Abstract
Cor triatriatum is a rare congenital cardiac disease in which a fibromuscular membrane divides the left atrium into 2 distinct chambers. The most common presenting symptoms in adults are dyspnea, hemoptysis, and orthopnea, which mimic mitral stenosis in presentation. Cor triatriatum is commonly evaluated and diagnosed by echocardiography.
Herein, we describe the case of a 39-year-old woman who had experienced worsening dyspnea for 7 months. Cor triatriatum was diagnosed by transthoracic and transesophageal echocardiography. A 3-dimensional reconstruction image produced by multidetector-row computed tomography (40 slices) clearly showed the intra-atrial membrane and the communicating fenestration, in conjunction with coronary and whole-heart evaluation in a single study. On the basis of our findings, we conclude that multidetector-row computed tomography may be a useful tool, as an adjunct to echocardiography, for whole-heart evaluation before operative correction of cor triatriatum.
Key words: Cor triatriatum/diagnosis; heart atria/abnormalities; heart defects, congenital/diagnosis; hypertension, pulmonary; tomography, X-ray computed
Cor triatriatum is an uncommon congenital cardiac anomaly that is found in only 0.1% of patients who have congenital heart disease.1 It is a condition wherein a fibromuscular membrane subdivides the left atrium into a postero-superior chamber that receives blood from the pulmonary veins and an antero-inferior chamber that contains the left atrial appendage and the mitral valve orifice. In most cases, the 2 chambers communicate through 1 or more perforations in the intra-atrial membrane. The clinical features on presentation can mimic those of mitral stenosis.
Cor triatriatum is frequently associated with other cardiovascular abnormalities. In adults, the most common associated abnormalities are atrial secundum septal defect,2 mitral regurgitation,3 and the presence of left superior vena cava with unroofed coronary sinus. Less common associated abnormalities are aortic regurgitation with dissecting aneurysm, and an anomalous partial pulmonary venous connection.
In this report, we describe the case of a 39-year-old woman who presented with dyspnea. Cor triatriatum was diagnosed by transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE). A multidetector-row computed tomographic (MDCT) (40 slices) 3-dimensional reconstruction image clearly showed the intra-atrial membrane and the opening of the membrane. Simultaneous whole-heart evaluation showed no other associated congenital anomalies and normal coronary vasculature.
Case Report
In February 2007, a 39-year-old woman with a 7-month history of progressive dyspnea, chest pain, and shortness of breath was referred to this medical center for further investigation. She had no significant history of disease. On physical examination, she was an otherwise healthy woman, 158 cm in height and 55 kg in weight. Her blood pressure was 122/72 mmHg; she had a heart rate of 74 beats/min and a regular respiratory rate of 16 breaths/min. Auscultation of the heart revealed a normal S1 with a loud pulmonic component of the S2; there was a grade 2/6 systolic murmur audible at the left sternal border. Her lungs were clear. Chest radiography showed a normal-sized heart with normal pulmonary vascularity. An electrocardiogram showed sinus rhythm. Transthoracic echocardiography (Fig. 1A) revealed a membrane that subdivided the dilated left atrium into 2 chambers. Color Doppler echocardiography showed turbulent flow across the membrane on the lateral aspect of the atrium. Pulsed-wave Doppler echocardiography demonstrated forward flow in both systole and diastole. The estimated mean transmembrane pressure gradient was 7 mmHg. There was mild-to-moderate tricuspid regurgitation, with a peak systolic pressure gradient of 29 mmHg, which suggested mild pulmonary artery hypertension. Transesophageal echocardiography showed a thin transatrial membrane attached to the interatrial septum medially and to the atrial appendage laterally, which divided the left atrium into posterior–superior and anterior–inferior compartments (Fig. 1B). There was flow across this membrane through a fenestration of about 1.5 cm in diameter.
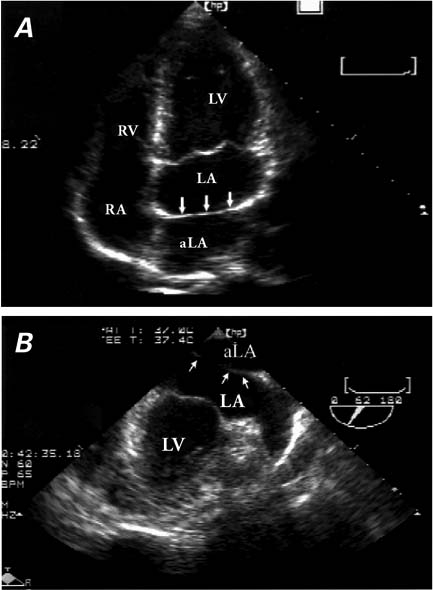
Fig. 1 A) Transthoracic echocardiography (apical 4-chamber view) reveals a membrane (arrows) that subdivides the dilated left atrium into 2 chambers—the true left atrium and an accessory left atrium. B) Transesophageal echocardiography revealsa thin intra-atrial membrane (arrows) attached to the interatrial septum medially and atrial appendage laterally, which divides the left atrium into posterior–superior (accessory left atrium) and anterior–inferior (true left atrium) compartments.
aLA = accessory left atrium; LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle
Subsequently, MDCT (Brilliance 40; Philips Medical Systems, Koninklijke Philips Electronics N.V.; Best, The Netherlands) showed a dilated left atrium with double-chamber conformation, due to the presence of a fibrous membrane between the interatrial septum and the lateral left atrial wall. The opening in the membrane was approximately 1.7 cm in diameter (Fig. 2). The Agatston coronary artery calcium score was zero, and there was no evidence of coronary stenosis. The left ventricular systolic motion was normal. The right ventricular, pulmonary arterial, and pulmonary venous diameters were within normal limits. The MDCT also enabled good visualization of the drainage of the pulmonary veins, all of which were connected to the postero–superior portion of the left atrium. There were no other associated cardiac or aortopulmonary anomalies, such as atrial septal defect, patent foramen ovale, atrioventricular canal defect, left superior vena cava, pulmonary vein stenosis, patent ductus arteriosus, or anomalous pulmonary venous return. The patient underwent surgery 15 months later and recovered well.
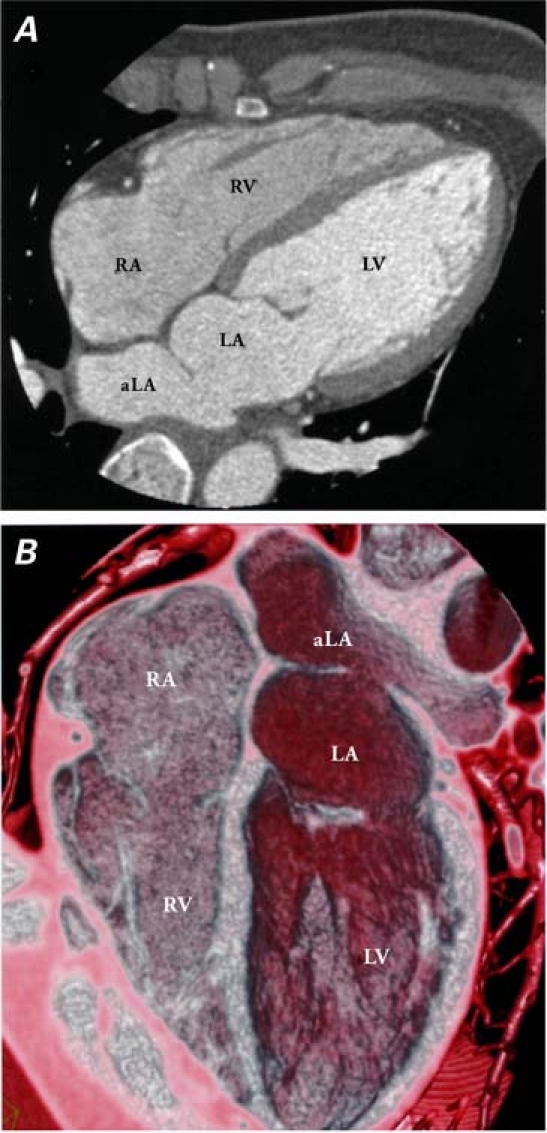
Fig. 2 Multidetector-row computed tomography. A) Four-chamber view reveals an intra-atrial membrane with an opening of approximately 1.7 cm in diameter. B) A 3-dimensional slab volume-rendering image reveals a dilated left atrium with double chambers (an accessory left atrium and a true left atrium), divided by a fibrous membrane between the interatrial septum and the lateral atrial wall.
aLA = accessory left atrium; LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle
Discussion
The ratio of men with cor triatriatum to women with the condition is 1.5:1. A fibromuscular membrane subdivides the left atrium into 2 chambers: the postero-superior chamber (the accessory left atrium) receives blood from the pulmonary veins; the antero-inferior chamber (the true left atrium) contains the left atrial appendage and the mitral valve orifice. Communication usually occurs between the 2 chambers, through 1 or more perforations in the membrane.
Several classification systems exist for cor triatriatum. Perhaps the best accepted is the one developed in 1949 by Loeffler,4 which classified lesions according to the number and size of the orifices in the fibromuscular septum: Group 1 lesions have no opening, and the accessory left atrium drains into the right heart; Group 2 lesions have few and small fenestrations in the membrane, resulting in a high degree of obstruction; and Group 3 lesions have large openings in the membrane, leading to little or no obstruction. The onset of symptoms and clinical manifestations depends on the size and number of the defects within the separating membrane, the morphology of the defects, and the presence of other cardiac anomalies. The most common presenting symptoms in adults are dyspnea, hemoptysis, and orthopnea. Patients in Group 3 can often survive into adulthood with minor or no symptoms, as in the case of our patient. Although cor triatriatum is frequently associated with other cardiac abnormalities, MDCT and echocardiographic evaluation disclosed no associated cardiac anomalies in our patient.
The diagnosis is usually established by TTE,5 TEE,6 or cardiac catheterization.7 Several other techniques, including computed tomography,8 magnetic resonance imaging,9 3-dimensional echocardiography, and intracardiac echocardiography are also useful in diagnosing the condition. Transesophageal echocardiography is superior to TTE because of its better spatial resolution of the left atrium, the left atrial appendage, and the dividing membrane. Multidetector-row computed tomography is a new and powerful imaging technique; however, to date, there have been few reports on the evaluation of cor triatriatum by MDCT.10,11 Chen and Thng10 reported the incidental detection of cor triatriatum in a 46-year-old man by MDCT, in a traditional horizontal cut. Thakrar and co-authors11 reported a case of cor triatriatum that was revealed by 64-slice MDCT, in traditional horizontal and paraseptal views. Our case, though, is unique in that we have delicately reconstructed a 3-dimensional image, which better defines the partitioning membrane with its surrounding structures. In cor triatriatum, MDCT can help the investigator to see a distinct septum in the left atrium, to evaluate the size and number of fenestrations, and to find associated congenital cardiovascular anomalies. This technique also enables the partitioning membrane to be viewed easily, without the risk and discomfort of scope intubation for TEE. Besides, MDCT carries none of the risks associated with invasive cardiac catheterization.
In this report, we have described the case of a 39-year-old woman with cor triatriatum diagnosed by TTE and TEE. The 3-dimensional MDCT reconstruction image showed a distinct septum in the left atrium, which divided the left atrium into an accessory left atrium and a true left atrium, with an opening of approximately 1.7 cm in the membrane. The MDCT also enabled good visualization of the drainage of the pulmonary veins into the accessory left atrium, and it revealed no associated congenital cardiovascular anomaly. On the basis of our findings, we conclude that multidetector-row computed tomography may be a useful tool, as an adjunct to echocardiography, for whole-heart evaluation before operative correction of cor triatriatum.
Footnotes
Address for reprints: Kae-Woei Liang, MD, Cardiovascular Center, Taichung Veterans General Hospital, 160 sec. 3, Taichung Kang Rd., Taichung 407, Taiwan
E-mail: ekwliang@ms17.hinet.net
References
- 1.Niwayama G. Cor triatriatum. Am Heart J 1960;59:291–317. [DOI] [PubMed]
- 2.Reddy TD, Valderrama E, Bierman FZ. Images in cardiology. Atrioventricular septal defect with cor triatriatum. Heart 2002;87(3):215. [DOI] [PMC free article] [PubMed]
- 3.Beller B, Childers R, Eckner F, Duchelle R, Ranniger K, Rabinowitz M. Cor triatriatum in the adult. Complicated by mitral insufficiency and aortic dissection. Am J Cardiol 1967; 19(5):749–54. [DOI] [PubMed]
- 4.Loeffler E. Unusual malformation of the left atrium; pulmonary sinus. Arch Pathol (Chic) 1949;48(5):371–6. [PubMed]
- 5.Slight RD, Nzewi OC, Mankad PS. Echocardiographic diagnosis of cor triatriatum sinister in the adult. Heart 2004;90 (1):63. [DOI] [PMC free article] [PubMed]
- 6.Tantibhedhyangkul W, Godoy I, Karp R, Lang RM. Cor triatriatum in a 70-year-old woman: role of transesophageal echocardiography and dynamic three-dimensional echocardiography in diagnostic assessment. J Am Soc Echocardiogr 1998;11(8):837–40. [DOI] [PubMed]
- 7.Chen Q, Guhathakurta S, Vadalapali G, Nalladaru Z, Easthope RN, Sharma AK. Cor triatriatum in adults: three new cases and a brief review. Tex Heart Inst J 1999;26(3):206–10. [PMC free article] [PubMed]
- 8.Tanaka F, Itoh M, Esaki H, Isobe J, Inoue R. Asymptomatic cor triatriatum incidentally revealed by computed tomography. Chest 1991;100(1):272–4. [DOI] [PubMed]
- 9.Ibrahim T, Schreiber K, Dennig K, Schomig A, Schwaiger M. Images in cardiovascular medicine. Assessment of cor triatriatum sinistrum by magnetic resonance imaging. Circulation 2003;108(15):e107. [DOI] [PubMed]
- 10.Chen K, Thng CH. Multislice computed tomography and two-dimensional echocardiographic images of cor triatriatum in a 46-year-old man. Circulation 2001;104(17):2117. [DOI] [PubMed]
- 11.Thakrar A, Shapiro MD, Jassal DS, Neilan TG, King ME, Abbara S. Cor triatriatum: the utility of cardiovascular imaging. Can J Cardiol 2007;23(2):143–5. [DOI] [PMC free article] [PubMed]


