and patients as a result of advantages such as the need for a single anesthetic and admission, a diminished combined length of hospital stay, cost [9, 45, 49, 61], use of narcotics, and a faster overall recovery than bilateral, staged TKA [5, 11, 17, 57]. However, the use of simultaneous BTKA remains the subject of intense debate [55, 60, 76]. Despite the suggestion by some authors that the rate of medical complications is low [2, 26–29, 35, 36, 51, 52, 59, 64, 65, 67, 72, 74, 78, 79], others [1, 4, 10, 11, 42, 44, 49, 53, 62, 63], including reports based on a recent meta-analysis [60], have questioned its safety.
Despite persistent controversy over this procedure, a paucity of nationally representative data on patient demographics, comorbidities, rate of complications, and mortality exist. The published results in the literature vary and are limited to high-volume institutions [19, 51, 55]. Available population-based studies on this topic are rare [4, 62, 78] and are limited to observations in the Medicare population [4]. Because BTKA is usually indicated in younger and healthier patients, many younger than age 65, the Medicare-based studies may not capture a large proportion of the target population undergoing BTKA. Nationally representative information is of importance for physicians, patients, administrators, researchers, and policymakers alike.
To overcome the previously mentioned limitations, we used data collected in the National Hospital Discharge Survey to answer the following research questions: (1) What are the patient demographics, comorbidity profiles, hospital characteristics, in-hospital complications, and mortality of patients undergoing BTKA in the United States? (2) How do the previously mentioned variables compare with those of patients undergoing UTKA and RTKA? (3) What are the independent risk factors for complications and mortality after arthroplasty procedures of the knee? We hypothesized in a nationally representative sample, that patients undergoing BTKA would have a higher complication rate and mortality; and that BTKA would be an independent factor for adverse outcomes.
Materials and Methods
The material for our study was obtained from multiyear data files of the National Hospital Discharge Survey (NHDS) (Centers for Disease Control and Prevention, Atlanta, GA). The plan and operation of the NHDS has been published in detail [12]. In summary, the NHDS includes medical information collected annually since 1965 by the National Center for Health Statistics with the purpose of compiling nationally representative data on inpatient utilization of short-stay hospitals (Appendix 1). The hospital universe includes Medicare-participating, noninstitutional hospitals of various sizes, exclusive of military, Veterans Affairs, and federal facilities in the 50 states and the District of Columbia. Hospitals included in the survey are required to have an average length of stay of less than 30 days to be considered short-stay or to be a general medical or surgical hospital regardless of length of stay. Facilities are also required to have at least six beds for patient use. Periodic updates of the hospital universe are performed to account for changes.
To ensure accurate, nationally representative sampling, the NHDS uses a complex three-stage probability design. Information collected in the survey includes diagnosis and procedure codes (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM]), age, gender, race, principal expected source of payment (insurance status), length of care, hospital size, US region, and patient discharge status. Weighted data, with weights derived from census data by the NHDS, were provided to generate unbiased national estimates from the sample (1% of all hospital discharges in the United States).
The NHDS has been used extensively in the past to analyze data associated with a wide range of procedures across a variety of medical specialties. Over 400 select medical publications that used data from the NHDS or the National Survey of Ambulatory Surgery (NSAS) since 1980 are listed on the Centers for Disease Control and Prevention web site [66].
Data collected for each year between 1990 and 2004 were obtained, read into a software program (SAS version 8.2; SAS Institute, Cary, NC), and analyzed. Discharges with a procedure code (ICD-9-CM) for primary or revision TKA (81.54, 81.55) were identified and included in the sample. Three procedure type groups were subsequently created: BTKA, UTKA, and RTKA. Patients who had UTKA were identified by the occurrence of the procedure code 81.54 once; those with BTKA had this procedure code listed twice. We identified 4,159,661 hospital discharges after TKA between years 1990 and 2004. Of those, 88.3% were UTKA, 3.7% BTKA, and 8% RTKA (Table 1).
Table 1.
Characteristics of patients discharged after different types of TKA
| Variable | BTKA | UTKA | RTKA | |||
|---|---|---|---|---|---|---|
| Number | Percent | Number | Percent | Number | Percent | |
| Number (percent of total) | 153,259 | 3.68 | 3,672,247 | 88.28 | 334,155 | 8.03 |
| Age in years (range)* (U and B and B and R only) | 66.6 (20–93) | 68.3 (3–99) | 68.4 (8–95) | |||
| Age group‡ | ||||||
| Younger than 45† | 1850 | 1.2 | 78,137 | 2.1 | 15,375 | 4.6 |
| 46–64† | 59,764 | 39 | 1,076,627 | 29.3 | 93,258 | 27.9 |
| 65–79† | 88,286 | 57.6 | 2,396,556 | 65.3 | 210,130 | 62.9 |
| 85+† | 3359 | 2.2 | 120,927 | 3.3 | 15,392 | 4.6 |
| Gender‡ | ||||||
| Male† | 63,078 | 41.2 | 1,328,856 | 36.2 | 140,776 | 42.1 |
| Female† | 90,181 | 58.8 | 2,343,391 | 63.8 | 193,379 | 57.9 |
| Race‡ | ||||||
| White† | 93,709 | 61.1 | 2,542,671 | 69.2 | 236,236 | 70.7 |
| Black† | 5553 | 3.6 | 177,894 | 4.8 | 18,890 | 5.7 |
| Other† | 2506 | 1.6 | 63,858 | 1.7 | 8870 | 2.7 |
| Not stated | 51,491 | 33.6 | 887,824 | 24.2 | 70,159 | 21 |
| Discharge status‡ | ||||||
| Routine discharge home† | 44,482 | 29 | 1,900,157 | 51.7 | 184,924 | 55.3 |
| Discharge to short-term facility† | 4842 | 3.2 | 342,989 | 9.3 | 27,399 | 8.2 |
| Discharge to long-term facility† | 56,954 | 37.2 | 720,712 | 19.6 | 57,738 | 17.3 |
| Alive, disposition not stated† | 36,779 | 24 | 625,688 | 17 | 55,125 | 16.5 |
| Dead† | 727 | 0.5 | 10,540 | 0.3 | 560 | 0.2 |
| Not stated or reported† | 9475 | 6.18 | 70,610 | 1.92 | 8409 | 2.52 |
| Bed size‡ | ||||||
| 6–99† | 28,147 | 18.4 | 766,745 | 20.9 | 60,589 | 18.1 |
| 100–199† | 32,503 | 21.2 | 1,022,898 | 27.9 | 87,410 | 26.2 |
| 200–299† | 39,884 | 26 | 777,853 | 21.2 | 73,550 | 22 |
| 300–499† | 38,768 | 25.3 | 804,740 | 21.9 | 78,599 | 23.5 |
| 500+† | 13,957 | 9.1 | 300,011 | 8.2 | 34,007 | 10.2 |
| Region‡ | ||||||
| Northeast† | 39,009 | 25.5 | 723,942 | 19.7 | 71,142 | 21.3 |
| Midwest†(U and B and B and R only) | 76,091 | 49.7 | 1,019,163 | 27.8 | 92,520 | 27.7 |
| Southern† | 27,118 | 17.7 | 1,283,728 | 35 | 111,132 | 33.3 |
| Western† | 11,041 | 7.2 | 645,414 | 17.6 | 59,361 | 17.8 |
| Insurance‡ | ||||||
| Medicare† | 75,726 | 49.4 | 2,044,410 | 55.7 | 179,863 | 53.8 |
| Medicaid† | 1920 | 1.3 | 114,601 | 3.1 | 14,279 | 4.3 |
| Private† | 52,586 | 34.3 | 1,007,580 | 27.4 | 89,028 | 26.6 |
| Other† | 22,423 | 14.6 | 458,274 | 12.5 | 46,546 | 13.9 |
| Not stated† (U and B and B and R only) | 604 | 0.4 | 47,382 | 1.3 | 4439 | 1.3 |
| Length of care in days (range)* (U and B only) | 5.8 (1–53) | 5.3 (1–101) | 5.4 (1–187) | |||
*p < 0.001 by general linear model between all groups or as indicated in parentheses; †p < 0.001 by z-scores between all groups or as indicated in parentheses; ‡p < 0.001 by chi square test between all groups or as indicated in parentheses; B = primary bilateral; U = primary unilateral; R = revision.
We determined the prevalence of procedure subtypes and respective demographics (age, gender, race, disposition status, primary source of payment, distribution of procedures by hospital size and US region, length of hospitalization). Frequencies of procedure-related complications were analyzed by determining cases that listed ICD-9-CM diagnosis codes specifying complications of surgical and medical care (ICD-9-CM 996.X to 999.X). For RTKA, device-related complications (996.X) most likely represented the primary preoperative indication for surgery and thus this diagnosis code was excluded from our analysis. In addition, we studied the prevalence of selected adverse diagnosis, including pulmonary embolism, thrombotic events, respiratory insufficiency after trauma or surgery/acute respiratory distress syndrome, acute posthemorrhagic anemia, and confusion, using appropriate ICD-9-CM diagnosis codes. Comorbidity profiles were analyzed by determining the prevalence of hypertension, hypercholesteremia, diabetes mellitus, obesity, pulmonary disease, and coronary artery disease. (See Appendix 2 for ICD-9-CM diagnosis codes used to determine the presence of comorbidities and adverse diagnoses.) Differences in in-hospital mortality between procedure subtypes were also assessed. Subsequently, multivariate regression analysis was performed and odds ratios and 95% confidence intervals were calculated to determine if type of surgery, age, and gender were independent predictors for in-hospital mortality and the occurrence of procedure-related complications.
Differences among procedure types were assessed first using chi square tests and then using z-scores for categorical variables where appropriate. We evaluated the importance of differences between procedure types for continuous variables using a general linear model (Scheffe's Test). We presumed a p value of 0.001 was clinically important.
To study the independent risk factors for complications after knee arthroplasty, we performed multivariate logistic regression analysis. The variables included in the model were procedure type, age, gender, race, hospital bed size, US region, source of payment, and comorbidities. The analysis was repeated for dependent variables to include the occurrence of any procedure-related complication, pulmonary and cardiac in particular, pulmonary embolism, and in-hospital mortality. All analysis was performed using SAS version 8.2 (SAS Institute).
Results
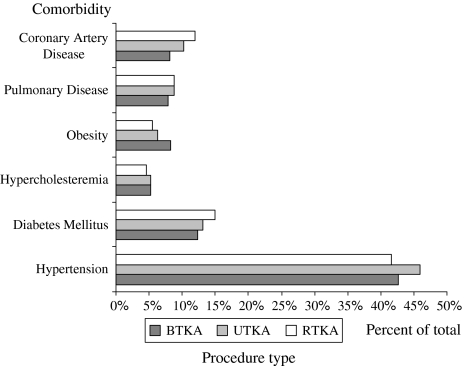
We identified an estimate of 153,259 discharges after BTKA. The average age of the patients at the time of surgery was 66.6 years with 40.2% aged younger than 65 years (Table 1). A total of 58.8% of patients were female. Further patient- and healthcare-system-related characteristics are detailed (Table 1). The most prevalent comorbidities among patients undergoing BTKA were hypertension (42.6%), diabetes mellitus (12.4%), and obesity (8.3%) (Fig. 1). The mean length of hospital stay was 5.8 days. Procedure-related complications occurred in 12.2%. Among the most frequently reported were hematoma formation (2.5%) and organ-specific complications, including cardiac (1.9%), respiratory (1.9%), gastrointestinal (1.4%), and genitourinary (1.4%) (Table 2). In-hospital death occurred in 0.5% of patients undergoing BTKA.
Fig. 1.
The figure shows the prevalence of comorbidities among patients undergoing different types of TKA procedures. The p value is less than 0.001 among all procedure types for all comorbidity groups (z-scores), except pulmonary (UTKA and BTKA and BTKA and RTKA only) and hypercholesteremia (UTKA and RTKA and BTKA and RTKA only). UTKA = unilateral TKA; BTKA = bilateral TKA; RTKA = revision TKA.
Table 2.
Procedure-related complications (ICD-9 997–999) among patients undergoing TKA
| Complications | BTKA | UTKA | RTKA | |||
|---|---|---|---|---|---|---|
| Number | Percent | Number | Percent | Number | Percent | |
| Complications affecting specific body systems (ICD-9 997) | ||||||
| CNS* | 355 | 0.2 | 5373 | 0.2 | 308 | 0.1 |
| Cardiac* | 2965 | 1.9 | 40,308 | 1.1 | 3141 | 0.9 |
| Peripheral vascular* | 1090 | 0.7 | 13,471 | 0.4 | 1959 | 0.6 |
| Respiratory* | 2869 | 1.9 | 41,710 | 1.1 | 4393 | 1.3 |
| GI* | 2188 | 1.4 | 36,291 | 1 | 1845 | 0.6 |
| GU* | 2170 | 1.4 | 35,153 | 1 | 3020 | 1 |
| Other (organ-specific)* | 500 | 0.3 | 8342 | 0.2 | 175 | 0.1 |
| Other complications of procedure (ICD-9 998) | ||||||
| Postoperative shock* | 76 | 0.1 | 520 | 0.01 | 81 | 0.02 |
| Hematoma or seroma* | 3785 | 2.5 | 39,863 | 1.1 | 6538 | 2 |
| Accidental puncture/laceration* | 210 | 0.1 | 1702 | 0.1 | 24 | 0.01 |
| Disruption operative wound* | 128 | 0.1 | 1294 | 0.1 | 854 | 0.3 |
| Postoperative infection* | 205 | 0.1 | 7934 | 0.2 | 2214 | 0.7 |
| Other* | 4499 | 2.9 | 93,512 | 2.6 | 7443 | 2.2 |
| Complications of medical care (ICD-9 999) | ||||||
| Complications of medical care* | 674 | 0.4 | 5622 | 0.2 | 948 | 0.7 |
| Patients with any procedure-related complication (ICD-9 997–999) | ||||||
| Any procedure-related complication* | 18,696 | 12.2 | 299,526 | 8.5 | 29,007 | 8.7 |
*p < 0.001 by z-scores between all groups within comorbidity or as indicated in parentheses; ICD-9 = International Classification of Diseases, 9th Revision; B = primary bilateral; U = primary unilateral; R = revision; CNS = central nervous system; GI = gastrointestinal; GU = genitourinary.
Patients undergoing BTKA were younger and had a more favorable comorbidity profile than those undergoing UTKA and RTKA. Patients undergoing BTKA were on average 1.5 years younger than those undergoing UTKA (68.3 years) and RTKA (68 years). The number of patients younger than 65 years of age at the time of surgery was higher in the BTKA group (40.2%), than in the UTKA (31.4%) and RTKA (32.5%) groups (Table 1). All three TKA procedures were more prevalent among female patients. However, for BTKA and RTKA, the gap between genders was smaller when compared with UTKA (Table 1). Hypertension was the most prevalent comorbidity for all three procedure types, affecting 42.6% of patients undergoing BTKA, 45.9% of UTKA, and 41.6% of RTKA, respectively (Fig. 1). Patients undergoing BTKA had a lower prevalence of hypertension, diabetes mellitus, hypercholesteremia, and pulmonary and coronary artery disease than those undergoing UTKA; and lower prevalence of diabetes mellitus, and pulmonary artery disease, and coronary artery disease than those undergoing RTKA. The only comorbidity for which patients undergoing BTKA had the highest prevalence among procedure types was obesity (8.3% versus 6.3% for UTKA; 5.6% for RTKA). The length of hospital stay was longest for BTKA (average, 5.8 days; range, 1–101 days). Patients were hospitalized an average of 5.3 days (range, 1–53 days) after UTKR; and 5.4 days (range, 1–187 days) after RTKA (Table 1).
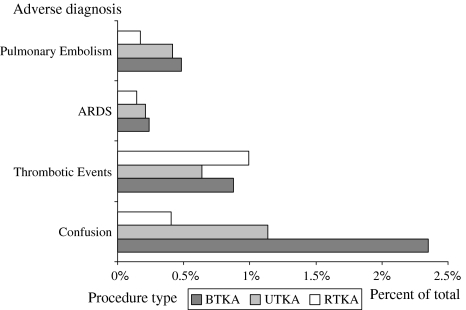
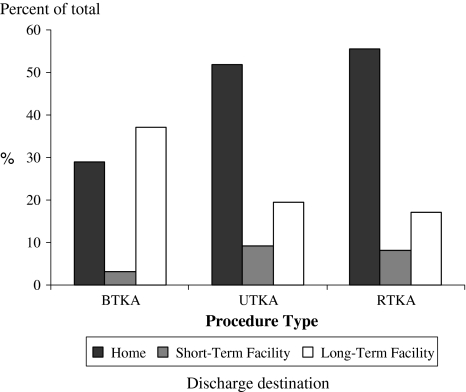
Procedure-related complications were approximately 50% more frequent among patients after BTKA (12.2%) than after UTKA (8.2%) and RTKA (8.7%) (Table 2). The incidence of pulmonary embolism, confusion, and thrombotic events was higher for BTKA when compared with UTKA. The incidence of these events (except for thrombotic events) was lowest among RTKA patients (Fig. 2). The incidence of posthemorrhagic anemia was 28.6% for BTKA, 15.3% for UTKA, and 13.1% for RTKA. In-hospital mortality rates were highest for BTKA (0.5%) followed by UTKA (0.3%) and RTKA (0.2%) (Table 1). The proportion of patients whose disposition was to a long-term care facility after BTKA (37.2%) was approximately double that of the other two procedures studied (UTKA 19.6%; RTKA 17.3%) (Fig. 3).
Fig. 2.
The figure shows the prevalence of selected adverse diagnoses among patients undergoing different types of TKA. ARDS = pulmonary insufficiency after trauma or surgery/ARDS. The p value is less than 0.001 between all procedure types for all adverse event groups (z-scores), except for ARDS (UTKA and RTKA and BTKA and RTKA only). UTKA = unilateral TKA; RTKA = revision TKA; BTKA = bilateral TKA.
Fig. 3.
The figure shows the discharge destination after different TKA procedures. The p value is less than 0.001 among all procedure types (chi square) and among discharge destination groups (z-scores). UTKA = unilateral TKA; BTKA = bilateral TKA; RTKA = revision TKA.
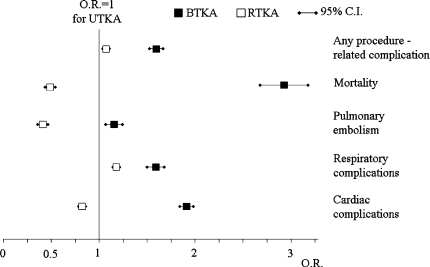
BTKA and increasing age were independent risk factors for procedure-related complications in general, and cardiac and respiratory complications in particular, when compared with UTKA. We found the same for in-hospital mortality and pulmonary embolism (Table 3) (Fig. 4). RTKA was associated with increased risk for the development of procedure-related complications and respiratory complications when compared with UTKA (Fig. 4). Male gender was also associated with an increased risk for adverse outcomes, except for pulmonary embolism (Table 3).
Table 3.
Evaluation of type of procedure, age, and gender as independent risk factors for adverse outcomes after TKA (expressed as odds ratios [95% confidence intervals])
| Variable | Risk factor | Any procedure-related complication | Mortality | Pulmonary embolism | Respiratory complications | Cardiac complications |
|---|---|---|---|---|---|---|
| Procedure type (referent: UTKA) | RTKA | 1.044 (1.031–1.057) | 0.482 (0.441–0.526) | 0.419 (0.385–0.455) | 1.180 (1.143–1.218) | 0.810 (0.781–0.840) |
| BTKA | 1.562 (1.537–1.587) | 2.884 (2.668;3.118) | 1.169 (1.084;1.260) | 1.611(1.550–1.675) | 1.883 (1.812–1.957) | |
| Age group (referent: 45–64 years) | Younger than 45 | 0.842 (0.820–0.866) | 1.004 (0.739–1.364) | 0.639 (0.562–0.727) | 0.271 (0.242–0.303) | 0.860 (0.788–0.938) |
| 65–84 | 1.262 (1.249–1.275) | 5.173 (4.737–5.649) | 0.875 (0.836–0.915) | 1.152 (1.122–1.183) | 1.590 (1.542–1.639) | |
| Older than 85 | 1.303 (1.276–1.330) | 22.202 (20.095–24.529) | 1.431 (1.321–1.550) | 1.470 (1.400–1.544) | 3.751 (3.595–3.914) | |
| Gender (referent: female) | Male | 1.375 (1.366;1.385) | 1.105 (1.064–1.148) | 0.718 (0.693–0.743) | 1.095 (1.075–1.116) | 1.171 (1.149–1.193) |
Odds ratios whose confidence intervals do not overlap with 1 represent a significantly different value when compared with UTKA; U = unilateral; R = revision; B = bilateral.
Fig. 4.
The figure shows the odds ratios (ORs) and 95% confidence intervals (95% CIs) for in-hospital mortality and selected medical complications in patients undergoing BTKA and RTKA. (Referent is UTKA; OR, 1.) All ORs are different from UTKA = 1. BTKA = bilateral TKA; RTKA = revision TKA; UTKA = unilateral TKA.
Discussion
In this study, we aimed to determine nationally representative patient- and healthcare-system-related characteristics, the prevalence of procedure-related complications, and in-hospital mortality associated with BTKA surgery. Furthermore, we compared these results with data of patients undergoing UTKA and those undergoing RTKA. We further assessed the independent role of the surgical procedure on postoperative outcomes by performing a multivariate regression analysis, thus controlling for a variety of relevant patient- and hospitalization-related variables captured in the survey. We identified BTKA to be a procedure with an increased risk of perioperative complications and mortality.
Our study is limited by a number of factors inherent to secondary data analysis of large administrative databases. As such, clinical information available in the NHDS is limited and our analysis must be interpreted in this context. Because of the nature of the NHDS, only in-patient data are available and thus complications and events after discharge are not captured. Furthermore, readmissions cannot be discerned from this database. Thus, conclusions should be limited to the acute postoperative setting with the notion that mortality and complications are likely underestimated. An additional limiting factor is the bias associated with the retrospective nature of our study. Nevertheless, because of the availability of data from a large, nationally representative sample, this type of analysis may provide a more accurate estimate of events surrounding TKA than various prospective studies that are limited in sample size and thus lack the ability to capture low-incidence outcomes. The use of ICD-9 coding poses some limitations. Although we identified patients undergoing BTKA by the occurrence of the code for UTKA twice, it is not possible to distinguish patients who had BTKA performed during the same session from those who underwent surgery at different times during their hospitalization [17, 62]. Furthermore, ICD-9 code 81.54 includes unicompartimental knee arthroplasty, which was not frequently performed during the study period in the United States. ICD-9 code 81.55 (revision knee arthroplasty) does not discriminate complex revisions from straightforward ones like the exchange of a polyethylene insert. Other authors have reported these problems when analyzing data from Medicare enrollees [4]. Although differences in outcomes between these different approaches may exist [43, 53, 60, 64, 69, 73], our data more likely provide an overview of actual practice. Moreover, the average length of hospitalization for patients undergoing BTKA in our analysis (5.8 days) was only a half day longer than that of patients undergoing UTKA (5.3 days), indicating probably in most of the admissions, BTKA was performed under the same anesthetic. Finally, despite rigorous quality assurance measures applied in the operation of the NHDS, undercoding of diagnosis, particularly of chronic conditions, is likely to influence analysis of comorbidities as risk factors. This problem has been described in the past [6, 30]. Iezzoni et al. [30] suggested many comorbidities that, on a clinical basis, should be associated with increased risk of adverse outcomes were erroneously linked with a lower risk of in-hospital death. Although undercoding should affect the reported prevalence of comorbidities for each procedure type equally and thus allow for comparative data analysis, attempting to identify certain comorbidities as risk factors, especially when low-incidence outcomes are analyzed, may yield misleading results and thus was not attempted in this study. However, the fact that both the exclusion and inclusion of comorbidities in the regression analysis had a negligible influence on results suggests these variables have little influence on the determination of other risk factors such as age and gender. We believe taking into consideration the previously mentioned limitations, our analysis is valid and clinically relevant.
We described the demographic, comorbidity profile, and healthcare system-related variables in patients undergoing BTKA, UTKA, and RTKA. The proportion of arthroplasties being performed in women was higher for all procedure types. Research suggests osteoarthritis is both more prevalent and incapacitating in females than males, which may explain discrepancies in use found between genders [23]. There was a higher proportion of male patients undergoing BTKA and RTKA in comparison to those undergoing UTKA. This observation has been previously made [28], including the Medicare population [4]. These findings should be assessed critically, because we identified male gender as an independent risk factor for procedure-related complications. Male gender has been linked to increased risk for mortality after simultaneous BTKA and TKA in general in the past [55, 63, 64].
We found a lower prevalence of comorbid diseases among patients undergoing BTKA, except for obesity. Obesity has been suggested as a cause of premature knee osteoarthritis [20, 75]. This may explain our and other authors’ observations of a higher prevalence of this comorbidity among patients undergoing BTKA [21, 75]. Of note should be the obese patient population may be at increased risk for adverse outcomes [3, 15, 16].
Increased comorbid burden such as preexisting cardiopulmonary disease and diabetes has been associated with worse outcome after TKA [50, 55]; hence, it is expected more invasive procedures such as BTKA, associated with increased risk of adverse perioperative events, are performed on healthier patients with less comorbid disease.
We and others [8] observed a similar length of hospital stay for all studied TKA procedures. However, a larger proportion of patients after BTKA were transferred to long-term care facilities as compared with UTKA and RTKA (37.2% versus 19.6% versus 17.3%, respectively). This observation most likely reflects the increased need for acute rehabilitation after BTKA [40, 45]. Thus, the apparent similar length of hospital stay of patients undergoing BTKA may represent a shift of care to rehabilitation centers, which are less costly than hospitals [24, 25]. It is of concern that this reduction in hospitalization time may shift the monitoring period for serious complications to an out-of-hospital environment. However, Parvizi et al. recently noted 90% of life-threatening complications after lower extremity total joint arthroplasty occurs within 4 days of surgery [54]. In the previously discussed study by Gandhi et al., 91% of patients developing a myocardial infarction after total joint arthroplasty did so in the first five postoperative days [18], which encompasses the mean hospital stay we found.
When compared with UTKA, a higher proportion of RTKAs and BTKAs were performed in hospitals with bed sizes over 200. This observation was most noticeable for BTKAs and has been observed in a previously discussed study of Medicare patients [4]. This finding may reflect the fact that larger hospitals may be better equipped to take care of presumably more complex procedures such as RTKA and BTKA. An association between higher hospital procedure volume and better outcomes after TKA has been described in the past [32, 71]. However, the relationship between outcomes and hospital size remains unstudied and requires further evaluation.
We identified BTKA as an independent risk factor for complications and mortality when compared with UTKA and RTKA (Fig. 4). This observation was made despite the presence of a more favorable comorbidity profile and lower average age in the BTKA group (Fig. 1). BTKA was associated with an approximately 50% higher overall procedure-related complication rate. The occurrence of most adverse events studied, including pulmonary embolism and confusion, was higher in the BTKA group, which is in concordance with reports in the literature. Studying Medicare participants, Barrett et al. reported the adjusted risk of pulmonary embolism was 80% higher after BTKA than UTKA (adjusted hazard ratio, 1.81) [4]. Restrepo et al. reported an increased risk of pulmonary embolism (odds ratio, 1.8) and cardiac complications (odds ratio, 2.49) after simultaneous compared with staged BTKA [60]. Gandhi et al. [18] analyzed the rate and timing of myocardial infarction among 3471 patients undergoing total joint arthroplasty at a single institution. In a multivariate analysis, increased body mass index and age, bilateral surgery, diabetes, and American Society of Anesthesiologists Class 3 were associated with increased risk of myocardial infarction [18]. Lane et al. reported postoperative confusion was four times more prevalent after BTKA (29%) than after UTKA (7%) [40]. The rate of posthemorrhagic anemia was 28.6% of all patients undergoing BTKA, approximately double that of unilateral procedures. An increase in the blood transfusions after BTKA versus UTKA has been reported in the literature [7, 44]. Lane et al. suggested the risk of having banked blood after bilateral procedures was 17 times increased, thus causing concern in the setting of transfusion-related complications, including transmission of disease [40].
We observed procedure-related infections and wound dehiscence were higher in the RTKA group. RTKA has been associated with increased infection rates compared with UTKA in the past [46]. Despite the higher rate of obesity in patients undergoing BTKA, those undergoing UTKA had higher rate of procedure-related infection. This may be explained by the fact that the latter group had an increased prevalence of other comorbidities, some that are linked to an increased risk of infection, ie, diabetes [50]. Huotari et al. reported BTKAs were not associated with increased risk of infection when compared with UTKAs [28].
The reasons for the difference in outcome profiles are poorly understood, but the exposure of organ systems to the various loads of microemboli during the implantation process and the ensuing inflammatory response may explain the differences in the observed incidence of a number of complications [33, 34, 39]. The fact that the procedure code for RTKA for a complete knee revision and isolated revisions of a polyethylene insert or a patella component [22] are the same under the current procedure coding system may explain the overall low prevalence of adverse events and procedure-related complications seen in the RTKA group.
We found an almost threefold increase in the risk of in-hospital mortality among patients undergoing BTKA and a reduced risk for patients undergoing RTKA when using UTKA as a referent. In the setting of similar length of hospitalization, differences in the capture timeframe can largely be excluded as a source of bias. Our findings are in agreement with existing data. Parvizi et al. identified risk factors for 30-day mortality to include simultaneous BTKA as compared with unilateral procedures and, interestingly, primary TKA as compared with RTKA [55]. In their recent meta-analysis, Restrepo et al. reported simultaneous BTKAs were associated with increased risk for mortality (odds ratio, 1.8) when compared with staged procedures [60]. In an analysis of the published data up to 2004, Oakes and Hanssen reported the early mortality rate of simultaneous BTKA (1%) was almost three times higher than that of staged BTKA (0.4%) [53]. Finally, Mangaleshkar et al. retrospectively reviewed the early complications of a consecutive series of 54 patients with simultaneous BTKA, 34 patients with staged BTKA, and 367 with UTKA. Four patients of the first group died in the early postoperative period. No deaths were observed in the other two groups [47].
We found advanced age was an independent risk factor for increased early complications and mortality after TKA surgery, thus confirming the observation of other authors [1, 6, 44, 55, 63, 70]. Patients between the ages of 65 and 84 years had a fivefold higher chance and those over 85 years a 22-fold higher chance of mortality after TKA than those aged 45 to 64 years. This observation is further supported by Parvizi et al. who, among other factors, identified advanced age (older than 70) to be associated with increased mortality [55]. Similarly, Mantilla et al. reported the rate of adverse events after lower extremity arthroplasty increases with advanced age, especially for patients aged 70 years or older [48]. Our observation that patients undergoing BTKA were younger than those undergoing UTKA and RTKA has also been made by others [28] and may, at least in part, reflect the clinician’s concern to perform this more invasive procedure in a younger and thus presumably healthier population.
Among 4,159,661 hospital discharges, we identified substantial differences in patient and hospital demographics and outcomes among BTKA, UTKA, and RTKA. In the setting of similar hospital stay, we found a higher in-hospital mortality and procedure-related complication rate among patients after BTKA when compared with UTKA and BTKA. These observations were made despite a more favorable comorbidity profile and younger age among patients undergoing BTKA. Furthermore, BTKA was identified as an independent risk factor for in-hospital mortality and procedure-related complications when compared with UTKA and RTKA. Taking the discussed limitations into account, our data can be used to inform and provide nationally representative data to physicians, administrators, researchers, policymakers, and patients on demographics and outcomes of various types of knee arthroplasties. Future efforts should concentrate on studying patient- and healthcare-related risk factors associated with complications and mortality after BTKA to diminish the perioperative risks.
Appendix
Appendix 1.
Information available in the National Hospital Discharge Survey
| Survey year |
| Newborn status |
| Age |
| Gender |
| Race |
| Marital status |
| Discharge month |
| Discharge status |
| Days of care |
| Length of stay |
| Geographic region |
| Number of hospital beds |
| Hospital ownership |
| Analysis weight |
| Diagnoses (up to seven possible) |
| Procedures (up to four possible) |
| Principal and secondary source of payment |
| Type of admission |
| Source of admission |
Appendix
Appendix 2.
List of ICD-9 diagnosis codes included to identify comorbidities, adverse diagnoses, and complications among discharges*
| Comorbidities | |
| Hypertension | 401, 402, 403, 404, 405 |
| Diabetes mellitus | 250 |
| Hypercholesteremia | 2720 |
| Obesity | 278 |
| Pulmonary disease | 490, 491, 492, 493, 494, 496 |
| Renal disease | 582, 585, 403 |
| Coronary artery disease | 412, 413, 414, 4292 |
| Procedure-related complications | |
| Central nervous system | 9970 |
| Cardiac | 9971 |
| Peripheral vascular | 9972 |
| Respiratory | 9973 |
| Gastrointestinal | 9974 |
| Genitourinary | 9975 |
| Other organ-specific | 9976–9979 |
| Postoperative shock | 9980 |
| Hematoma or seroma | 9981 |
| Accidental puncture or laceration | 9982 |
| Disruption operative wound | 9983 |
| Postoperative infection | 9985 |
| Other complications of procedure | 9986–9989 |
| Complications of medical care | 999 |
| Other adverse events | |
| Acute posthemorrhagic anemia | 2851 |
| Pulmonary embolism | 4151 |
| Psychosis | 291, 292, 293 |
| Pulmonary insufficiency after trauma and surgery or acute respiratory distress syndrome | 5185 |
| Thromboembolic events | 4511, 4512, 4518, 4519, 4532, 4538, 4539 |
*Four- and five-digit codes are included under the respective three- and four-digit codes; ICD-9 = International Classification of Diseases, 9th Revision.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article. This study was partially funded by a Young Investigator Award of the Department of Anesthesia at Hospital for Special Surgery.
References
- 1.Adili A, Bhandari M, Petruccelli D, De Beer J. Sequential bilateral total knee arthroplasty under 1 anesthetic in patients > or = 75 years old: complications and functional outcomes. J Arthroplasty. 2001;16:271–278. [DOI] [PubMed]
- 2.Alemparte J, Johnson GV, Worland RL, Jessup DE, Keenan J. Results of simultaneous bilateral total knee replacement: a study of 1208 knees in 604 patients. J South Orthop Assoc. 2002;11:153–156. [PubMed]
- 3.Amin AK, Clayton RA, Patton JT, Gaston M, Cook RE, Brenkel IJ. Total knee replacement in morbidly obese patients. Results of a prospective, matched study. J Bone Joint Surg Br. 2006;88:1321–1326. [DOI] [PubMed]
- 4.Barrett J, Baron JA, Losina E, Wright J, Mahomed NN, Katz JN. Bilateral total knee replacement: staging and pulmonary embolism. J Bone Joint Surg Am. 2006;88:2146–2151. [DOI] [PubMed]
- 5.Besser MI. Bilateral Attenborough total knee replacement as a single procedure. Arch Orthop Trauma Surg. 1983;101:271–272. [DOI] [PubMed]
- 6.Bhattacharyya T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am. 2002;84:562–572. [DOI] [PubMed]
- 7.Bottner F, Pavone V, Johnson T, Heitkemper S, Sculco TP. Blood management after bilateral total knee arthroplasty. Clin Orthop Relat Res. 2003;410:254–261. [DOI] [PubMed]
- 8.Bozic KJ, Durbhakula S, Berry DJ, Naessens JM, Rappaport K, Cisternas M, Saleh KJ, Rubash HE. Differences in patient and procedure characteristics and hospital resource use in primary and revision total joint arthroplasty: a multicenter study. J Arthroplasty. 2005;20:17–25. [DOI] [PubMed]
- 9.Brotherton SL, Roberson JR, de Andrade JR, Fleming LL. Staged versus simultaneous bilateral total knee replacement. J Arthroplasty. 1986;1:221–228. [DOI] [PubMed]
- 10.Bullock DP, Sporer SM, Shirreffs TG Jr. Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am. 2003;85:1981–1986. [DOI] [PubMed]
- 11.Dennis DA. Debate: bilateral simultaneous total knee arthroplasty. Clin Orthop Relat Res. 2004;428:82–83. [DOI] [PubMed]
- 12.Dennison C, Pokras R. Design, operation of the National Hospital Discharge Survey: 1988 redesign. In: Vital and Health Statistics. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2000;39:1–42. [PubMed]
- 13.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D. Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79:575–582. [DOI] [PubMed]
- 14.Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86. [DOI] [PubMed]
- 15.Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am. 2004;86:1609–1615. [DOI] [PubMed]
- 16.Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004;19:817–824. [DOI] [PubMed]
- 17.Forster MC, Bauze AJ, Bailie AG, Falworth MS, Oakeshott RD. A retrospective comparative study of bilateral total knee replacement staged at a one-week interval. J Bone Joint Surg Br. 2006;88:1006–1010. [DOI] [PubMed]
- 18.Gandhi R, Petruccelli D, Devereaux PJ, Adili A, Hubmann M, de Beer J. Incidence and timing of myocardial infarction after total joint arthroplasty. J Arthroplasty. 2006;21:874–877. [DOI] [PubMed]
- 19.Gill GS, Mills D, Joshi AB. Mortality following primary total knee arthroplasty. J Bone Joint Surg Am. 2003;85:432–435. [DOI] [PubMed]
- 20.Gillespie GN, Porteous AJ. Obesity and knee arthroplasty. Knee. 2007;14:81–86. [DOI] [PubMed]
- 21.Griffin FM, Scuderi GR, Insall JN, Colizza W. Total knee arthroplasty in patients who were obese with 10 years followup. Clin Orthop Relat Res. 1998;356:28–33. [DOI] [PubMed]
- 22.Hanssen AD, Pagnano MW. Revision of failed patellar components. Instr Course Lect. 2004;53:201–206. [PubMed]
- 23.Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R, Badley EM. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1016–1022. [DOI] [PubMed]
- 24.Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am. 2002;84:348–353. [DOI] [PubMed]
- 25.Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29:377–388. [DOI] [PubMed]
- 26.Hersekli MA, Akpinar S, Ozalay M, Ozkoc G, Uysal M, Cesur N, Tandogan RN. A comparison between single- and two-staged bilateral total knee arthroplasty operations in terms of the amount of blood loss and transfusion, perioperative complications, hospital stay, and cost-effectiveness. Acta Orthop Traumatol Turc. 2004;38:241–246. [PubMed]
- 27.Horne G, Devane P, Adams K. Complications and outcomes of single-stage bilateral total knee arthroplasty. ANZ J Surg. 2005;75:734–738. [DOI] [PubMed]
- 28.Huotari K, Lyytikainen O, Seitsalo S. Patient outcomes after simultaneous bilateral total hip and knee joint replacements. J Hosp Infect. 2007;65:219–225. [DOI] [PubMed]
- 29.Hutchinson JR, Parish EN, Cross MJ. A comparison of bilateral uncemented total knee arthroplasty: simultaneous or staged? J Bone Joint Surg Br. 2006;88:40–43. [DOI] [PubMed]
- 30.Iezzoni LI, Foley SM, Daley J, Hughes J, Fisher ES, Heeren T. Comorbidities, complications, and coding bias. Does the number of diagnosis codes matter in predicting in-hospital mortality? JAMA. 1992;267:2197–2203. [DOI] [PubMed]
- 31.Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R, Katz JN. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005;52:3928–3933. [DOI] [PubMed]
- 32.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909–1916. [DOI] [PubMed]
- 33.Kim YH. Incidence of fat embolism syndrome after cemented or cementless bilateral simultaneous and unilateral total knee arthroplasty. J Arthroplasty. 2001;16:730–739. [DOI] [PubMed]
- 34.Kim YH, Oh SW, Kim JS. Prevalence of fat embolism following bilateral simultaneous and unilateral total hip arthroplasty performed with or without cement: a prospective, randomized clinical study. J Bone Joint Surg Am. 2002;84:1372–1379. [DOI] [PubMed]
- 35.Kolettis GT, Wixson RL, Peruzzi WT, Blake MJ, Wardell S, Stulberg SD. Safety of 1-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;309:102–109. [PubMed]
- 36.Kovacik MW, Singri P, Khanna S, Gradisar IA. Medical and financial aspects of same-day bilateral total knee arthroplasties. Biomed Sci Instrum. 1997;33:429–434. [PubMed]
- 37.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. [DOI] [PubMed]
- 38.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. [DOI] [PubMed]
- 39.Lachiewicz PF, Ranawat CS. Fat embolism syndrome following bilateral total knee replacement with total condylar prosthesis: report of two cases. Clin Orthop Relat Res. 1981;160:106–108. [PubMed]
- 40.Lane GJ, Hozack WJ, Shah S, Rothman RH, Booth RE Jr, Eng K, Smith P. Simultaneous bilateral versus unilateral total knee arthroplasty. Outcomes analysis. Clin Orthop Relat Res. 1997;345:106–112. [DOI] [PubMed]
- 41.Leitch KK, Dalgorf D, Borkhoff CM, Kreder HJ. Bilateral total knee arthroplasty–staged or simultaneous? Ontario’s orthopedic surgeons reply. Can J Surg. 2005;48:273–276. [PMC free article] [PubMed]
- 42.Leonard L, Williamson DM, Ivory JP, Jennison C. An evaluation of the safety and efficacy of simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2003;18:972–978. [DOI] [PubMed]
- 43.Liu TK, Chen SH. Simultaneous bilateral total knee arthroplasty in a single procedure. Int Orthop. 1998;22:390–393. [DOI] [PMC free article] [PubMed]
- 44.Lombardi AV, Mallory TH, Fada RA, Hartman JF, Capps SG, Kefauver CA, Dodds K, Adams JB. Simultaneous bilateral total knee arthroplasties: who decides? Clin Orthop Relat Res. 2001;392:319–329. [DOI] [PubMed]
- 45.Macario A, Schilling P, Rubio R, Goodman S. Economics of one-stage versus two-stage bilateral total knee arthroplasties. Clin Orthop Relat Res. 2003;414:149–156. [DOI] [PubMed]
- 46.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87:1222–1228. [DOI] [PubMed]
- 47.Mangaleshkar SR, Prasad PS, Chugh S, Thomas AP. Staged bilateral total knee replacement–a safer approach in older patients. Knee. 2001;8:207–211. [DOI] [PubMed]
- 48.Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology. 2002;96:1140–1146. [DOI] [PubMed]
- 49.March LM, Cross M, Tribe KL, Lapsley HM, Courtenay BG, Cross MJ, Brooks PM, Cass C, Coolican M, Neil M, Pinczewski L, Quain S, Robertson F, Ruff S, Walter W, Zicat B. Two knees or not two knees? Patient costs and outcomes following bilateral and unilateral total knee joint replacement surgery for OA. Osteoarthritis Cartilage. 2004;12:400–408. [DOI] [PubMed]
- 50.Meding JB, Reddleman K, Keating ME, Klay A, Ritter MA, Faris PM, Berend ME. Total knee replacement in patients with diabetes mellitus. Clin Orthop Relat Res. 2003;416:208–216. [DOI] [PubMed]
- 51.Morrey BF, Adams RA, Ilstrup DM, Bryan RS. Complications and mortality associated with bilateral or unilateral total knee arthroplasty. J Bone Joint Surg Am. 1987;69:484–488. [PubMed]
- 52.Nunley RM, Lachiewicz PF. Mortality after total hip and knee arthroplasty in a medium-volume university practice. J Arthroplasty. 2003;18:278–285. [DOI] [PubMed]
- 53.Oakes DA, Hanssen AD. Bilateral total knee replacement using the same anesthetic is not justified by assessment of the risks. Clin Orthop Relat Res. 2004;428:87–91. [DOI] [PubMed]
- 54.Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32. [DOI] [PubMed]
- 55.Parvizi J, Sullivan TA, Trousdale RT, Lewallen DG. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg Am. 2001;83:1157–1161. [DOI] [PubMed]
- 56.Pavone V, Johnson T, Saulog PS, Sculco TP, Bottner F. Perioperative morbidity in bilateral one-stage total knee replacements. Clin Orthop Relat Res. 2004;421:155–161. [DOI] [PubMed]
- 57.Powell RS, Pulido P, Tuason MS, Colwell CW Jr, Ezzet KA. Bilateral vs unilateral total knee arthroplasty: a patient-based comparison of pain levels and recovery of ambulatory skills. J Arthroplasty. 2006;21:642–649. [DOI] [PubMed]
- 58.Primary total hip and total knee arthroplasty projections to 2030. Bulletin of the American Academy of Orthopaedic Surgeons. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1998.
- 59.Radmer S, Andresen R, Sparmann M. Simultaneous bilateral total knee arthroplasty in patients with rheumatoid arthritis. Z Orthop Ihre Grenzgeb. 2006;144:472–476. [DOI] [PubMed]
- 60.Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2007;89:1220–1226. [DOI] [PubMed]
- 61.Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13:172–179. [DOI] [PubMed]
- 62.Ritter M, Mamlin LA, Melfi CA, Katz BP, Freund DA, Arthur DS. Outcome implications for the timing of bilateral total knee arthroplasties. Clin Orthop Relat Res. 1997;345:99–105. [DOI] [PubMed]
- 63.Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res. 2004;428:84–86. [DOI] [PubMed]
- 64.Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Joint Surg Am. 2003;85:1532–1537. [DOI] [PubMed]
- 65.Schafer M, Elke R, Young JR, Gancs P, Kindler CH. Safety of one-stage bilateral hip and knee arthroplasties under regional anaesthesia and routine anaesthetic monitoring. J Bone Joint Surg Br. 2005;87:1134–1139. [DOI] [PubMed]
- 66.Selected articles using National Hospital Discharge Survey or National Survey of Ambulatory Surgery data. Centers for Disease Control and Prevention. 2007. Available at: http://www.cdc.gov/nchs/data/hdasd/NHDS2007articleupdate.pdf. Accessed October 19, 2007.
- 67.Shah K, Smith J, Jones B, Hullin M. Bilateral total knee replacement under a single anaesthetic, using a cementless implant is not unsafe. Knee Surg Sports Traumatol Arthrosc. 2007;15:269–275. [DOI] [PubMed]
- 68.Sierra RJ, Cooney WP 4th, Pagnano MW, Trousdale RT, Rand JA. Reoperations after 3200 revision TKAs: rates, etiology, and lessons learned. Clin Orthop Relat Res. 2004;425:200–206. [DOI] [PubMed]
- 69.Sliva CD, Callaghan JJ, Goetz DD, Taylor SG. Staggered bilateral total knee arthroplasty performed four to seven days apart during a single hospitalization. J Bone Joint Surg Am. 2005;87:508–513. [DOI] [PubMed]
- 70.SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88:480–485. [DOI] [PubMed]
- 71.SooHoo NF, Zingmond DS, Lieberman JR, Ko CY. Primary total knee arthroplasty in California 1991 to 2001: does hospital volume affect outcomes? J Arthroplasty. 2006;21:199–205. [DOI] [PubMed]
- 72.Soudry M, Binazzi R, Insall JN, Nordstrom TJ, Pellicci PM, Goulet JA. Successive bilateral total knee replacement. J Bone Joint Surg Am. 1985;67:573–576. [PubMed]
- 73.Stanley D, Stockley I, Getty CJ. Simultaneous or staged bilateral total knee replacements in rheumatoid arthritis. A prospective study. J Bone Joint Surg Br. 1990;72:772–774. [DOI] [PubMed]
- 74.Stubbs G, Pryke SE, Tewari S, Rogers J, Crowe B, Bridgfoot L, Smith N. Safety and cost benefits of bilateral total knee replacement in an acute hospital. ANZ J Surg. 2005;75:739–746. [DOI] [PubMed]
- 75.Sturmer T, Gunther KP, Brenner H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol. 2000;53:307–313. [DOI] [PubMed]
- 76.Vessely M, Harmsen WS, Schleck C, Melton LJ, Kurland R, Berry D. James A. Rand Award Paper: a population based study of trends in use of total hip and knee arthroplasty. J Arthroplasty. 2007;22:303. [DOI]
- 77.Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat Award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006;452:28–34. [DOI] [PubMed]
- 78.Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade. Data from the Scottish Arthroplasty Project. Knee. 2006;13:102–105. [DOI] [PubMed]
- 79.Worland RL, Jessup DE, Clelland C. Simultaneous bilateral total knee replacement versus unilateral replacement. Am J Orthop. 1996;25:292–295. [PubMed]