Abstract
Ankle dorsiflexion range of motion (ROM) typically decreases after prolonged immobilization. Anterior-to-posterior talocrural joint mobilizations are purported to increase dorsiflexion ROM and decrease joint stiffness after immobilization. The purpose of this study was to determine if a single bout of Grade III anterior-to-posterior talocrural joint mobilizations immediately affected measures of dorsiflexion ROM, posterior ankle joint stiffness, and posterior talar translation in ankles of patients who had been immobilized at least 14 days. Ten physically active patients (5 males, 5 females; age=21.4±3.3 years) participated. Each had the ankle immobilized following a lower extremity injury for at least 14 days and presented with at least a 5° dorsiflexion ROM deficit compared to the contralateral ankle. A crossover design was employed so that half of the subjects received joint mobilizations first and half of the subjects received the control intervention (no treatment) first. All subjects ultimately received both treatments. Active dorsiflexion ROM was assessed with a bubble inclinometer, and posterior ankle stiffness and talar translation were assessed with an instrumented ankle arthrometer. After a single application of grade III anterior-to-posterior talocrural joint mobilization, dorsiflexion ROM and posterior ankle joint stiffness were significantly increased. There was also a trend toward less posterior talar translation immediately after mobilization. The trend toward decreased posterior talar translation and increased posterior ankle joint stiffness supports the positional fault theory. Correction of an anterior talar positional fault offers a possible explanation for these results.
Keywords: Dorsiflexion, Grade III Mobilization, Positional Fault, Tibiotalar Joint
Passive joint mobilizations consist of gentle oscillating movements of the articular surfaces that create the movement of joints by a means other than the musculotendinous units that normally act on those particular segments. Joint mobilizations are purported to relieve pain and improve range of motion (ROM) of injured joints1,2,3,4. Such improvements can in turn lead to an increase in functional activities1,5. Using Maitland's classification6, Grade I and Grade II joint mobilizations are performed primarily to decrease joint pain, and Grade III and Grade IV joint mobilizations are used to increase joint ROM.
Restrictions in ankle dorsiflexion are often observed clinically after prolonged immobilization of the ankle joint. One purported cause of decreased dorsiflexion ROM may be restricted posterior glide of the talus on the tibia7. There is an emerging body of evidence demonstrating the effectiveness of joint mobilizations, especially anterior-to-posterior mobilization of the talus on the tibia, to increase ankle dorsiflexion ROM1,5,8,9,10. Wilson et al5 demonstrated improved plantar flexion and dorsiflexion ROM and functional ability in a pilot study of patients recovering from ankle fractures who received 5 weeks of talocrural and subtalar joint mobilizations and therapeutic exercise compared to a group that received only therapeutic exercise. Green et al1 demonstrated that pain-free ankle dorsiflexion ROM was increased with anterior-posterior joint mobilizations in those recovering from acute ankle sprains. Joint mobilizations led to a reduction in pain and improvements in pain-free dorsiflexion ROM in comparison to control subjects. Likewise, Collins et al9 demonstrated immediate improvement in dorsiflexion ROM after mobilization in patients with subacute ankle sprains. Additionally, Vicenzino et al10 recently demonstrated that dorsiflexion ROM gains after ankle joint mobilization in patients with recurrent ankle sprains were strongly correlated to increases in posterior talar glide.
One possible explanation for the effectiveness of anterior-to-posterior talocrural mobilizations in improving dorsiflexion ROM is the correction of a positional fault in which the talus is subluxated anteriorly on the tibia11. To date, there is limited quantitative evidence to verify the legitimacy of a positional fault at the ankle, a theory advocated by Brian Mulligan. Instrumented ankle arthrometry offers a method to quantify talar mobility under known loads by measuring rear-foot displacement and translational force during anterior and posterior drawer maneuvers12,13. If the talus was positioned in an abnormally anterior position and posteriorly directed mobilizations were able to correct this positional fault, the magnitude of available posterior talar translation may be decreased after joint mobilization. If posterior talar translation was reduced under the same load, this would actually indicate an increase in the measured stiffness (slope of the force-displacement curve) of the ankle during posterior translation.
Our purpose was to determine if a single session of Maitland Grade III anterior-to-posterior talocrural joint mobilizations applied following a period of prolonged ankle immobilization would cause immediate increases in dorsiflexion ROM and posterior ankle joint stiffness, and decreases in posterior talar translation.
Methods
Design
A crossover design was employed to assess the effect of treatment order (joint mobilization first, control treatment first) on dorsiflexion ROM, posterior talar translation, and posterior talocrural joint stiffness.
Subjects
Ten subjects (5 males, 5 female; age 21.4±3.3 years, height 171.7±11.6 cm, mass 72.3±17.9 kg) participated. All subjects had lower extremity injuries that required prolonged immobilization in a lower leg cast or walking boot; otherwise, the subjects were in good health (Table 1). Inclusion criteria for this study included ankle immobilization for at least 14 days and a deficit of at least 5° dorsiflexion ROM compared to the contralateral ankle. Subjects had an average ROM deficit of 7.9°±2.9° at baseline. Exclusion criteria included osteoarthritis at the ankle, unstable fractures, intra-articular fixation in the ankle joint, rheumatoid arthritis, and connective tissue disorders such as Marfan's or Ehlers-Danlos syndromes. All subjects signed an informed consent agreement prior to participation in this study. Human subject approval was obtained through the local university institutional review board.
TABLE 1.
Subject characteristics.
| Subject | Injury | Length of Immobilization | Type of Immobilization | Initial Dorsiflexion ROM Deficit* | Final Dorsiflexion ROM Deficit* |
|---|---|---|---|---|---|
| 1 | Flexor hallicis longus repair | 5 weeks | Walking boot | 6° | 0° |
| 2 | Ankle sprain | 2 weeks | Walking boot | 7° | 4° |
| 3 | Tibial stress fracture | 2 weeks | Walking boot | 14° | 10° |
| 4 | Fibular stress fracture | 4 weeks | Walking boot | 11° | 4° |
| 5 | Tibial stress fracture | 4 weeks | Walking boot | 7° | 5° |
| 6 | Great toe fracture | 2 weeks | Walking boot | 10° | 0° |
| 7 | Tibial stress fracture | 4 weeks | Walking boot | 7° | 0° |
| 8 | Tibial stress fracture | 3 weeks | Walking boot | 5° | 3° |
| 9 | Heel spur | 3 weeks | Walking boot | 5° | 2° |
| 10 | Fif h metatarsal fracture | 9 weeks | Splint (2 wks) Cast (6 wks) | ||
| Walking boot (4 days) | 6° | 6° | |||
Refers to comparison of opposite extremity dorsif exion
Instruments
Ankle dorsiflexion ROM was measured using a bubble inclinometer (Fabrication Enterprises Inc., White Plains, NY). Posterior talar mobility and stiffness were measured using an ankle arthrometer (Blue Bay Research Inc., Milton, FL)12,13. The ankle arthrometer measures the amount of joint displacement along with the force used to generate the displacement. The spatial kinematic linkage system of the arthrometer measures the relative motion between the arthrometer footplate and the reference pad placed on the tibia thus quantifying movement of the rear foot in relation to the tibia12,13. The ankle arthrometer data were collected and analyzed utilizing a custom software program operated through the LabView software program (National Instruments Corp., Austin, TX).
Testing procedures
All subjects underwent three series of measurements (baseline, post-first treatment, and post-second treatment). Each series included measures of ankle dorsiflexion ROM, posterior talar mobility, and posterior joint stiffness. All subjects received both treatments (joint mobilization, control). A crossover design was utilized so that the order of the joint mobilizations and control treatments was applied randomly. The tester (ELL) was blinded to the order of treatments received by each subject. The order of treatments was randomized and revealed to the clinician administering the treatments via sealed envelope allocation.
Subjects were asked to remove shoes and socks prior to testing. First, a baseline measure of open-chain, straight-knee dorsiflexion ROM was measured with a bubble inclinometer using methods previously described by Denegar et al14. The reliability of this method has been reported previously (ICC = .96–.97, SEM = .99°–1.34°)14. Second, the arthrometer and affected ankle were prepared for testing with a spray adhesive to minimize any slipping between the skin and the arthrometer. During arthrometer testing, subjects were lying supine with a styrofoam bolster underneath the knee of the test limb (Figure 1a). The styrofoam bolster was applied in order to standardize lower extremity positioning with knee flexion at 30° and to optimize patient comfort during arthrometer testing. To ensure consistency of measures, a felt tip pen marking was placed on the lower extremity at the junction between the subject's leg and the plinth. With the ankle in neutral position, a posteriorly-directed force of 170 N was applied to the subject's ankle via the arthrometer, and measures of posterior talar translation and joint stiffness were taken (Figure 1b). Posterior translation of the talus was measured in millimeters (mm), and stiffness was defined as the slope of the force-displacement curve. The arthrometer was then removed and the tester left the room. The reliability of the anterior-posterior translation measures in vivo with this arthrometer have previously been reported (ICC=.91, SEM=.89 mm)15. Additionally, the validity of this measurement has been demonstrated in a cadaver study in which the arthrometer measures were highly correlated (r=.88) to actual bone motion13.
Figure 1A.
(top) Positioning of subject's limb for arthrometer testing.
Figure 1B.
(bottom) Examiner positioning for arthrometer testing. The arrow represents the posteriorly directed force applied through the arthrometer.
The first treatment consisted of either a 30-second application of Grade III anterior-to-posterior talocrural joint mobilizations or the control treatment consisting of 30 seconds of rest in the presence of the same clinician who administered the joint mobilizations. For the purposes of this study, Grade III mobilizations were operationally defined as large-amplitude rhythmic oscillations from the joint's mid-range to the end-range with translation taken to the point of tissue resistance. All joint mobilizations were performed by the same physical therapist (BMK), who had over 15 years of clinical practice experience in orthopedic physical therapy.
After the first intervention was complete, the tester returned and a second series of measures was taken. After the second measurements were taken, the arthrometer was removed, the tester left the room, and the second intervention (the opposite of what was first received) was applied by the same clinician as the first intervention. After the second intervention was complete, the final series of measures was taken by the tester.
Statistical analysis
The three dependent variables were dorsiflexion ROM, posterior talar translation, and joint stiffness. The independent variables were treatment order group, a between-factor variable with two levels (joint mobilization first, control first), and time, a within-factor variable with three levels (baseline, post-first treatment, and post-second treatment). For each dependent variable, a 2×3 mixed model ANOVA was run to compare the influence of treatment order and time. In the event of a significant interaction or main effect, Tukey's post hoc tests were computed to identify specific differences. All analyses were performed using SPSS 13.0 (SPSS Inc, Chicago, IL), and the alpha level was set a priori at p≤0.05.
Results
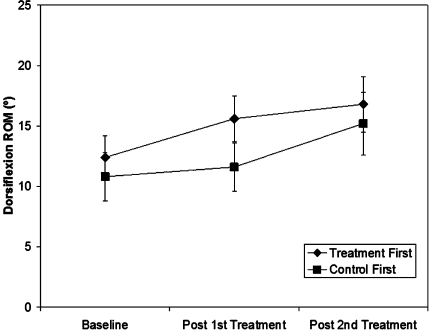
Descriptive statistics for each measure may be seen in Table 2 and are illustrated in Figures 2–4. For the dorsiflexion ROM, there was a significant main effect for time (p=.013); however, there was not a significant treatment order by time interaction (p=.29, 1-ß=.28) or treatment order main effect (p=.44, 1-ß=.11). The mean (±SD) dorsiflexion ROM was 11.6°±4.3° at baseline, 13.6° ± 4.7° after the first treatment, and 16.0°±5.6° after the second treatment. Post hoc testing revealed that the post-first treatment measure was significantly greater than the baseline measure and that the post-second treatment measure was significantly greater than the two previous measures (p<0.05).
TABLE 2.
Means and standard deviation of the dependent variables.
| Treatment First Group | Control First Group | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Post- Treatment 1 | Post- Treatment 2 | Baseline | Post- Treatment 1 | Post- Treatment 2 | Baseline | Post- Treatment 1 | Post- Treatment 2 | |
| Dorsif exion ROM (°) | 12.4+4.9 | 15.6+5.4 | 16.8+6.0 | 10.8+4.1 | 11.6+4.0 | 15.2+5.8 | 11.6+.3 | 13.6+4.7Λ | 16.0+5.5Λ |
| Posterior Talar Displacement (mm) | 6.3+1.5 | 6.4+3.0 | 4.7+1.4 | 7.9+1.1 | 5.6+0.6 | 5.8+2.0 | 6.7+1.2 | 5.9+1.7 | 5.4+1.8 |
| Posterior Stif ness* | 22.0+4.4 | 22.6+8.3 | 26.6+5.0 | 18.5+4.4 | 25.8+4.2 | 24.2+7.1 | 19.8+4.5 | 24.6+5.7 | 25.1+6.2⁁ |
Stif ness is estimated as the slope of the force-displacement curve.
Significantly dif erent from baseline (p<.05)
Figure 2.
Dorsiflexion range of motion (ROM) means (± SE) for both groups at each testing interval. There was not a significant time by group interaction (p=.49), but there was a significant time main effect (p=.03) indicating that regardless of group membership, there was improved ROM at each testing interval.
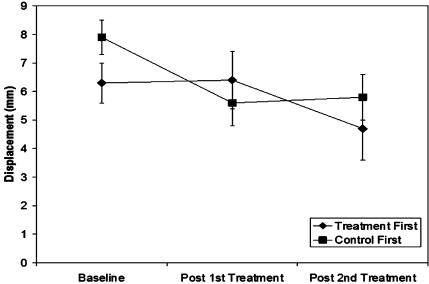
Figure 4.
Posterior talar translation means (± SE) for both groups at each testing interval. There was not a significant time by group interaction (p=.25) or time main effect (p=.08).
For the posterior talar translation measures, there was no significant treatment order by time interaction (p=.25, 1-ß=.38) or treatment order main effect (p=.75, 1-ß=.12). There was a trend towards a time main effect, but this did not reach a statistically significant level (p=.08, 1-ß=.39). Across all subjects, the mean (±SD) amount of posterior talar translation was 6.7±1.2 mm at baseline, 5.9±1.7 mm after the first treatment, and 5.4±1.8 mm after the second treatment.
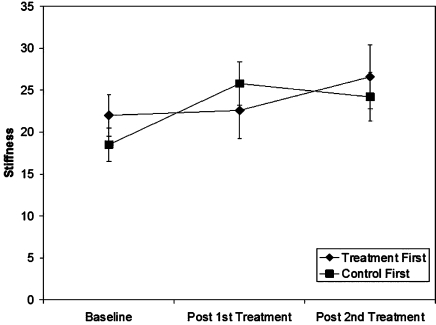
For the stiffness measures, there was a significant main effect for time (p=0.04), but there was not a significant treatment order by time interaction (p=.81, 1-ß=.25) or treatment order main effect (p=.15, 1-ß=.15). The mean slope of the stiffness curve was 19.8±4.5 at baseline, 24.6±5.7 after the first treatment, and 25.1±6.2 after the second treatment. Post hoc testing revealed that the post-second treatment slope was significantly higher than the baseline measure (p=0.02).
Discussion
Our results provide preliminary evidence in support of the immediate effectiveness of Grade III anterior-to-posterior talocurural joint mobilizations in the treatment of patients with limited dorsiflexion ROM. Ankle dorsiflexion ROM increased significantly at each assessment period. At the final follow-up after all subjects had received the active intervention, dorsiflexion ROM had increased an average of 4.4±3.0° compared to baseline. This increase greatly exceed the reported SEM of the dorsiflexion ROM measure (.99°–1.34°)14, thus providing confidence that the interventions, and not measurement error, was the cause of the ROM increase. A possible reason for this increase in dorsiflexion ROM could be due to correction of an anterior positional fault of the talus after joint mobilizations. The amount of posterior talar translation decreased, albeit at non-significant levels, at each successive measurement session. Because the amount of force was constant across all measures and the amount of posterior translation decreased at each testing interval, estimates of joint stiffness substantially increased with each consecutive measure following joint mobilizations.
In a 2×3 crossover study design such as the one we employed, an extremely efficacious active treatment intervention would ideally result in a statistically significant treatment order by time interaction. While this did not occur for any of the three dependent measures, significant time main effects were found for dorsiflexion ROM and stiffness measures, and the posterior talar translation measure approached significance (p= 0.08). The significant time main effects indicate that measures changed significantly at successive measurement intervals across all subjects regardless of treatment order. Examination of Figure 2 clearly shows more dramatic increases in dorsiflexion ROM in measures immediately after the active treatment was received compared to the control treatment. The direct effects of joint mobilization on the talar translation and stiffness measures are less intuitive (Figures 3–4).
Figure 3.
Estimates of posterior talocrural joint stiffness means (± SE) for both groups at each testing interval. Stiffness was estimated as the slope of the force-displacement curve from the arthrometer testing. There was not a significant time by group interaction (p=.19), but there was a significant time main effect (p=.04). Regardless of group membership, there was increased stiffness at the last testing interval compared to baseline.
The increase in dorsiflexion ROM after joint mobilization in our study is consistent with the outcomes of previous studies of ankle-injured patients1,5,9,10. In a pilot study of patients recovering from ankle fractures, Wilson et al5 demonstrated that a 5-week intervention of talocrural and subtalar joint mobilizations in combination with therapeutic exercise produced greater dorsiflexion and plantar flexion ROM gains and functional recovery than did therapeutic exercise alone. Green et al1 reported that anteroposterior mobilization of the talus using a gentle force resulted in greater improvement in dorsiflexion ROM and return to normal gait pattern in patients who received an average of 3 sessions over the 2 weeks following acute ankle sprain. Likewise, Collins et al9 demonstrated immediate improvements in dorsiflexion ROM in subacute ankle sprain patients receiving a single application of mobilizations with movement (MWM); Vicenzino et al10 presented similar findings in patients suffering from recurrent ankle sprains. While our study had a more heterogeneous population with patients recovering from a variety of lower extremity pathologies, we identified similar ROM improvements after mobilizations to the previous studies1,5,9,10, which utilized subjects with ankle sprains.
With each subsequent arthrometer measurement, stiffness measures increased while posterior talar translation measures decreased. It is plausible that the starting position of the talus was more posterior at the second and third measures compared to baseline, thus resulting in less posterior translation. A mean (±SD) difference of 1.3±1.3 mm was found between baseline and final follow-up measures across all subjects. This change exceeds the previously reported SEM of this measure (.89 mm)15, thus providing confidence that the change in this measure was likely due to the intervention and not measurement error. The cause of the apparent posterior shift in the resting talar position could come from two sources: the talocrural joint mobilizations (as hypothesized) or the arthrometer used for testing. It must be noted that the posterior rear-foot displacement provided by the arthrometer during testing may resemble a single repetition of posteriorly directed joint mobilization. This issue most likely could only be clarified in a study that used imaging techniques to assess resting talar position before and after applications of joint mobilizations and arthrometer testing.
Mulligan's positional fault theory11 may help explain our findings. Residual loss of the posterior talar glide may be representative of an anterior positional fault of the talus on the tibia and may result in an abnormal axis of talocrural rotation7. Through an acute mechanism of injury, such as ankle sprain, the talus may anteriorly subluxate and become stuck, thus resulting in restricted posterior glide and compromised ankle function14. It is possible that the patients in our study who were immobilized for a prolonged period of time also developed positional faults of the talus and that these positional faults were corrected via either the joint mobilizations and/or the arthrometer testing. Further research is necessary to explore this hypothesis.
This study did have a few limitations. We had a relatively small sample size (n=10) and the post hoc power analyses for the nonsignificant findings indicate that there was inadequate statistical power. In addition, the subjects were not homogenous as the injuries for which they were immobilized included a variety of lower extremity injuries as different as ankle sprains, stress fractures, and fifth metatarsal fractures (Table 1). Along with improved subject homogeneity, the type of immobilization devices was not identical. Most subjects were immobilized with walking boots whereas one subject was immobilized with a hard cast. The length of ankle immobilization also varied widely from a minimum of 2 weeks to a maximum of 9 weeks. Additionally, the ideal force needed in order to adequately perform a measure of posterior talar translation with the arthrometer is not known. For this study, 170 N was the maximum posteriorly directed force applied. We chose this value following extensive pilot testing of healthy subjects but it may not be the ideal force for such a measure. This study also only concentrated on the immediate short-term effects of joint mobilizations. Similar research needs to be done to assess the immediate and long-term effects, including both mechanistic properties and patient functional outcomes, of single and multiple applications of joint mobilizations.
Conclusion
We found that a single application of Grade III anterior-to-posterior talocrural joint mobilizations appears to increase ankle dorsiflexion ROM in a population with dorsiflexion ROM restrictions resulting from prolonged ankle immobilization. We also found that the joint mobilizations appeared to result in a decreased amount of posterior talar displacement and, thus, increased posterior joint stiffness as assessed with an ankle arthrometer. These results may be related to a correction of a positional fault at the talocrural joint although further research is needed to verify this hypothesis.
Acknowledgements
“The views expressed in this article are those of the authors and do not reflect the official policy of the Department of the Navy, the Department of Defense, nor the United States Government.”
Contributor Information
Elizabeth L. Landrum, Assistant Athletic Trainer, University of Alabama-Birmingham, Birmingham, AL..
Cdr. Brent M. Kelln, Director of Clinical Support Services, Naval Health Clinic Hawaii, United States Navy, Honolulu, HI..
William R. Parente, Assistant Athletic Trainer, University of Virginia, Charlottesville, VA..
Christopher D. Ingersoll, Joe H. Gieck Professor of Sports Medicine, University of Virginia, Charlottesville, VA..
Jay Hertel, Associate Professor of Kinesiology, University of Virginia, Charlottesville, VA..
REFERENCES
- 1.Green T, Refshauge K, Crosbie J, Adams R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther. 2001;81:984–994. [PubMed] [Google Scholar]
- 2.Cassidy JD, Lopes A, Yong-Hing K. The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: A randomized controlled trial. J Manipulative Physiol Ther. 1992;15:570–575. [PubMed] [Google Scholar]
- 3.Sluka KA, Wright A. Knee joint mobilization reduces secondary mechanical hyperalgesia induced by capsaicin injection into the ankle joint. Eur J Pain. 2001;5:81–87. doi: 10.1053/eujp.2000.0223. [DOI] [PubMed] [Google Scholar]
- 4.Hanrahan S, Van Lunen BL, Tamburello M, Walker ML. The short-term effects of joint mobilizations on acute mechanical low back dysfunction in collegiate athletics. J Athl Train. 2005;42:88–93. [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson FM. Manual therapy versus traditional exercises in mobilisation of the ankle post-ankle fracture: A pilot study. NZ J Physiother. 1991;19:11–16. [Google Scholar]
- 6.Maitland GD. Peripheral Manipulation. London, UK: Butterworths; 1978. [Google Scholar]
- 7.Denegar CR, Miller SJ. Can chronic ankle instability be prevented? Rethinking management of lateral ankle sprains. J Athl Train. 2002;37:430–435. [PMC free article] [PubMed] [Google Scholar]
- 8.van der Wees PJ, Lenssen AF, Hendriks EJ, Stomp DJ, Dekker J, de Bie RA. Effectiveness of exercise therapy and manual mobilisation in ankle sprain and functional instability: A systematic review. Aust J Physiother. 2006;52:27–37. doi: 10.1016/s0004-9514(06)70059-9. [DOI] [PubMed] [Google Scholar]
- 9.Collins N, Teys P, Vicenzino B. The initial effects of a Mulligan's mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004;9:77–82. doi: 10.1016/S1356-689X(03)00101-2. [DOI] [PubMed] [Google Scholar]
- 10.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36:464–471. doi: 10.2519/jospt.2006.2265. [DOI] [PubMed] [Google Scholar]
- 11.Mulligan BR. Manual therapy “NAGS,” “SNAGS,” “MWMS,” etc. 4th ed. Wellington, NZ: Plane View Services; 1999. [Google Scholar]
- 12.Kovaleski JE, Gurchiek LR, Heitman RJ, Hollis JM, Pearsall AW. Instrumented measurement of anteroposterior and inversion-eversion laxity of the normal ankle joint complex. Foot Ankle Int. 1999;20:808–814. doi: 10.1177/107110079902001210. [DOI] [PubMed] [Google Scholar]
- 13.Kovaleski JE, Hollis JM, Heitman RJ, Gurchiek LR, Pearsall AW. Assessment of ankle-subtalar-joint-complex laxity using an instrumented ankle arthrometer: An experimental cadaveric investigation. J Athl Train. 2002;37:467–474. [PMC free article] [PubMed] [Google Scholar]
- 14.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32:166–172. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- 15.Hubbard TJ, Kovaleski JE, Kaminski TW. Reliability of intra and intertester measurements derived from an instrumented ankle arthrometer. J Sport Rehabil. 2003;12:208–220. [Google Scholar]