Abstract
With substantial interest devoted to improving knee flexion after TKA, it is important to document the relationship between high range of motion and patient-rated outcomes shown. We therefore asked whether single-design high-flexion mobile-bearing posterior-stabilized TKA resulted in: (1) improved knee function; (2) satisfying subjective results; (3) participation recreational and sporting activities; and (4) function correlated to the final range of motion. We prospectively followed 445 consecutive patients having 516 TKAs from September 2000 to January 2005. The same high-flexion posterior-stabilized mobile-bearing implant was used in all patients. Mean patient age was 71 ± 8 years and mean body mass index was 28 ± 4 kg/m2. The minimum clinical followup was 2 years (mean, 3 years; range, 2–4 years). The postoperative range of knee flexion was 128° ± 4° and the mean Knee Society function and knee scores were 91 ± 6 and 96 ± 3, respectively. Eighty-two percent of patients were involved in sporting activities and 86% returned to their previous level of activity. These data confirm that high postoperative range of knee flexion improve patient-rated outcomes.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA provides functional improvement and pain relief for most patients with advanced knee osteoarthritis [3, 6, 11, 34]. Previous studies analyzing the patient-reported activity level after TKA suggest a high percentage participate in sporting activity [6, 10, 11, 14, 22]. Huch et al. [14] reported 34% of patients engaged in sporting activity 5 years after the surgery. Dahm et al. [6] reported 74% of patients engaged in activity at a mean of 5.7 years after arthroplasty. To take into account these changes in patient demographics and demands toward functional activities, new prosthesis designs have been developed [4, 13, 16].
A number of authors advocate mobile-bearing TKA designs for younger or higher-demand patients owing to their potential to reduce polyethylene wear and restore more normal kinematics [1, 4, 7–9, 13, 16]. These active patients may also require greater ranges of knee flexion to perform their activities [1, 13, 23]. Achieving deep knee flexion with standard TKA may increase the risk of failure by transferring the load onto the posterior aspect of the tibial insert up to six times the body weight in vertical direction and up to three times the body weight in posterior direction as reported in previous studies [1, 13, 23, 30].
To limit potential drawbacks of deep flexion such as excessive load on the tibial insert or TKA dislocation in case of posterior-stabilized implants, high-flexion posterior-stabilized mobile-bearing TKAs have been designed to provide more normal knee kinematics and improve range of knee flexion [1, 7, 8]. In a previous in vivo 3-D fluoroscopic study, we demonstrated this type of design can replicate healthy knee motion and restore normal knee kinematics without increasing the load on the posterior aspect of the knee [7]. However, the theoretical advantages of these design changes must be clinically confirmed. Furthermore, the relationship between high range of motion and patient-rated outcomes improvement must be shown.
We therefore asked whether high-flexion mobile-bearing posterior-stabilized TKA resulted in: (1) improved knee function; (2) satisfying subjective results as measured by the Knee Osteoarthritis Outcomes scores; (3) participation recreational and sporting activities as measured by the University of California–Los Angeles score; and (4) function correlated to the final range of motion.
Materials and Methods
We prospectively followed 455 consecutive patients who underwent 516 primary high-flexion mobile-bearing posterior-stabilized TKAs by one surgeon (JNA) between 2001 and 2005. The inclusion criteria were: primary TKA, osteoarthritis or rheumatoid arthritis of the knee, functional collateral ligament according to the preoperative clinical exam, and varus or valgus deformity lower than 25° measured on the preoperative full-limb radiographs. The exclusion criteria were: lack of followup, mental limitation and inability to fill out the auto questionnaire, significant neurological or musculoskeletal disorders or disease that may interfere with normal gait or weight bearing, any congenital, developmental, or other bone disease or previous hip surgery that may, in the surgeon’s judgment, interfere with TKA survival or success. The clinical evaluation was performed between January 2004 and February 2007 by two independent observers (SP, AA), including the evaluation of patient range of knee flexion and the classic items to complete the Knee Society score [15]. At the same time, patients were also asked to complete a specific survey, including the KOOS [24, 29], the UCLA score [5, 6], and specific questions concerning their recreational or sporting activities. All patients had a minimum clinical followup of 2 years (mean, 3 years; range, 2-4 years). Local ethical committee approval was obtained.
There were 299 women (67%) and 146 men (33%) in the series (256 right knees, 260 left knees). The procedure was bilateral for 70 patients (16%) and unilateral for 375 patients (84%). The mean age of the patients at the time of surgery was 71.6 ± 8 years (range, 22–96 years). The mean body mass index of the patients was 28.3 ± 4.6 kg/m2 (range, 16–44 kg/m2). The etiology was primary osteoarthritis for 474 knees (92%), rheumatoid arthritis for 11 knees (2%), and another cause (posttraumatic, avascular osteonecrosis, systemic disease) for 31 knees (6%). The mean delay before surgery was 39 ± 30 months. For 387 (75%), the preoperative alignment was in varus. In this group, the mean preoperative alignment was 171.4° ± 7° (range, 164°–179°). For 129 (25%) knees, the preoperative alignment was in valgus. In this group, the mean preoperative alignment was 188.4° ± 8° (range, 181°–202°). Concerning the activity level at the time of surgery, 173 (34%) patients were inactive, 274 (54%) were limited in their activities of daily living, 46 (9%) were still engaged in labor or sporting activities, and the activity level was unknown for 14 (3%) patients. Six patients (six knees) died before the time of evaluation; two knees had a two-stage implant revision for septic loosening at 11 and 15 months. At the time of followup, five patients (five knees) were unable to fully comprehend and complete the subjective survey and were therefore excluded and 20 patients (20 knees) were lost to followup or unable to complete the clinical evaluation. Four patients (four knees) who underwent a revision without implant exchange for postoperative stiffness (two cases) or effusion (two cases) were included in the final evaluation. Thus, we were able to analyze data for 412 patients (483 knees).
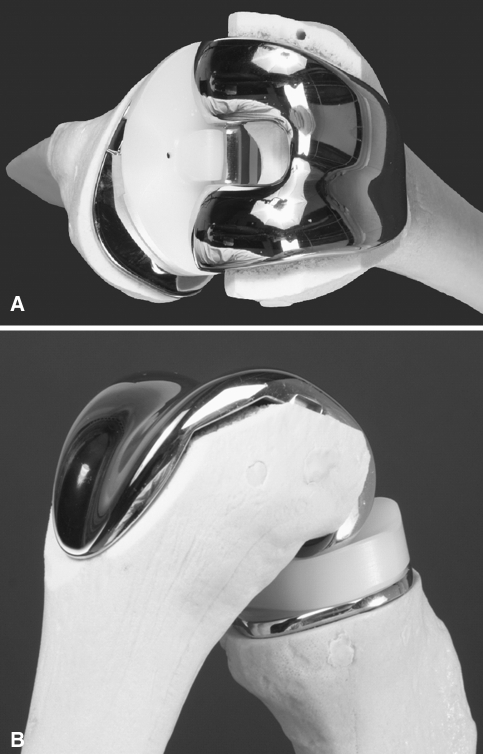
All procedures were performed by the senior author (JNA) using a cemented high-flexion mobile-bearing posterior-stabilized TKA (LPS Flex Mobile; Zimmer, Warsaw, IN) (Fig. 1) [1, 7]. All cases were performed through a standard medial parapatellar approach, all components were cemented, and the patella was systematically resurfaced. The thickness of the polyethylene liner ranged from 10 mm to 16 mm. An immediate full-weight-bearing rehabilitation protocol was used for all patients. All patients received routine prophylaxis with low-molecular-weight heparin postoperatively for 21 days.
Fig. 1A–B.
(A) Superior view of the implant on bone models shows the mobile tibial insert. (B) Posterolateral view of the implant on bone models shows the potential range of knee flexion.
We evaluated all patients clinically preoperatively, 3 months postoperatively, at 1 year, and the full study evaluation between 2 and 4 years of followup. A clinical evaluation (without knowing the results of the subjective questionnaire) of all patients was performed by two independent observers (SP, AA) using the Knee Society knee score [15]. The measure of the range of knee flexion was performed using a two-arm goniometer [17].
The patient-reported outcomes concerning the functional subjective postoperative evaluation was performed using the French version of the KOOS [24]. The KOOS is a self-administered knee-related quality-of-life questionnaire corresponding to a validated and improved WOMAC [24, 29]. The KOOS includes five dimensions scored separately: pain (nine items), symptoms (seven items), activities of daily life function (17 items), sporting and recreation function (five items), and quality of life (four items) [24, 29]. Because it is desirable to analyze and interpret the five dimensions separately, an aggregate score was not calculated [29]. All items are scored from 0 to 4, and each of the five scores is calculated as the sum of the items included as performed for the WOMAC osteoarthritis index [2, 29]. Scores are then transformed using free calculation software available online (www.koos.nu) to a 0 to 100 scale with zero representing extreme knee problems and 100 representing no knee problems [24, 29].
We evaluated the patient level of activity using the UCLA score [5, 6]. The UCLA score is a self-administered questionnaire in which the patient is asked to indicate on a 10-point scale (from 0, completely inactive to 10, regularly practice high-impact sports) his or her level of activity [5, 6]. We also asked patients to answer questions such as (1) time to return to sports or recreational activities after surgery (number of days), (2) type of sport most frequently performed, the frequency of the activity (more than twice a week, once a week, twice a month, less than twice a month), (3) the final level of return to the previous activity (same level, better, lower); and (4) patient perception of the limitation related to the knee during these activities (no, slight, major limitation).
We described patient demographics using means and standard deviations or medians and ranges for continuous variables and counts (percent) for categorical variables. We compared pre- and postoperative mean Knee Society knee and function score and the range of knee motion using a paired t-test [27]. We described the results of the KOOS score using means and standard deviation. As the sample was large and the distribution normal, the results of the Knee Society score and of the KOOS score were analyzed as parametric scores [27]. To determine whether knees with full flexion activities had a better KOOS, we compared a group with a postoperative flexion equal or higher than 125° to a group with a postoperative flexion lower than 125° using a two-sample t-test [27]. The activity levels and the characteristics of the sport practiced were described using means and standard deviations. We investigated the relationship between the subjective patient-rated outcomes (KOOS) and the postoperative range of knee flexion and the Knee Society knee scores using a multivariable linear regression [27]. To adjust the effects of confounding factors, we analyzed first the relationship between the KOOS results for its association with age, gender, body mass index, preoperative and postoperative range of knee flexion and pre- and postoperative Knee Society knee score using a univariable linear regression analysis [27]. For those factors showing differences or statistical tendency (p < 0.1), we adjusted the relationship using a multivariable linear regression analysis [26]. We performed statistical analysis using SPSS software (version 12; Chicago, IL).
Results
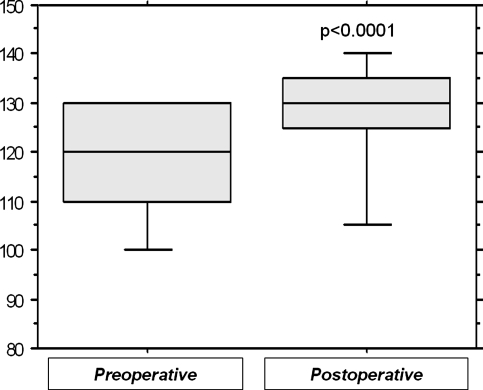
The Knee Society knee and function scores improved at last followup (Table 1). Mean active knee flexion improved (p < 0.0001) from 117° ± 13° (range, 80°–140°) preoperatively to 128° ± 4° (range, 85°–155°) at the time of the clinical evaluation (Fig. 2).
Table 1.
Pre- and postoperative values of the knee and function Knee Society scores
| Knee Society score | Preoperative score | Postoperative score | p value |
|---|---|---|---|
| Knee score | 55 ± 7 (range, 10–70) | 96 ± 3 (range, 65–100) | < 0.001 |
| Function score | 38 ± 12 (range, 5–65) | 91 ± 6 (range, 55–100) | < 0.001 |
All values are mean ± standard deviation.
Fig. 2.
The significant postoperative improvement of the range of knee flexion is shown. The boundaries of the boxes indicate the 25th and 75th percentiles and the black lines within the boxes mark the mean values. The whiskers above and below the boxes indicate the 90th and 10th percentiles.
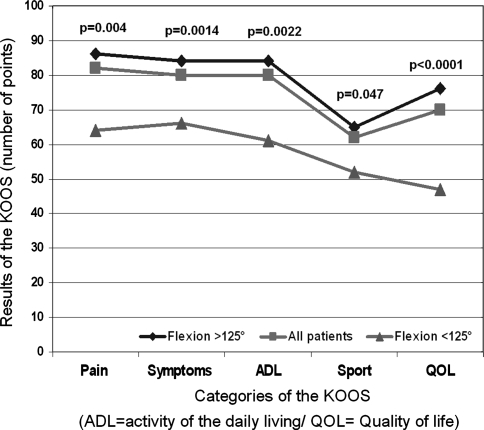
The results of the KOOS were significantly better in the group with a flexion greater than 125° for all the categories of the KOOS (pain, p = 0.004; symptoms, p = 0.0014; activity daily living, p = 0.0022; sport, p = 0.047; quality of life, p < 0.0001) (Fig. 3). The mean KOOS values at the time of the evaluation were 82 ± 16 (range, 21–100) for the pain category, 80 ± 15 (range, 27–100) for the symptoms category, 79 ± 20 (range, 21–100) for the activities of daily living category, 62 ± 32 (range, 0–100) for the sport category, and 71 ± 28 (range, 0–100) for the quality-of-life category.
Fig. 3.
Substantially better results of patient-rated outcomes were observed in the different categories of the Knee Osteoarthritis Outcomes Scores (KOOS) on a scale from 0 to 100 points for the group with a postoperative flexion higher than 125° compared to the global series and the group with a flexion lower than 125°. The intermediate curve represents the mean value of the KOOS in all series.
Three-hundred thirty-seven patients (82%) reported involvement in a sport activity at the time of the evaluation. The mean UCLA score was 6.9 ± 1.6. The delay reported by the patients before returning to their sporting activity was 6 ± 4 months. The more frequently practiced activities were walking or hiking, gardening, swimming, exercising (including cardio respiratory training), cycling, and golfing. Among the group of 337 patients involved in sport activities, 86% reported being at the same level (47 patients [14%]) or at a better level (243 patients [72%]) than before surgery and 14% (47 patients) at a lower level. Among the group of 337 patients involved in sport activities, 118 patients (35%) reported perceiving no knee-related limitation during their activities, 168 patients a slight limitation, and 51 patients (14%) a major limitation.
After adjustment for the confounding factors (Table 2), the patient-rated outcomes were correlated (p < 0.0001) with the postoperative range of knee flexion for the five categories of the KOOS.
Table 2.
Results of the correlation analysis between the postoperative range of knee flexion and the different categories of the KOOS
| Categories of the KOOS | Tested parameters | Correlation analysis | ||
|---|---|---|---|---|
| Pearson correlation coefficient | 95% confidence interval | p value | ||
| Pain | Preop flexion | 0.079 | −0.54 to 0.21 | 0.2451 |
| Postop flexion | 0.437 | 0.324 to 0.537 | < 0.0001 | |
| Preop KSS | 0.022 | −0.110 to 0.152 | 0.7459 | |
| Postop KSS | 0.403 | 0.289 to 0.506 | < 0.0001 | |
| Age | 0.007 | −0.122 to 0.136 | 0.9122 | |
| Gender | −0.079 | −0.206 to 0.050 | 0.2313 | |
| BMI | 0.025 | −0.104 to 0.154 | 0.7014 | |
| Symptoms | Preop flexion | 0.115 | 0.0917 to 0.019 | 0.244 |
| Postop flexion | 0.434 | 0.321 to 0.535 | < 0.0001 | |
| Preop KSS | 0.072 | −0.060 to 0.201 | 0.2831 | |
| Postop KSS | 0.384 | 0.269 to 0.489 | < 0.0001 | |
| Age | 0.104 | −0.025 to 0.229 | 0.1153 | |
| Gender | −0.065 | −0.192 to 0.064 | 0.3256 | |
| BMI | −0.003 | −0.132 to 0.126 | 0.9665 | |
| Activities of daily living | Preop flexion | 0.022 | −0.111 to 0.154 | 0.7465 |
| Postop flexion | 0.437 | 0.324 to 0.537 | < 0.0001 | |
| Preop KSS | −0.36 | −0.166 to 0.96 | 0.5931 | |
| Postop KSS | 0.335 | 0.216 to 0.445 | < 0.0001 | |
| Age | −0.133 | −0.258 to 0.005 | 0.0424 | |
| Gender | −0.152 | −0.276 to 0.24 | 0.0203 | |
| BMI | −0.031 | −0.160 to 0.098 | 0.6374 | |
| Sport | Preop flexion | −0.006 | −0.139 to 0.127 | 0.9310 |
| Postop flexion | 0.212 | 0.083 to 0.334 | 0.0014 | |
| Preop KSS | −0.024 | −0.155 to 0.107 | 0.7181 | |
| Postop KSS | 0.090 | −0.39 to 0.217 | 0.1703 | |
| Age | 0.041 | −0.089 to 0.169 | 0.539 | |
| Gender | −0.193 | −0.314 to −0.066 | 0.0031 | |
| BMI | −0.117 | −0.242 to 0.012 | 0.0758 | |
| Quality of life | Preop flexion | 0.036 | −0.98 to 0.168 | 0.5994 |
| Postop flexion | 0.379 | 0.261 to 0.486 | < 0.0001 | |
| Preop KSS | 0.022 | −0.109 to 0.153 | 0.7408 | |
| Postop KSS | 0.353 | 0.234 to 0.460 | < 0.0001 | |
| Age | 0.026 | −0.103 to 0.155 | 0.6901 | |
| Gender | 0.014 | −0.115 to 0.143 | 0.8279 | |
| BMI | 0.074 | −0.056 to 0.201 | 0.2639 | |
KOOS = Knee Osteoarthritis Outcomes scores; ROM = range of motion; KSS = Knee Society score.
Discussion
Achieving deep knee flexion with standard TKA may increase the load on the posterior aspect of the tibial insert and contribute to higher rate of failure [1, 13, 23]. To limit potential drawbacks of deep flexion such as excessive load on the tibial insert or TKA dislocation in case of posterior-stabilized implants, high-flexion posterior-stabilized mobile-bearing TKAs have been designed to provide more normal knee kinematics and improve range of knee flexion [1, 7, 8]. However, the theoretical advantages of these design changes have never been confirmed clinically. Furthermore, the relationship between high range of motion and the patient-rated outcomes improvement must be shown. We specifically asked whether high-flexion mobile-bearing posterior-stabilized TKA (1) improved knee function as measured by Knee Society scores and range of knee flexion; (2) resulted in satisfying subjective results; (3) allowed the patient to perform recreational and sporting activities; and (4) if the patient-rated outcomes would be directly correlated to the final range of motion after TKA as measured by the correlation coefficient between these two parameters.
One of the limitations of our study was the lack of direct prospective comparison between a group of patients implanted with a standard implant and a group implanted with a high-flexion mobile-bearing implant. We cannot say the outcomes were directly related either to the specific implant we used or the presence of a mobile-bearing rather than patient selection, general features of the design, or surgical technique. However, our goal was to evaluate the relationship between patient-rated outcomes and range of knee flexion rather than comparing this design with another one. Another limitation was the use of a single type of design which limits the extension to another type of implant of the observed correlation between the range of knee motion and the patient-rated outcomes. These outcomes may not apply to other designs or surgical techniques. However, using this study design with a single design, we were able to obtain a large sample of patients operated on by a single surgeon representative of a typical knee replacement population. This large sample population allowed us to obtain a broader distribution of the objective and subjective data. As mentioned by Padua et al. [25], this parameter is important when studying correlations between objective and subjective outcomes. A final limitation of our study may be the absence of subjective evaluation of the knee status preoperatively using the KOOS. We did not use the KOOS preoperatively because this score was not available at the time of the preoperative evaluation for a large majority of patients [24, 29]. However, in a large series we evaluated patient knee function, patient perception of their knee function, and quality of life after last-generation mobile-bearing posterior-stabilized TKA.
Our data suggest this particular high-flexion mobile-bearing TKA was associated with relief of pain and restoration of knee function as measured by the Knee Society score and by the knee-related quality-of-life score (KOOS). Furthermore, the percentage of return to a previous level of activity was high and the patient perception of their ability to return to their previous level was satisfying. Finally, we observed a correlation between the postoperative range of knee flexion and the patient-rated quality-of-life outcomes (KOOS).
Since functional results of high-flexion mobile-bearing TKA have, to our knowledge, not been reported previously in a Western population, direct comparisons of our results with previous reports in the literature are limited. The range of knee flexion we observed was greater than that reported in the literature for Western patients (mean range of flexion between 120° and 125°), but lower than that reported for Asian patients (mean range of knee flexion between 135° and 140°) [25, 35]. Direct comparison of range of knee flexion between different series in the literature appears difficult because a broad range of variation between different studied populations exists and Western populations cannot be directly compared with Asian populations [25, 35]. Also, the methods of knee flexion evaluation used in the studies are different [17, 25, 28, 35]. Manual evaluation using a two-arm goniometer is widely used even if the accuracy and the intra- and interobserver repeatability are limited [17, 28]. Objective tools to measure range of knee flexion such as electrogoniometer, fluoroscopy, or 3-D analysis in the gait laboratory are available to analyze knee motion; however, these 3-D objective tools are too expensive and time-consuming to be applied to a large group of patients [17, 28]. We observed ranges of knee flexion comparable with the range of knee flexion observed in our previous fluoroscopic evaluation for the same type of implant [1, 7]. However, new portable tools, including accelerometers, gyroscopes, and magnetometers should be developed to accurately measure dynamic knee range of flexion and allow reliable comparison among the different series. Evaluation using these new portable tools during activities of daily living should be performed to define the exact patient need [12, 17, 28]. To date, data concerning the range of knee flexion required during activities of daily living in different populations are limited and further studies using these new tools will probably help to define the target for knee flexion after TKA in all populations [12].
Bullens et al. [3] reported discrepancies between patient satisfaction and surgeon satisfaction and concluded both types of evaluations should be performed. Following this advice, four studies directly compared subjective and objective results after TKA. Miner et al. [21] reported no correlation between the results of the WOMAC sport and the range of postoperative knee flexion measured using a two-arm goniometer. Park et al. [26] reported poor correlation between the WOMAC and the SF-36 quality-of-life questionnaire in Asian patients. Witvrouw et al. [35] reported objective assessment using an objective measurement tool (DynaPort knee test) did not predict the WOMAC score. Padua et al. [25], in a study of Caucasian patients, demonstrated range of knee motion after TKA was correlated with patient perception of outcomes. We also found range of knee motion correlated with patient perception of outcomes. The KOOS has been more complete than the WOMAC to evaluate functional results, more adapted for younger patients, and more specific than the SF-36 to evaluate the patient’s quality of life after TKA [18, 19, 24, 29]. The differences in the scores used in our series may also explain the discrepancies with previous studies. Furthermore, in our series, 82% of patients reported being involved in sports or recreational activities. This point was not reported in the previously mentioned series and should be included in the description of the studied population. Weiss et al. [33] asked what functional activities were important to patients with total knee replacement. We observed similar data on sport and recreational activities to those reported by Weiss et al. [33], showing knee arthroplasty successfully restores a considerable degree of function during recreational and sport activities. Our results were also consistent with those reported by Dahm et al. [6]. Patient expectations before surgery have been previously evaluated, but data concerning patient expectations and need after TKA remain limited and require further evaluations in all concerned populations, particularly regarding sport and recreational activities [20]. To do so, complementary approaches using specific patient perception scores, activity scores, and objective range of motion measures during activities of daily living with accurate modern 3-D portable objective tools during different tasks of daily living should be performed.
Our evaluation of functional activity is consistent with data from in-vivo kinematic studies [1, 7]. These studies reported consistent posterior femoral rollback and high weightbearing range of motion for patients with high objective knee scores [1, 7]. We observed correlations among objective results, particularly considering range of knee flexion and patient-rated results in a group with a high percentage of patients involved in recreational or sport activities. The patients were also satisfied with their replaced knee during these activities. These data seem to confirm that high postoperative range of knee flexion improves patient satisfaction. This point may justify the use of designs combining posterior-stabilized high-flexion and mobile-bearing total knee arthroplasties to perform activities requiring high knee flexion without increasing the risk of dislocation or the load on the posterior aspect of the tibial insert. The results from these sorts of design changes should be confirmed in future mid-term and long-term studies.
Acknowledgments
We thank Sandra Coudreuse, MD, for the data collection and Vanessa Pauly, MS, for the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Argenson JN, Komistek RD, Mahfouz M, Walker SA, Aubaniac JM, Dennis DA. A high flexion total knee arthroplasty design replicates healthy knee motion. Clin Orthop Relat Res. 2004; 428:174–179. [DOI] [PubMed]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed]
- 3.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16:740–747. [DOI] [PubMed]
- 4.Callaghan JJ. Mobile-bearing knee replacement: clinical results: a review of the literature. Clin Orthop Relat Res. 2001;392:221–225. [DOI] [PubMed]
- 5.Dahm DL, Barnes SA, Harrington JR, Berry DJ. Patient reported activity after revision total knee arthroplasty. J Arthroplasty. 2007;22:106–110. [DOI] [PubMed]
- 6.Dahm DL, Barnes SA, Harrington JR, Sayeed SA, Berry DJ. Patient Reported Activity Level Following Total Knee Arthroplasty. J Arthroplasty. 2008;23:401–407. [DOI] [PubMed]
- 7.Dennis D, Komistek R, Scuderi G, Argenson JN, Insall J, Mahfouz M, Aubaniac JM, Haas B. In vivo three-dimensional determination of kinematics for subjects with a normal knee or a unicompartmental or total knee replacement. J Bone Joint Surg Am. 2001;83-A (Suppl 2 Pt 2):104–115. [DOI] [PubMed]
- 8.Dennis DA, Komistek RD. Kinematics of mobile-bearing total knee arthroplasty. Instr Course Lect. 2005;54:207–220. [PubMed]
- 9.Dennis DA, Komistek RD, Mahfouz MR, Outten JT, Sharma A. Mobile-bearing total knee arthroplasty: do the polyethylene bearings rotate? Clin Orthop Relat Res. 2005;440:88–95. [DOI] [PubMed]
- 10.Dennis DA, Komistek RD, Scuderi GR, Zingde S. Factors Affecting Flexion after Total Knee Arthroplasty. Clin Orthop Relat Res. 2007;464:53–60. [DOI] [PubMed]
- 11.Healy WL, Iorio R, Lemos MJ. Athletic activity after total knee arthroplasty. Clin Orthop Relat Res. 2000;380:65–71. [DOI] [PubMed]
- 12.Hemmerich A, Brown H, Smith S, Marthandam SS, Wyss UP. Hip, knee, and ankle kinematics of high range of motion activities of daily living. J Orthop Res. 2006;24:770–781. [DOI] [PubMed]
- 13.Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty: a minimum of 2 years of follow-up. J Arthroplasty. 2005;20:674–679. [DOI] [PubMed]
- 14.Huch K, Muller KA, Sturmer T, Brenner H, Puhl W, Gunther KP. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64:1715–1720. [DOI] [PMC free article] [PubMed]
- 15.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 16.Jones RE, Huo MH. Rotating platform knees: an emerging clinical standard: in the affirmative. J Arthroplasty. 2006;21:33–36. [DOI] [PubMed]
- 17.Lea RD, Gerhardt JJ. Range-of-motion measurements. J Bone Joint Surg Am. 1995;77:784–798. [DOI] [PubMed]
- 18.Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86-A:2179–2186. [DOI] [PubMed]
- 19.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB. Validity, responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am. 2001;83-A:1856–1864. [DOI] [PubMed]
- 20.Lingard EA, Sledge CB, Learmonth ID, Group KO. Patients expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am. 2006;88:1201–1207. [DOI] [PubMed]
- 21.Miner AL, Lingard EA, Wright EA, Sledge CB, Katz JN. Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty. 2003;18:286–294. [DOI] [PubMed]
- 22.Mont MA, Marker DR, Seyler TM, Gordon N, Hungerford DS, Jones LC. Knee Arthroplasties Have Similar Results in High-and Low-activity Patients. Clin Orthop Relat Res. 2007;460:165–173. [DOI] [PubMed]
- 23.Nagura T, Otani T, Suda Y, Matsumoto H, Toyama Y. Is high flexion following total knee arthroplasty safe?: evaluation of knee joint loads in the patients during maximal flexion. J Arthroplasty. 2005;20:647–651. [DOI] [PubMed]
- 24.Ornetti P, Parratte S, Gossec L, Tavernier C, Argenson JN, Roos EM, Guillemin F, Maillefert JF. Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthritis Cartilage. 2007;16:423–424. [DOI] [PubMed]
- 25.Padua R, Ceccarelli E, Bondi R, Campi A, Padua L. Range of Motion Correlates with Patient Perception of TKA Outcome. Clin Orthop Relat Res. 2007;460:174–177. [DOI] [PubMed]
- 26.Park KK, Chang CB, Kang YG, Seong SC, Kim TK. Correlation of maximum flexion with clinical outcome after total knee replacement in Asian patients. J Bone Joint Surg Br. 2007;89:604–608. [DOI] [PubMed]
- 27.Petrie A. Statistics in orthopaedic papers. J Bone Joint Surg Br. 2006;88:1121–1136. [DOI] [PubMed]
- 28.Piriyaprasarth P, Morris ME. Psychometric properties of measurement tools for quantifying knee joint position and movement: a systematic review. Knee. 2007;14:2–8. [DOI] [PubMed]
- 29.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed]
- 30.Sharma A, Komistek RD, Scuderi GR, Cates HE Jr. High-flexion TKA designs: what are their in vivo contact mechanics? Clin Orthop Relat Res. 2007; 464:117–126. [DOI] [PubMed]
- 31.Victor J, Bellemans J. Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res. 2006;452:53–58. [DOI] [PubMed]
- 32.Victor J, Ries M, Bellemans J, Robb WM, Van Hellemondt G. High-flexion, motion-guided total knee arthroplasty: who benefits the most? Orthopedics. 2007;30:77–79. [PubMed]
- 33.Weiss JM, Noble PC, Conditt MA, Kohl HW, Roberts S, Cook KF, Gordon MJ, Mathis KB. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;404:172–188. [DOI] [PubMed]
- 34.Wells VM, Hearn TC, McCaul KA, Anderton SM, Wigg AE, Graves SE. Changing incidence of primary total hip arthroplasty and total knee arthroplasty for primary osteoarthritis. J Arthroplasty. 2002;17:267–273. [DOI] [PubMed]
- 35.Witvrouw E, Victor J, Bellemans J, Rock B, Van Lummel R, Van Der Slikke R, Verdonk R. A correlation study of objective functionality and WOMAC in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2002;10:347–351. [DOI] [PubMed]