Abstract
It has been reported that in Western society as many as 16% of individuals experience cervicogenic headache, which can lead to significant amounts of pain and perceived disability. Cervicogenic headache is characterized by unilateral occipital-temporal pain that is increased by neck movement; it is accompanied by cervical hypomobility, postural changes, and/or increased cervical muscle tone. This case report describes the physical therapy differential diagnosis, management, and outcomes of a patient with cervicogenic headache. The patient was a 40-year-old woman referred by her physiatrist with complaints of cervical pain and ipsilateral temporal headache. The patient presented with increased muscle tone, multiple-level joint hypomobility in the cervical and thoracic spine, muscle weakness, and postural changes. Self-report outcome measures included the Visual Analog Scale for headache pain intensity and the Neck Disability Index. Management consisted of various thrust and non-thrust manipulations, soft tissue mobilizations, postural re-education, and exercise to address postural deficits and cervical and thoracic hypomobility and diminished strength. At discharge, the patient demonstrated clinically meaningful improvements with regard to pain, disability, and headache. This case report indicates that a multimodal physical therapy treatment program may be effective in the management of a patient diagnosed with cervicogenic headache.
Key Words: Cervicogenic Headache, Manipulation, Thrust, Exercise, Physical Therapy
Cervicogenic headaches are commonly encountered in physical therapy (PT) practice. Cervicogenic headache is a headache type validated recently by the International Headache Society (IHS) that is hypothesized to originate due to nociception in the cervical area. In a Scandinavian population study, its prevalence was established at approximately 16%1. Table 1 outlines the diagnostic criteria for cervical headaches as described by the IHS2.
TABLE 1.
Diagnostic criteria for cervical headaches as described by the International Headache Society2.
|
Horn and Smith3 reviewed the literature on approaches to management of cervicogenic headache using orthopedic manual physical therapy (OMPT) principles. They recommended careful examination to identify all impairments, to provide a differential diagnosis, and to plan appropriate intervention. Recommended interventions included joint mobilization, soft tissue mobilization, retraining of specific postural muscle groups, and patient education. The authors recommended that emphasis should be placed on home and self-management skills and on increasing patient understanding of the predisposing factors with regard to cervicogenic headache. Jull4 also described the importance of an accurate differential diagnosis ascertaining the cervical musculoskeletal origin of the headache to assure success with management of a cervical headache patient. She described the history and symptomatic features of cervical headache following the description of the IHS2, and she noted the role of physical impairments in the articular, muscular, and nervous system. She suggested that the diagnosis of cervical headache was dependent on the presence of both articular and muscle impairments, accompanied by acute or chronic poor neuromotor control.
The presence of painful upper cervical joint dysfunction accompanied by impairments in the deep cervical flexors, scapular postural muscles, and cervical kinaesthesia can indicate that a headache is cervical in origin4. Other physical impairments that are often present in a cervical headache patient include postural abnormalities, muscle tightness, and neural tissue mechanosensitivity. However, Jull4 also noted that the absence of the above impairments does not necessarily preclude a cervical headache diagnosis. Jull4 emphasized the importance of specific retraining of upper cervical flexor muscles, the lower trapezius, and serratus anterior, combined with postural retraining and ergonomic and lifestyle advice.
Various authors have identified current approaches in the management of cervical headaches using OMPT principles3,5–11. Intervention may include joint mobilization/manipulation, soft tissue mobilization and stretching techniques, retraining specific postural muscle groups, and patient education. This literature suggests that emphasis should be placed on addressing joint mobility, posture, muscle strength, and imbalances in the upper back and neck with attention also directed toward life style, habits, and stress management.
The literature discussed above provides preliminary evidence to demonstrate the utility of a thorough clinical examination as well as the effectiveness of OMPT intervention as a component of a multimodal approach to managing patients with cervicogenic headaches. The purpose of this case report is to describe the PT differential diagnosis and management of a patient with cervical headaches.
Case Description
The patient was referred by her physiatrist to an orthopaedic outpatient PT clinic with a diagnosis of cervical spondylosis, myofascial pain, and headaches. An ABPTS (American Board of Physical Therapy Special ties)-certified orthopedic PT clinical specialist, who was also certified in manual therapy and had 15 years of clinical experience, performed the standardized examination described below. The examination followed the spinal evaluation format as described by Paris and Loubert12 (Table 2).
TABLE 2.
Spinal examination format as described by Paris and Loubert12.
|
Pain Assessment
Headache pain intensity was assessed using a visual analog scale (VAS). The VAS is a self-report instrument that consists of a 100-mm straight horizontal or vertical line that is anchored by two extremes of pain: “no pain” and “pain as bad as it could be”13. Test-retest reliability of the VAS was established as good to excellent (κ=0.71–0.99). Correlation with the McGill Pain Questionnaire was fair (r=0.30) and correlation with the Numeric Pain Rating Scale was excellent (r=0.95)14. Data on interpretation indicate that a score >30 (mm) is equal to or greater than “moderate” pain and a score >54 (mm) is equal to or greater than “severe” pain. The minimal detectable change on the VAS is 28 (mm)15. The VAS was used to describe the patient's current pain and the worst pain over the last 24 hours. The rating by this patient on the VAS scale was 20 (mm) in the early mornings, increasing to 80 (mm) later in the day. Current pain rating was 34 (mm) and average rating was 41 (mm). The frequency of the headaches was two to three times per week; the duration of the headaches fluctuated from one day to three days.
The patient reported that her headaches limited her in performing several functional activities: lifting and carrying more than 5 Ibs, grocery shopping, maintaining a prolonged flexed posture, spending sufficient time with the children in her class, and performing repetitive reaching (especially overhead activities), and housekeeping. In addition to verbal report, the Neck Disability Index (NDI)16 was used to identify the patient's disability level in a more standardized manner. The NDI consists often sections with questions ranging from pain intensity and headache frequency to interference with personal care, work, and recreation. Every question has six answers to choose from, grading the activity from easy to perform without any pain to not being able to perform the activity at all. The NDI is easy to use in the clinical setting to monitor change in functional status. The instrument has good test-retest reliability (ICC=0.89–0.94) and internal consistency (Crohnbach's α=0.80-0.87)16. Responsiveness estimates indicate that a change score of >7 points represents the minimal clinically significant difference for this outcome measure and it is thereby indicative of a clinically meaningful change; a change score of <3 points rules out a change14. Construct validity is good, as expressed by correlation with the Patient-Specific Functional Scale and Short Form-36 functional outcomes measures (r=0.54–0.81)16. This patient's score was 20 out of a possible 50, which is indicative of a moderate disability (this category ranges from 15–24)16.
Initial Observation
The patient presented at the initial visit in no apparent distress. She demonstrated no guarding of the upper extremities. Right rotation movement guarding involving the neck was noticed as the patient positioned herself in a chair so as to avoid having to look right towards the physical therapist, who was seated to her right.
History and Interview
PRESENT HISTORY
The patient was a 40-year-old Caucasian female who was employed as a kindergarten teacher. Her symptoms of neck pain and headache had started three years before with no known cause. The patient's present complaints were right-sided occipital and temporal headaches. Over time the frequency, duration, and intensity of the headaches had increased, leading to an increased frequency of missing work. Pain-increasing factors included stress and working at the low tables in a stooped posture for more than 30 minutes. Pain-relieving factors were resting, supporting the head in a supine or reclined position, and taking over-the-counter anti-inflammatory medications. The pain intensity of the headache generally would increase as the day progressed. The headache and neck pain was occasionally present at night when at its worst. Change in position of the neck decreased the intensity of the pain.
PREVIOUS HISTORY
The patient's medical system screening was negative. Specific areas of interest related to headache symptoms were included in the history. The patient was asked if she had any vision, hearing, smell, or taste problems to screen for diseases of the eye, ear, nose, or throat. The patient was also asked if she experienced any vomiting associated with nausea, sleepiness, dimmed vision, or a stiff neck with severe increasing headache to screen for traction or inflammatory headaches caused by mass lesions, such as tumors, edema, or hematoma, migraine headaches, cluster headaches, and hypertensive headaches. Additional screening was performed for vertebral artery deficiency symptoms, including a negative patient report of position-dependent dizziness and blurred vision. The patient denied any history of cervical trauma. Up to five years before, she had worked as a roofer and had performed heavy lifting activities. The patient indicated she was in general good health. The patient was a physically active individual who enjoyed going to the gym, which she had not done as much as she would have liked to in the last three months due to the severity of her headaches. She was married and had a teenage daughter. No data were found with regard to the diagnostic accuracy of the history items used to exclude non-musculoskeletal pathology, other headache types, and vertebral artery deficiency.
MEDICATION HISTORY
The patient was not taking any prescription medication. She used over-the-counter anti-inflammatory medication when her symptoms were at their worst.
BEHAVIORAL ASPECTS
The patient's primary concern was her loss of function resulting from the increasing symptoms she was experiencing. Her decreased ability to continue her active lifestyle and the impact on her family life were primary motivators for seeking PT treatment.
Structural Inspection
Visual postural observation revealed a slight degree of forward head posture with protracted shoulders (right more noticeable than left), decreased curvatures of the thoracic and cervical spine, and right scapular winging. The patient was unable to maintain a corrected posture for >30 (s) at the time of the initial evaluation due to reported muscle fatigue. Intrarater reliability of visual assessment of spinal curvature has been reported as moderate (κ= 0.50) and interrater reliability as poor (κ= 0.16)17.
Active Movements
Active range of motion assessment of the subcranial, cervical, and thoracic spine was performed using visual estimation with a 4-point rating scale consisting of the rating points no, minimal, moderate, and considerable restriction. It included forward (FB) and backward bending (BB), rotation (ROT), and sidebending (SB) in the frontal plane. These tests revealed considerable restriction in subcranial FB and right ROT, and moderate restriction in left SB. For this case report, the subcranial region was defined as including the C0–C2 spinal segments. Mid-cervical frontal plane right SB and ROT were moderately restricted; frontal plane left SB was minimally restricted. Moderate restriction was noted in right SB and ROT in the upper thoracic region. Youdas et al18 reported on interrater reliability of visual estimation of active range of motion in degrees. They reported ICC=0.42 for cervical flexion and extension, 0.63 for SB, and 0.70–0.82 for ROT (one side at a time).
Palpation for Condition, Position, Mobility
Palpation for condition revealed increased muscle tone and tenderness of the suboccipital, bilateral upper and lower trapezius, levator scapulae, and rhomboid muscles, most pronounced on the right side. Palpation of the right-sided C1-C2 and C2-C3 facet joints produced a pain response. The interrater reliability of pain provocation with palpation has been reported as low (κ=0.14–0.31)19 to moderate-good (κ=0.42-0.79)14,20. Aprill et al21 found a 60% positive predictive value for occipital headaches originating in the C1–C2 joint with a combination of findings including pain in the (sub)occipital region, tenderness on palpation of the lateral C1–C2 joint, and restricted C1–C2 rotation. The interrater reliability of palpation for muscle tone has been reported as low to moderate (κ=0.16-0.39)22.
Palpation for position revealed the spinous processes of T6 and T8 in left rotated positions. Interrater reliability of palpation for vertebral position has been reported as poor (κ=−0.04–0.03)23, indicating that these particular test findings should be interpreted with caution.
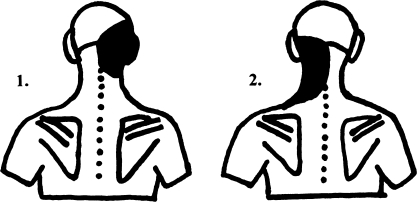
Palpation for mobility by way of passive intervertebral motion (PIVM) testing was performed after the vertebral artery test (discussed below) was found to be negative, using a 7-point rating scale (Table 3). Mid-cervical PIVM was performed using the segmental sidebending technique (downslide, Fig. 1) and the direct facet palpation (upslide, Fig. 2)24. Subcranial PIVM included the use of the FB and BB nodding technique, ROT of occiput around long axis of the neck, ROT of the occiput on axis with neck fixed in SB position, and SB slide of the atlas assessment technique24. Upper thoracic spine PIVM included the use of intervertebral palpation for mobility while passively moving the cervical spine in FB, BB, ROT, and SB24. First rib depression mobility was also assessed by way of an inferior-medial glide of this rib. Mid-thoracic PIVM included the performance of spring tests via the transverse processes for postero-anterior (PA) glide25. Considerable joint hypomobility was found in C0-C1 FB, Cl-2 right ROT, C7-T1 right ROT and SB, and right first rib depression. Slight joint hypomobility was found in C0-C1 left SB and C2-3 right ROT and SB. Slight joint hypermobility was found in C5-C6 right SB and ROT. Thoracic PA testing revealed slight hypomobility at T6-T8.
TABLE 3.
Rating scale as described by Paris and Loubert12.
| Grade | Description | Criteria |
|---|---|---|
| 0 | Ankylosed | No detectable movement |
| 1 | Considerable hypomobility | Significant decrease in expected range and significant resistance to movement |
| 2 | Slight hypomobility | Slight decrease in mobility and resistance to movement |
| 3 | Normal | Expected movement |
| 4 | Slight hypermobility | Slight increase in expected mobility and less than normal resistance to movement |
| 5 | Considerable hypermobility | Significant increase in expected mobility, eventually restricted by periarticular structures |
| 6 | Unstable | Significant increase in expected mobility without restraint of periarticular structures |
Fig. 1.
Segmental side-bending technique (downslide) as described by Paris24. With the patient supine and the head supported on a pillow in physiological neutral, the operator contacted the articular pillar with the MP II joint of the hand. Downslide of the right facet joint was assessed when the right side was pressed producing a sidebending to the right.
Fig. 2.
Direct facet palpation (upslide) as described by Paris24. With the patient supine, head supported on a pillow, the operator supported the left side of the head with the left hand and placed the thenars of the right hand on the right side. The head was moved in a physiological side bending left and rotation left, and the facet upslide was palpated with the index finger of the right hand.
Smedmark et al26 reported poor to moderate interrater reliability for PIVM in rotation of the cervical spine and for assessment of first rib mobility (κ=0.28–0.43). Pool et al27 reported similar findings for interrater reliability of PIVM in cervical sidebending (κ=0.08–0.63). These authors also reported poor to substantial interrater reliability of pain provocation with PIVM testing (κ=0.22–0.80). These values are similar to the ranges reported by Huijbregts28 in a review of reliability studies of spinal motion palpation. This review also reported that the intrarater reliability of PIVM of the cervical spine in the literature ranged from poor to excellent (κ=0.01–0.81) and that in the thoracic spine it was moderate (κ=0.43–0.55). Thoracic interrater reliability was reported as poor to fair (κ= −0.03–0.35). Jull et al29 studied the diagnostic accuracy of manual diagnosis by a trained manipulative therapist in determining symptomatic facet joints in a series of 20 patients with cervical pain. The therapist performed a subjective examination followed by PA glides and PIVM testing in flexion, extension, SB, and ROT, noting end-feel, resistance to motion, and pain reproduction in order to identify the presence and level of symptomatic facet joints. The gold standard test was pain relief on image-guided diagnostic nerve blocks. With sensitivity and specificity both at 100%, manual diagnosis was as accurate as diagnostic nerve blocks in the diagnosis of cervical facet joint. Zito et al30 reported that pain on manual examination of the upper cervical joints (C0-C3) could discriminate cervicogenic headache subjects from other subjects (controls and migraine-with-aura subjects) with an 80% sensitivity, compared to a gold standard of headache classification based on the diagnostic criteria described by the IHS. Jull et al31 reported intrarater reliability of manual examination as excellent (κ=0.78–1.0).
Neurovascular Findings
Neurovascular assessment was unremarkable with normal upper-limb tension tests (ULTT) with median, ulnar, and radial nerve bias, deep tendon reflexes, and sharp and dull sensation tests of the upper extremities. Wainner et al32 compared clinical tests for the diagnosis of cervical radiculopathy to the gold standard test of electrodiagnostic studies. They reported specificity of 0.93–0.95 and sensitivity of 0.03–0.24 for upper extremity DTK testing; specificity of 0.22 and sensitivity of 0.97 for the median nerve bias ULTT; specificity of 0.33 and sensitivity of 0.72 for the radial nerve bias ULTT; and specificity of 0.66-0.86 and sensitivity of 0.12-0.29 for dermatomal sensation testing of the upper extremity for the diagnosis of cervical radiculopathy.
Vertebral artery testing (VAT) was performed using the DeKleyn-Nieuwenhuyse (sustained extension-rotation) test and prolonged cervical extension24, both with negative results. The validity of VAT for the diagnosis of clinically significant perfusion abnormalities involving the posterior circulation is debated in the literature. Rivett et al33 found that end-range positions of extension and rotation resulted in significant reductions in blood flow velocity of the vertebral artery (as assessed by Doppler ultrasonography) in a sample of 20 symptomatic and asymptomatic patients. However, Licht et al34 did not find changes in flow velocity when studying 11 subjects undergoing vertebral artery testing. Zaina et al35 also did not find changes in volume flow rate of the vertebral arteries in 20 subjects in various degrees of cervical rotation.
Upper-Quarter Assessment
Upper-quarter strength assessment revealed muscle weakness of 3+/5 for the lower trapezius and serratus anterior muscles. Strength testing was performed using the 0-5 rating scale as described by Kendall et al36. Intra- and interrater reliability of manual muscle testing have been reported by multiple authors37–40, with reported correlation coefficients for intrarater reliability ranging from 0.71-0.99 and interrater reliability ranging from 0.72-0.96, indicating good to excellent reliability. The patient populations included in these studies were patients with muscular dystrophy, upper extremity neuropathies, and a general orthopedic population. Muscles tested in these studies included both upper-extremity and lower-extremity muscles.
Neck flexor muscle endurance was tested as described by Harris et al41. For this test, the patient, positioned in supine hook lying, was asked to lift her head with the chin maximally retracted one inch above the plinth. The patient was timed until the chin position was no longer maintained or the head was no longer maintaining the one-inch distance to the plinth. The intrarater reliability for this test was good to excellent (ICC=0.82–0.91) for subjects without neck pain, and the interrater reliability was moderate to good (ICC=0.67–0.78) for subjects with and without neck pain. In this reliability study, Harris et al found that the results for a group without neck pain (mean=38.95 (sec), SD=26.4) were significantly different from the results for a group with neck pain (mean=24.1 (sec), SD=12.8). The patient in this case study was able to maintain the position for 18 (sec). This score was well below the mean scores for both the symptomatic and asymptomatic group mean scores reported by Harris et al. Based on the assumption of a normal distribution, standardized scores were calculated to interpret the patient's standing relative to symptomatic group (z= −0.46) and the asymptomatic group (z= −0.80); this patient's score was in the 32nd percentile of the symptomatic group and in the 21st percentile of the asymptomatic group substantiating a score well below the established mean for both groups and indicating to the authors of this case report the need for specific intervention.
Muscle length testing as described by Kendall et al36 revealed muscle shortening in the right pectoralis minor and major, left pectoralis minor, right levator scapulae, and the bilateral upper trapezius muscles (right side more than left). Barr et al37 reported good interrater reliability (ICC=0.76) and moderate to excellent intrarater reliability (ICC=0.33–0.97) for manual muscle length testing using a rating scale of normal or tight. Zito et al30 reported a K score range of 0.4–1.0 for muscle extensibility testing, classifying muscles either as normal or tight.
Imaging and Other Medical Data
Plain film radiography using a lateral view of the cervical spine showed a loss of cervical lordosis and decreased disc space evident at C5-C6. Loss of cervical lordosis has been attributed to muscle spasm in response to underlying pathology42. McAviney et al43 found that subjects with a lordosis of 20° or less on cervical radiographs were significantly more likely to have cervical symptoms. They also found a statistically significant relationship between the presence of cervical pain and a radiographic lordosis of 0° or less. In this study, the odds that a patient with cervical pain had a lordosis of 0° or less was 18 times greater than for a patient without cervical pain. However, Helliwell et al44 compared the incidence of loss of radiographic cervical lordosis in patients with and without cervical pain and did not find a such a relationship. Decreased height of disc spaces on the lateral view may be a radiographic indication of degenerative disc disease42. Kettler et al45 found excellent agreement (κ=0.90) between the radiological observation of decreased disc height and macroscopically observed degenerative changes of the cervical intervertebral disc. Osteophyte formation was noted both anteriorly and posteriorly around the osseous margin of the endplates of the vertebral bodies of C5 and C6 in our patient.
Summary of Findings
The patient presented with signs and symptoms characteristic of cervical headache as defined by the IHS2 (Table 2). This patient presented with the following pathophysiologic impairments relevant to subsequent treatment planning:
Unilateral headaches and suboccipital pain, aggravated by head movements and prolonged flexed posture
C0-C1 FB and left SB restriction
C1-C2 right ROT restriction
C2-C3 right ROT and right SB restriction
C5-C6 right ROT and right SB hypermobility
C7-T1 right ROT and right SB restriction
Right first rib depression restriction
Hypomobility on T6-T8 PA testing
Increased muscle tone in the suboccipital, bilateral upper and lower trapezius, levator scapulae, and rhomboid muscles, most pronounced on the right side
Shortening of bilateral pectoralis minor and right pectoralis major, right levator scapulae, and the upper trapezius muscles
Decreased strength and endurance of trapezius, serratus anterior, and deep cervical flexor musculature
Forward head posture, protracted shoulders, and slight right scapular winging
In our clinical opinion, the medical diagnosis of cervicogenic headache was supported by the findings of the history and examination outlined above. Specifically, the headache pattern, the presence of cervical joint dysfunction, the presence of muscle tenderness and decreased extensibility, the abnormal posture and pathology reported in the radiological examination supported this diagnosis. The patient met all three criteria established by Aprill et al21 and noted above for the diagnosis of cervicogenic headache, and the pain reported on manual examination of C0-C3 also satisfied the criteria established by Zito et al30 discussed above.
We recognize that limitations exist related to the psychometric data for the tests and measures used in the evaluation of this patient, especially with regard to low levels of reliability and/or validity reported in the literature and discussed above. The absence of psychometric data, such as minimal detectable change, for a number of the tests and measures limits their use as diagnostic tests and specifically as outcome measures. Thus, caution should be exercised when making diagnostic decisions or inferences regarding treatment outcomes based on these tests and measures. More specifically, of the tests done in the neurovascular examination, only the negative ULTT test would seem to have sufficient sensitivity to confidently exclude a diagnosis of cervical radiculopathy for this patient. Questionable construct validity and the complete absence of data on predictive validity with regard to adverse effects after thrust or non thrust manipulation for the VAT render interpretation of its results questionable at best.
Palpation findings clearly played a major role in the diagnosis of this particular patient. The reliability data for PIVM testing, palpation for condition, and palpation for tenderness of cervical facet joints suggest that the reliability is poor to moderate when these tests are performed in isolation. However, most relevant to this case report are studies by Jull et al29, Zito et al30, and Aprill et al21. These studies suggest that when the manual examination incorporates information from the subjective evaluation and information regarding joint mobility in multiple directions noting end-feel, resistance to motion, and pain reproduction, the psychometric properties of this compound manual examination in the cervical spine (interrater reliability, sensitivity, and specificity) are such that confidence can be placed in use of manual examination in the identification of symptomatic cervical facet joints and in the discrimination of subjects with cervicogenic headaches from those with migraine headaches and control subjects. However, we again recognize that Zito et al30 and Aprill et all21 only established values for sensitivity (80%) and positive predictive value (60%), respectively, for their diagnostic criteria. Data on sensitivity are diagnostically useful only when tests are negative and then only when sensitivity values are high to rule out a condition and not to rule in a condition as was done here. Positive predictive values are only relevant if the prevalence in the study population is similar to the one encountered in the clinic.
Explanation and Prognosis
The results of a recent RCT46 that tested the effectiveness of therapeutic exercise and manipulation on subjects with cervicogenic headache indicated that 75% of subjects achieved at least a 50% reduction in headache frequency. This study did not reveal a consistent pattern of predictors of successful short- and long-term treatment outcomes (defined as an at least 50% reduction in headaches) from variables in the demographics and headache history of the subjects. Absence of lightheadedness was a relevant and consistent prognostic indicator of successful long-term treatment outcomes only. The patient's age, the chronicity of the headache, and the presence of headaches of at least moderate intensity did not reduce the odds of successful treatment outcomes. Coeytaux and Spierings47 indicated that a diagnosis of migraine might predict a less favorable prognosis than other types of headaches in patients receiving treatment in a specialized headache clinic. The authors did not further specify the exact type of treatment given to each patient. In this study, gender, age, age at headache onset, and the presence of a daily headache did not predict poor prognosis. Based on these studies, the patient in this case report would seem to have a good prognosis of achieving at least a 50% decrease in headache symptoms.
The functional goals for the identified impairments were as follows:
The patient reports a clinically significant improvement, for her, in her ability to perform house work-activities.
The patient reports a clinically significant improvement, for her, in her ability to perform lifting activities and grocery shopping.
The patient reports a clinically significant improvement, for her, in her ability to perform work-related activities, such as working at the children's low desks in a prolonged flexed posture.
The patient reports a clinically significant improvement, for her, in her ability to perform recreational activities including reading and driving for several hours, and returning to a fitness program.
Interventions
The interventions used in the treatment of this patient are summarized in table 4. Techniques used to improve mobility of the subcranial region included: C0-C1 Atlas Lateral Press (Fig. 3) and Unilateral Nod (Fig. 4), C1-C2 Rotation in Sitting (Fig. 5), and C2-C3 Facet Downward Slide (Fig. 6), all as described by Paris24. The Atlas Lateral Press technique was used to restore SB, and the Unilateral Nod technique was used to restore FB at C0-C1. The C2-C3 Facet Downward Slide technique was used to restore mobility of the C2-3 facet joint in the biomechanically coupled directions of right ROT and right SB.
TABLE 4.
Interventions.
| Interventions | Measures | |
|---|---|---|
| Week 1 | Myofascial manipulation of suboccipital and upper thoracic muscles35 and suboccipital distraction. Grade III mobilization of subcranial region in flexion, side-bending, and rotation. Upslide/downslide facet mobilization of C2-C3 and C7-T1. | No headaches reported, pain 40mm on VAS scale. Muscle tone, TOP of facet joints decreased. |
| Week 2 | Added contract-relax stretching of trapezius, pectoralis minor, and levator scapulae. Grade III progressive oscillations to T6-T9 and 1st rib manipulation. | Reoccurrence of cervicogenic headaches T6-T8 mobility normalized. Subcranial PIVM improved to moderate, with decreased TOP. |
| Week 3 | As above. | Headache frequency, duration, and intensity decreased. Pain VAS score 21mm. Subcranial mobility normalized, with exception of C1-C2 RR. 1st rib mobility improved. |
| Week 4 | Strength and endurance training of deep cervical flexors, lower trapezius, and serratus anterior. Grade III-IV mobilization of C1-C2 RR, 1st rib. Postural re-education. Myofascial mobilization and muscle stretching continued. | Increased intensity of headache to 68mm on VAS. C1-C2 RR mobility regressed to significant, with increased TOP. |
| Week 5 | HVLA thrust manipulation C1-C2 RR. Muscle strengthening, stretching, and postural re-education continued. Instruction in body mechanics and workstation adaptations. | No headaches or cervical pain reported. Neck flexor endurance improved to 25 sec, strength of trapezius and serratus anterior 4/5. PIVM of cervical and thoracic facet joints normalized. Muscle length normalized. |
| Weeks 6-9 | Strength and endurance training of deep cervical flexors, lower trapezius, and serratus anterior continued. Postural re-education. Progression to home program. | No headaches or cervical pain reported. Neck flexor endurance normalized to 35 sec, strength of trapezius and serratus anterior normalized to 5/5. Able to maintain corrected posture > 5 min. NDI score 3/50. |
| VAS–Visual Analog Scale; TOP–Tenderness on palpation; PIVM–Passive Intervertebral motion; RR–Right rotation; NDI–Neck Disability Index | ||
Fig. 3.
C0-C1 Atlas Lateral Press technique as described by Paris24. The operator contacted the transverse process C1 with the metacarpophalangeal joint of the index finger, while the other arm stabilized the head and chin in opposite sidebending. The force was directed medially through the MP joint contact to impart a side-gliding action on the atlas, restoring C0-1 sidebending to the opposite side.
Fig. 4.
Unilateral Nod technique as described by Paris24. The posterior arch of C1 on the side of the restriction was contacted with the middle finger of the opposite hand, and the ipsilateral hand passively imparted a unilateral nod through the patient's forehead.
Fig. 5.
C2-C3 Facet Downward Slide technique as described by Paris24. With the patient situated in supine, the operator contacted the lower aspect of the facet joint with the 2nd metacarpophalageal joint of the ipsilateral hand. The other hand was placed on the contralateral side of the head and imparted sidebending towards the involved side down to the restricted level. A progressive oscillatory force was imparted through the MP II joint in an inferior, medial, and posterior direction.
Fig. 6.
C1-C2 Rotation in Sitting technique as described by Paris24. In order to improve right rotation, the operator stood on the right side, with the right forearm and hand contacting the head of the patient. The left thumb was placed against the lamina of C2. The patient's head was rotated towards the right around a vertical axis using gentle progressive oscillations, while the left thumb blocked movement at C2.
At Week 5, a distinct and isolated joint restriction of C1-C2 rotation remained, and it was decided to use a high-velocity, low-amplitude (HVLA) thrust manipulation to treat this restriction and thereby affect the remaining headache complaints. Before performing the C1-C2 HVLA gapping manipulation technique as described by Hartman48 (Fig. 7), the alar odontoid integrity test24,48, the Sharp-Purser test48, and the VAT12,48 were performed to identify potential contraindications to this technique. The VAT has traditionally been recommended as a pre-manipulation test to screen for vertebral artery pathology that could lead to higher incidence of adverse effects following HVLA thrust manipulation. However, as noted above, the clinical usefulness of this test has recently been questioned and its construct and predictive validity has been debated in the literature33–35. Thiel and Rix49 asserted that careful history taking and physical examination could identify those patients at risk for vertebral artery pathology, and that provocative testing was very unlikely to provide additional useful information. Upper cervical ligamentous stability testing is routinely performed to evaluate the ligamentous integrity of the subcranial region50. The Sharp-Purser test is used to evaluate anterior C1-C2 stability48. Uitvlugt and Indenbaum51 reported a predictive value of this test of 85%, a specificity of 96%, and a sensitivity of 85% albeit in a population of patients diagnosed with rheumatoid arthritis. Cattrysse et al50 reported the intrarater reliability of this test in a population of patients with Down's syndrome as fair to substantial (κ=0.29–0.67); interrater reliability was poor to substantial (κ=0.09–0.67). No psychometric data could be identified in the literature for the alar odontoid integrity test. We acknowledge that the psychometric data available for the ligamentous stability tests for the upper cervical spine is insufficient for confident diagnostic decision making in this particular patient.
Fig. 7.
C1-C2 high-velocity, low-amplitude gapping manipulation technique as described by Hartman48.
We also recognize the diagnostic uncertainty with which a clinician is faced in the absence of substantive data on diagnostic and predictive accuracy for the tests and measures in history and physical examination purported to establish a contraindication to the use of HVLA in the upper cervical spine. However, it should be noted that Di Fabio52 described the risk of cervical HVLA thrust manipulation in the cervical spine as similar to low-velocity manipulation and mobilization. Also, with no findings in the history and physical examination and after obtaining informed consent from the patient, the use of this upper cervical HVLA technique seemed appropriate to both the treating clinician and the patient. An additional rationale for using this technique was that the use of the grade III–IV joint manipulations described earlier had been effective for restoring most joint restrictions with exception of C1–C2 right ROT, which was a likely remaining source for the continued headaches. In addition, localized right C1–C2 muscle guarding was present, which had increased in intensity in comparison with the prior visits. The grade III and IV joint manipulations were painful and caused increased muscle guarding, but the HVLA thrust manipulation technique was not painful and resulted in immediate localized muscle relaxation and restoration of normal joint mobility. After performing the HVLA joint manipulation, the patient's headache was immediately relieved.
Deep neck flexor endurance training was performed in the previously described test position41, with the patient lifting the head one inch from the surface with the chin maximally retracted. The contraction time was progressively increased based on patient tolerance.
Outcomes
The patient was seen for a total of 16 visits over a 9-week period of time. The initial frequency of treatment was 3 times per week and was gradually decreased to once weekly during Weeks 6–9 to monitor progression of the home program. At time of discharge, the patient had reported no headaches for three weeks. Her NDI score had decreased to 3/50 from an initial level of 20/50, which indicated that a clinically meaningful change had occurred based on the minimal clinically important difference of 7 points16. The VAS pain scale score ranged from 0–5 (mm) with some daily variation, compared to a maximal initial level of 80 (mm), which represented a true change based on a minimal detectable change of 28 (mm)16. The location of the remaining pain was in the upper thoracic region.
Active cervical range of motion assessed by visual estimation had normalized. Segmental PIVM tests of the subcranial, mid-cervical, and thoracic joints that were initially identified as hypomobile now revealed normal range and end-feel, and did not reproduce pain. Moderate hypermobility of the C5-C6 vertebral segment on PIVM testing remained unchanged but as this passive test is not a test of functional stability, this test result was expected. Muscle length of upper trapezius, pectoralis minor, and levator scapulae muscles was normal upon re-evaluation. Neck flexor endurance41 had improved to 35 seconds compared to an initial score of 18 seconds, placing this patient's score in the 44th percentile of the reported normative asymptomatic group (compared to 21st percentile initially), and in the 80th percentile of the symptomatic group (compared to 32nd percentile initially); both scores seem to indicate normalization of this impairment identified on the initial evaluation. Strength of the lower trapezius and serratus anterior muscles had increased to 5/5. Postural awareness and control had improved, with the patient able to reproduce and maintain corrected posture for extended periods of time, i.e., >5 (min) as compared to being unable to hold corrected posture for 30 (sec) on the initial evaluation. The patient was contacted 6 months and 1 year after discharge, and at both instances she reported that her status was essentially unchanged from the time of discharge indicating positive long-term effects in addition to the positive effects noted upon discharge from PT treatment as described above.
Discussion
This case report describes the PT differential diagnosis, management, and outcomes of a patient with cervicogenic headache. The patient was a 40-year-old woman referred by her physiatrist with complaints of cervical pain and ipsilateral temporal headache. The patient presented with increased muscle tone, multiple-level cervical and thoracic joint hypomobility, muscle weakness, and postural changes. We used the VAS and NDI as self-report standardized and validated outcome measures. Management consisted of various thrust and non-thrust manipulations, soft tissue mobilizations, postural re-education, and exercise to address the identified impairments noted above. At discharge, the patient demonstrated clinically meaningful improvements with regard to pain, disability, and headache intensity and frequency. The patient's improvement on the NDI and VAS outcomes measures exceeded the minimal clinically important difference and minimal detectable change reported for these measures, respectively, and thus represented a clinically meaningful and true change, respectively, in patient status. This case report indicates that a multimodal PT treatment program including OMPT using thrust and non-thrust joint manipulation and soft tissue techniques, exercise, and education may be effective in the management of a patient diagnosed with cervicogenic headache.
It has been suggested that there is a direct relationship between cervical joint dysfunction and headaches. Bogduk and Marsland53 used diagnostic cervical medial branch and zygapophyseal joint blocks to identify the C1-C2 and C2-C3 joints as a source of head and neck pain in 24 patients with neck pain and headache. Aprill et al54 assessed the pain referral patterns of cervical facet joints by analyzing pain distribution charts from 10 patients and confirming the suspected segmental location of the symptomatic joint by using diagnostic joint blocks; their study showed that pain from C2-C3 was distinguished from C3-C4 by referral pattern of the former into the head (Fig. 8). The relationship between cervical muscle hypertonicity and headache generation was studied by Hack et al55. Anatomical research had shown that a connective tissue band existed between the rectus capitis posterior minor muscle and the posterior atlanto-occipital membrane. This membrane was attached to the underlying spinal dura. Contraction of the rectus capitis posterior minor muscle was hypothesized to cause tension on the dura mater and thereby produce a headache. Bogduk56 described a direct anatomical relationship of the dura mater of the upper cervical cord, posterior cranial fossa, and the ventral rami of the upper three cervical nerves. Painful joint dysfunction of the upper three segments was therefore a possible pain source in cervical headaches. Zito et al30 investigated the presence of cervical musculoskeletal impairments in subjects with cervicogenic headaches, migraines with aura, and control subjects and found that the cervicogenic headache group had significantly less range of motion in cervical flexion/extension, a significantly higher incidence of painful upper cervical joint dysfunction, and a significantly higher incidence of muscle tightness. These authors also reported that manual examination of the upper cervical facet joints could discriminate between the cervicogenic headache group and the other groups combined with a sensitivity of 80%.
Fig. 8.
Zygapophyseal joint pain referral pattern from 1) C2-3; 2) C3-C4 (Redrawn from Aprill et al54).
When presented with any patient, the physical therapist first needs to decide if this patient indeed belongs in physical therapy. One aspect of this screening process is to determine whether the signs and symptoms identified during history and physical examination indeed match the medical diagnosis provided. Findings that would indicate a discrepancy between actual patient presentation and medical diagnosis would indicate the need to at least contact the referring physician. In the case of a patient with headache, it is important that the physical therapist is aware of other headache types that may closely resemble cervicogenic headache but that either present an indication for medical management, pose a contraindication to PT intervention, or at the very least are not amenable to (sole) PT management. The pattern identified in the review of the literature above of cervical joint dysfunction, postural changes, muscular dysfunction, and cervical headaches was present in the case presented in this paper. Following the physical examination and analysis of data, we concluded that the patient had headache symptoms and cervical joint and muscular dysfunction that might be related to each other.
Headaches can be classified in three major types: vascular, traction (inflammatory), and headache of musculoskeletal origin24. Vascular headaches include migraines, cluster headaches, toxic vascular, and hypertensive headaches. The patient's headache symptoms were not vascular in origin because they did not follow the typical migraine or cluster headache description, and the patient did not show any signs of toxic vascular or hypertensive disease in her medical history. Traction or inflammatory headaches are caused by mass lesions, such as tumors, edema, haematoma, diseases of the eye, ear, nose, and throat, or by occlusive vascular disease. The patient's medical history and physical examination did not reveal any warning signs associated with this type of headache, such as vomiting associated with nausea, sleepiness, dimmed vision, or a stiff neck with severe rapidly increasing headache.
Headaches of musculoskeletal origins are the tension type headache and the cervicogenic or cervical headache as described by IHS2. The patient presented with signs and symptoms characteristic of cervical headache. The major findings that led to this diagnosis were (a) unilateral headaches and suboccipital pain, aggravated by certain head movements and prolonged flexed posture; (b) cervical joint dysfunction; (c) muscle hypertonicity, tenderness, and decreased extensibility; and (d) abnormal posture and pathology reported in the radiological examination. Other relevant clinical findings in this case were hypermobility of one cervical level (C5-C6), upper and mid-thoracic joint restrictions, and the presence of decreased strength and endurance in specific postural musculature. Tension-type headache criteria include headache lasting from 30 minutes to 7 days, two of the criteria of pressing/tightening quality, mild to moderate intensity (not inhibiting activity), bilateral location, not aggravated by walking or stair climbing, no vomiting, nausea, or presence of photophobia. Since this patient presented with unilateral, high-intensity headaches that were of long duration, were aggravated by activity, and affected the patient's function, it was felt that the criteria for tension-type headache were not met.
Physical therapy management within the evidence based practice paradigm is decided by best available evidence. In many cases—including the case report discussed here—best evidence means a combination of pathophysiologic hypotheses and research evidence. A limited number of studies have investigated the outcomes of various interventions for the treatment of cervicogenic headaches. We performed a review of the literature using computerized literature searches of the following databases: CINAHL, FirstSearch (incl. MedLine), OVID, ProQuest, and ScienceDirect. We used MeSH terms and other keywords including cervicogenic headaches, physical therapy, manual therapy, manipulation, mobilization, and exercise. The results of this literature review supported the diagnosis and management of this patient. The effectiveness of treatment of this case is comparable with the outcomes described in the literature. A recent clinical trial by Jull et al6 involving 200 patients with cervicogenic headaches, compared the effect of various combinations of specific strengthening and endurance exercises of the deep neck flexors and other postural muscles, and manual therapy treatment of the cervical joints. That study used four treatment groups: manipulative therapy group, exercise group, combined manipulative therapy and exercise group, and a control group. Outcomes measures included the frequency of headaches, headache intensity and duration, the Northwick Park Neck Pain Index, medication intake, and patient satisfaction. Patients who received active exercise, manual therapy, or a combination of active exercise and manual therapy displayed significantly better outcomes (frequency of headaches, pain intensity, neck pain) than the control group. This effect was maintained at the 12-month follow-up. There was no statistically significant difference in outcomes among the different treatment groups; however, 10% more patients experienced relief with the combination of manipulative therapy and exercise than with any of these interventions alone. Nilsson57 conducted an RCT of 53 subjects with cervicogenic headache, comparing the outcomes of HVLA manipulation of the cervical spine to a control group who received low-level laser treatment and deep friction massage. The intensity, duration, and frequency of headaches were significantly reduced in the HVLA manipulation group immediately following the 3-week treatment protocol; however, long-term follow-up was not performed. Gross et al58 performed a Cochrane systematic review of 33 randomized clinical trials evaluating the effectiveness of manipulation and mobilization compared to other forms of conservative therapy for the treatment of mechanical neck disorders. These authors concluded that strong evidence exists for the effectiveness of multimodal care (manipulation and/or mobilization in combination with exercise) in the treatment of mechanical neck disorders with or without headache; however, they did not find evidence for the effectiveness of manipulation and/or mobilization done as the only intervention. Molina8 performed a review of clinical trials, descriptive studies, and case reports regarding the treatment efficacy of manipulation related to upper cervical spine dysfunction and cervical headaches. Efficacy studies were described measuring the effect of manipulation on symptoms, cervical mobility, and proprioception-dependent performance. The outcome of these studies showed a moderate to good effectiveness of treatment measured during or immediately post-treatment and moderate long-term (3 to 6 months post-treatment) effectiveness; however, the author noted that the descriptions of the study designs and specificity of the description of interventions used were insufficient in a number of the studies reviewed, and the number of quality studies was limited. A recent study59 evaluating the methodological quality of RCTs of spinal manipulation and mobilization in the treatment of headaches reached a similar conclusion that the number of studies in this area is limited, and that the methodological quality of these papers is typically low. The authors identified the clear need for additional high-quality RCTs in this area.
A forward head posture and weakness of the upper cervical flexors has been commonly observed in headache patients60,61. Watson and Trott5 investigated the relationship between forward head posture and weakness of the upper cervical flexor musculature in cervical headache patients. In this study, 60 female subjects, aged 25–40, were divided in two groups (headache and non-headache group). The protocol to examine the subjects consisted of lateral photographs of natural head posture, isometric strength and endurance testing of upper cervical flexor muscle group, passive intervertebral movement testing, and the completion of a questionnaire (by the headache group). The headache group was found to be significantly different from the non-headache group with respect to increased forward head posture, less isometric strength, and less endurance of the upper cervical flexor musculature. It was concluded that cervical headache patients exhibited forward head posture and demonstrated weakness and lack of endurance of the upper cervical flexor musculature. The authors found a significant relationship of endurance and forward head posture in cases of cervical headaches as analyzed by the Chi-square test (χ2 = 13.7, p <0.01), in that lower endurance values corresponded with a more pronounced forward head posture. They concluded that management of patients with cervical headaches should emphasize postural correction and re-education in addition to specific endurance training of upper cervical flexor musculature.
Primary impairments (abnormalities of structure or function62) can result in the development of secondary impairments. For this patient, we considered it likely that significant restrictions of the cervico-thoracic junction and mid-thoracic region, in combination with postural deficits (primary impairment), resulted in the subcranial dysfunction (secondary impairment). Restrictions in both subcranial and thoracic spine could then have caused increased stress to the C5-C6 segment, resulting in its hypermobility. Prolonged positioning of the head in forward head position and of the shoulders in a rounded position could have resulted in the observed adaptive shortening of the pectoralis minor and major, the upper trapezius muscles, and the right levator scapulae muscle, and decreased strength of the scapular stabilizing muscles. The muscle weakness and the resulting inability to maintain a corrected posture for any length of time might also have been one of the underlying causes of the patient's postural deficits.
This case report describes a multimodal treatment approach to management of cervical headaches patients by physical therapists. This multimodal treatment approach was based on a combination of the evidence provided in the literature and pathophysiologic hypotheses. Manipulation techniques, including HVLA thrust, appear to be effective interventions for the management of cervical joint dysfunction when integrated in a comprehensive treatment approach. Several studies described the importance of postural correction and the specific endurance training of the deep cervical flexors3–6,8. It is essential that underlying impairments of decreased mobility, strength, endurance, and postural control be addressed in addition to managing subjective symptoms. A comprehensive treatment approach emphasizing the restoration of normal joint mobility, strengthening of specific postural muscle groups, postural retraining, and patient education in self-management skills may provide long-term treatment success. Of course, the format of a case report does not allow us to infer a cause-and effect relationship between intervention and reported outcomes and indicates the need for further outcome studies in this area. This case report also clearly identified the need of further research in the area of psychometric properties of a number of tests and measures used in the evaluation of patients with cervicogenic headaches, including upper cervical ligament stability testing, evaluation of muscle tone, postural analysis, and methods used for manual diagnosis.
Conclusion
This case report illustrates the PT differential diagnosis, management, and outcomes of a patient diagnosed with cervicogenic headaches. This patient presented with headache symptoms matching the classification of cervicogenic headache as defined by the IHS2, dysfunctions in the subcranial, the mid-cervical, and thoracic joints, decreased strength and endurance in postural musculature, and postural deficits. A multimodal PT treatment approach was used based on evidence in the literature and pathophysiologic hypotheses, and it included the use of non-thrust and thrust manipulation techniques, therapeutic exercise, and postural correction. Clinically meaningful short- and long-term improvements with regard to pain, disability, and headache were reported with at least a temporal relation to this treatment approach. Physical therapy management of the cervical headache patient should address all identified impairments with interventions including non-thrust joint manipulation, HVLA thrust manipulation, soft tissue manipulation and stretching techniques, retraining specific postural muscle groups, and patient education. A need for further research exists in the areas of psychometric properties of a number of the tests and measures commonly used during the diagnostic process for these patients and in the area of outcomes of PT treatment of patients with cervicogenic headaches.
REFERENCES
- 1.Nilsson N. The prevalence of cervicogenic headache in a random population sample of 20–59 year olds. Spine. 1995;20:1884–1888. doi: 10.1097/00007632-199509000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders. 2nd edition. Cephalalgia 2004;24:suppl 1. [DOI] [PubMed]
- 3.Horn C, Smith KL. Cervicogenic headache Part II: Clinical examination, findings and approaches to management. J Manual Manipulative Ther. 1997;5:171–175. [Google Scholar]
- 4.Jull G. Management of cervical headache. Man Ther. 1997;2:182–190. doi: 10.1054/math.1997.0298. [DOI] [PubMed] [Google Scholar]
- 5.Watson DH, Trott PH. Cervical headache: An investigation of natural head posture and upper cervical flexor performance. Cephalalgia. 1993;13:272–284. doi: 10.1046/j.1468-2982.1993.1304272.x. [DOI] [PubMed] [Google Scholar]
- 6.Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27:1835–1843. doi: 10.1097/00007632-200209010-00004. [DOI] [PubMed] [Google Scholar]
- 7.Vernon H. Spinal manipulation in the management of tension-type migraine and cervicogenic headaches: The state of evidence. Topics Clin Practice. 2002;9:14–20. [Google Scholar]
- 8.Molina P. Management of upper cervical spine disorders and cervicogenic headache. Orthop Phys Ther Clinics N Am. 1999;8(1):45–67. [Google Scholar]
- 9.Vernon H, Steiman I, Hagino C. Cervicogenic dysfunction in muscle contraction headache and migraine: A descriptive study. J Manipulative Physiol Ther. 1992;15:418–429. [PubMed] [Google Scholar]
- 10.Jensen O, Nielsen F, Vosmar L. An open study comparing manual therapy with the use of cold packs in the treatment of post-traumatic headache. Cephalalgia. 1990;10:241–250. doi: 10.1046/j.1468-2982.1990.1005241.x. [DOI] [PubMed] [Google Scholar]
- 11.Schoensee SK, Jensen G, Nicholson G, Gossman M, Katholi C. The effect of mobilization on cervical headaches. J Orthop Sports Phys Ther. 1995;21:184–196. doi: 10.2519/jospt.1995.21.4.184. [DOI] [PubMed] [Google Scholar]
- 12.Paris SV, Loubert PV. Foundation of Clinical Orthopedics. 3rd ed. St. Augustine, FL: Institute Press; 1999. pp. 308–312. [Google Scholar]
- 13.Huskinsson EC. Visual analogue scales. In: Melzack R, editor. Pain Measurement and Assessment. New York, NY: Raven Press; 1983. pp. 33–37. [Google Scholar]
- 14.Finch E, Brooks D, Stratford PW, Mayo NE. Physical Rehabilitation Outcomes Measures. 2nd ed. Hamilton, ON: BC Decker; 2000. pp. 173–174. [Google Scholar]
- 15.Bertilson B, Grunnosjo M, Strender L. Reliability of clinical tests in the assessment of patients with neck/shoulder problems: Impact of history. Spine. 2003;28:2222–2231. doi: 10.1097/01.BRS.0000089685.55629.2E. [DOI] [PubMed] [Google Scholar]
- 16.Vernon H, Mior S. The neck disability index: A study of reliability and validity. J Manipulative Physiol Ther. 1991;14:411. [PubMed] [Google Scholar]
- 17.Fedorak C, Ashworth N, Marshall J, Paull H. Reliability of the visual assessment of cervical and lumbar lordosis: How good are we? Spine. 2000;28:1857–1859. doi: 10.1097/01.BRS.0000083281.48923.BD. [DOI] [PubMed] [Google Scholar]
- 18.Youdas J, Cary J, Garrett T. Reliability of measurement of cervical spine ROM: Comparison of three models. Phys Ther. 1991;71:98–106. doi: 10.1093/ptj/71.2.98. [DOI] [PubMed] [Google Scholar]
- 19.Van Suijlekom H, deVet H, van den Berg S, Weber W. Interobserver reliability in physical examination of the cervical spine in patients with headache. Headache. 2000;40:581–586. doi: 10.1046/j.1526-4610.2000.00090.x. [DOI] [PubMed] [Google Scholar]
- 20.Viikari-Juntura E. Interexaminer reliability of observations in physical examinations of the neck. Phys Ther. 1987;67:1526–1532. doi: 10.1093/ptj/67.10.1526. [DOI] [PubMed] [Google Scholar]
- 21.Aprill C, Axinn MJ, Bogduk N. Occipital headaches stemming from the lateral atlanto-axial (C1-2) joint. Cephalalgia. 2002;22:15–22. doi: 10.1046/j.1468-2982.2002.00293.x. [DOI] [PubMed] [Google Scholar]
- 22.Schoeps P, Pfingsten M, Siebert U. Reliabilität manualmedizinischer Untersuchungstechniken an der Halswirbelsäule. Studie zur Qualitätssicherung in der manuellen Diagnostik. Z Orthop Ihre Grenzgeb. 2000;138:2–7. doi: 10.1055/s-2000-10105. [DOI] [PubMed] [Google Scholar]
- 23.Keating J, Bergmann T, Jacobs G, Finer B, Larson K. Interexaminer reliability of eight evaluative dimensions of lumbar segmental abnormality. J Manipulative Physiol Ther. 1990;13:463–470. [PubMed] [Google Scholar]
- 24.Paris SV. Course notes S3. Atlanta, GA: Institute Press; 1988. [Google Scholar]
- 25.Paris SV, Nyberg R, Irwin M. Course notes S2. St. Augustine, FL: Institute of Physical Therapy; 1993. [Google Scholar]
- 26.Smedmark V, Wallin M, Arvidsson I. Inter-examiner reliability in assessing passive intervertebral motion of the cervical spine. Man Ther. 2000;5:97–101. doi: 10.1054/math.2000.0234. [DOI] [PubMed] [Google Scholar]
- 27.Pool J, Hoving J, de Vet H, van Memeren H, Bouter L. The interexaminer reproducibility of physical examination of the cervical spine. J Manipulative Physiol Ther. 2003;27:84–90. doi: 10.1016/j.jmpt.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Huijbregts PA. Spinal motion palpation: A review of reliability studies. J Manual Manipulative Ther. 2002;10:24–39. [Google Scholar]
- 29.Jull G, Bogduk N, Marsland A. The accuracy of manual diagnosis for cervical zygapophysial joint pain syndromes. Med J Aust. 1988;148(5):233–236. doi: 10.5694/j.1326-5377.1988.tb99431.x. [DOI] [PubMed] [Google Scholar]
- 30.Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther. 2006;11:118–129. doi: 10.1016/j.math.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 31.Jull G, Zito G, Trott P, Potter H, Shirley D, Richardson C. Interexaminer reliability to detect painful upper cervical joint dysfunction. Aust J Physiother. 1997;43:125–129. doi: 10.1016/s0004-9514(14)60406-2. [DOI] [PubMed] [Google Scholar]
- 32.Wainner R, Fritz J, Irrgang J, Boninger M, Deltto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 33.Rivett DA, Sharples KJ, Milburn PD. Effect of premanipulative tests on vertebral artery and internal carotid artery blood flow: A pilot study. J Manipulative Physiol Ther. 1999;22:368–375. doi: 10.1016/s0161-4754(99)70081-3. [DOI] [PubMed] [Google Scholar]
- 34.Licht PB, Chistensen HW, Hoilund-Carlsen PF. Carotid artery blood flow during premanipulative testing. J Manipulative Physiol Ther. 2002;25:568–572. doi: 10.1067/mmt.2002.128367. [DOI] [PubMed] [Google Scholar]
- 35.Zaina C, Grant R, Johnson C, Dansie B, Taylor J, Spyropolous P. The effect of cervical rotation on blood flow in the contralateral vertebral artery. Man Ther. 2003;8:103–109. doi: 10.1016/s1356-689x(02)00155-8. [DOI] [PubMed] [Google Scholar]
- 36.Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. 4th ed. Baltimore, MD: Williams and Wilkins; 1995. [Google Scholar]
- 37.Barr AE, Diamond BE, Wade CK, Harashima T, Pecorella WA, Potts CC, Rosenthal H, Fleiss JL, McMahon DJ. Reliability of testing measures in Duchenne or Becker muscular dystrophy. Arch Phys Med Rehabil. 1991;72:315–319. [PubMed] [Google Scholar]
- 38.Brandsma JW, Schreuders TA, Birke JA, Piefer A, Oostendorp R. Manual muscle strength testing: Intraobserver and interobserver reliabilities for the intrinsic muscles of the hand. J Hand Ther. 1995;8:185–190. doi: 10.1016/s0894-1130(12)80014-7. [DOI] [PubMed] [Google Scholar]
- 39.Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH. Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther. 1987;67:1342–1347. doi: 10.1093/ptj/67.9.1342. [DOI] [PubMed] [Google Scholar]
- 40.Florence JM, Pandya S, King WM, Robison JD, Baty J, Miller JP, Schierbecker J, Signore LC. Intrarater reliability of manual muscle test (Medical Research Council scale) grades in Duchenne's muscular atrophy. Phys Ther. 1992;72:115–122. doi: 10.1093/ptj/72.2.115. [DOI] [PubMed] [Google Scholar]
- 41.Harris KD, Heer DM, Roy TC, Santos DM, Whitman JM, Wainner RS. Reliability of a measurement of neck flexor muscle endurance. Phys Ther. 2005;85:1349. [PubMed] [Google Scholar]
- 42.McKinnis LN. Fundamentals of Orthopedic Radiology. Philadelphia, PA: FA Davis Company; 1997. [Google Scholar]
- 43.McAviney J, Schulz D, Bock R, Harrison D, Holland B. Determining the relationship between cervical lordosis and neck complaints. J Manipulative Physiol Ther. 2005;28:187–193. doi: 10.1016/j.jmpt.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 44.Helliwell PS, Evans PF, Wright V. The straight cervical spine: Does it indicate muscle spasm? J Bone Joint Surg Br. 1994;76:103–106. [PubMed] [Google Scholar]
- 45.Kettler A, Rolmann F, Neidlinger-Wilke C, Werner K, Claes, Wilke HJ. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration. Part II: Cervical spine. Eur Spine J. 2006;15:732–741. doi: 10.1007/s00586-005-1037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jull GA, Stanton WR. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2004;25:101–108. doi: 10.1111/j.1468-2982.2004.00811.x. [DOI] [PubMed] [Google Scholar]
- 47.Coeytaux RR, Spierings ELH. Prognostic factors, disability, and functional status among patients in a headache specialty practice. Cephalalgia. 2005;26:7–13. doi: 10.1111/j.1468-2982.2005.00976.x. [DOI] [PubMed] [Google Scholar]
- 48.Hartman L. Handbook of Osteopathic Technique. 3rd ed. Cheltenham, UK: Stanley Thornes Ltd.; 1998. pp. 185–186. [Google Scholar]
- 49.Thiel H, Rix E. Is it time to stop functional pre-manipulation testing of the cervical spine? Man Ther. 2005;10:154–158. doi: 10.1016/j.math.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 50.Cattrysse E, Swinkels RAHM, Oostendorp RAB, Duquet W. Upper cervical instability: Are clinical tests reliable? Man Ther. 1997;2:91–97. doi: 10.1054/math.1997.0290. [DOI] [PubMed] [Google Scholar]
- 51.Uitvlugt G, Indenbaum S. Clinical assessment of atlantoaxial instability using the Sharp-Purser test. Arthritis Rheum. 1988;31:918–922. doi: 10.1002/art.1780310715. [DOI] [PubMed] [Google Scholar]
- 52.Di Fabio RP. Manipulation of the cervical spine: Risks and benefits. Phys Ther. 1999;79:50–65. [PubMed] [Google Scholar]
- 53.Bogduk N, Marsland A. The cervical zygapophysial joints as a source of neck pain. Spine. 1988;13:610–617. [PubMed] [Google Scholar]
- 54.Aprill C, Dwyer A, Bogduk N. Cervical zygapophyseal joint pain patterns II: A clinical evaluation. Spine. 1990;15(6):458–461. doi: 10.1097/00007632-199006000-00005. [DOI] [PubMed] [Google Scholar]
- 55.Hack G, Koritzer T, Robinson W, Hallgren R, Greenman P. Anatomic relation between the rectus capitus posterior minor muscle and the dura mater. Spine. 1995;20(23):2484–2486. doi: 10.1097/00007632-199512000-00003. [DOI] [PubMed] [Google Scholar]
- 56.Bogduk N. Cervical causes of headache and dizziness. In: Boyling J, Palastanga N, editors. Grieve's Modern Manual Therapy of the Vertebral Column. Edinburgh, UK: Churchill Livingstone; 1994. pp. 317–332. [Google Scholar]
- 57.Nilsson N, Christensen HW, Hartvigsen J. The effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther. 1997;20:326–330. [PubMed] [Google Scholar]
- 58.Gross AR, Hoving JL, Haines TA, et al. A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine. 2004;29(14):1541–1548. doi: 10.1097/01.brs.0000131218.35875.ed. [DOI] [PubMed] [Google Scholar]
- 59.Fernandez-de-las-Penas C, Alonso-Blanco C, San-Roman J, Miangolarra-Page JC. Methodological quality of randomized controlled trials of spinal manipulation and mobilization in tension-type headache, migraine, and cervicogenic headaches. J Orthop Sports Phys Ther. 2006;36(3):160–169. doi: 10.2519/jospt.2006.36.3.160. [DOI] [PubMed] [Google Scholar]
- 60.Janda V. Muscles and cervicogenic pain syndromes. In: Grant R, editor. Physical therapy of cervical and thoracic spine. Edinburgh, UK: Churchill Livingston; 1988. [Google Scholar]
- 61.Paris V. Cervical symptoms of forward head posture. Topics Geriatric Rehabil. 1990;5:11–19. [Google Scholar]
- 62.Guide to Physical Therapist Practice, 2nd Ed. Phys Ther. 2001;81:9–744. [PubMed] [Google Scholar]