Abstract
The necessity to develop cardiac surgery centers in the emerging world is widely accepted. Numerous groups and organizations from the developed world are involved in such work; however, the best method in which to develop a sustainable center in the emerging world is still debated. Herein, we present an approach that we have used in several such projects, which involves regular and frequent instructional visits with progressive reduction of our instructional support. Data to support our approach are presented.
Key words: Cardiovascular surgical procedures/statistics & numerical data; developing countries; international cooperation; medical missions, official; outcome assessment (health care); thoracic surgery/education; world health
In recent years, considerable attention has been given to medical care accessibility throughout the world, not only in the field of communicable diseases and public health, but also in more technical specialties such as cardiac surgery. The world today is populated by some 6.5 billion inhabitants, of which number approximately 1 billion live in the developed world and 5.5 billion in developing areas that lack ready access to many medical specialties.
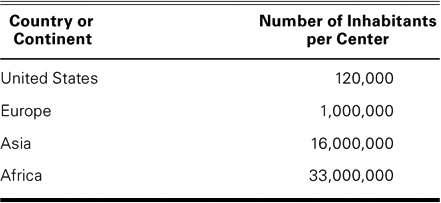
There is much debate in cardiac surgical societies concerning how to achieve a better distribution of cardiac surgery services in these countries. Attention was first drawn to this problem at a major international meeting by Dr. James L. Cox in his presidential address to the American Association for Cardiothoracic Surgery in San Diego in 2001. He spoke eloquently of the various needs for cardiac surgery in developing countries and of the urgent need to act.1 He also presented figures concerning the highly uneven distribution of cardiac surgery centers in the world, which are shown in Table I.
Table I. Distribution of Cardiac Surgery Centers around the World
Others have also reported their approaches, experiences, and thoughts on the problem. Among them is Dr. Thomas Pezzella, who has devoted much time to heart surgery in China.2 He is associated with the World Heart Foundation, which was founded in 1999 to help develop cardiac surgery in the emerging world. Its approach is essentially oriented toward teaching via the Internet, although Dr. Pezzella has made many teaching visits to emerging nations.
Ghosh3 has presented his extensive hands-on experience, describing the multiple phases of the projects with which he has been involved. The European Association of Cardiothoracic Surgery and its International Committee, on the other hand, does not believe that the best solution is achieved by sending teams to the developing world.
Teamwork is particularly important in cardiac surgery, because the weakest link can determine the ultimate results. A star surgeon cannot perform without adequate support from anesthesia, perfusion, and postoperative care, or without a precise preoperative diagnosis. This team approach renders training in our specialty difficult in countries where there are no established or experienced training centers; foreign aid becomes mandatory.
The training of foreign residents in developed countries is not easy. Busy, well-organized centers are too preoccupied with their own daily business to train a foreign resident. Furthermore, if and when trainees return to their own country, initiation of a program is difficult, because no infrastructure and no team are ready. Training of a complete team from a developing country in a foreign center is even more cumbersome, complex, and expensive, and is often impossible without an established vision of the future that is adapted to local needs.
The alternative is transmitting knowledge within the developing country itself by making regular and frequent visits to a selected center and performing surgery with the aid of local specialists. This alternative manner of training has the further advantage of giving immediate high-quality care to the local population, which is usually sorely in need, because there is often a huge backlog of patients. This is the approach that we have used since 1998 and would like to describe herein.
We are reporting on an overall 10-year experience in 4 projects in 4 different countries, but for simplicity's sake we will focus on our latest project in Tbilisi, the capital of Georgia, a former republic of the Soviet Union now independent (since 1991). This last project was completed recently. We will first describe the numerous stages of such projects and then describe a simple evaluation of the results of the project in Tbilisi.
Materials and Methods
Location of Projects
Our projects were in Sarajevo (Bosnia and Herzegovina) from 1998 through 2002; in Skopje (Macedonia) from 2000 through 2004; in Algiers (Algeria) from 2002 through 2004; and in Tbilisi (Georgia) from June 2002 through December 2007. Over these 10 years and within the context of these 4 projects, more than 100 one-week visits were made and more than 1,200 patients were operated upon in these countries. The same method was used in all 4 projects, although the situations were not exactly the same: in Bosnia and Macedonia there was no center for cardiac surgery at all before our arrival, whereas in Georgia facilities and some junior staff for cardiac surgery existed but were not functioning, and Algeria requested training in coronary surgery only. Some projects were carried out in public hospitals (government-owned), others in privatized hospitals (government-owned but with private investment and government-insurance reimbursement). The language used for communication in most countries was English, except for Algeria, where French is spoken.
Teamwork
An exploratory visit is made to establish contacts with government representatives and health ministries and to ensure local support if the invitation did not originate from governmental sources directly. During this visit, the levels of local experience and knowledge are assessed and the available equipment is examined and tested. A long-term project is proposed for a duration dependent upon the level of local expertise, and a team of fully trained specialists is proposed for regular visits, the composition of the team depending on the local needs.
A cardiologist is included, primarily for invasive diagnosis, if one is not available locally. The proposed cardiovascular surgical team is made up of a surgeon, an anesthetist, a perfusionist, a scrub nurse, an intensive care nurse or a respiratory therapist (or both), and a ward nurse, if necessary. Most of the members of the team are associated with the Hôpital de la Tour in Geneva and take leave voluntarily with the permission of the management of the hospital, but with no loss of salary.
In most projects, our team was the only foreign visiting team training the local staff; in Tbilisi, visits to the same hospital were made by other groups, but much less frequently. These other groups performed 10% of the volume of surgery that we had done and made one tenth of the number of visits.
The plan is to progressively reduce the visiting team as skills and knowledge are acquired by the local specialists, according to evaluations that are made regularly.
Frequency
We always made monthly visits, usually of 1 week's duration, and this 10 times a year. With this frequency, the local staff had time to admit patients and to discharge them after the departure of the visiting team. This frequency also enabled the local team to remember the techniques and routines, which is not the case if visits are too far apart. This was all the more true in those projects in which no surgery was performed between our visits—at least not early in the project.
Caseload
A sufficient number of cases is mandatory if the intention is to render the local staff independent. However, as we have said, in most developing countries there is a huge backlog of cases, but financing surgery for so many patients may be a problem. In Sarajevo, for example, our foundation participated in the cost of diagnostic procedures and surgical treatment to afford patients free access to cardiac surgery. Patients are supplied through regular contacts and meetings with the local diagnostic team. Usually, at the beginning of each project, 2 cardiac cases are scheduled daily; later, as experience increases, a 3rd and even a 4th case can be performed in a day. However, the teaching process requires time, and excessive caseloads are deleterious to teaching. Therefore, we prefer to handle 10 to 12 cases in a week's sojourn, allowing time for bedside rounds, teaching, and meetings with the cardiology staff to review newly diagnosed cases for future visits.
The Local Team
In all the described projects, we did not have the possibility of selecting the local team. In several instances, however, we did suggest dismissing certain individuals, who, after a trial period, we judged incompetent and not adapted to cardiac surgery, and we similarly questioned the necessity of training excessive numbers of surgeons and anesthetists. To acquire sufficient hands-on experience, the number of surgeons and anesthetists must be limited, as has been suggested by others.3
Equipment
In all of these countries, the local authorities definitely wanted to initiate, develop, or improve cardiovascular medicine—cardiac surgery in particular. Investment for the acquisition of equipment was made by the local hospital or governmental authorities. The ordering of disposable material was also left to the local hospital administration. This was considered evidence of the transient role of the visiting team—that is, it enabled the locals to learn how and where to obtain the necessary cardiologic, anesthetic, and surgical material for daily use with the visiting team, and also for use once the local team took over. Advice was available from the visiting team, and suggestions regarding the choice of equipment were made by us when requested.
Donations of used equipment came from hospitals and companies with which we have contacts at home—especially after the projects had gained momentum and results could be demonstrated, to show the donors that the projects were worthwhile and sustainable.
Financing
The initiation of projects varied. In Bosnia and Algeria, we were invited by the government, which wished to initiate cardiac surgery or coronary surgery. In Macedonia and Georgia, hospital authorities requested our collaboration. In this manner, financial support varied from 1 project to another: some projects were government-sponsored; in others, charitable foundations, which we had founded, were used. In the course of our experience, 2 foundations have been created (The Medaid Foundation and the Frederic and Jean Maurice Foundation) to help support the projects and enable us to offer expertise without expense to the recipients. The latter foundation supported the project in Tbilisi. However, with time and experience, we also discovered that it is not always beneficial for the purpose of teaching and transmission of knowledge, to make projects totally free of charge. In some countries and in some settings, hospital authorities do not encourage teaching if patient care can be given by experienced foreign physicians at no charge. We now encourage joint ventures between the local government or hospital and our foundations, the prices of services being minimal and adapted to local standards, but not totally free.
Reducing the Visiting Team
One of the key features of the projects was to progressively reduce the number of visiting team members in order to give the local staff responsibility and lead them to total independence. As soon as possible, local personnel were given the opportunity to conduct anesthetic or other procedures and to perform surgery in the presence of the visiting surgeon. The size of the visiting team was reduced on the basis of a review of a week's work abroad, once the participants had returned home. Often, the local staff requested supplementary visits by one or another member of the visiting team to teach refinements, and these were always granted.
Results
Visits and Cases
In all the projects, we tried to visit monthly for at least 1 week at a time, at least 10 times a year. We believe that repeated visits are necessary to teach the local team and then to help it maintain its new skills. Usually, 2 cases were scheduled for surgery each day, which provided time for anesthetic preparation and the teaching of anesthesia, in addition to the teaching of surgery. In some instances, the pressure of a large waiting list forced more cases onto the program, but this was avoided when possible for the benefit of education. The weekly organization and the selection of cases were done in such a way that more complex cases (which required extra postoperative care) were performed first, at the beginning of each week. We usually left the simpler cases to the postoperative care of the local team after our departure for home. As the projects advanced, we had to adapt these rules, because when the caseload became greater, a greater number of difficult cases was accepted for surgery, and the local teams started operating on their own.
The total caseload in the Tbilisi project is shown in Figure 1. Note that the project was initiated late in 2002 and that only 3 visits were made that year, whereas by 2007 the local team was operating during the periods between our visits, which led to a much higher volume of surgery than is shown. It is interesting to see that the caseload per week increased as the project progressed (Fig. 2). This is explained not only by better teamwork inside the center, but also by outside factors such as additional governmental support and a greater demand for surgery as the confidence of patients increased.

Fig. 1 Evolution of annual caseload during project in Tbilisi, 2002–2007.
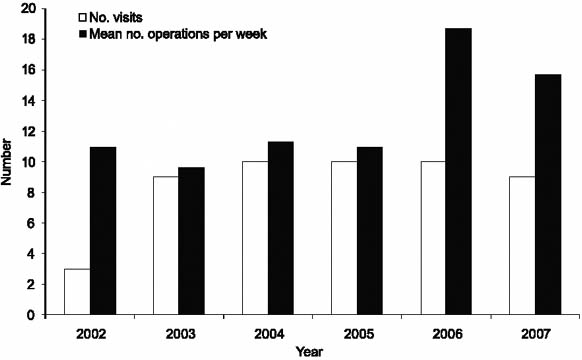
Fig. 2 Evolution of weekly caseload, Tbilisi, 2002–2007.
We undertook, with no selection bias, all cases referred to the hospital, save for patients who could be treated by percutaneous interventions, who did not require surgery according to American Heart Association guidelines, or who were at excessive operative risk.
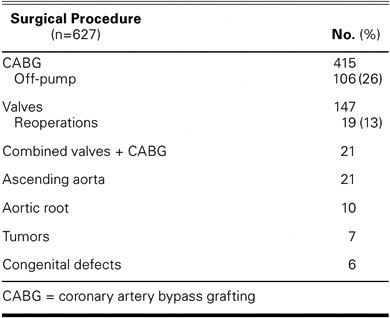
The types of operations performed during the whole project period are shown in Table II.
Table II. Breakdown by Type of Procedure: Total Caseload during the Tbilisi Project, June 2002 through December 2007
Reduction of the Visiting Team
Because the aim of the projects was the independent management of surgical patients by the local staff, we strove to reduce the visiting team as quickly as was feasible within the constraints of patient welfare. The progressive reduction of our team during the project in Tbilisi from 2002 through 2007 is shown in Figure 3. In Tbilisi, the visiting nursing staff was withdrawn first, then the perfusionist, and then the anesthetist, which left the surgeon alone during the last 2 years of the project. A similar reduction schedule was followed in our other long-term projects.
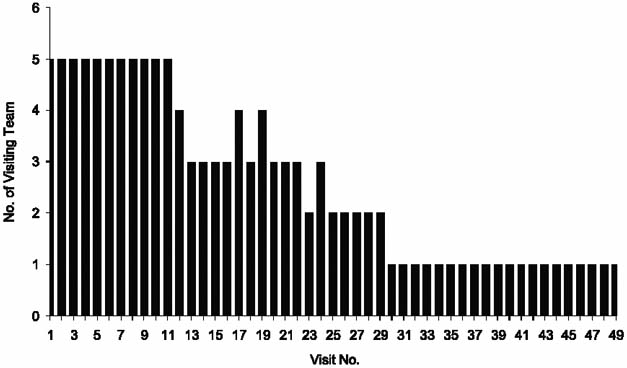
Fig. 3 Reduction in number of team members, Tbilisi, 2002– 2007.
During this progressive reduction in the visiting team, the local team was encouraged to make therapeutic decisions from the very beginning, be it in the operating room or in the intensive care unit. The surgeons were put in charge of patients and performed surgery progressively with the assistance of the visiting surgeon, or only in the passive presence of the (non-scrubbed) visiting surgeon.
Finally, in February 2007, the local staff was allowed to start operating in the absence of the visiting team, and in the course of the last 10 months of that year, 127 operations were performed by the local team, with 2 deaths or a mortality rate of 1.6%. The local surgeon performed mainly coronary surgery and, later, started valve surgery in progressive steps.
The volume of surgery, types of operations, and results are shown in Table III.
Table III. Summary of Surgical Activity of Georgian Team without Foreign Assistance, February through December 2007

Objective Evaluation of the Local Team and of Results Obtained
In the course of the project in Georgia, we formally evaluated the results of surgery in order to gauge the risks of reducing the visiting team. We reviewed the phases of our project and looked at the patients' mortality rates as predicted by the Euroscore system with reference to the weekly caseload, length of intensive care unit stay, and total hospital stay. We also looked at the frequency of off-pump coronary surgery, which is reputedly difficult to teach. For the purposes of this study, we divided the duration of the project into 3 periods—A, when the full visiting team was present; B, when the transition was taking place; and C, when the visiting team gave minimal support. The complete team consisted of 5 members, and we determined the average number of team members present during each period under study.
Our study, as shown in Table IV, confirms that there were no deleterious effects (in regard to mortality or morbidity rates) associated with progressively conferring the responsibility of patient care upon the local team.
Table IV. Comparison of Predicted Mortality by Euroscore and Observed Mortality, Tbilisi, 2002–2007
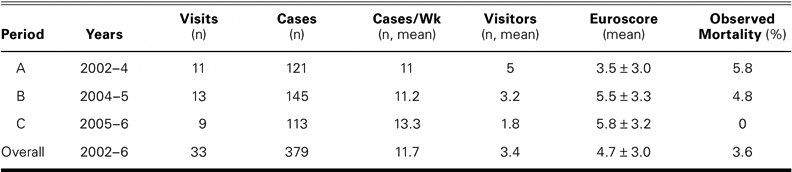
The Euroscore was calculated by the standard arithmetic model as described by Roques and colleagues.4
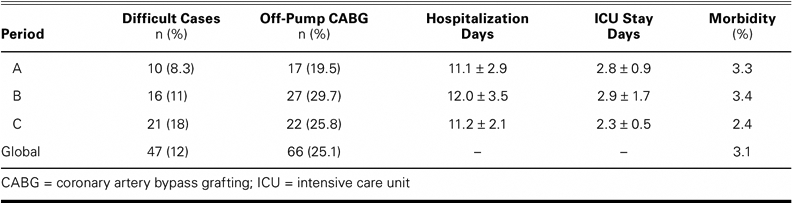
We also reviewed the durations of stay in the hospital and intensive care unit, the morbidity (defined as intubation of more than 36 hours, deep wound infection, or postoperative dialysis), and the incidence of off-pump coronary surgery. Furthermore, we ranked cases by a simplified qualitative method into difficult and routine: difficult cases were defined as those involving a left ventricular ejection fraction < 0.35, double or triple valve replacement, severe pulmonary hypertension, aortic surgery, or reoperation. The results, shown in Table V, confirm progressive increases both in caseload and in the difficulty of cases treated as the project advanced, but no increase in the durations of stay, either in the intensive care unit or in the hospital as a whole. Furthermore, a tendency towards more frequent off-pump surgery was observed.
TABLE V. Comparison of Morbidity and Duration of Hospital and ICU Stays over the Course of the Project in Tbilisi, 2002–2007
Discussion
The project was terminated in December 2007: regular visits stopped after the Georgian team, working alone during the last 10 months of the year, showed itself to be effective and safe. We proposed in the future to maintain a supportive relationship by assisting in difficult cases only. Two such visits were made by our surgeons, who contributed to only 23 out of a total of 204 operations performed between January and August 2008. Furthermore, for the purpose of primary prevention (which is underdeveloped in Georgia), our foundation is currently sponsoring an epidemiologic study of the siblings of patients who underwent operation for coronary disease during the 5.5 years of our surgical project.
Our experience in Georgia confirms, in our minds, that teaching heart surgery can be done locally and can lead to sustained independence in emerging nations. In the course of this period in Georgia, more than 700 patients benefited from surgery that they would not have undergone, had the teaching been done in Europe. Furthermore, our data support the safety of our teaching method for local patients and its effectiveness in the training of local staff. Many of the younger local staff members had never performed surgery or anesthesia, and 5 years later they were doing so alone, notwithstanding the intermittent nature of the program. We were pleased to see that the local staff remained stable and that relatively few changes occurred during the project.
We were fortunate in Georgia to have had an understanding and competent hospital management and a very hard-working and devoted local team, and to have avoided—by luck, experience, and multiple brief interventions—the many possible pitfalls of such projects. In our previous experiences in other countries, we had occasionally encountered noncooperation from the local staff or management, and jealousy, incompetence, and corruption, among a variety of other problems. All of these, combined, often led to the slowing and sometimes to the failure of the project.
Conclusion
We are convinced that the method described here can be recommended. Doubtless, other ways of teaching hospital staff and of organizing cardiovascular surgery centers in emerging nations can also be applied with success. It should be the role of professional societies—with the assistance of forums such as the World Health Organization and the World Heart Foundation—to evaluate, recommend, and endorse the multiple possible approaches for the task. In this manner, these institutions can suggest the best techniques, thereby enabling the multiplication of efficient projects in the developed world.
Footnotes
Address for reprints: Vladimir Velebit, MD, Cardiovascular Department, Hôpital de la Tour, 3 Ave JD Maillard, 1217 Meyrin-Geneva, Switzerland
E-mail: vvelebit@latour.ch
The project described herein was made possible by the financial support of the Frederic and Jean Maurice Foundation, Geneva, Switzerland (http://www.fondationmaurice.org).
Presented in part at the 15th International Symposium of the Denton A. Cooley Cardiovascular Surgical Society, Houston, Texas, 25–27 October 2007.
References
- 1.Cox JL. Presidential address: changing boundaries. J Thorac Cardiovasc Surg 2001;122(3):413–8. [DOI] [PubMed]
- 2.Pezzella AT. Progress in international cardiac surgery: emerging strategies. Ann Thorac Surg 2001;71(2):407–8. [DOI] [PubMed]
- 3.Ghosh P. Setting up an open heart surgical program in a developing country. Asian Cardiovasc Thorac Ann 2005;13(4): 299–301. [DOI] [PubMed]
- 4.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg 1999;15(6): 816–23. [DOI] [PubMed]


