Abstract
Polyethylene tibial post wear in posterior-stabilized knee designs is a major problem. The Insall-Burstein II (IB PS II) reportedly has severe anterior wear of the post in retrieved implants. We hypothesized the more anterior placement in the IB PS II would be reflected in greater wear at the anterior face than the IB PS I. We examined 234 retrieved inserts using subjective scales to grade post damage and wear. Of the IB PS II inserts, 38% demonstrated severe wear compared with only 25% of IB PS I inserts. The most prevalent damage location for the IB PS II was the anterior face, whereas the IB PS I sustained wear mainly on the medial face. While the IB PS post was not designed to constrain posterior femoral displacement, our observations confirm contact in hyperextension or other paradoxic anterior tibial translation is common and design-dependent. Minimizing wear and damage through proper post placement and changes in implant design to anticipate contact on the anterior post should be considered for future posterior stabilized knee replacements. These changes cannot occur in isolation, however, because changes in post placement and design also depend on their relation to the shape and location of the tibial bearing surfaces.
Introduction
The original Insall-Burstein posterior-stabilized (IB PS I) total knee replacement has provided pain relief, restoration of function, and long-term survivorship of 94% at 18 years [4, 19]. The design was introduced in the 1970s with the intent of improving range of motion and joint stability over total condylar prostheses [12]. The original design was offered with both an all-polyethylene tibial component and a monoblock metal-backed polyethylene tibial component in which the ultra-high-molecular-weight polyethylene (UHMWPE) was molded on the metal tray by the manufacturer. In 1988, the IB PS II was introduced with several modifications, including a broader range of size options, a deeper trochlear groove on the femoral component, a modular metal-backed tibial component, and alteration of the location and height of the tibial post. The latter design modification was to allow for increased flexion. Initial clinical results from the IB PS II demonstrated more than twice the dislocation rate than reported for the IB PS I [14]. In response, the post was moved 2 mm anteriorly and increased in height by 2 mm; the femoral box design was not altered.
Wear of the UHMWPE tibial post in posterior-stabilized designs has been identified as a potential source of substantial wear debris with retrieval studies revealing evidence of post wear on 100% of the implants for all designs examined [3, 7, 9, 14, 16, 17]. Kinematic factors such as loss of anterior cruciate ligament function during knee replacement, hyperextension, and collateral instability can be associated with anterior post wear or contact. Although wear and damage to the posterior surface of the post is to be expected given the intended function of the design in restricting anterior translation of the femur during flexion, the retrieval analyses revealed severe anterior post wear or complete fracture in as many as half of the retrieved implants. These studies, however, did not identify the influence of implant design on the propensity or severity of wear and facture, and none included examination of retrieved components from the original posterior-stabilized design, the IB PS I.
Therefore, we compared the location and severity of wear and damage to the polyethylene post in a series of retrieved IB PS I and IB PS II total knee replacements. This afforded us the opportunity to examine the effect of changes to the post design in two implants that otherwise were similar in design, including the design of the bearing surfaces. We hypothesized the differences in post placement affected the articulation of the femoral component with the tibial insert and that, as a result of the design change, IB PS II inserts would exhibit greater anterior post wear than the IB PS I inserts.
Materials and Methods
We have retrieved 234 IB PS I and IB PS II total knee inserts since 1978 as part of a large, ongoing, Institutional Review Board-approved implant retrieval system at our institution. The collection contained 48 IB PS I tibial components and 186 IB PS II tibial components. Within the IB PS I group, 39 were manufactured by Zimmer, Inc (Warsaw, IN) and nine were manufactured by Johnson & Johnson (Raynham, MA). Within the IB PS II group, 32 had the original post location; the remaining 154 had the modified post location. All of the IB PS II components were manufactured by Zimmer, Inc. All of the polyethylene tibial inserts had been gamma-radiated in air.
Patient demographic data were available for 211 of the retrieved inserts: age, weight, height, length of implantation, and reason for revision (Table 1). The most common reasons for revision were mechanical failure (36% of the cases) followed by infection (34%), aseptic loosening (14%), and other miscellaneous diagnoses (16%). The average length of implantation was similar: 3 ± 3.4 years (range, 0.25–10 years) for IB I inserts and 6 ± 13 years (range, 0.16–12.2 years) for IB II inserts. However, within the IB I group, the few Johnson & Johnson components were in for a substantially longer length of implantation than the Zimmer inserts (Table 1).
Table 1.
Patient demographics with subgroups for manufacturer and design changes
| Design | Weight (kg) | Height (cm) | Age (years) | Length of implantation (years) |
|---|---|---|---|---|
| IB PS I | 78 ± 20 | 161 ± 18 | 69 ± 12 | 4 ± 4.1 |
| Zimmer (n = 39) | 80 ± 20 | 161 ± 19 | 68 ± 12 | 3.5 ± 3.7* |
| Johnson & Johnson (n = 9) | 68 ± 17 | 163 ± 9 | 71 ± 13 | 7.1 ± 5* |
| IB PS II | 87 ± 21 | 168 ± 12 | 63 ± 14 | 3.9 ± 7.8 |
| Original (n = 32) | 87 ± 20 | 170 ± 13 | 65 ± 14 | 3.4 ± 3.1 |
| Modified (n = 154) | 88 ± 21 | 167 ± 11 | 63 ± 14 | 4 ± 8.5 |
All values are means ± standard deviation; *within subgroups, the only significant difference was in length of implantation between the Zimmer and Johnson & Johnson IB PS I components.
Radiographic evaluation was performed by one of the investigators (MK) using the method of Ewald [5]. The investigator was blinded to the demographic and retrieval data at the time of the evaluation. From the anteroposterior view, the femoral joint line angle was measured from a line drawn parallel to the femoral condyles to a line drawn along the femoral shaft axis. This femoral angle was referenced from neutral and reported as varus or valgus. The tibial angle was measured between the line drawn parallel to the plateau of the metallic tibial tray and a line drawn along the tibial shaft axis. On the lateral view, femoral component flexion-extension angle was measured between a line perpendicular to the box cut for the femoral component, (5° anteriorly for IB I and 12° anteriorly for IB II) and a line parallel to the femoral shaft axis. Anterior and posterior sloping of the tibial component was measured between a line parallel to the plateau of the metallic tibial tray and the line denoting the tibial shaft axis. Measurements reported were femoral varus-valgus angle, tibial angle, femoral component flexion-extension angle, and tibial posterior slope (Table 2).
Table 2.
Component orientation (in degrees) determined radiographically with subgroups for manufacturer and design changes
| Design | Femoral varus-valgus | Tibial angle | Femoral flexion-extension | Tibial posterior slope |
|---|---|---|---|---|
| IB PS I | 10.9 valgus ± 12° | −1.7 varus ± 5.8° | 1.3 flexion ± 7.4° | 2.5 ± 6.7° |
| Zimmer (n = 39) | 7.6 valgus ± 6°* | −1.6 varus ± 3.2° | 0.3 flexion ± 5.8° | 1.2 ± 4.1° |
| Johnson & Johnson (n = 7) | 20.7 valgus ± 19°* | −2.1 varus ± 10.7° | 4.3 flexion ± 11.3° | 1.2 ± 4.1° |
| IB PS II | 7.1 valgus ± 5.4° | −0.7 varus ± 3.3° | 2.2 flexion ± 6° | 0.3 ± 1.6° |
| Original | 8.3 valgus ± 5.3° | −0.7 varus ± 3.8° | 3.3 flexion ± 5.3° | 0.1 ± 0.5° |
| Modified | 6.7 valgus ± 5.4° | −0.7 varus ± 3.2° | 1.9 flexion ± 5.1° | 0.4 ± 1.8° |
*Within subgroups, the only significant difference was in femoral varus-valgus angle between the Zimmer and Johnson & Johnson IB PS I components.
All inserts were examined for evidence of surface damage and wear to the anterior, medial, and lateral faces of the post. Damage was determined by the extent of the face that was involved with surface damage as defined by the method of Hood et al. [10], and a similar subjective scale of 0 to 3 was used to grade the severity of wear damage based on removal of material (Table 3). Grading was performed by two independent observers (BF, MK) blinded to the demographic and radiographic data at the time of the grading. Any discrepancies in scoring were resolved by a third independent observer (TMW). The scores for each damage mode were totaled to determine the most prevalent modes. Additionally, the location and mode associated with the greatest amount of wear were also noted.
Table 3.
Definitions of grading scores for damage and wear of the tibial post
| Score | Damage* | Wear |
|---|---|---|
| 0 | 0% of face of post | No visible removal of material |
| 1 | < 10% | Minimal removal of material |
| 2 | 10% to 50% | Measurable removal of material |
| 3 | > 50% | Severe removal of material |
*As defined by the method of Hood et al. [6].
To determine if design changes had influenced wear damage to the post, the dominant wear locations of the retrieved IB I and IB II inserts were compared using the Fisher’s exact test, which assumes no ordering in severity based on location. Patient demographics were compared using Student’s t-test; wear scores, damage scores, and for the IB I inserts, manufacturer, were compared using the Mann-Whitney test. Correlations were determined using the Spearman rank correlation. The Type I error rate was set at 0.05.
Results
All 234 inserts showed evidence of wear and damage to the tibial UHMWPE post. The wear and damage scores were similar (p = 0.37) between the Zimmer and Johnson & Johnson IB I inserts so we pooled the data from IB PS I inserts. Scores were also similar (p = 0.22) between IB II inserts implanted before 1990, the original design, and those implanted after 1990, the modified design, so these data were also pooled. We observed few differences in demographic and radiographic data between the subdivisions for IB PS I (by manufacturer) and IB PS II (by original versus modified designs), further validating pooling of the data from the groups (Tables 1, 2). Furthermore, removing the few poorly aligned IB I Johnson & Johnson components in extreme flexion did not alter the results.
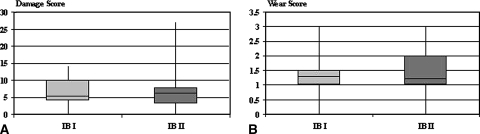
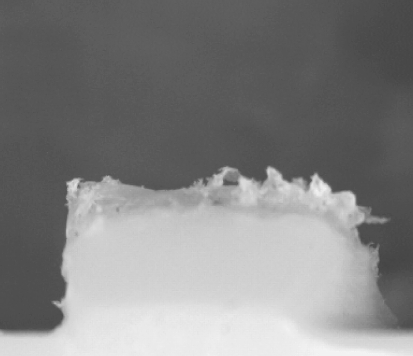
The total damage scores for IB I and IB II inserts were similar (p = 0.09), although 38% of IB II inserts received severe grades compared with only 25% of IB I inserts. The range of values for the total damage scores were 6.65 ± 3.89 (range, 0–16) for the IB PS I and 5.88 ± 4.24 (range, 0–27) for the IB PS II inserts (Fig. 1). The most prevalent damage mode was burnishing, found on 45 (94%) of the IB I inserts and 152 (82%) of the IB II inserts. Delamination and fracture were noted in only one each of the IB I retrieved inserts, whereas for the IB II inserts, pitting was found in 20 inserts (11%) and delamination in 10 (5%); three IB II posts had fractured from the remainder of the insert (Fig. 2).
Fig. 1A–B.
Box plots for damage and wear scores for IB I and IB II. No statistical differences were found in (A) total damage or (B) total wear scores for all IB PS I versus all IB PS II components.
Fig. 2.
Fractured post of IB II posterior stabilized tibial insert is shown. Complete fracture of the post was found on three IB II inserts and one IB I insert.
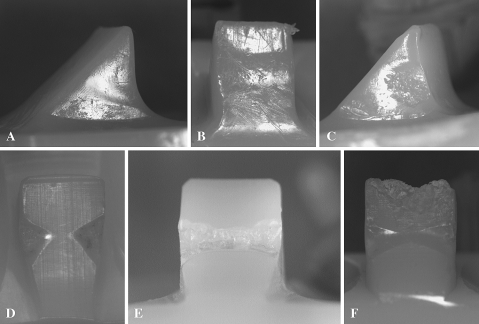
We observed damage most often on the medial face of the post for IB I inserts and on the anterior face of the post of IB II inserts (Table 4); damage was more prevalent (p = 0.002) in these two locations as compared with the other faces of the posts on these two designs. The damage scores for the medial and anterior faces on the IB PS I inserts correlated (r2 = 0.47, p = 0.03) with the femoral varus-valgus angle. Those implants in a more valgus alignment had higher damage scores on the medial and anterior faces. For the IB I inserts, the wear modes most associated with measurable wear (with a score ≥ 2) were burnishing and pitting, most commonly found on the anterior and lateral faces of the post (Fig. 3A–C). For the IB II inserts, burnishing was also the damage mode most associated with measurable wear. Burnishing was most commonly found (in 61 of the 64 inserts) on the anterior face of the post (Fig. 3D–F). Damage on the anterior face of both designs was often restricted to a bowtie-shaped area matching the geometry of the contacting femoral component in extension (Fig. 3D–F). The border of the bowtie formed the edge of the fracture surface of some of the fractured posts (Figs. 2, 3F) consistent with the damage being associated with fracture initiation.
Table 4.
Dominant wear location on posts for IB I and IB II retrieved inserts
| Design | Medial | Lateral | Anterior | Top |
|---|---|---|---|---|
| IB PS I | 46% | 27% | 27% | 0% |
| IB PS II | 35% | 11% | 53% | 0.5% |
Fig. 3A–F.
Damage patterns on medial and anterior faces of the tibial post on IB I and IB II retrieved inserts. Design, location, and length of implantation are identified for each figure. The dominant wear locations were on the medial face for the IB I inserts and on the anterior face for the IB II inserts. (A) IB I, medial, 4 years; (B) IB I, anterior, 2.9 years; (C) IB I, medial, 10.3 years; (D) IB II, anterior, 2.5 years; (E) IB II, anterior, 7 years; (F) IB II, anterior, 6.3 years.
No correlation was found between the amount of flexion in which the femoral component was oriented and anterior post wear. The only demographic data that correlated to the wear and damage scores were length of implantation. For both IB I and IB II designs, damage scores increased (p < 0.001) with increasing length of implantation.
Discussion
Changes made in the post placement between the IB PS I and IB PS II total knee designs led to increased clinical dislocation rates [14], which we hypothesized would be associated with greater wear damage on the anterior surface of the post because the more anterior post placement creates in effect a constraint against hyperextension and posterior translation of the femur on the tibia. Reports [7, 17] of substantial post wear emphasize the important effect these design parameters might have on long-term clinical success of PS designs.
As with any study of retrieved implants, conclusions that can be drawn are limited in that the implants were retrieved at reoperation and thus might not represent well-functioning knee replacements. For example, our collection included knee replacements revised for instability, for which hyperextension and accompanying impingement on the anterior post would be expected. Nonetheless, our study mirrors others in the literature [1, 3, 7, 9, 14, 16, 17] in suggesting that anterior impingement is a common occurrence in posterior-stabilized knee designs regardless of revision diagnosis.
The emphasis in our study was on polyethylene wear and surface damage, which can be measured subjectively in retrospective retrieval studies [10]. The predominance of wear on the anterior surface of the post in IB II inserts compared with IB I inserts was probably related to the more anterior post location. Moving the post anteriorly in the IB II design causes contact with the front inside edge of the intercondylar metallic femoral box to occur at smaller angles of hyperextension. This contact occurs with the implant components in hyperextension but, because of anterior bow of the femur and/or posterior slope of the tibial tray, this might correspond to full extension or a few degrees of physiological flexion.
Contact with the box would also occur with smaller posterior displacements of the femoral component when the joint was in extension. However, such displacements are unlikely given the condylar nature of the bearing surfaces and the large compressive loads across the joint for most activities near extension (for example, the stance phase of gait). Indeed, fluoroscopic studies of patients in activities such as gait, stairclimbing, and deep knee bends showed little evidence of such posterior femoral translation [2, 6, 18]. Furthermore, the dominance of the bowtie appearance on the anterior faces of the posts also suggests hyperextension rather than posterior displacements of the femoral component because this shape is consistent only with the shape of the anterior box of the femoral component when the component is in hyperextension. Posterior displacement would cause impingement higher up on the anterior face and result in a shape different than a bowtie. The severity of the wear could be affected by other factors such as length of implantation, although no such effect was found in our results; nonetheless, such factors would not be expected to affect the location of wear damage.
A possible explanation for the higher preponderance of wear on the lateral face of IB I compared with IB II posts was the higher degree of valgus alignment for the femoral components in the IB I, making contact more likely with the side (rather than the front) of the post. Nonetheless, the much lower anterior wear and damage observed on the IB I inserts suggests moving the post anteriorly to gain additional range of motion in the IB II design may have been compromised by greater wear damage and liberation of greater amounts of wear debris.
The dominance of anterior wear that we observed on the retrieved implants suggests impingement with the femoral component was a common occurrence in this group of patients. Contact between the tibial post and the anterior intercondylar femoral box was never intended as a constraint to posterior displacement of the femoral component during hyperextension. Nonetheless, recent in vitro tests using conditions of heel strike showed box-post impingement acts as a substitute for the anterior cruciate ligament in posterior-stabilized knee implants [13]. Contact during vigorous hyperextension can create major local stresses in the polyethylene, consistent with fatigue wear modes (pitting and delamination) and crack initiation and fracture. These stresses can be ameliorated by redesign of the anterior femoral box and tibial post as contact surfaces, which should reduce the propensity for wear damage and fracture [8, 11, 15]. Anterior post impingement might also affect the kinematics of the knee by altering or limiting the internal/external rotation of the femur depending on the relative orientation of the tibial and femoral components [1], another reason for considering design changes to these structures.
In summary, our data support the hypothesis that a more anterior placement of the post on posterior-stabilized tibial knee components adversely affects polyethylene wear and damage. Posterior-stabilized designs should incorporate this important consideration among other considerations (for example, range of motion and susceptibility to dislocation) in positioning the post-cam mechanism.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Banks SA, Harman MK, Hodge WA. Mechanism of anterior impingement damage in total knee arthroplasty. J Bone Joint Surg Am. 2002;84(Suppl 2):37–42. [DOI] [PubMed]
- 2.Banks SA, Hodge WA. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty. 2004;19:809–816. [DOI] [PubMed]
- 3.Clarke HD, Math KR, Scuderi GR. Polyethylene post failure in posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:652–657. [DOI] [PubMed]
- 4.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D. Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79:575–582. [DOI] [PubMed]
- 5.Ewald F. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed]
- 6.Fantozzi S, Catani F, Ensini A, Leardini A, Giannini S. Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res. 2006;24:2222–2229. [DOI] [PubMed]
- 7.Furman B, Gillis AM, Schmieg JJ, Bhattacharyya S, Li S. Wear and damage to the post in posterior stabilized total knee replacements: an unexpected source of polyethylene debris. Trans Soc Biomatls. 1999;22.
- 8.Gortner M, Lipman J, Wright T, Bartel D. Finite element analysis of anterior post impingement on posterior stabilizing total knee prostheses. Trans Orthop Res Soc. 2006;31:570.
- 9.Hendel D, Garti A, Weisbort M. Fracture of the central polyethylene tibial spine in posterior stabilized total knee arthroplasty. J Arthroplasty. 2003;18:672–674. [DOI] [PubMed]
- 10.Hood R, Wright TM, Burstein AH. Retrieval analysis of total knee prostheses: a method and its application to 48 total condylar prostheses. J Biomed Mater Res. 1983;17:829–942. [DOI] [PubMed]
- 11.Huang CH, Liau JJ, Huang CH, Cheng CK. Stress analysis of the anterior tibial post in posterior stabilized knee prostheses. J Orthop Res. 2007;25:442–449. [DOI] [PubMed]
- 12.Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: a modification of the total condylar design. Two to four-year clinical experience. J Bone Joint Surg Am. 1982;64:1317–1323. [PubMed]
- 13.Li G, Papannagari R, Most E, Park SE, Johnson T, Tanamal L, Rubash HE. Anterior tibial post impingement in a posterior stabilized total knee arthroplasty. J Orthop Res. 2005;23:536–541. [DOI] [PubMed]
- 14.Lombardi AV Jr, Mallory TH, Vaughn BK, Krugel R, Honkala TK, Sorscher M, Kolczun M. Dislocation following primary posterior-stabilized total knee arthroplasty. J Arthroplasty. 1993;8:633–639. [DOI] [PubMed]
- 15.Nakayama K, Matsuda S, Miura H, Iwamoto Y, Higaki H, Otsuka K. Contact stress at the post-cam mechanism in posterior-stabilized total knee arthroplasty. J Bone Joint Surg Br. 2005;87:483–488. [DOI] [PubMed]
- 16.O’Rourke MR, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Osteolysis associated with a cemented modular posterior-cruciate-substituting total knee design: five to eight-year follow-up. J Bone Joint Surg Am. 2002;84:1362–1371. [DOI] [PubMed]
- 17.Puloski SK, McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB. Tibial post wear in posterior-stabilized total knee arthroplasty: an unrecognized source of polyethylene debris. J Bone Joint Surg Am. 2001;83:390–397. [DOI] [PubMed]
- 18.Ranawat CS, Komistek RD, Rodriguez JA, Dennis DA, Anderle M. In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res. 2004;418:184–190. [DOI] [PubMed]
- 19.Stern S, Insall J. Posterior stabilized prosthesis. Results after follow-up of nine to twelve years. J Bone Joint Surg Am. 1992;74:980–986. [PubMed]