Abstract
Chronic cervical pain is a common source of disability in society, and evidence suggests that individuals with neck pain have impairment of the deep cervical flexor (DCF) muscles. This study investigated the recruitment pattern of the neck muscles, particularly the DCF, during the Craniocervical Flexion Test (CCFT), using ultrasound measurement of muscle activity in asymptomatic subjects. In a cross-sectional design, 10 subjects, of both sexes, with no history of neck pain participated in the study. Participants were instructed to perform the CCFT, and changes in thickness from resting baseline values during the five incremental stages of the test were obtained for DCF and sternocleidomastoid (SCM) muscles using ultrasonography. The most significant changes found in DCF thickness were between phase 1 and phases 4 (p<0.001) and 5 (p= <0.001). For SCM, differences were most significant between phases 1 and 3 (p<0.001), 4 (p<0.001), and 5 (p<0.001); and between phases 3 and 5 (p<0.003). No differences were found between DCF and SCM muscles. The present study confirms the evidence that CCFT increases DCF recruitment. However, the ultrasonography test protocol did not identify differences in recruitment between deep and superficial neck muscles. The present study confirms the evidence that the CCFT challenges the cervical spine and that DCF activity is increased during this maneuver.
Keywords: Craniocervical Flextion Test, Motor Control, Neck Muscles, Ultrasonography
Disability associated with chronic cervical pain is becoming increasingly prevalent in the community1. Chronic neck pain can be defined as a condition with episodes of persistent or recurrent and disabling pain2, with symptoms lasting longer than 3 months3,4. Data indicate that 66.7% of individuals will suffer from this condition at some stage of their lives1. Due to the great prevalence of cervical pain, effective management of this dysfunction is important to relieve symptoms and prevent its recurrence and the associated high healthcare costs5,6.
Mechanical stability of the cervical spine is provided primarily by the surrounding musculature7, and altered patterns of neck flexor synergy are known to be present in individuals with neck pain8,9. Individuals with chronic neck pain seem to have less activity of the deep cervical flexors (DCF), longus capitis and longus colli, the primary muscles involved in the support and control of the cervical curve10, compared to asymptomatic subjects11,12,13.
Ultrasonography is a well-established method for evaluating changes in muscle thickness, fiber pennation, and muscle fascicle length14,15. It is a non-invasive technique, with no occurrence of cross-talk of adjacent muscles and with acceptable reliability for the assessment of deep muscle recruitment15,16. Although traditionally it is used to visualize lumbar spine muscles, there are a few studies showing its use in cervical spine muscle assessment17,18,19,20,21. These studies were identified after a search strategy combining the words ultrasound (ultrasonography), cervical (neck), muscles (muscl*), motor control, and (stabil*) in the PubMed and PEDro databases. To our knowledge, no study has specifically investigated the pattern of recruitment of the DCF muscles using ultrasonography.
Therefore, the aim of this study was to investigate the recruitment pattern of the neck muscles using ultrasonography measurement of muscle activity in asymptomatic subjects, while performing a specific action, namely the Craniocervical Flexion Test (CCFT)9. This preliminary study was taken to collect baseline data and to investigate the sensitivity of the protocol developed.
Methods
Subjects
Ten subjects (4 female, 6 male), mean age 26 (SD=6.7) years, with no history of cervical pain volunteered for this experiment. Subjects were included in the study if they were free from neck or upper limb complaints and had no history of musculoskeletal or neurological conditions affecting the cervical spine. All subjects consented to participate in this study.The study was approved by the Federal University of Minas Gerais Research Ethics Committee (ETIC 517/06'Ad 01/07).
Ultrasonography recordings of sternocleidomastoideous (SCM) and DCF were made unilaterally (right side), using the Siemens Sonoline SL-1 Ultrasound (Bayswater Victoria, Australia). The positioning of the instrument was developed for this experiment, since no previous study design was identified that specifically targeted ultrasound activity of cervical flexors. A 7.5 MHz transducer was positioned longitudinally on the anterior neck, in parallel with the orientation of the trachea and approximately 5 cm from its midline. In this position, the ultrasound allowed proper visualization of the muscles being investigated, the right carotid artery, and vertebral lamina.
Procedure
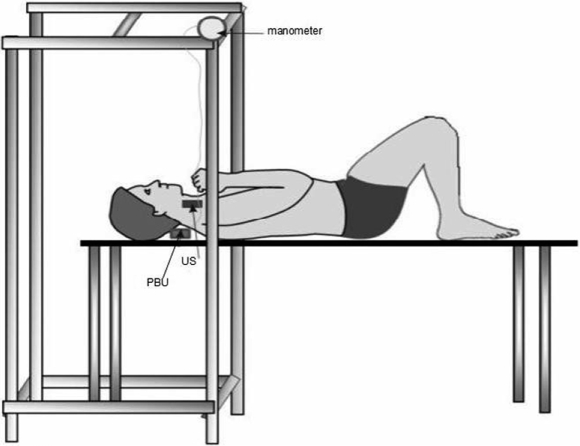
Subjects were positioned in supine lying with the knees bent and the arms crossed on the chest. The head and neck were placed in a standardized position so the subject's forehead and chin were horizontal and in a mid-position. The Pressure Biofeedback Unit- PBU, (Chattanooga Group, Hixon, TN) was placed suboccipitally and inflated to a 20 mm Hg baseline pressure. This unit is a sensitive apparatus for recording increases in pressure with cervical nodding, and it is a reliable tool for discriminating between individuals with chronic neck pain and asymptomatic ones, using the CCFT9. Feedback on pressure level was provided viaa manometer visible to the subject (Figure 1).
Figure 1.
Experimental setup. Subjects were positioned in supine with the pressure biofeedback unit (PBU) placed suboccipitally to detect increases in pressure with craniocervical flexion. Visual feedback of pressure level was provided by a manometer. Ultrasound transducer (US) was placed anterior and longitudinally for image recording during the CCFT.
During the CCFT, subjects were instructed to perform a nodding movement, representing the craniocervical flexion, in five incremental levels, from 22 to 30 mm Hg: thus, 22, 24, 26, 28, and 30 mmHg9. In each stage, subjects performed the action and held the target pressure for 10 seconds, with a 2-minute rest between trials. Ultrasonography images were recorded at the baseline resting phase and at the end of each successive stage. To guarantee the accuracy of the performance during the test, the examiner taught the movement passively to each subject and returned the head to neutral to initiate the test. The study administers verbally discouraged neck retraction that resulted in a visual increase in superficial muscle contraction.
Data Management and Analyses
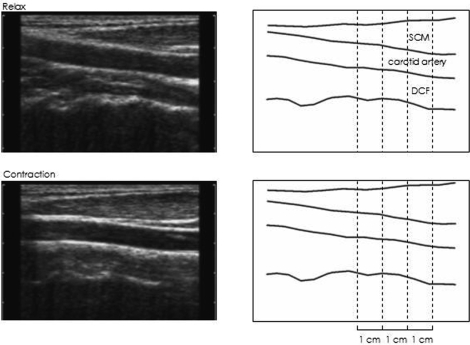
Two repetitions of the CCFT were performed and recorded, and the trial with the best image, i.e., permitting proper visualization of the cervical flexors, was considered for data analysis. Ultrasonography data were measured with a custom-designed software (Distance Software) using Lab View (National Instruments, North Ryde, NSW, Australia). This software was specially designed to measure muscle thickness between fascia borders because previous studies have employed ultrasound-built software to measure muscle cross-sectional area17,18. A grid was placed over each image, and measures of muscle thickness of DCF and SCM were made at sites 1, 2, and 3 cm to the right of the midline (Figure 2). Cursors were placed on the screen over the superficial and deep boundaries of the SCM muscle, and the outlines of the DCF were identified superiorly by carotid boundaries and inferiorly by the echogenic vertebral lamina. The average of the 3 measurements on all images for each muscle was calculated. Changes in thickness during the CCFT were expressed as a proportion of muscle thickness at rest. Means and 95% confidence intervals of measures were used for descriptive analysis. Statistical analysis of the ultrasound data was performed using an analysis of variance (ANOVA) with the between factors being the muscles and the within factors being the test phases. Duncan's post hoc testing was also performed when main factors or interactions were obtained. Significance was accepted at the 5% level (p ≤ 0.05).
Figure 2.
Ultrasound images of the anatomic location for the deep cervical flexors (DCF) and sternocleidomastoid (SCM) muscles during relaxed (upper panels) and contracted (lower panels) conditions for a trial to 30mm Hg pressure. Sites of thickness measurement are indicated by the vertical dashed lines.
Results
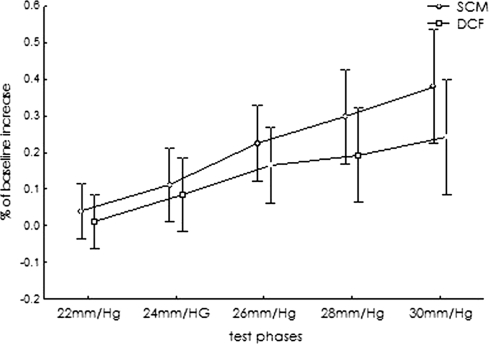
Descriptive analysis revealed an increase in DCF and SCM recruitment with each progressive phase of the test (Figure 3). No significant differences were found between DCF and SCM changes in thickness. The ANOVA analysis only showed a significant effect between CCFT phases (F=24.070; p<0.001), and no interaction effect was identified (F=1.09; p=0.369).
Figure 3.
Means and 95% confidence interval changes in thickness as a proportion of baseline resting thickness for the deep cervical flexors (DCF) and sternocleidomastoid (SCM) muscles during the CCFT phases. Note the progressive increase in thickness for both SCM and DCF muscles during the increment phases of the test.
For DCF, post hoc analysis indicated that the comparisons that were significantly different were between phases 1 and 3 (mean difference=.16; 95% CI: .08 to .23; p=0.003), 4 (mean difference=.18; 95%CI: .09 to .28; p<0.001), and 5 (mean difference=.23; 95%CI: .10 to .36; p<0.001); and between phases 2 and 4 (mean difference =.11; 95%CI:.02 to .20; p= 0.035) and 5 (mean difference=.16; 95%CI:.04 to .27; p= 0.003).
For SCM, the comparisons that were significantly different were between phases 1 and 3 (mean difference=.18; 95%CI:.08 to .29; p<0.001), 4 (mean difference=.26; 95%CI:.11 to .41; p<0.001), and 5 (mean difference=.34; 95%CI:.18 to .50; p<0.001); between phases 2 and 3 (mean difference=.13; 95%CI:.05 to .22; p=0.03); and finally, between phases 3 and 5 (mean difference=.16; 95%CI:.05 to .26; p= 0.003).
Discussion
There is a nonlinear relationship between changes in thickness seen with ultrasound imaging and muscle electromyography during tasks involving less than 30% of the maximum voluntary contraction15. Ultrasonography was used in the present study to investigate whether changes in pressure during the CCFT were associated with changes in DCF and SCM thickness. We were not able to provide any comparison between our findings and other ultrasound data, since no previous data related to ultrasonography measurement of the neck muscles were found in the literature although the present findings reinforce the evidence that the CCFT recruits deep and superficial neck flexors22.
Although in the present study no differences were found between SCM and DCF recruitment, there was a tendency towards a greater increase in thickness for SCM than for DCF during the last three phases of the test. Because DCF muscles have a smaller cross-sectional area compared to superficial neck muscles, possible mechanical compression from the surrounding musculature reducing the thickness of the deep muscles during each of the craniocervical movement phases should not be ruled out. We did not employ electromyography via intramuscular fine-wire electrodes, the known gold standard test procedure to assess neck flexors recruitment11,22, thus we cannot clearly separate muscle activity from mechanical compression.
It is known that CCFT can discriminate between those with chronic cervical pain individuals from those without12. Individuals who suffer from neck pain have impaired performance during the test, with less amplitude of DCF electromyography activity and significantly higher EMG amplitude of superficial muscles when compared with controls11. It seems that there is a specific effect of neck trauma on muscle function12 and that pain can cause alterations and significant deficits in fine motor control of the spine23. Our hypothesis was that ultrasonography measurements during the CCFT would be sensitive enough to detect DCF dysfunction in chronic neck pain patients and that these subjects would have smaller increases in DCF thickness during the test compared to asymptomatic subjects. These studies are currently under development.
Conclusion
The present study reinforces the evidence that the CCFT challenges DCF recruitment as measured by ultrasonography; however, differences between deep and superficial neck muscles were not identified. The protocol developed in this study appears to have potential clinical application to assess and monitor muscle impairment in neck pain patients, providing a feasible noninvasive and objective assessment of neck flexors recruitment, but further research is required to investigate its reliability and discriminatory validity.
Contributor Information
Fabianna M.R. Jesus, Masters student, Department of Physiotherapy; School of Physical Education, Physiotherapy and Occupational Therapy; Federal University of Minas Gerais, Belo Horizonte, Brazil..
Paulo H. Ferreira, Lecturer, School of Physiotherapy; Faculty of Health Sciences; University of Sydney, Sydney, Australia..
Manuela L. Ferreira, Research Fellow, Faculty of Health Sciences; University of Sydney, Sydney, Australia..
REFERENCES
- 1.Côté P, Cassidy JD, Carrol L. The Saskatchewan health and back pain survey: The prevalence of neck pain and related disability in Saskatchewan adults. Spine. 1998;23:1689–1698. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Côté P, Cassidy JD, Carrol L, Kristman V. The annual incidence and course of neck pain in the general population: A population based-cohort study. Pain. 2004;112:267–273. doi: 10.1016/j.pain.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Guez M, Hildingsson C, Stegmayr B, Toolanen G. Chronic neck pain of traumatic and non-traumatic origin: A population-based study. Acta Orthop Scand. 2003;74:575–579. doi: 10.1080/00016470310017983. [DOI] [PubMed] [Google Scholar]
- 4.Ylinen J, Takala EP, Kautiainen H, et al. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non-specific neck pain. Eur J Pain. 2004;8:473–478. doi: 10.1016/j.ejpain.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Borghouts JAJ, Koes BW, Vondeling H, Bouter LM. Cost-of-illness of neck pain in The Netherlands in 1996. Pain. 1999;80:629–636. doi: 10.1016/S0304-3959(98)00268-1. [DOI] [PubMed] [Google Scholar]
- 6.Falla D. Unravelling the complexity of muscle impairment in chronic neck pain. Man Ther. 2004;9:125–133. doi: 10.1016/j.math.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Panjabi MM, Cholewicki J, Nibu K, Grauer J, Babat LB, Dvorak J. Critical load of the human cervical spine: An in vitro experimental study. Clin Biomech. 1998;13:11–17. doi: 10.1016/s0268-0033(97)00057-0. [DOI] [PubMed] [Google Scholar]
- 8.Barton P, Hayes K. Neck flexor muscle strength, efficiency and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch Phys Med Rehabi. 1996;77:680–686. doi: 10.1016/s0003-9993(96)90008-8. [DOI] [PubMed] [Google Scholar]
- 9.Jull GA, Barrett C, Magee R, Ho P. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia. 1999;19:179–185. doi: 10.1046/j.1468-2982.1999.1903179.x. [DOI] [PubMed] [Google Scholar]
- 10.Mayoux-Benhamou M, Revel M, Vallée C, Roudier R, Barbet JP, Bargy F. Longus colli has a postural function on cervical curvature. Surg Radiol Anat. 1994;16:367–371. doi: 10.1007/BF01627655. [DOI] [PubMed] [Google Scholar]
- 11.Falla D, Jull GA, Hodges P. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine. 2004;29:2108–2114. doi: 10.1097/01.brs.0000141170.89317.0e. [DOI] [PubMed] [Google Scholar]
- 12.Jull G, Kristjanson E, Dall'alba P. Impairment in the cervical flexors: A comparison of the whiplash and insidious onset neck pain patients. Man Ther. 2004;9:89–94. doi: 10.1016/S1356-689X(03)00086-9. [DOI] [PubMed] [Google Scholar]
- 13.O'Leary SP, Vincenzino BT, Jull GA. A new method of isometric dynamometry for the craniocervical flexor muscles. Phys Ther. 2005;85:556–564. [PubMed] [Google Scholar]
- 14.Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003;27:682–692. doi: 10.1002/mus.10375. [DOI] [PubMed] [Google Scholar]
- 15.Mcmeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech. 2004;19:337–342. doi: 10.1016/j.clinbiomech.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Bunce SM, Moore AP, Hough AD. M-mode ultrasound: A reliable measure of transverses abdominis thickness? Clin Biomech. 2002;17:315–317. doi: 10.1016/s0268-0033(02)00011-6. [DOI] [PubMed] [Google Scholar]
- 17.Emshoff R, Bertram S, Strobl H. Ultrasonographic cross-sectional characteristics of muscles of the head and neck. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:93–106. doi: 10.1016/s1079-2104(99)70302-1. [DOI] [PubMed] [Google Scholar]
- 18.Kristjansson E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic subjects. Man Ther. 2004;9:83–88. doi: 10.1016/S1356-689X(03)00059-6. [DOI] [PubMed] [Google Scholar]
- 19.Lee JP, Tseng WY, Shau YW, Wang CL, Wang HK, Wang SF. Measurement of segmental cervical multifidus contraction by ultrasonography in asymptomatic adults. Man Ther. 2007;12:286–294. doi: 10.1016/j.math.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Rankin G, Stokes M, Newham D. Size and shape of the posterior neck muscles measured by ultrasound imaging: Normal values in males and females of different ages. Man Ther. 2005;10:10–15. doi: 10.1016/j.math.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Jull G, Amiri M, Bullock-Saxton J, Darnell R, Lander C. Cervical musculoskeletal impairment in frequent intermittent headache. Part 1: Subjects with single headaches. Cephalalgia. 2007;27:793–802. doi: 10.1111/j.1468-2982.2007.01345.x. [DOI] [PubMed] [Google Scholar]
- 22.Falla D, Jull G, Dall'Alba P, et al. An electromyographic analysis of the deep cervical flexor muscles in performance of craniocervical flexion. Phys Ther. 2003;83:899–906. [PubMed] [Google Scholar]
- 23.Falla D, Farina D, Dahl MK, Graven-Nielsen T. Muscle pain induces task-dependent changes in cervical agonist/antagonist activity. J App Physiol. 2007;102:601–609. doi: 10.1152/japplphysiol.00602.2006. [DOI] [PubMed] [Google Scholar]