Abstract
Objective:
To identify the coping strategies used by adults with pediatric-onset spinal cord injuries (SCI) and to determine how these coping strategies were related to demographics, injury-related factors, and adult outcomes.
Methods:
Study Participants were adults who sustained SCI at age 18 years or younger and were interviewed at age 24 years or older. This is part of a large longitudinal study for which there were 864 eligible participants. There were 353 (41%) interviewed, 259 of which were assessed for coping skills. The telephone interview included a questionnaire and several standardized measures (Functional Independence Measure, Craig Handicap Assessment and Reporting Technique, Short-Form 12 measure of health-related quality of life, Satisfaction With Life Scale, Patient Health Questionnaire-9, and the Brief COPE adapted).
Results:
Of 259 participants, 62% were male and 58% had tetraplegia. The average age at injury was 14 years (0–18 years) and average age at interview was 30 years (24–42 years). Of 8 coping strategies assessed, 99% of participants used acceptance, 94% used positive reframing, 93% used active coping, 89% used emotional support, 89% used humor, and 74% used religion. The negative coping skills of behavioral disengagement and substance use were used by 28% and 15%, respectively. A hierarchical regression analysis was used to predict higher adult life satisfaction by using the positive coping strategies of seeking emotional support, acceptance, and religion; it was negatively associated with substance use.
Conclusions:
Positive coping strategies tend to be used by a majority of adults with pediatric-onset SCI, and several coping styles are associated with greater life satisfaction.
Keywords: Spinal cord injuries, pediatric onset; Adolescence; Tetraplegia; Paraplegia; Coping skills; Life satisfaction; Functional assessment; Quality of life
INTRODUCTION
It is easily assumed that when stressful events occur, the strategies individuals use to cope with these events will ultimately impact the outcomes of their lives. The work of Folkman and Lazarus has provided a useful foundation for studying the process of coping (1–3). These authors and their colleagues suggest that there is first a cognitive appraisal process through which a person evaluates the stressful event to determine if it threatens their well-being. If they are threatened, they may use various ways of coping. Coping is defined as a person's constantly changing cognitive and behavioral efforts to manage the stress (1). Folkman and Lazarus showed that more or less successful outcomes are associated with differences in coping strategies (1). These authors have emphasized, however, that although associations may be identified between coping and outcomes, it may not be clear which is the cause and which is the effect (2,3).
Spinal cord injuries (SCI) are clearly challenging and threatening events to individuals when they occur. Using some of the assessment techniques and theories of Folkman and Lazarus, Frank and his colleagues studied the coping strategies of individuals with SCI and found differences in coping strategies among those with more and those with less psychological distress (4). This work was extended further in another study, which identified that those individuals who were more distressed were likely to use, for example, wish-fulfilling strategies, self-blame, and emotional expression strategies compared with others who were less distressed (5). Another group of researchers compared coping strategies used by individuals 6 weeks after injury and strategies used by another group of individuals 4 to 7 years after injury and reported some differences in the coping strategies but emphasized a need for longitudinal studies (6). In 2000, this research group published a longitudinal study of individuals with SCI who were followed at several points during initial rehabilitation and for 24 months after discharge (7). They found significant stability in types of coping styles over time. That group also initiated a controlled study to determine whether teaching strategies of coping would improve adjustment and found reduced anxiety and depression in the treatment group compared with the control group (8). Other studies have continued to identify the types of coping strategies that seem to result in better outcomes. For example, in a report of Swedish patients, acceptance, “fighting spirit,” and seeking social support were all associated with more positive outcomes than was dependence or helplessness (9).
The above studies focused on individuals who were primarily injured as adults. For individuals who are injured as children or adolescents, there is little known about coping style with regard to demographics, severity and age of injury, or outcomes, nor is it clear whether adults with pediatric-onset SCI would typically use the same coping styles as those injured as adults. When young children sustain SCI, their coping strategies are limited to those available at their developmental level and presumably change as their cognitive skills mature (10,11). For example, as children reach adolescence and develop formal operational thinking, they are less concrete and able to view situations from many perspectives. This would allow them to envision more varied coping options. In addition, throughout their years of development, the coping strategies of children and adolescents may be influenced by the strategies used or encouraged by their caregivers or other adults in their lives. By the time children and adolescents with SCI enter adulthood, they have had years of experience in coping with SCI, although not in relation to the demands of the adult world. The goal of this study was to identify the coping strategies used by adults with pediatric-onset SCI and to determine how these coping strategies are related to the adult outcomes of these individuals. This study is part of a larger project to assess adult outcomes of individuals with pediatric-onset SCI (12–15). However, until the present study there have been no published reports of the relationship between coping strategies and the outcomes of employment, community participation, independent living, and life satisfaction in this population.
METHODS
Eligible study participants were individuals who sustained an SCI at age 18 years or younger, were 24 years or older at follow up, were capable of understanding and responding to the questions, and were living in the United States or Canada. All individuals who had received care at the SCI programs of a single hospital system were potential participants for this study. Care was provided free of charge, and there were no financial or insurance restrictions. Patients were permanently discharged from the system when they reached the age of 21 years.
Of all 864 participants eligible for the overall long-term outcome study, a search was completed on 594. Of those, 365 (61%) completed interviews, 96 (16%) were lost to follow-up, 51 (9%) died, and 82 (14%) refused to participate. Of the 365 interviewed, 259 individuals completed the Brief COPE because it had been added to the follow-up protocol in 2003.
Procedures
This project was approved by the Institutional Review Boards of our hospitals, and all institutional regulations concerning the ethical use of human volunteers were followed during the course of this research. Eligible patients were identified and contact information sought by using the following methods: review of contact information from medical charts; performance of a computer search of white pages directories, such as TheUltimates.com, and the Social Security Death Index; and search by a professional search service. Each patient contacted was informed of the purposes, procedure, confidentiality, and voluntary nature of participation in the study. After obtaining signed informed consents, the participants were enrolled in the study and interviewed by telephone. All interviews were conducted by research assistants who had not participated in the care of the patients. In addition, medical chart reviews and the Shriners Hospitals for Children SCI database were used to obtain injury-related information, such as level of injury, completeness of injury, and date of injury.
Instruments
A structured questionnaire designed for this study was used to determine demographic information, such as employment status and living situation. Standardized measures were also used, all of them commonly applied to SCI populations. Information on the reliability and validity of the measures is included in the references. Impairment was measured using the ASIA motor score and the level of injury (paraplegia or tetraplegia) as defined by the International Standards for the Neurological Classification of Spinal Cord Injury (16). The ASIA motor score is the sum of the muscle grades (range of 0–5) for each of the key muscles on both sides of the body. ASIA motor scores range from 0–100. Functional limitations were assessed with the motor portions of the Functional Independence Measure, which was administered by telephone using the standard instructions for the FONE FIM (17–19). This administration included 13 items assessing self-care, mobility, and sphincter control. A 7-point scale is used to identify the level of independence with which an individual performs each activity. Higher scores indicate more functional independence. Health status was assessed with the Short-Form 12, which includes 12 questions from which mental and physical component scores are generated (20). This standardized measure assesses an individual's perception of health, with higher scores indicating greater perceived health. Each of the component scores has a mean of 50 and a range of about 10 to 70 in the normative population. Community participation was measured by the Craig Handicap Assessment and Reporting Technique (CHART) (21–23). The CHART produces a total score as well as scores for 6 separate subscales: physical independence, cognitive independence, mobility, occupation, social integration, and economic self-sufficiency. The physical independence subscale assesses how much assistance one needs and takes into account those who are able to direct their own care as being more independent than those who cannot. The cognitive independence subscale assesses amount of assistance needed for cognitive problems, such as remembering, decision making, and judgment. The mobility subscale assesses ability to move about effectively in the community, including being able to go when and where the individual wishes. The occupation subscale assesses how individuals productively use their time, including school, work, household activities, volunteer activities, and hobbies but not including such activities as watching television and sleeping. The social integration subscale assesses the ability to participate in and maintain adult social relationships. The economic self-sufficiency subscale assesses the ability to maintain customary financial independence. Each dimension is scored on a 100-point scale, with higher scores indicating greater community integration. Perceived global life satisfaction was assessed with the Satisfaction With Life Scale (SWLS) (24). This scale consists of 5 statements that individuals rate on a 7-point scale (strongly disagree to strongly agree), with higher scores reflecting more satisfaction.
To assess depression, the screening tool Patient Health Questionnaire-9 was used (25). This tool consists of 9 statements that reflect the diagnostic elements of depression as given in the Diagnostic and Statistical Manual (26). Participants are asked to score each item based on how much they have been bothered by the issues raised in the item over the past 2 weeks: not at all (0), several days (1), more than half the days (2), or nearly every day (3). Either a total score or a category score can be used. Category scores are determined by the total score divided into the following: no depressive symptoms (0), minimal depressive symptoms (scores 1–4), mild depressive symptoms (scores 5–9), moderate depressive symptoms (scores 10–14), moderate/severe depressive symptoms (scores 15–19), severe depressive scores (scores 20–27).
A modified version of the Brief COPE was used to assess the relative importance of each of 8 different coping strategies (27). The decision to modify the Brief COPE by assessing 8 rather than 14 coping strategies was made in accordance with the instructions of Carver, Brief COPE's author, who suggests that, to reduce the time burden of responders, selective coping strategies may be assessed (27). The 8 selected were deemed particularly relevant to this population based on the clinical experience of the investigators. The participants in this study were asked, “What ways do you use to cope with having a spinal cord injury?” Each strategy was defined by 2 statements that participants rated by the following response scale: (a) “I don't do this at all,” (b) “I do this a little bit,” (c) “I do this a medium amount,” (d) “I do this a lot.” Although only 2 items were included for each strategy, the author of this instrument has demonstrated reliability of responses over 3 administrations (27). This study assessed the relative importance of the following 8 coping strategies: (a) Acceptance: “I've been accepting the reality of the fact that it happened” and “I've been learning to live with it.” (b) Positive reframing: “I've been trying to see it in a different light to make it seem more positive” and “I've been looking for something good in what happened.” (c) Active coping: “I've been concentrating my efforts on doing something about the situation I'm in” and “I've been taking action to try to make the situation better.” (d) Religion: “I've been trying to find comfort in my religion or spiritual beliefs” and “I've been praying or meditating.” (e) Using emotional support: “I've been getting emotional support from others” and “I've been getting comfort and understanding from someone.” (f) Humor: “I've been making jokes about it” and “I've been making fun of the situation.” (g) Behavioral disengagement: “I've been giving up trying to deal with it” and “I've been giving up the attempt to cope.” (h) Substance use: “I've been using alcohol or other drugs to make myself feel better” and “I've been using alcohol or other drugs to help me get through it.”
Data Analysis
Descriptive analyses were used to characterize the sample. Group mean scores were generated for each of the 8 coping strategies. The scores for each of the 2 statements in each coping style were summed, producing a range of scores 2 to 8 for each coping style for each individual. The percentage of individuals who used a coping strategy (whether a little, a medium amount, or a lot) on either of the 2 items was calculated. Relationships of coping strategies with demographic or severity or age of injury and outcomes were determined by t tests or Pearson correlations. To adjust for multiple analyses, the more conservative P value of <0.005 instead of <0.05 was used to indicate significance. In addition, multiple regression analyses were used to determine the relative predictive value of coping strategies compared with other independent variables for 4 outcomes. Correlations between coping styles were assessed and multicollinearity was not a problem. In addition, the residuals of the dependent variables of the linear regressions were examined and met the criteria for normality. For the outcomes of SWLS and CHART total, hierarchical multiple linear regression analyses were used, to determine how much additional variance would be contributed by adding coping strategies. For independent living and employment, logistic regression analyses were used. Independent living was defined as living away from the parents, and employment was defined as either part-time or full-time employment as reported by the participant during the interview. The independent variables used, in addition to the coping strategies, in the regression for life satisfaction were gender, age at injury, age at interview, level of injury (tetraplegia or paraplegia), ASIA motor score, Functional Independence Measure motor score, Short-Form 12 mental and physical component summary scores, education (college degree or not), employment, independent living, marriage, driving, and 5 CHART subscales (excluding economic self-sufficiency). The subscale of economic self-sufficiency was excluded because so many individuals did not respond to that subscale. The same factors were used in the regression for CHART total, except the CHART subscales were excluded. Logistic regression analyses were conducted for the outcomes of employment and independent living. For independent living, the same factors were used as for life satisfaction, except independent living and marriage were excluded. For employment, the same factors were used as with life satisfaction, except that the occupation subscale of the CHART was excluded. It should be noted that in some cases, such as with the CHART and independent living, some measures that are outcomes were also used as independent variables for other outcomes. The analyses were conducted using the SPSS statistical package 11.5.
RESULTS
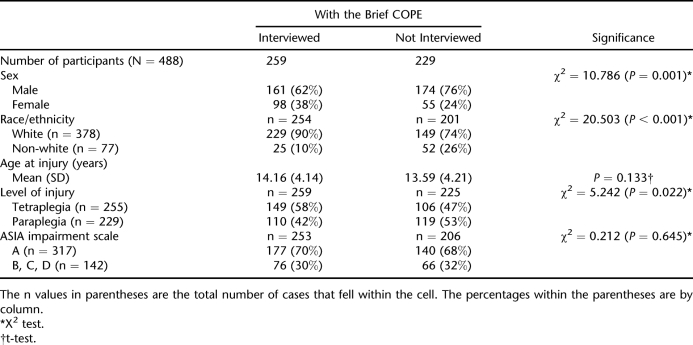
A description of the participants and a comparison of those interviewed compared with those eligible but not interviewed is included in Table 1. Of 259 participants, 62% were male, 90% were white, 58% had tetraplegia, and 70% had complete injuries. Those interviewed were more likely to be female, to be white, and to have tetraplegia than those not interviewed. Table 2 shows mean scores for each of the coping strategies, listed from highest to lowest; higher mean scores represent strategies that individuals report that they are most likely to use.
Table 1.
Comparison of Those Interviewed With Those Not Interviewed
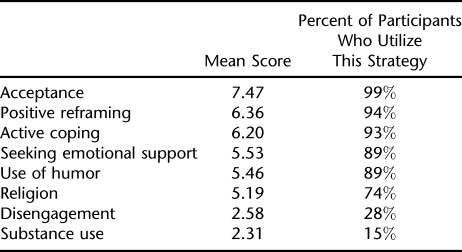
Table 2.
Coping Strategies
Acceptance, positive reframing, and active coping have the highest mean scores. The lowest mean scores are for the negative coping strategies, behavioral disengagement, and substance use. The percentage of participants who use a coping style at all (whether they use it a little, some, or a lot) is also reported. The majority of participants report using acceptance, positive reframing, active coping, emotional support, humor, and religion. Many fewer use behavioral disengagement and substance use.
The association of particular coping strategies with demographic factors and factors related to injury was also analyzed. Women were significantly more likely (t = 3.165, P = 0.002) to use emotional support than men were, and men were more likely (t = 3.492, P = 0.001) to use humor than women were. Individuals who were older at interview and those with a longer duration of injury were more likely to use acceptance (Pearson correlations 0.205, P = 0.001 and 0.186, P = 0.003, respectively). Race, age at injury, level of injury (tetraplegia or paraplegia), and completeness of injury were not associated with any of the coping strategies.
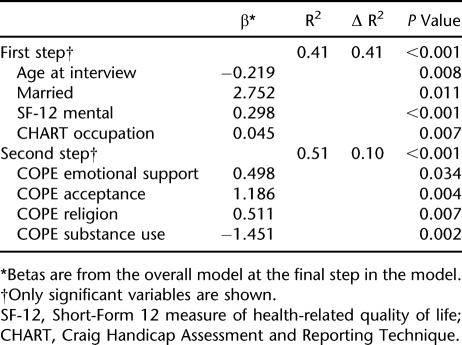
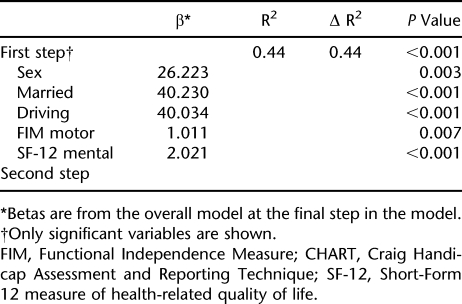
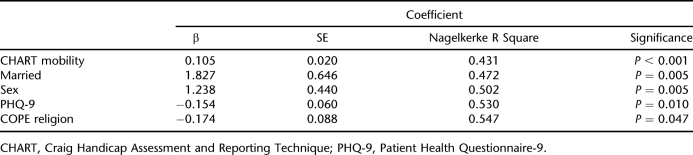
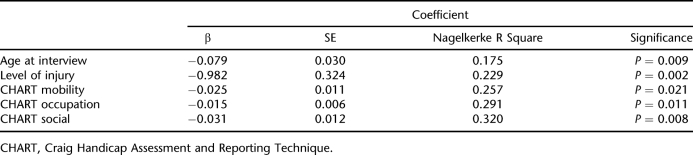
Multiple regression analyses were conducted for 4 adult outcomes: SWLS, CHART total, employment, and independent living. For SWLS, predictors included 4 coping strategies: religion, emotional support, substance use, and acceptance (Table 3). The total model accounted for 51% of the variance, with the coping strategies contributing 10%. For CHART total, no coping strategies were included in the model (Table 4). For the outcomes of employment (Table 5) and independent living (Table 6), logistic regression analyses were used. For employment, the only coping strategy that entered the model was religion, adding about 2% to the total variance in the model that accounted for 55% of the variance. However, that was a negative association such that those unemployed were more likely to use religion as a coping strategy. No coping strategies were predictive of independent living.
Table 3.
Hierarchical Multiple Linear Regression for Satisfaction With Life Scale
Table 4.
Hierarchical Multiple Linear Regression for CHART Total
Table 5.
Multiple Logistic Regression for Employment
Table 6.
Multiple Logistic Regression for Independent Living
DISCUSSION
There are similarities in the types of coping strategies that most individuals with pediatric-onset SCI in this study report using. The vast majority use positive rather than negative coping strategies, and 99% use the strategy of acceptance at least part of the time. More than 90% use positive reframing and active coping. In contrast, the negative strategies of disengagement and substance use are used by only 28% and 15%, respectively. These findings are similar to the findings of a study of adult-onset SCI, in which the most used strategies were also positive; in that study and the present one, the most commonly used strategy was acceptance (7). Furthermore, in that study, behavioral disengagement and substance use were among the least used strategies, which is true of the present study. This suggests that whether an SCI occurs in childhood or adulthood, the adult mechanisms for coping with the injury may be similar.
A key finding of this study is that certain coping strategies are associated with the outcome of life satisfaction in these adults with pediatric-onset SCI. Those strategies are seeking emotional support, accepting the reality of the injury, and using religion or spirituality. Substance use was also significantly associated, although in a negative manner; therefore, greater substance use is associated with less life satisfaction. These findings are not surprising to health care professionals, but they provide concrete data to help direct clinical treatment and education for future patients who have sustained an SCI and for their families. Many investigators have postulated that subjective life satisfaction or quality of life is the most important outcome to assess when measuring treatment effects, because a person's own overall view of their life can be seen as the gold standard of outcome measurement for that individual (28,29). Calling attention to ways of coping that may lead to greater life satisfaction is an important issue. The findings of this study, however, specify associations and not cause-and-effect relationships. For example, less life satisfaction might lead to substance use rather than the reverse.
In the multiple regression analyses, no coping strategies were significantly associated with the outcomes of community participation as measured by the CHART or independent living, and employment was only negatively associated with one coping strategy (religion). Other investigators have shown that coping strategies are associated with psychological outcomes, such as depression and anxiety after SCI in adults (6,30). Previous work of the present investigators has shown a relationship between depression and some aspects of community participation of adults with pediatric-onset SCI (31). For example, the CHART occupation subscale, measuring employment and other meaningful activity, was a predictor of depression. That is, a lower score on the occupation subscale was a predictor of greater depression. Further studies are needed to understand the links that may connect coping with all of these psychological and participation outcomes.
Demographic and SCI factors were seldom associated with coping styles. Women were more likely than men to seek emotional support in coping, but this gender difference has been reported for women without disabilities as well (32). Men were more likely to use humor than women as a means of coping. There was not a strong association between gender and acceptance, although other studies have found that women with SCI are more accepting of the injury than men are (33).
Older age at interview and longer duration of injury were both associated with greater use of acceptance in coping. Longer duration of injury has previously been reported to be associated with greater acceptance and better adjustment in individuals with adult-onset SCI (34,35). Aside from duration of injury, there were no other associations of coping style and level of injury, age at injury, or completeness of injury. This suggests that characteristics of the injury are not strong determinants of coping strategies selected.
Limitations
This study is limited to former patients from a single hospital system who could be located and were willing to participate; therefore, using the findings to make generalizations about the coping strategies of other populations is not possible. In addition, this was a cross-sectional study identifying coping strategies that were self-identified as used at a particular time. A longitudinal study would be helpful to look at the stability of coping strategies. Finally, although the Brief COPE is a quick and easy tool to assess coping strategies, it shows some limitations because the investigators do not know how individuals were interpreting the question as they responded. For example, humor has a broad range and may be used as friendly wit or sarcasm, which are very different coping approaches. More open-ended or qualitative studies might be helpful.
CONCLUSIONS
Adults with pediatric-onset SCI tend to use positive coping styles, and acceptance is a style used by almost all of them. Although the outcomes of community participation and independent living were not directly predicted by any specific coping style, the outcome of greater life satisfaction was predicted by the strategies of seeking emotional support, acceptance, religion, and lack of substance use.
REFERENCES
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen R. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Coping as a mediator of emotion. J Pers Soc Psychol. 1988;54:466–475. [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. The relationship between coping and emotion: implications for theory and research. Soc Sci Med. 1988;26:309–317. doi: 10.1016/0277-9536(88)90395-4. [DOI] [PubMed] [Google Scholar]
- Frank RG, Umlauf RL, Wonderlich SA, Askanazi GS, Buckelew SP, Elliot TR. Differences in coping styles among persons with spinal cord injury: a cluster-analytic approach. J Consult Clin Psychol. 1987;55:727–731. doi: 10.1037//0022-006x.55.5.727. [DOI] [PubMed] [Google Scholar]
- Buckelew SP, Baumstark KE, Frank RG, Hewett JE. Adjustment following spinal cord injury. Rehabil Psychol. 1990;35:101–109. [Google Scholar]
- Kennedy P, Lowe R, Grey N, Short E. Traumatic spinal cord injury and psychological impact: a cross-sectional analysis of coping strategies. Br J Clin Psychol. 1995;34:627–639. doi: 10.1111/j.2044-8260.1995.tb01496.x. [DOI] [PubMed] [Google Scholar]
- Kennedy P, Marsh N, Lowe R, Grey N, Short E, Rogers B. A longitudinal analysis of psychological impact and coping strategies following spinal cord injury. Br J Health Psychol. 2000;5:157–172. [Google Scholar]
- Kennedy P, Duff J, Evans M, Beedie A. Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol. 2003;42:41–52. doi: 10.1348/014466503762842002. [DOI] [PubMed] [Google Scholar]
- Elfstrohm ML, Ryden A, Kreuter M, Persson L-O, Sullivan M. Linkages between coping and psychological outcome in the spinal cord lesioned: development of SCI-related measures. Spinal Cord. 2002;40:23–29. doi: 10.1038/sj.sc.3101238. [DOI] [PubMed] [Google Scholar]
- Compas BE, Malcarne VL, Fondacaro KM. Coping with stressful events in older children and young adolescents. J Consult Clin Psychol. 1988;56:405–411. doi: 10.1037//0022-006x.56.3.405. [DOI] [PubMed] [Google Scholar]
- Compas BE. Coping with stress during childhood and adolescence. Psychol Bull. 1987;101:393–403. [PubMed] [Google Scholar]
- Anderson CJ, Vogel LC. Employment outcomes of adults who sustained spinal cord injuries as children or adolescents. Arch Phys Med Rehabil. 2002;83:791–801. doi: 10.1053/apmr.2002.32742. [DOI] [PubMed] [Google Scholar]
- Vogel LC, Krajci KA, Anderson CJ. Adults with pediatric-onset spinal cord injuries: part 3: impact of medical complications. J Spinal Cord Med. 2002;25:297–305. doi: 10.1080/10790268.2002.11753632. [DOI] [PubMed] [Google Scholar]
- Vogel LC, Anderson CJ. Outcomes of adults with pediatric-onset spinal cord injury. Top Spinal Cord Inj Rehabil. 2005;10((4)):109–115. [Google Scholar]
- Anderson CJ, Vogel LC, Willis KM, Betz RR. Stability of transition to adulthood among individuals with pediatric-onset spinal cord injuries. J Spinal Cord Med. 2006;29:46–56. doi: 10.1080/10790268.2006.11753856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury. Chicago, IL: American Spinal Injury Association; 2002. [Google Scholar]
- Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74:531–536. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the functional independence measure. Arch Phys Med Rehabil. 1994;75:127–132. [PubMed] [Google Scholar]
- Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level functional independence measure (FIM) Scand J Rehabil Med. 1994;26:115–119. [PubMed] [Google Scholar]
- Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil. 1992;73:519–526. [PubMed] [Google Scholar]
- Hall KM, Dijkers M, Whiteneck G, Brooks CA, Krause JS. The Craig handicap assessment and reporting technique (CHART): metric properties and scoring. J Rehabil Outcomes Meas. 1998;2:39–49. [Google Scholar]
- Whiteneck GG, Brooks CA, Charlifue S, et al. Craig Handicap Assessment and Reporting Technique. Englewood, CO: Craig Hospital; 1992. [Google Scholar]
- Pavot W, Diener R, Larson R, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams J. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Fuhrer MJ. Subjective well-being: implications for medical rehabilitation outcomes and models of disablement. Am J Phys Med Rehabil. 1994;73:358–364. doi: 10.1097/00002060-199409000-00010. [DOI] [PubMed] [Google Scholar]
- deLateur BJ. Quality of life: a patient-centered outcome. Arch Phys Med Rehabil. 1997;78:237–239. doi: 10.1016/s0003-9993(97)90026-5. [DOI] [PubMed] [Google Scholar]
- Galvin JR, Godfrey HPD. The impact of coping on emotional adjustment to spinal cord injury (SCI): review of the literature and application of a stress appraisal and coping formulation. Spinal Cord. 2001;39:615–627. doi: 10.1038/sj.sc.3101221. [DOI] [PubMed] [Google Scholar]
- Anderson CJ, Vogel LC, Chlan KM, Betz RR, McDonald CM. Depression in adults who sustained spinal cord injuries as children or adolescents. J Spinal Cord Med. 2007;30:S76–S82. doi: 10.1080/10790268.2007.11754609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamres LK, Janicki D, Helgeson VS. Sex differences in coping behavior: a meta-analytic review and an examination of relative coping. Pers Soc Psychol Rev. 2002;6:2–30. [Google Scholar]
- Woodrich F, Patterson JB. Variables related to the acceptance of disability in persons with spinal cord injuries. J Rehabil. 1983;49((3)):26–30. [PubMed] [Google Scholar]
- Dijkers MP. Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80:867–876. doi: 10.1016/s0003-9993(99)90076-x. [DOI] [PubMed] [Google Scholar]
- Krause JS, Broderick L. A 25-year longitudinal study of the natural course of aging after spinal cord injury. Spinal Cord. 2005;43:349–356. doi: 10.1038/sj.sc.3101726. [DOI] [PubMed] [Google Scholar]