Abstract
Background:
Extradural lesions are most commonly metastatic neoplasms. Extradural meningioma accounts for 2.7 to 10% of spinal neoplasms and most commonly is found in the thoracic spine.
Design:
Case report.
Findings:
A 45-year-old woman presented with posterior cervicothoracic pain for 8 months following a motor vehicle crash. Magnetic resonance imaging of the cervical spine revealed an enhancing epidural mass. Computerized tomography of the chest, abdomen, and pelvis revealed no systemic disease. Due to the lesion's unusual signal characteristics and location, an open surgical biopsy was completed, which revealed a psammomatous meningioma. Surgical decompression of the spinal cord and nerve roots was then performed. The resection was subtotal due to the extension of the tumor around the vertebral artery.
Conclusion:
Meningiomas should be considered in the differential diagnosis of contrast-enhancing lesions in the cervical spine.
Keywords: Meningioma; psammomatous; Epidural tumor; Vertebrae, cervical
INTRODUCTION
Tumors of the spinal column and spinal cord are classified as either extradural or intradural. Intradural tumors are further divided into intramedullary or extramedullary. The commonest intradural extramedullary tumors are schwannomas, neurofibromas, and meningiomas. Extradural lesions are most commonly metastatic neoplasms (1). The literature reports the occurrence of extradural meningioma as 2.7 to 10% of spinal neoplasms (2–12), occurring most commonly in the thoracic spine (3,4,8,10,13).
Case Report
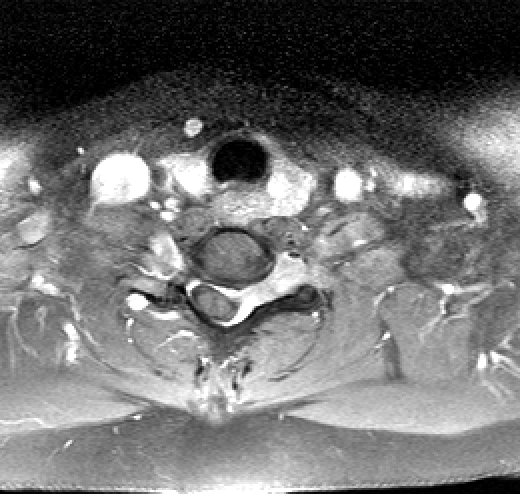
A 45-year-old woman noted chronic posterior cervicothoracic pain for 8 months following a low-speed motor vehicle crash. She also reported mild bladder disturbance for 7 months. Magnetic resonance imaging (MRI) revealed an epidural mass at C5-C7 (Figures 1 and 2) on the left side of the spinal canal and neural foramina, with significant spinal cord compression. MRI of neuraxes revealed no other lesions. Computerized tomography of the cervical spine revealed left neuroforaminal widening at C6-C7.
Figure 1. Sagittal T2 magnetic resonance image showing an enhancing epidural mass from C5 to C7.
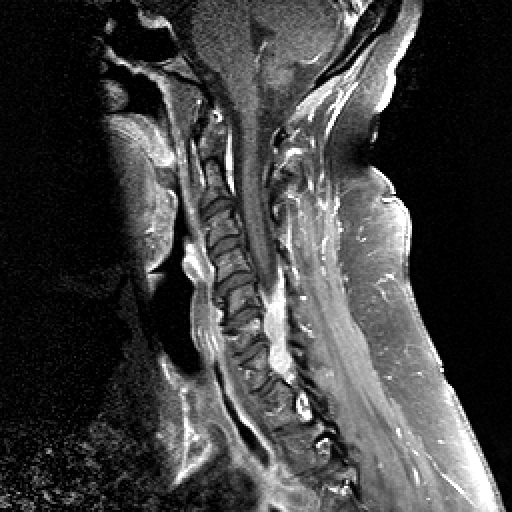
Figure 2. Axial T2 magnetic resonance image showing an enhancing epidural mass with spinal cord displacement and compression.
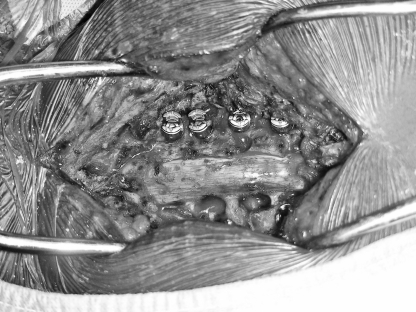
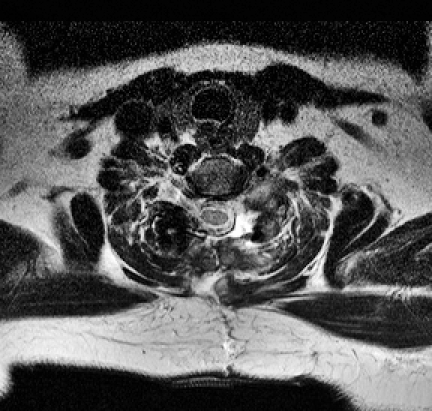
On physical examination, the patient had full muscle strength except for mild weakness of the hand intrinsic muscles and the triceps on the left side; she had no noted sensory deficits, pathologic reflexes, or long tract signs. In this case, metastatic evaluation revealed no additional lesions. An open biopsy was performed through a left C6-C7 foraminotomy and partial laminectomy. Pathological examination revealed a psammomatous meningioma that was resected 2 weeks later. A C5-C7 laminectomy and left-sided foraminotomies with C5-T1 instrumentation were performed (Figure 3). Due to proximity to the vertebral artery, only subtotal resection was attempted (Figures 4 and 5). Immediately after surgery, the patient manifested increased weakness of the left triceps (4/5), which progressively returned to baseline.
Figure 3. Intraoperative photograph of the C5-C7 laminectomy and C5-T1 instrumentation.
Figure 4. Postoperative sagittal T2 magnetic resonance image showing subtotal resection of epidural mass.

Figure 5. Postoperative axial T2 magnetic resonance image showing subtotal resection of epidural mass.
The patient was followed by using serial MRI every 3 months. At the most recent follow-up (6-months post-op), she had no evidence of recurrence and did not report any symptoms.
FINDINGS AND DISCUSSION
Individuals who present with extradural lesions need to have a metastatic process excluded, including hematopoietic disease (ie, lymphoma). In this type of patient, with a negative metastatic evaluation and from a younger age group, a wider differential diagnosis must be considered. Additional possibilities include schwannoma, neurofibromas, chordoma, synovial cyst, infectious processes, and meningioma (14).
Although considered in the differential, a nerve sheath lesion (neurofibroma/schwannoma) was ruled out because the signal characteristic illustrated that the mass was extradural and not contiguous with the neural element (14). Chordoma MRI radiographic features are isointense to the marrow on a T1 medical resonance image, but in this case the lesion was isointense to the spinal cord and did not appear to arise from the bony element (14). Synovial cysts are contiguous with the joint, spherical, and generally not larger than 1 to 2 cm (14).
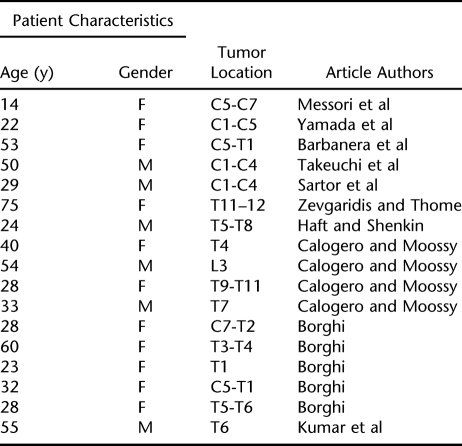
Literature review identified 17 case reports of extradural meningioma. Patients ranged in age from 14 to 75 years (mean, 38 years), with 47% of affected patients younger than age 30 years. The majority of affected individuals were female (64.7%), with an even higher proportion among patients younger than age 30 years (75%). This gender and age preference may arise from the ongoing hormonal changes promoting the development and growth of meningioma (4).
The majority of cases were thoracic, representing 52.9% of cases reviewed. Cervical extradural meningiomas made up 41.2% of cases. Additionally, of the 17 cases reviewed, 70.6% were exclusively extradural. The remainder was intra-extradural meningiomas (Table 1).
Table 1.
Published Cases of Extradural and Intra-extradural Meningiomas
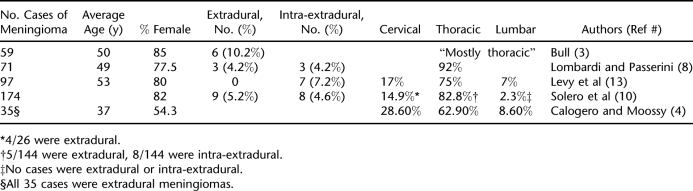
An analysis of the intradural spinal meningiomas reported in the literature (Table 2) revealed a mean age of 47 years, nearly 10 years older than that of the extradural variant. These cases also had a female preponderance (75.7%), which was slightly higher than that of the extradural meningiomas. Extradural meningiomas tended to be located in the thoracic region (52.9%), but to a lesser degree than the intradural meningiomas (78.2%). These differences may be the result of sample size.
Table 2.
Analysis of Important Cases of Meningioma in the Literature
This patient's presentation was typical for a patient with extradural meningioma, based on the literature reviewed. The presenting history of trauma associated with meningiomas has been previously reported (15,16). Schiffer et al (16) present the case of one patient with a cranial fracture, which they correlated with an intracranial meningioma diagnosed 15 years later; another patient had a left temporal craniectomy 37 years prior to diagnosis; a third patient had fallen several feet and fractured the left parietal bone 8 years prior to the meningioma diagnosis. In a review of the literature, Kasantikul and colleagues (15) presented a case of spinal meningioma secondary to trauma, which resulted in paraplegia (3 years prior to the diagnosis of subdural meningioma). Although the authors suggested a cause and an effect, this relationship has been disputed and pathogenesis is unclear (15,16).
In the current patient, the preceding motor vehicle crash likely did not cause her meningioma, but it may have been involved in precipitation of the symptoms. In patients presenting with meningiomas after trauma, the diagnosis was typically made at least 3 years posttrauma. As for other cases studied, diagnosis was made 6 months to several years after the initial complaint. Cohen-Gadol and colleagues (5) studied 21-years worth of cases of spinal meningiomas in patients younger than age 50. Symptom duration averaged 12.4 months. Additionally, Sartor and colleagues (17) discussed the case of a patient who had a history of 2 motor vehicle crashes, at 4 and 2 years prior to diagnosis, respectively. The patient had neck and back pain following the first accident, but diagnosis of meningioma was made by using angiography 4 years later.
Authors have suggested worse prognoses for patients with extradural meningiomas because of the difficulty in completely removing the tumor. They suggest that location of the tumor and invasion of the dura make it more difficult in these cases to achieve complete resection, allowing for recurrence (3,6,13). If complete resection is possible, there may be no difference in patients' prognoses (10). In the 17 case reports reviewed, 11 patients had total resections, 1 patient died for unclear reasons (18), 1 patient had a recurrence 13 years after the initial complete tumor removal (4), and 1 patient improved but did not completely recover from the initial neurological deficit (7). One case report did not present follow-up data (12), and the rest of the cited series reported that patients were asymptomatic at their most recent follow-up exam (2,4,9,11,19). In cases of subtotal resection, 1 author did not provide follow up information (17), 2 patients died (4,20), 2 patients had paresis (2), and 1 patient developed paraplegia (2).
CONCLUSION
Extradural meningiomas are rare but should be included in the differential diagnosis of extradural masses. Prognosis relates to the extent of resection. If considered safe, complete resection should be attempted to decrease risk of recurrence.
REFERENCES
- McPhee SJ, Papadakis MA, Tierney LM Jr, Gonzales R, Zeiger R, editors. Current Medical Diagnosis & Treatment 2007. 46th ed. New York: The McGraw-Hill Companies; 2007. [Google Scholar]
- Borghi G. Extradural spinal meningiomas. Acta Neurochir (Wien). 1973;29:195–202. [Google Scholar]
- Bull JWD. Spinal meningiomas and neurofibromas. Acta Radiol. 1953;40:283–300. doi: 10.3109/00016925309176591. [DOI] [PubMed] [Google Scholar]
- Calogero JA, Moossy J. Extradural spinal meningiomas: report of four cases. J Neurosurg. 1972;37:442–447. doi: 10.3171/jns.1972.37.4.0442. [DOI] [PubMed] [Google Scholar]
- Cohen-Gadol AA, Zikel OM, Koch CA, Scheithauer BW, Krauss WE. Spinal meningiomas in patients younger than 50 years of age: a 21-year experience. J Neurosurg Spine. 2003;98:258–263. doi: 10.3171/spi.2003.98.3.0258. [DOI] [PubMed] [Google Scholar]
- Early CB, Sayers MP. Spinal epidural meningioma: case report. J Neurosurg. 1966;25:571–573. doi: 10.3171/jns.1966.25.5.0571. [DOI] [PubMed] [Google Scholar]
- Haft H, Shenkin HA. Spinal epidural meningioma. J Neurosurg. 1963;20:801–804. doi: 10.3171/jns.1963.20.9.0801. [DOI] [PubMed] [Google Scholar]
- Lombardi G, Passerini A. Spinal cord tumors. Radiology. 1961;76:381–392. doi: 10.1148/76.3.381. [DOI] [PubMed] [Google Scholar]
- Messori A, Rychlicki F, Salvolini U. Spinal epidural en-plaque meningioma with an unusual pattern of calcification in a 14-year-old girl: case report and review of literature. Neuroradiology. 2002;44:256–260. doi: 10.1007/s00234-001-0709-3. [DOI] [PubMed] [Google Scholar]
- Solero CL, Fornari M, Giombini S, et al. Spinal meningiomas: review of 174 operated cases. Neurosurgery. 1989;25:153–160. [PubMed] [Google Scholar]
- Yamada S, Kawai S, Yonezawa T, Masui K, Nishi N, Fujiwara K. Cervical extradural en-plaque meningioma. Neurol Med Chir. 2007;47:38–39. doi: 10.2176/nmc.47.36. [DOI] [PubMed] [Google Scholar]
- Zevgaridis D, Thome C. Purely epidural spinal meningioma mimicking metastasis tumor: case report and review of literature. Spine. 2002;27:403–405. doi: 10.1097/00007632-200209150-00021. [DOI] [PubMed] [Google Scholar]
- Levy W, Bay J, Dohn D. Spinal cord meningioma. J Neurosurg. 1982;57:804–812. doi: 10.3171/jns.1982.57.6.0804. [DOI] [PubMed] [Google Scholar]
- Ross J, Brant-Zawadzki M, Chen M, Moore K, Salzman K. Diagnostic Imaging: Spine. 1st ed. Salt Lake City, UT: Amirsys; 2004. Meningioma; pp. IV1–78-IV1-81. [Google Scholar]
- Kasantikul V, Charuchaikul S, Shuangshoti S. Extramedullary subdural meningioma after trauma. Neurosurgery. 1991;29:930–931. doi: 10.1097/00006123-199112000-00025. [DOI] [PubMed] [Google Scholar]
- Schiffer J, Avidan D, Rapp A. Posttraumatic meningioma. Neurosurgery. 1985;17:84–87. doi: 10.1227/00006123-198507000-00015. [DOI] [PubMed] [Google Scholar]
- Sartor K, Fliedner E, Pfingst E. Angiographic demonstration of cervical extradural meningioma. Neuroradiology. 1977;14:147–149. doi: 10.1007/BF00333059. [DOI] [PubMed] [Google Scholar]
- Kumar S, Kaza RC, Maitra TK, Chandra M. Extradural spinal meningioma arising from a nerve root. J Neurosurg. 1980;52:728–729. doi: 10.3171/jns.1980.52.5.0728. [DOI] [PubMed] [Google Scholar]
- Takeuchi H, Kubota T, Sato K, Hirose S. Cervical extradural meningioma with rapidly progressive myelopathy. J Clin Neurosci. 2006;13:397–400. doi: 10.1016/j.jocn.2005.05.018. [DOI] [PubMed] [Google Scholar]
- Barbanera A, Nina P, Serchi E, Ascanio F. Aggressive recurrence of intra-extradural cervico-thoracic meningothelial meningioma. Acta Neurochir (Wien). 2007;149:83–86. doi: 10.1007/s00701-006-1056-2. [DOI] [PubMed] [Google Scholar]