Abstract
Controversy exists as to whether bearing mobility facilitates centralization of the extensor mechanism after TKA. To assess the incidence of lateral retinacular release, we retrospectively reviewed 1318 consecutive primary TKAs (1032 patients) performed by one surgeon using either a rotating-platform bearing (940) or a fixed bearing (378) from the same implant system. The selection of a fixed- versus mobile-bearing TKA was primarily based on age with patients younger than 70 years receiving a mobile-bearing TKA. We performed a lateral release whenever continuous symmetric patellar facet contact with the trochlear groove from 0° to 90° of flexion was not obtained using the rule of no thumb after tourniquet release. One hundred four of 1318 knees (7.9%) had a lateral release. We performed more lateral releases in the fixed-bearing group (14.3% [54 of 378]) than in the mobile-bearing group (5.3% [50 of 940]). Patellar tilt occurred more often in the mobile-bearing group (10% [94 of 940]) than in the fixed-bearing group (6.9% [26 of 378]), although the magnitude of mean patellar tilt was small in both groups (mobile-bearing 3.0°; fixed bearing 2.55°). No patient had patellar subluxation greater than 5 mm. We suspect the fewer lateral releases in the mobile-bearing group is the result of better extensor mechanism centralization provided by bearing rotation.
Level of Evidence: Level III, prognostic study. See the Guidelines for a complete description of levels of evidence.
Introduction
TKA has become a standard operative procedure to relieve pain and restore function in patients with disabling arthritis of the knee. Several studies have been conducted on the outcome of TKA and the results have been very encouraging [6, 9, 10, 29, 30]. Current total knee prosthetic devices can be subdivided into two groups based on mobility of the polyethylene bearing. In fixed-bearing knees, the polyethylene tibial insert is locked into the tibial tray, whereas in mobile-bearing TKA designs, motion of the polyethylene insert relative to the tibial tray is permitted [22]. Use of mobile-bearing TKA has been a focus of renewed interest in North America in recent years [8, 11, 12]. This renewed interest, at least in part, has been related to recent kinematic analyses demonstrating a rotating-platform polyethylene insert self-aligns with the femoral component during knee flexion, independent of the rotation of the tibial tray. Polyethylene bearing self-alignment in mobile-bearing designs creates the potential to accommodate small mismatches in the rotational position of the tibial and femoral components, potentially facilitating central patellar tracking, thereby decreasing the incidence of lateral retinacular release and postoperative patellar tilt or subluxation. In a prospectively randomized study, Pagnano et al. [26], however, reported no difference in the incidence of lateral retinacular release in a multisurgeon analysis of 160 fixed-bearing versus 80 rotating-platform posterior-stabilized TKA subjects.
In this review, we asked the following questions: (1) Will the incidence of lateral release be lower in a larger mobile-bearing cohort performed using a standardized technique? (2) What was the incidence and magnitude of patellar tilt in a series of fixed- and mobile-bearing TKA? and (3) Was the amount of patellar tilt reduced if a lateral retinacular release was performed?
Materials and Methods
We retrospectively reviewed 1032 consecutive patients (1318 TKAs) with advanced osteoarthritis or rheumatoid arthritis who had a primary tricompartmental TKA between September 2000 and March 2007. No inclusion or exclusion criteria were used to select patients for this study other than having a primary TKA performed by the senior author during the study period. All subjects were implanted with a single posterior-stabilized knee design (PFC® Sigma™; DePuy Orthopaedics, Inc, Warsaw, IN) using bone cement fixation for all components. The femoral and patellar components were identical and the tibial component type was either a mobile-bearing rotating-platform tibial design or a fixed-bearing tibial design (all-polyethylene or modular metal-backed tibial component). The selection of a fixed- versus mobile-bearing TKA was primarily based on age and lifestyle with patients younger than 70 years of age receiving a mobile-bearing TKA. There were 608 women and 424 men in the study with a mean age of 66 years (range, 24–87 years). Females predominated in both the fixed- (72.9% females) and mobile-bearing (53.9% females) groups. There were 652 left TKAs and 666 right TKAs. Mobile-bearing TKA devices were implanted in 940 cases (71.3%) and fixed-bearing knees were implanted in 378 cases (28.7%), including 300 all-polyethylene tibial components and 78 modular metal-backed tibial components. The minimum followup was 1 year with a range up to 78 months. We had complete radiographic followup at a minimum of one year in all patients, but not complete clinical data.
All surgery was performed by the senior author (DAD). A standard anterior midline skin incision and medial parapatellar arthrotomy was used to expose the knee in all patients. The medial and lateral soft tissues were balanced in the standard manner using previously described ligamentous balancing techniques [18]. All knee procedures were performed using a gap-balancing technique with the anteroposterior [2] and transepicondylar axes [3] serving as secondary determinants of the rotational orientation of the femoral component. All implanted patellar components were an onlay, all-polyethylene ovalized dome-shaped design with three fixation lugs. The preresection thickness of the patella was measured in all cases and the patellar resection performed with a specialized cutting jig designed to create a composite thickness of the patellar component and the remaining patellar bone that duplicated the native patella thickness. All patella components were positioned to reproduce the position of the native patella high point as described by Yoshii et al. [33] whenever possible.
The intraoperative assessment of patellar tracking was performed after component insertion using the “rule of no thumb” [31] in which the patella was reduced into the trochlear groove and the knee was placed through a full range of motion without any additional thumb stabilization. A strict guideline was used in all cases to determine acceptable tracking of the patellar component. Acceptable tracking was defined as a patella that remained centered in the trochlear groove with bicondylar contact through 90° of flexion with no tendency for subluxation or separation of a patellar facet from the trochlear groove. If patellar tracking was inadequate (ie, lack of perfect bicondylar contact), the pneumatic tourniquet was deflated and tracking was reassessed using the rule of no thumb [20]. If bicondylar contact of both the medial and lateral patellar facets from 0° to 90° of flexion was not present , then a lateral retinacular release procedure was performed (inside-out technique). Any release of retinacular tissue including piecrusting was considered a lateral release.
Postoperatively, all patients began continuous passive motion beginning at 60° of flexion on the day of surgery. This was continued and increased daily during the patient’s hospital stay. Physiotherapy was initiated on the day of operation or the first postoperative day and included walker or bilateral crutch ambulation (weightbearing as tolerated), knee range of motion, muscle strengthening, and stair training. The majority of patients in both groups were discharged on the second or third postoperative day and participated in an outpatient physiotherapy program three times weekly for a period of 4 to 6 weeks.
Clinic charts, operative reports, and radiographs were retrospectively reviewed. The routine patient followup intervals used in this study were 2 weeks, 6 weeks, 3 months, 12 months, and every 2 years thereafter.
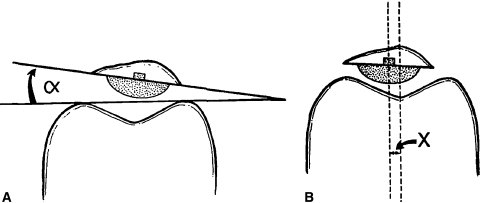
Initial postoperative radiographs were obtained within the first 6 weeks after the surgical procedure. These included a standing anteroposterior view of both knees, a lateral radiograph, a Merchant view of the patella, and a full-length standard hip-knee-ankle radiograph [23]. These same radiographs were obtained at sequential postoperative visits (at least annually) to recalculate alignment and the position of the components. All radiographic measurements were performed in accordance with the Knee Society roentgenographic evaluation and scoring system [15]. Patellar tilt and subluxation were measured according to the technique of Gomes et al. [16]. For our study, patellar tilt of more than 5° and subluxation of more than 5 mm were defined as noteworthy [4] (Fig. 1).
Fig. 1A–B.
Diagrams illustrate the radiographic measurements used to determine (A) patellar tilt angle (α) and (B) patellar subluxation from the center of the trochlear groove (X). (Reprinted with permission and copyright © 1993 of Lippincott Williams & Wilkins from Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop Relat Res. 1993;286:103–109.)
Statistical analysis for nominal variables was carried out using Fisher’s exact test. For the continuous variables, Student’s t test (for equal variances) and Welch’s analysis of variance test (for unequal variances) were used for the statistical comparison. Check for equality of variance was carried out using Levene’s test. Differences in the incidence of the lateral retinacular release (treated as a nominal variable) were compared between the fixed-bearing tibial components and the rotating-platform tibial components using Fisher’s exact test. The amount of patellar tilt was treated as a continuous variable. Differences in patellar tilt using parametric tests (the data were normally distributed using the Shapiro-Wilk test for normality) were compared for two cases: (1) between the fixed-bearing tibial components and the rotating-platform tibial components; and (2) between those patients having lateral retinacular release and patients who did not have lateral retinacular release. For these cases, check for equality of variance was first carried out using Levene’s test. This was followed by the Student’s t-test (when the variances were equal) and Welch’s analysis of variance test (when the variances were unequal). All statistical tests were carried out in the commercially available JMP® Statistical DiscoveryTM Software (SAS Institute Inc, Cary, NC).
Results
The overall lateral retinacular release rate in the study was 7.9% (104 of 1318 knees) after primary cemented TKA. The incidence of lateral retinacular release was higher (p < 0.0001) for knees with a fixed-bearing tibial component (54 of 378 [14.3%]) than for knees with a rotating-platform tibial component (50 of 940 [5.3%]).
The overall incidence of postoperative patellar tilt of 5° or more shown on Merchant followup radiographs of the patella was 9.1% (120 of 1317 knees). One patient had prior total patellectomy and thus was excluded from this measurement. The incidence of residual patellar tilt was higher (p = 0.0122) in the mobile-bearing group (94 of 940 [10.0%]) than in the fixed-bearing group (26 of 378 [6.9%]). The incidence, direction (medial or lateral), and mean patellar tilt angles for the three cohorts have been described (Table 1). The mean patellar tilt angle for the entire group was 2.89°, for the entire mobile-bearing cohort was 3.0°, and for the fixed-bearing group was 2.55°.
Table 1.
Incidence, direction, and magnitude of patellar tilt
| Cohort | Incidence | Medial tilt (number) | Mean medial patellar tilt angle* | Lateral tilt (number) | Mean lateral patellar tilt angle† | Mean patellar tilt angle‡ |
|---|---|---|---|---|---|---|
| Entire cohort (N = 1318) | 120 (9.1%) | 23 | 7.4° (5.1°–14°; SD = 1.9°) | 97 | 8.6° (5.3°–16°; SD = 2.7°) | 2.89° |
| Mobile-bearing (N = 940) | 94 (10.0%) | 14 | 7.1° (5.1°–10°; SD = 1.5°) | 80 | 8.6° (5.5°–15.2°; SD = 2.7°) | 3.0° |
| Fixed-bearing (N = 378) | 26 (6.9%) | 9 | 7.9° (6°–14°; SD = 2.5°) | 17 | 8.6° (6°–16°; SD = 3.0°) | 2.55° |
*Mean tilt angle of those demonstrating medial patellar tilt; †mean tilt angle of those demonstrating lateral patellar tilt; ‡mean tilt angle of all cohort subjects (medial tilt, lateral tilt, or no tilt); SD = standard deviation.
In both the fixed-bearing group (p = 0.0212) and the mobile-bearing group (p = 0.0002), the amount of patellar tilt was higher in patients in whom a lateral retinacular release was not performed.
No patient in either study group demonstrated patellar subluxation of more than 5 mm on followup radiographs. No patient had patellar dislocation postoperatively.
Discussion
The aims of this study were to determine if the incidence of lateral retinacular release would be lower in a large cohort of subjects who had received a rotating-platform TKA implanted by a single surgeon using a standardized technique. Additionally, we sought to determine the incidence and magnitude of patellar tilt in patients implanted with either a fixed- versus mobile-bearing TKA and if the amount of patellar tilt was reduced if a lateral retinacular release was performed.
Although we evaluated the incidence of lateral retinacular release and patellar tilt in fixed- and mobile-bearing TKAs, we did not evaluate other parameters such as long-term clinical results. A second limitation is its nonrandomized nature with specific selection criteria (age older than 70 years receiving a fixed-bearing TKA). The gender distribution was unequal in the two groups, possibly influencing the number of lateral retinacular releases performed. Additionally, preoperative alignment data were not available for all subjects and complete clinical followup was not available in all patients. To minimize these limitations, we selected a large cohort of consecutive patients undergoing TKA performed by a single surgeon using a single, standardized surgical technique on each patient. Additionally, a single TKA implant system with identical femoral and patellar component condylar geometry was used, thus limiting design variations that could interfere with the results. Lastly, a single, strict lateral release selection criterion was used in all cases regardless of the type of prosthesis.
The overall lateral retinacular release rate in our entire study group was 7.9% after primary cemented TKA. When comparing fixed-bearing versus mobile-bearing TKA, the incidence of lateral retinacular release was lower in the mobile-bearing group (5.3%) than in the fixed-bearing group (14.3%). In the current literature, the lateral retinacular release rate has varied from 0% to as high as 40% [14, 20, 26]. Traditional teaching has emphasized the importance of performing a lateral retinacular release to enhance proper patella tracking [1, 5, 17]. A lateral retinacular release, however, risks potential complications, including an increased risk of hematoma and postoperative bleeding, disruption of patellar blood flow with subsequent patellar avascular necrosis and fracture as well as extensor mechanism disruption, wound and skin complications, medial patellar instability, and symptomatic snapping of the retinacular tissue edge over the lateral “corner” of the femoral component during flexion [7, 20, 21, 24, 25, 28, 32]. For these reasons, this procedure should be performed with caution.
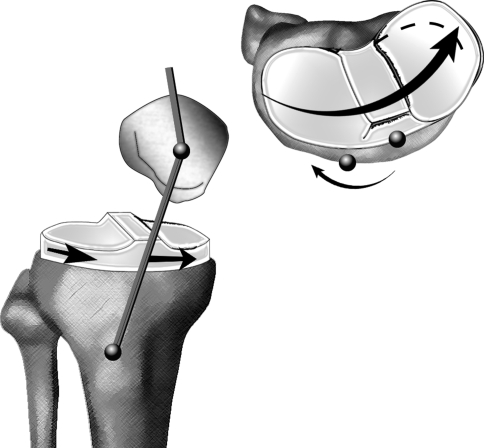
The authors hypothesize that the reduced need for lateral retinacular release in patients implanted with a mobile-bearing TKA is the result of the ability of a mobile-bearing (rotating-platform) polyethylene insert to self-align with the femoral component. This phenomenon allows for accommodation of small mismatches in the rotational position of the tibial and femoral components, which can be seen in fixed-bearing TKAs. We believe this self-aligning feature facilitates centralization of the extensor mechanism and a subsequent reduction in the incidence of patellar subluxation and the need to perform a lateral retinacular release. In contrast, if a fixed-bearing tibial component is positioned internally rotated on the proximal tibia, the potential to derotate its position to self-center with the femoral component is less, resulting in lateralization of the tibial tubercle, an increase in the Q angle, and an increased lateral force vector on the patella (Fig. 2). This hypothesis is supported by numerous fluoroscopic kinematic analyses [13, 19, 27]. Two fluoroscopic kinematic studies have been performed in which tantalum beads were implanted within the polyethylene insert, which permitted fluoroscopic tracking of motion of the polyethylene bearing [13, 19]. In both reports, mobility of the polyethylene bearing was observed in all subjects and the bearing primarily rotated with the femoral component, confirming the self-centering concept. In an additional fluoroscopic kinematic evaluation of patellofemoral kinematics of fixed- versus mobile-bearing TKA, Rees et al. [27] observed the patellofemoral kinematics of mobile-bearing TKA designs more closely replicated those of the normal, nonimplanted knee.
Fig. 2.
A diagram demonstrates how placement of a fixed-bearing tibial component internally rotated on the proximal tibia results in lateralization of the tibial tubercle, an increase in Q angle, and a subsequent increased lateral force vector on the patella.
In contrast to our results, Pagnano et al. [26] reported on a prospective, randomized study of 240 primary TKAs (80 fixed-bearing TKAs with a modular, metal-backed tibial component, 80 fixed-bearing TKAs with an all-polyethylene tibial component, and 80 mobile-bearing TKAs with a rotating-platform tibial component) using the same implant system we used and observed no difference in the incidence of lateral retinacular release with the use of a rotating-platform versus a fixed-bearing implant. The operative procedures in this report were performed by four different yet highly experienced surgeons. We theorize the differing results in these two reports may be related, at least in part, to both technical differences in surgical technique among participating surgeons as well as differences in the threshold used by individual surgeons in choosing to perform a lateral retinacular release. The incidence of lateral retinacular release was higher in our study (7.9%) than that reported by Pagnano et al. [26] (nine of 240 patients [3.8%]), which is likely reflective of the strict criteria (perfect bicondylar contact of both patellar facets from 0° to 90° of flexion) we used to perform a lateral retinacular release.
Patellar tilt, as observed on postoperative Merchant radiographs, may represent a more subtle form of patellar maltracking. The overall incidence of radiographic patellar tilt in our study was 9.1% and was slightly higher in the mobile-bearing group (10.0%) than in the fixed-bearing group (6.9%). In both groups, the amount of patellar tilt was higher in patients in whom a lateral retinacular release was not performed. This could account for the minor increase in patellar tilt observed in the mobile-bearing group, because this group had a substantially lower number of lateral retinacular release procedures performed. For example, patellar tilt was noted in only one of 50 (2%) mobile-bearing TKAs in which a lateral release was performed. We theorize the long-term clinical importance of the current minor differences in incidence and magnitude of patellar tilt observed between the fixed- (incidence, 6.9%; mean patellar tilt, 2.55°) and mobile-bearing (incidence, 10.0%; mean patellar tilt, 3.0°) cohorts will not likely result in substantial clinical differences at long-term clinical followup, particularly in light of the fact we observed no patellar subluxation greater than 5 mm in either the fixed- or mobile-bearing groups. This is supported by the analysis of Bindelglass et al. [4] who reported pain, flexion, and fixation were not affected by patellar tilt or displacement.
In both the fixed and mobile-bearing groups, the amount of patellar tilt was higher in those subjects in which a lateral retinacular release was not performed. This suggests the value of a lateral retinacular release in improving patellar tracking should considerable patellar tilt be encountered. This is in contrast to the study of Bindelglass et al. [4] who observed no improvement in patellar tilt in patients in whom a lateral retinacular release was performed.
In this large, single-surgeon series, a posterior-stabilized rotating-platform mobile-bearing TKA was associated with a lower incidence of lateral retinacular release when compared with a posterior-stabilized fixed-bearing TKA. Only with further followup can it be determined whether rotating-platform TKA designs do or do not confirm their other theoretical longer-term benefits in regard to reduced polyethylene wear, more durable long-term fixation, and patellofemoral performance.
Acknowledgments
We thank the staff of the Rocky Mountain Musculoskeletal Research Laboratory for support in the production of this research.
Footnotes
One of the authors (DAD) has received funding from DePuy, Inc.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aglietti P, Buzzi R, Gaudenzi A. Patellofemoral functional results and complications with the posterior stabilized condylar knee prosthesis. J Arthroplasty. 1988;3:17–25. [DOI] [PubMed]
- 2.Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotation alignment based on the anteroposterior axis in total knee arthroplasty. J Bone Joint Surg Am. 1995;77:1331–1334. [DOI] [PubMed]
- 3.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotation alignment of the femoral component in the total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed]
- 4.Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop Relat Res. 1993;286:103–109. [PubMed]
- 5.Brick GW, Scott RD. The patellofemoral component of total knee arthroplasty. Clin Orthop Relat Res. 1988;231:163–178. [PubMed]
- 6.Buechel FF Sr. Long-term follow-up after mobile-bearing total knee replacement. Clin Orthop Relat Res. 2002;404:40–50. [DOI] [PubMed]
- 7.Busch MT, DeHaven KE. Pitfalls of the lateral retinacular release. Clin Sports Med. 1989;8:279–290. [PubMed]
- 8.Callaghan JJ, Insall JN, Greenwald AS, Dennis DA, Komistek RD, Murray DW, Bourne RB, Rorabeck CH, Dorr LD. Mobile-bearing knee replacement: concepts and results. J Bone Joint Surg Am. 2000;82:1020–1139. [PubMed]
- 9.Callaghan JJ, O’Rourke MR, Iossi MF, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC. Cemented rotating-platform total knee replacement: a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2005;87:1995–1998. [DOI] [PubMed]
- 10.Dennis DA, Clayton ML, O’Donnell S, Mack RP, Stringer EA. Posterior cruciate condylar total knee arthroplasty: average 11-year follow-up evaluation. Clin Orthop Relat Res. 1992;281:168–176. [PubMed]
- 11.Dennis DA, Komistek RD. Kinematics of mobile-bearing total knee arthroplasty. Instr Course Lect. 2005;54:207–220. [PubMed]
- 12.Dennis DA, Komistek RD. Mobile-bearing total knee arthroplasty: design factors in minimizing wear. Clin Orthop Relat Res. 2006;452:70–77. [DOI] [PubMed]
- 13.Dennis DA, Komistek RD, Mahfouz MR, Outten JT, Sharma A. Mobile-bearing total knee arthroplasty: do the polyethylene bearings rotate? Clin Orthop Relat Res. 2005;440:88–95. [DOI] [PubMed]
- 14.Engh GA, Parks NL, Ammeen DJ. Influence of surgical approach on lateral retinacular releases in total knee arthroplasty. Clin Orthop Relat Res. 1998;331:56–63. [DOI] [PubMed]
- 15.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed]
- 16.Gomes LS, Bechtold JE, Gustilo RB. Patellar prosthesis positioning in total knee arthroplasty: a roentgenographic study. Clin Orthop Relat Res. 1988;236:72–81. [PubMed]
- 17.Grace JN, Rand JA. Patellar instability after total knee arthroplasty. Clin Orthop Relat Res. 1988;237:184–189. [PubMed]
- 18.Insall JN, Windsor RE, Scott WN, Kelly MA, Aglietti P, eds. Surgery of the Knee. New York, NY: Churchill Livingstone; 1993.
- 19.Komistek RD, Dennis DA, Mahfouz MR, Walker SA, Tucker A. In vivo polyethylene bearing mobility is maintained in posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 2004;428:207–213. [DOI] [PubMed]
- 20.Laskin RS. Lateral release rates after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:88–93. [DOI] [PubMed]
- 21.Lee GC, Cushner FD, Scuderi GR, Insall JN. Optimizing patellofemoral tracking during total knee arthroplasty. J Knee Surg. 2004;17:144–149. [DOI] [PubMed]
- 22.McEwen HM, Barnett PL, Bell CJ, Farrar R, Auger DD, Stone MH, Fisher J. The influence of design, materials and kinematics on the in vitro wear of total knee replacements. J Biomech. 2005;38:357–365. [DOI] [PubMed]
- 23.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed]
- 24.Merkow RL, Soudry M, Insall JN. Patellar dislocation following total knee replacement. J Bone Joint Surg Am. 1985;67:1321–1327. [PubMed]
- 25.Nicholls RL, Green D, Kuster MS. Patella intraosseous blood flow disturbance during a medial or lateral arthrotomy in total knee arthroplasty: a laser Doppler flowmetry study. Knee Surg Sports Traumatol Arthrosc. 2006;14:411–416. [DOI] [PubMed]
- 26.Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ. Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res. 2004;428:221–227. [DOI] [PubMed]
- 27.Rees JL, Beard DJ, Price AJ, Gill HS, McLardy-Smith P, Dodd PA, Murray DW. Real in vivo kinematics differences between mobile-bearing and fixed-bearing total knee arthroplasties. Clin Orthop Relat Res. 2005;432:204–209. [DOI] [PubMed]
- 28.Ritter M, Herbst S, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty: effect of a lateral release and sacrifice of the superior lateral geniculate artery. J Arthroplasty. 1996;11:368–372. [DOI] [PubMed]
- 29.Schai PA, Thornhill TS, Scott RD. Total knee arthroplasty with the PFC system: results at a minimum of ten years and survivorship analysis. J Bone Joint Surg Br. 1998;80:850–858. [DOI] [PubMed]
- 30.Schurman DJ, Parker JN, Orstein D. Total condylar knee replacement. J Bone Joint Surg Am. 1985;67:1006–1010. [PubMed]
- 31.Scott RD. Prosthetic placement of the patellofemoral joint. Orthop Clin North Am. 1979;10:129–137. [PubMed]
- 32.Scuderi GR, Scuderi DM. Patellar fragmentation. Am J Knee Surg. 1994;7:125–129.
- 33.Yoshii I, Whiteside LA, Anouchi YS. The effect of patellar button placement and femoral component design on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1992;275:211–219. [PubMed]