Abstract
Complementary and alternative medicine approaches to treatment for tension-type headache are increasingly popular among patients, but evidence supporting its efficacy is limited. The objective of this study was to assess short term changes on primary and secondary headache pain measures in patients with tension-type headache (TTH) receiving a structured massage therapy program with a focus on myofascial trigger point therapy. Participants were enrolled in an open label trial using a baseline control with four 3-week phases: baseline, massage (two 3-week phases) and follow-up. Twice weekly, 45-minute massage sessions commenced following the baseline phase. A daily headache diary was maintained throughout the study in which participants recorded headache incidence, intensity, and duration. The Headache Disability Index was administered upon study entry and at 3-week intervals thereafter. 18 subjects were enrolled with 16 completing all headache diary, evaluation, and massage assignments. Study participants reported a median of 7.5 years with TTH. Headache frequency decreased from 4.7±0.7 episodes per week during baseline to 3.7±0.9 during treatment period 2 (P<0.001); reduction was also noted during the follow-up phase (3.2±1.0). Secondary measures of headache also decreased across the study phases with headache intensity decreasing by 30% (P<0.01) and headache duration from 4.0±1.3 to 2.8±0.5 hours (P<0.05). A corresponding improvement in Headache Disability Index was found with massage (P<0.001). This pilot study provides preliminary evidence for reduction in headache pain and disability with massage therapy that targets myofascial trigger points, suggesting the need for more rigorously controlled studies.
Keywords: Complementary and Alternative Medicine, Headache Disability Index, Manual Therapy, Myofasical Pain, Myofascial Trigger Points
Tension-type headache (TTH) is the most prevalent of the headache disorders, yet research into specific treatments is inadequate and lags other headache classifications such as migraine1. The lack of suitable conventional medical options may explain the popularity of non-pharmaceutical therapies for TTH. A recent report noted that 40% of patients visiting a headache clinic use one or more complementary and alternative medicine modalities to reduce pain associated with chronic TTH2. Manual therapies, including chiropractic medicine and massage therapy, receive much attention from the lay public as alternative treatments for TTH, which suggests an assumed patient benefit despite limited research evidence2.
Self-massage of cranial musculature is regularly employed by 25% of TTH patients as a quick means to reduce pain, although the immediate benefit is reported to be of short duration3. In clinical trials, two studies utilizing massage as part of a physical therapy program for treating tension-type headache note a significant reduction in headache frequency4,5. More directly related to massage, Puustjarvi et al report that women with chronic tension-type headache receiving massage experience a reduction in the number of days with pain, even at a six month follow-up6. More recently, a case series employing highly trained massage therapists reported reduction in headache frequency by 50% after as few as two 30-minute massage sessions7.
The 2004 International Classification of Headache Disorders published by the International Headache Society (IHS) indicates a muscular involvement for some forms of tension-type headache (Subclasses 2.2.1 and 2.3.1)8. In addition, physiological abnormalities, such as increased tenderness and greater incidence of myofascial trigger points in skeletal muscle are commonly reported for those with TTH9,10,11,12,13. Likewise, physical abnormalities associated with the musculature are also noted and include a forward head posture and reduced cervical muscle strength and endurance12,14,15,16. The implication of a muscular involvement in TTH is further supported by the finding that botulinum toxin type A injected at anatomically defined sites improved headache intensity and headache free days in chronic TTH subjects17,18. Therefore, it is not surprising that treatments to alleviate muscle tension are of interest as a means for reducing headache pain.
While manual therapies for the treatment of tension-type headache are frequently used by the general public2, skepticism from the medical community exists due to lack of scientific support19. The objective of this study was to evaluate a specific massage therapy treatment directed at cervical and cranial musculature on primary and secondary measures of headache as well as a measure of disability associated with headache.
Methods
Study design
A cohort of subjects with TTH received 12 × 45-minute massage sessions over six weeks. Massage was directed toward soft tissues of the cervical and cranial regions with a focus on alleviating myofascial trigger point activity, connective tissue viscosity, and muscle hypertonicity. A 3-week baseline period preceded six weeks of massage and a 3-week follow-up period. Primary (frequency) and secondary (peak intensity, duration) measures of headache, as well as a measure of disability (Headache Disability Index) were monitored in accord with recently published guidelines20. Subjects recorded headache measures in a daily headache diary; the Headache Disability Index (HDI) was administered at 3-week intervals. The Institutional Review Board at The Boulder College of Massage Therapy approved this study; all subjects signed informed consent prior to study enrollment.
Subjects
Selection criteria conformed to the 2004 IHS guidelines for episodic or chronic TTH: experiencing regular headache pain for at least the prior 6 months, each headache bout lasting at least 4 hours; 21–65 years of age; and 1 or fewer migraine headaches per month8. Subjects taking anti-psychotic or anti-depressant medications were excluded from the study. Subjects were recruited from fliers placed in local medical physician offices and advertisements in a local newspaper. Enrollment criteria were verified by interview, review of headache diary and confirmatory diagnosis by the subjects' medical physician. A total of 18 subjects met selection criteria and agreed to participate in the study. Two participants were subsequently removed from the study due to either involvement in a motor vehicle accident or an insufficiently maintained headache diary.
Massage therapists
Subjects were randomly assigned to one of 6 massage therapists for the duration of the treatment phase. The continuity of therapist was selected because clients typically receive treatment from the same practitioner and familiarity with the practitioner reduces associated anxiety. Massage therapists employed in this study had an average of 6 years of professional massage experience, 5 had taught massage techniques at a local massage school, and all therapists underwent at least 6 hours of training specific to the protocol prior to study onset. To isolate the effect of the massage procedure from therapist-subject camaraderie, therapists and subjects were directed to minimize conversation and to not discuss headache history; communication between subject and therapist was limited to current treatment (i.e. depth of massage pressure, presence of referred pain, and overall patient comfort). The massage therapists were not informed regarding participant progression with headache status throughout the study.
Massage protocol
Two 45-minute massage sessions were conducted each week over a 6-week period. Each massage session was separated by at least 48 hours. The first 15 minutes of each massage session involved palmar gliding strokes to warm-up the tissues of the back, shoulders, chest, and neck. Over the next 15 minutes, up to 6 active myofascial trigger points were palpated and treated using myofascial trigger point release techniques as previously published7,21,22. Skeletal muscles addressed included the upper trapezius, sternocleidomastoid, suboccipital, and splenius capitis. The final 15 minutes of each massage session consisted of 5 minutes of post-isometric relaxation directed at the right and left lateral cervical flexion, 5 minutes of circular or cross fiber friction on the masseter, temporalis, and occipital-frontalis muscles, and 5 minutes of gentle effleurage and petrissage strokes to the neck and shoulders24.
Headache diary
Each subject maintained a daily headache diary, which was completed immediately before retiring for sleep25. Subjects recorded the presence of a tension-type headache each day. If a headache occurred, the duration was recorded in hours and minutes, and the peak headache intensity was recorded on a 100mm visual analogue scale where 0 indicated no headache pain and 100 indicated maximal headache pain26. Diaries were collected at 3-week intervals.
Headache disability index
To quantify the impact TTH has on daily living the HDI was administered. The HDI consists of 25 items each requiring a “yes” (4 points) “sometimes” (2 points) or “no” (0 points) response based on items derived empirically from case history responses from subjects with headache27. This index has been reported in the headache literature as a criterion standard measure for disability in patients with headache20. A total score change of at least 29 points is necessary for effects to be considered clinically significant27. Emotional and functional subscales are contained within the inventory. The HDI has good internal consistency (0.89), robust long-term test-re-test reliability (0.83), and good construct validity27. The HDI was administered 5 times at 3-week intervals to each participant, including twice during the baseline phase, after 3 and 6 weeks of massage therapy and at a 3-week follow-up. To avoid a confounding immediate effect of massage, the HDI was administered either prior to or on a day separate from massage treatment.
Statistics
The study was divided into four 3-week phases: baseline, massage (two 3-week phases), and follow-up phase. Headache frequency was reported as the weekly average over each study phase. The average peak headache intensity, duration of headache, and the HDI were presented for each phase. Statistical analysis was conducted using StatView for Windows (SAS Institute) and statistical significance was accepted at p<0.05. Unless otherwise noted, data were presented as the mean ± 95% confidence interval (CI) and were assessed by repeated measures analysis of variance (RM-ANOVA). Post hoc analysis was conducted using paired t-tests with Bonferroni correction; due to the pilot nature of the study only comparisons to baseline values were conducted, thus three comparisons were performed for each analysis and adjustments required a p value of <0.017 for significance.
Results
Demographic data
The mean (±SD) subject age was 43.8±9.3 (range 28–56) and subjects had been experiencing TTH for a median of 7.5 years (range 0.5–40). Twelve females and 4 males completed the study. In the six months prior to study enrollment, 4 subjects reported having received no massage and 12 reported at least 1 massage from a professional massage therapist.
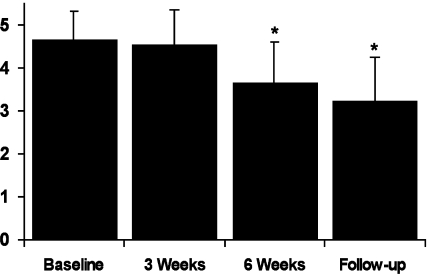
Headache frequency
Subjects reported an average of 4.7±0.7 days per week with headache during the 3-week baseline period (Figure 1). A significant reduction in headache incidence was detected across time (F(3,15) = 8.95, p <0.001) with both the second massage phase (3.7±0.9 headaches/week) and the 3-week follow-up (3.2±1.0 headaches/week) periods reporting significantly fewer headaches compared to baseline (p<0.01). The highest 1-week headache incidence was recorded during the first week of massage treatment (5.0) and the lowest single week average occurred during both the last week of massage and second week of the follow-up phase with an average of 3.1 episodes.
Figure 1.
Headache incidence was recorded in a daily diary. The mean number of days that headache was experienced per week during the respective study phase is presented (±95% CI). Headache incidence decreased over the course of the study (P<0.001). * denotes P< 0.01 compared to Baseline.
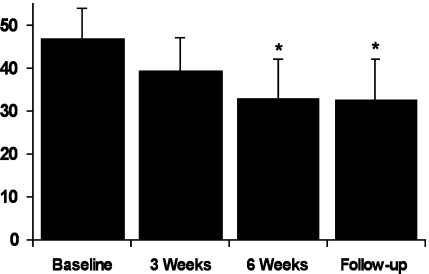
Headache intensity
The average peak pain intensity for each headache bout was recorded on a visual analog scale (0–100 mm) and is displayed in Figure 2. Headache pain during the baseline period was of moderate intensity (46.9±6.9 mm) but decreased by 30% over the course of the study (F(3,45) = 6.07, p=0.001) reaching a low of 32.8±9.4 mm during the follow-up phase. Post hoc analysis indicated a significant reduction in peak headache pain intensity from baseline during the second massage phase 2 (p=0.002) as well as the follow-up (p=0.004).
Figure 2.
Headache intensity. The peak inten- sity of each headache bout was recorded in a headache diary on a visual analogue scale (VAS) with a range from 0-100 mm. Headache intensity in each respective phase was averaged and is presented (±95% CI). Headache intensity decreased over the study time frame (P<.001). * denotes P< 0.01 compared to Baseline.
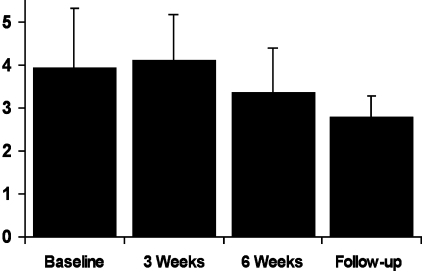
Headache duration
The duration of a headache event for each study phase is presented in Figure 3. The mean headache duration during the baseline phase was 4.0±1.3 hours, which decreased to 3.4±1.0 hours during the second massage phase and to 2.8±0.5 hours for the follow-up phase (F(3, 45) = 3.17, p<0.05).
Figure 3.
Headache Duration. The duration of each headache was recorded in a headache diary. The average duration of headache during each respective phase is presented (±95% CI). A significant change across time was noted (P<0.05).
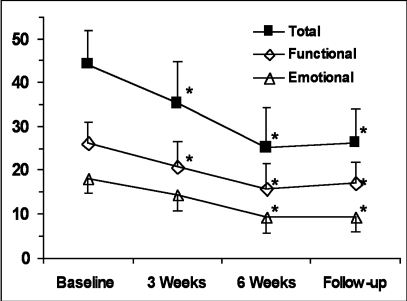
Headache disability index
Subjects were administered the HDI questionnaire at the beginning and end of the baseline phase and at 3-week intervals for the duration of the study (Figure 4). There was no statistical difference in subject scores between the two baseline tests (p=0.94) thus each was subsequently pooled. A significant effect across time was noted (F(3,45) = 14.1, p<0.001) with the baseline scores averaging 44.2 and decreased to 25.1 at the end of massage treatment. On average, 11 to 22 questions on the HDI evoked a response with subjects reporting improvement on between 5 to 10 of the 25 questions. Both the HDI functional and emotional subscales improved significantly over the course of the study, however, significant improvement in the functional subscale was detected on the test administered after three weeks of massage (P<0.01) whereas the emotional component did not reach statistical significance until after the sixth week of massage (P<0.01).
Figure 4.
Headache Disability Index. Mean scores for the Total as well as Functional and Emotional subscales of the HDI are presented (±95% CI). The test was administered five times at three-week intervals, including twice during Baseline. No statistical difference was detected between Baseline scores (P=0.94) and were subsequently pooled. A significant change across time was noted for Total score and each subscale (P<0.001). HDI denotes Headache Disability Index; * denotes P<0.01 from respective Baseline value.
Secondary analysis
Thirteen subjects met IHS criteria for chronic tension-type headache and 3 met the criteria for episodic tension-type headache8. Descriptive statistics for headache parameters (Table 1) and the HDI (Table 2) are presented for qualitative comparison of these subgroups. To minimize the risk of Type I or II errors we chose not to perform statistical analysis on these populations; statistical analysis is provided only for the complete set of 16 subjects.
TABLE 1.
Descriptive statistics for headache parameters of chronic (n=13) and episodic (n=3) tension-type headache subjects.
| Group | Baseline | 3 Weeks | 6 Weeks | Follow-up | |
|---|---|---|---|---|---|
| HA Frequency (Days/Week) | CTTH | 5.33 ± 0.54 | 4.93 ± 0.75 | 4.28 ± 0.88 | 3.67 ± 1.18 |
| ETTH | 2.57 ± 0.85 | 2.57 ± 1.71 | 1.00 ± 0.33 | 1.33 ± 0.33 | |
| HA Intensity (VAS 0-100) | CTTH | 43.2 ± 6.30 | 38.7 ± 9.18 | 31.9 ± 9.39 | 32.8 ± 10.3 |
| ETTH | 60.3 ± 22.5 | 41.2 ± 20.0 | 43.1 ± 28.4 | 40.6 ± 23.2 | |
| HA Duration (h) | CTTH | 3.58 ± 1.10 | 3.96 ± 1.01 | 2.85 ± 0.70 | 2.70 ± 0.48 |
| ETTH | 5.73 ± 5.38 | 4.77 ± 3.80 | 5.37 ± 3.93 | 2.90 ± 1.65 | |
CTTH chronic tension-type headache; ETTH episodic tension-type headache.
TABLE 2.
Descriptive statistics for the Headache Disability Index of chronic (n=13) and episodic (n=3) tension-type headache subjects.
| Group | Baseline | 3 Weeks | 6 Weeks | Follow-up | |
|---|---|---|---|---|---|
| HDI–Total | CTTH | 43.6 ± 7.66 | 34.0 ± 9.55 | 23.3 ± 10.6 | 26.4 ± 9.20 |
| ETTH | 47.0 ± 29.1 | 40.6 ± 34.6 | 33.4 ± 14.6 | 26.6 ± 10.2 | |
| HDI–Emotional | CTTH | 17.8 ± 3.58 | 14.3 ± 4.19 | 9.08 ± 4.32 | 9.85 ± 4.18 |
| ETTH | 19.0 ± 13.1 | 15.3 ± 12.9 | 10.7 ± 7.28 | 7.33 ± 3.46 | |
| HDI–Functional | CTTH | 25.8 ± 4.80 | 19.7 ± 5.66 | 14.2 ± 6.57 | 16.5 ± 5.34 |
| ETTH | 28.0 ± 16.1 | 25.3 ± 21.8 | 22.7 ± 7.96 | 19.3 ± 6.92 | |
HDI Headache Disability Index.
CTTH chronic tension-type headache; ETTH episodic tension-type headache.
Discussion
Primary and secondary measures of headache were reduced from baseline for TTH subjects receiving a six-week course of 12 massage sessions that focused on myofascial trigger point therapy and was administered by highly trained therapists. Headache-free days increased by an average of 1 day per week during the second massage phase and 1.5 days per week during the follow-up phase. Furthermore, a 30% decrease in the peak intensity and a 1.2 hour decrease (to 2.8 hours) in the duration of each successive headache incidence was observed. Significant group effects were not apparent until the second three week period of massage therapy. Concomitant with a reduction in headache measures was a decrease in headache-specific disability as measured by the HDI. Importantly, short-term changes associated with massage persisted beyond the massage treatment period as both primary and secondary headache measures during the follow-up period were significantly lower than baseline and were comparable to the second massage period.
Pericranial muscle tenderness is greater in TTH than control or migraineurs and provides an association between peripheral tissues and headache pain28,29. Muscle tenderness remains apparent even during a headache-free period28,30. More recently, Fernandez-de-las-Penas et al have drawn attention to myofascial trigger points (MTrPs) in skeletal muscle as sites of interest in TTH31,32. An active MTrP is a tightly contracted region within a muscle that elicits pain locally (point tenderness) as well as at characteristic distant sites (referred pain), the latter of which can mimic the pain syndrome of the patient33. Therefore, the MTrP is of particular interest due to its association with local muscle tenderness and its ability to refer pain that mimics the patient complaint, thus providing a peripheral site(s) directly linked with the headache. A focus in this massage study was on reducing active MTrP activity in cervical and cranial muscles, which has been shown to be of higher presence in the upper trapezius and suboccipital muscles of TTH than control subjects11,34. The value of treating MTrPs of the muscles addressed in the present study is underscored by a recent review article, which concludes that MTrPs are a causative factor for tension-type headache and play a role in the progression from episodic to chronic headache forms35.
Multiple methods aimed at reducing MTrP activity have been previously investigated, with mechanical pressure from manual (massage) techniques commonly cited36,37,38,39. Specific to massage at the MTrP is a study conducted by Gam et al40 who report a significant decrease in the number of MTrPs in the neck and shoulders after a massage and exercise program; the addition of ultrasound to the treatment regimen did not improve results. Furthermore, manual compression applied to myofascial trigger points increases pain threshold and tolerance at the MTrP23,41. The majority of the specific massage treatment used in this study was directed at reducing active MTrPs in musculature that refer pain to the head region. Although physiological measures of the MTrP were not taken during this study, the therapists reported that MTrPs became increasingly difficult to locate and required greater pressure to elicit referred pain phenomenon following repeated massage visits, factors that suggest a reduction in its metabolic activity.
The mechanism by which a MTrP elicits pain has not been clearly identified. Shah et al found an elevation in chemicals associated with nociception such as bradykinin, substance P, and reduced pH at an active MTrP, but not a latent MTrP or healthy muscle tissue42. The presence of bradykinin in the MTrP may be an important component in the referred pain phenomenon as injection of a cocktail containing bradykinin into the tibialis anterior resulted in referred pain sensation43,44. In this regard, massage may mechanically force the muscle fiber sarcomeres at the MTrP nodule apart, thus reducing ischemia and allowing blood flow to the region, which may flush pain-inducing chemicals and allow for tissue recovery to occur36. Persistent nociceptive stimulation of the central nervous system from the periphery has been argued as a means of progression from episodic to chronic TTH11,45. Therefore, both peripheral and central mechanisms may be involved with the etiology of TTH46, which may explain some variability in the effectiveness of massage. It may be necessary to independently address both peripheral and central mechanisms to alleviate persistent tension-type headache pain.
Verbal reports from the participants strongly support a positive effect from massage on headache pain. However, the reduction, but not complete abrogation, of headache pain by massage prompts inquiry into whether a longer duration massage (e.g. 60 minute), additional massage sessions, or a less standardized massage protocol that is tailored to each specific patient would result in a greater effect. Continued improvement in headache measures across the study timeframe suggests that the effectiveness of massage was not exhausted within six weeks, thus additional massage treatments may be beneficial. It is also important to recognize that behavioral changes by the patient such as postural or nutritional adjustments, stress reduction, or breathing mechanics may be necessary to prevent reactivation of a MTrP that can perpetuate headache. Although 12 participants in this study had received professional massage in the 6 months prior to study enrollment, it is unlikely that this experience had a direct effect on treatment outcome. These massages were not headache treatment oriented and all massage was prohibited during baseline data collection. Furthermore, we did not observe significant group effects until after 3 weeks of massage treatment (6 massages), which would argue against prior treatments impacting the study findings.
It is interesting to note that headache instances increased in the week immediately following massage onset, but also continued to decrease for a period following massage cessation. Isometric muscle contraction associated with the myofascial trigger point release technique can result in over-stimulation of a MTrP and perpetuate referred pain and headache phenomenon33. The initial week of massage denotes a period where the subject becomes acquainted with the therapist and myofascial trigger point therapy techniques; subjects may be unaccustomed to pressure and appropriate sensation for optimizing this type of treatment. The first week following the massage phases may allow a recovery of the MTrPs without additional stimulation from massage, thus allowing residual pain to subside.
While statistically significant, reductions in total as well as the functional and emotional subscales for the Headache Disability Index were found. This finding should be interpreted with caution since a decrease of 19.1 units was noted in this study, yet a 29 point change has been reported as necessary for clinical change27. The relatively large change necessary for clinical significance limits the robustness of the test as subjects initially reporting moderate disability scores must virtually eliminate associated disability and those with scores below this value are limited by a basement effect20.
The comparison to a baseline standard and not a placebo control group limits the ability to assess causality of the treatment. However, selection of participants experiencing TTH for a median of 7.5 years and a 3-week baseline period argues against day-to-day fluctuations causing the observed effects. While a 4-week baseline period is optimal to avoid any fluctuations in headache due to menstrual cycles20, two-week periods have been argued as satisfactory for TTH research studies47. Potentially confounding treatments such as an exercise program, physical therapy, or chiropractic adjustments that are often co-administered with massage were not permitted in this study, thus isolating the massage treatment. Our study also employed massage therapists with extensive experience in the field and a specifically designed protocol was followed during each session. This degree of attention to the massage aspect of a treatment regimen for TTH has been insufficiently addressed in previous studies. It is hoped that this initial foray provides impetus for additional research into massage for chronic pain conditions such as TTH.
Conclusion
In this pilot study, a massage therapy treatment program, with an emphasis on reducing myofascial trigger point activity, was administered to patients meeting IHS criteria for episodic or chronic TTH. During the second three week phase of massage, reductions in primary and secondary headache measures were noted relative to a baseline-monitoring period. Importantly, the frequency of headache events decreased, but it is also notable that successive headaches experienced by study participants were of reduced intensity and duration and these reductions persisted at least 3 weeks following massage therapy. Collectively, the observed improvement in clinical headache parameters provides an intriguing look into the therapeutic effect of massage and is encouraging for placebo-controlled research in complementary and alternative treatments for TTH.
Acknowledgements
The authors would like to thank Nathan Butryn, Maria Hassett, Marjorie Johnson, Rob Killam, and Lynn St. Denis for their role as massage therapists in this study.
Footnotes
The National Headache Foundation, Chicago, Illinois provided financial support for this study.
Contributor Information
Albert Moraska, School of Nursing, University of Colorado Health Sciences Center, Aurora, CO.
Clint Chandler, Boulder College of Massage Therapy, Boulder, CO..
REFERENCES
- 1.Jensen R. Diagnosis, epidemiology, and impact of tension-type headache. Curr Pain Headache Rep. 2003;7:455–459. doi: 10.1007/s11916-003-0061-x. [DOI] [PubMed] [Google Scholar]
- 2.Rossi P, Di Lorenzo G, Faroni J, Malpezzi MG, Cesarino F, Nappi G. Use of complementary and alternative medicine by patients with chronic tension-type headache: Results of a headache clinic survey. Headache. 2006;46:622–631. doi: 10.1111/j.1526-4610.2006.00412.x. [DOI] [PubMed] [Google Scholar]
- 3.Zanchin G, Maggioni F, Granella F, Rossi P, Falco L, Manzoni GC. Self-administered pain-relieving manoeuvres in primary headaches. Cephalalgia. 2001;21:718–726. doi: 10.1046/j.1468-2982.2001.00199.x. [DOI] [PubMed] [Google Scholar]
- 4.Hammill JM, Cook TM, Rosecrance JC. Effectiveness of a physical therapy regimen in the treatment of tension-type headache. Headache. 1996;36:149–153. doi: 10.1046/j.1526-4610.1996.3603149.x. [DOI] [PubMed] [Google Scholar]
- 5.Torelli P, Jensen R, Olesen J. Physiotherapy for tension-type headache: A controlled study. Cephalalgia. 2004;24:29–36. doi: 10.1111/j.1468-2982.2004.00633.x. [DOI] [PubMed] [Google Scholar]
- 6.Puustjarvi K, Airaksinen O, Pontinen PJ. The effects of massage in patients with chronic tension headache. Acupunct Electrother Res. 1990;15:159–162. doi: 10.3727/036012990816358234. [DOI] [PubMed] [Google Scholar]
- 7.Quinn C, Chandler C, Moraska A. Massage therapy and frequency of chronic tension headaches. Am J Public Health. 2002;92:1657–1661. doi: 10.2105/ajph.92.10.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Headache Classification Subcommittee of the International Headache Society The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 9.Jensen R, Bendtsen L, Olesen J. Muscular factors are of importance in tension-type headache. Headache. 1998;38:10–17. doi: 10.1046/j.1526-4610.1998.3801010.x. [DOI] [PubMed] [Google Scholar]
- 10.Jull G, Barrett C, Magee R, Ho P. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia. 1999;19:179–185. doi: 10.1046/j.1468-2982.1999.1903179.x. [DOI] [PubMed] [Google Scholar]
- 11.Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Myofascial trigger points in the suboccipital muscles in episodic tension-type headache. Man Ther. 2006;11:225–230. doi: 10.1016/j.math.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache. 2006;46:454–460. doi: 10.1111/j.1526-4610.2006.00288.x. [DOI] [PubMed] [Google Scholar]
- 13.Rubin D. Myofascial trigger point syndromes: An approach to management. Arch Phys Med Rehabil. 1981;62:107–110. [PubMed] [Google Scholar]
- 14.Barton PM, Hayes KC. Neck flexor muscle strength, efficiency, and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch Phys Med Rehabil. 1996;77:680–687. doi: 10.1016/s0003-9993(96)90008-8. [DOI] [PubMed] [Google Scholar]
- 15.Watson DH, Trott PH. Cervical headache: An investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13:272–284. doi: 10.1046/j.1468-2982.1993.1304272.x. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Forward head posture and neck mobility in chronic tension-type headache: A blinded, controlled study. Cephalalgia. 2006;26:314–319. doi: 10.1111/j.1468-2982.2005.01042.x. [DOI] [PubMed] [Google Scholar]
- 17.Freund BJ, Schwartz M. Relief of tension-type headache symptoms in subjects with temporomandibular disorders treated with botulinum toxin-a. Headache. 2002;42:1033–1037. doi: 10.1046/j.1526-4610.2002.02234.x. [DOI] [PubMed] [Google Scholar]
- 18.Smuts JA, Baker MK, Smuts HM, Stassen J, Rossouw E, Barnard P. Prophylactic treatment of chronic tension-type headache using botulinum toxin type a. Eur J Neurol. 1999;6(suppl 4):S99–S102. [Google Scholar]
- 19.Fernandez-de-las-Penas C, Alonso-Blanco C, San-Roman J, Miangolarra-Page JC. Methodological quality of randomized controlled trials of spinal manipulation and mobilization in tension-type headache, migraine, and cervicogenic headache. J Orthop Sports Phys Ther. 2006;36:160–169. doi: 10.2519/jospt.2006.36.3.160. [DOI] [PubMed] [Google Scholar]
- 20.Andrasik F, Lipchik GL, McCrory DC, Wittrock DA. Outcome measurement in behavioral headache research: Headache parameters and psychosocial outcomes. Headache. 2005;45:429–437. doi: 10.1111/j.1526-4610.2005.05094.x. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez-de-las-Penas C, Alonso-Blanco C, Fernandez-Carnero J, Miangolarra-Page JC. The immediate effect of ischemic compression technique and transverse friction massage on tenderness of active and latent mofascial trigger points: A pilot study. J Bodywork Movement Ther. 2006;10:3–9. [Google Scholar]
- 22.Fryer G, Hodgson L. The effect of manual pressure release on myofascial trigger points in the upper trapezius muscle. J Bodywork Movement Ther. 2005;9:248–255. [Google Scholar]
- 23.Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ. Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch Phys Med Rehabil. 2002;83:1406–1414. doi: 10.1053/apmr.2002.34834. [DOI] [PubMed] [Google Scholar]
- 24.Hendrickson T. Massage for Orthopedic Conditions. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 25.Andrasik F, Holroyd KA. Reliability and concurrent validity of headache questionnaire data. Headache. 1980;20:44–46. doi: 10.1111/j.1526-4610.1980.hed2001044.x. [DOI] [PubMed] [Google Scholar]
- 26.Niere K, Jerak A. Measurement of headache frequency, intensity and duration: Comparison of patient report by questionnaire and headache diary. Physiother Res Int. 2004;9:149–156. doi: 10.1002/pri.318. [DOI] [PubMed] [Google Scholar]
- 27.Jacobson GP, Ramadan NM, Aggarwal SK, Newman CW. The Henry Ford hospital headache disability inventory (HDI) Neurology. 1994;44:837–842. doi: 10.1212/wnl.44.5.837. [DOI] [PubMed] [Google Scholar]
- 28.Hatch JP, Moore PJ, Cyr-Provost M, Boutros NN, Seleshi E, Borcherding S. The use of electromyography and muscle palpation in the diagnosis of tension-type headache with and without pericranial muscle involvement. Pain. 1992;49:175–178. doi: 10.1016/0304-3959(92)90140-7. [DOI] [PubMed] [Google Scholar]
- 29.Lipchik GL, Holroyd KA, France CR, et al. Central and peripheral mechanisms in chronic tension-type headache. Pain. 1996;64:467–475. doi: 10.1016/0304-3959(95)00174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nathan PA, Meadows KD. Neuromusculoskeletal conditions of the upper extremity: Are they due to repetitive occupational trauma? Occup Med. 2000;15:677–693. iii. [PubMed] [Google Scholar]
- 31.Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Myofascial trigger points and their relationship to headache clinical parameters in chronic tension-type headache. Headache. 2006;46:1264–1272. doi: 10.1111/j.1526-4610.2006.00440.x. [DOI] [PubMed] [Google Scholar]
- 32.Fernandez-de-las-Penas C, Arendt-Nielsen L, Simons DG. Contributions of myofascial trigger points to chronic tension type headache. J Man Manip Ther. 2006;14:222–231. [Google Scholar]
- 33.Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Baltimore: Williams & Wilkins; 1999. [Google Scholar]
- 34.Fernandez-de-las-Penas C, Ge HY, Arendt-Nielsen L, Cuadrado ML, Pareja JA. Referred pain from trapezius muscle trigger points shares similar characteristics with chronic tension type headache. Eur J Pain. 2006;11:475–482. doi: 10.1016/j.ejpain.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 35.Fernandez-de-las-Penas C, Cuadrado ML, Arendt-Nielsen L, Simons DG, Pareja JA. Myofascial trigger points and sensitization: An updated pain model for tension-type headache. Cephalalgia. 2007;27:383–393. doi: 10.1111/j.1468-2982.2007.01295.x. [DOI] [PubMed] [Google Scholar]
- 36.Simons DG. Review of enigmatic MTRPs as a common cause of enigmatic musculoskeletal pain and dysfunction. J Electromyogr Kinesiol. 2004;14:95–107. doi: 10.1016/j.jelekin.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 37.Simons DG. Understanding effective treatments of myofascial trigger points. J Bodywork Movement Ther. 2002;6:81–88. [Google Scholar]
- 38.Wheeler AH. Myofascial pain disorders: Theory to therapy. Drugs. 2004;64:45–62. doi: 10.2165/00003495-200464010-00004. [DOI] [PubMed] [Google Scholar]
- 39.Hong CZ, Simons DG. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil. 1998;79:863–872. doi: 10.1016/s0003-9993(98)90371-9. [DOI] [PubMed] [Google Scholar]
- 40.Gam AN, Warming S, Larsen LH, et al. Treatment of myofascial trigger-points with ultrasound combined with massage and exercise: A randomised controlled trial. Pain. 1998;77:73–79. doi: 10.1016/S0304-3959(98)00084-0. [DOI] [PubMed] [Google Scholar]
- 41.Hanten WP, Olson SL, Butts NL, Nowicki AL. Effectiveness of a home program of ischemic pressure followed by sustained stretch for treatment of myofascial trigger points. Phys Ther. 2000;80:997–1003. [PubMed] [Google Scholar]
- 42.Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol. 2005;99:1977–1984. doi: 10.1152/japplphysiol.00419.2005. [DOI] [PubMed] [Google Scholar]
- 43.Babenko V, Graven-Nielsen T, Svensson P, Drewes AM, Jensen TS, Arendt-Nielsen L. Experimental human muscle pain and muscular hyperalgesia induced by combinations of serotonin and bradykinin. Pain. 1999;82:1–8. doi: 10.1016/S0304-3959(99)00026-3. [DOI] [PubMed] [Google Scholar]
- 44.Babenko VV, Graven-Nielsen T, Svensson P, Drewes AM, Jensen TS, Arendt-Nielsen L. Experimental human muscle pain induced by intramuscular injections of bradykinin, serotonin, and substance P. Eur J Pain. 1999;3:93–102. doi: 10.1053/eujp.1998.0103. [DOI] [PubMed] [Google Scholar]
- 45.Jensen R. Pathophysiological mechanisms of tension-type headache: A review of epidemiological and experimental studies. Cephalalgia. 1999;19:602–621. doi: 10.1046/j.1468-2982.1999.019006602.x. [DOI] [PubMed] [Google Scholar]
- 46.Bendtsen L. Central sensitization in tension-type headache–possible pathophysiological mechanisms. Cephalalgia. 2000;20:486–508. doi: 10.1046/j.1468-2982.2000.00070.x. [DOI] [PubMed] [Google Scholar]
- 47.Blanchard EB, Hillhouse J, Appelbaum KA, Jaccard J. What is an adequate length of baseline in research and clinical practice with chronic headache? Biofeedback Self Regul. 1987;12:323–329. doi: 10.1007/BF00998723. [DOI] [PubMed] [Google Scholar]