Abstract
This case series describes the pragmatic use of a treatment-based classification system for the management of four patients with a chief complaint of low back pain. Patients were initially classified into stabilization, manipulation, or specific exercise subgroups based on history and clinical examination. Each patient was reassessed during the course of clinical care to determine whether to continue treating according to the initially assigned subgroup or to alter management and incorporate a mechanism-based classification addressing identified impairments. Patient #1 was initially classified in the manipulation category. Within three visits, he reported being “a great deal better” on the Global Rating of Change (GROC) and had a 6-point improvement in his Oswestry Disability Index (ODI). Patient #2, classified in the specific exercise/extension category, reported being “moderately better” using the GROC and had a 22-point improvement in her ODI within six visits. Patient #3, classified in the stabilization category, reported being “a very great deal better” on the GROC and had a 30-point improvement in his ODI Index within four visits. Patient #4 was categorized initially in the manipulation category and subsequently in the specific exercise category; after five visits, he noted being “quite a bit better” using the GROC and he reported a 58-point improvement on his ODI. All four patients in this study were managed using a dynamic pragmatic treatment-based classification approach that allowed for the change of subgroup classification and treatment of impairments and all achieved a clinically meaningful improvement in pain and disability
Key Words: Low Back Pain, Manipulation, Stabilization, Specific Exercise, Treatment-Based Classification, Mechanism-Based Classification
The prevalence of low back pain (LBP) in the US, as well as the disability and financial burden associated with it, continues to increase1. Treatment costs are consistently rising by at least 7% per year in the United States, and they have a total impact in excess of $170 billion annually. The direct costs of LBP are reportedly between $33 to $55 billion per year2. Additionally, individuals with LBP experience health expenditures that are 60% greater than those without LBP, 37% of which are a direct result of physical therapy (PT) and allied specialist services3.
Multiple diagnostic classification systems have been developed in an attempt to guide clinicians in the management of LBP4. Generally, these diagnostic systems can be classified into unidimensional systems, which include pathoanatomical, signs and symptoms, prognosis, and mechanism-based classification systems, and a single multidimensional classification system. The pathoanatomical classification system attempts to identify the nociceptive source of the patient's symptoms based on diagnostic imaging or diagnostic injections5. The signs and symptoms classification system utilizes a treatment-based approach, wherein a cluster of signs and symptoms from the patient history and physical examination are used to classify patients with LBP into subgroups with specific implications for management6, 7. The prognosis classification system is based on the potential future outcome of the patient8. The mechanism-based classification system is based on the premise that impairments identified during examination are the cause of musculoskeletal pain and dysfunction9. Finally, the multi-dimensional classification system classifies patients by a combination of the following: the stage of disorder, pathoanatomical diagnosis, signs and symptoms, and psychosocial factors8.
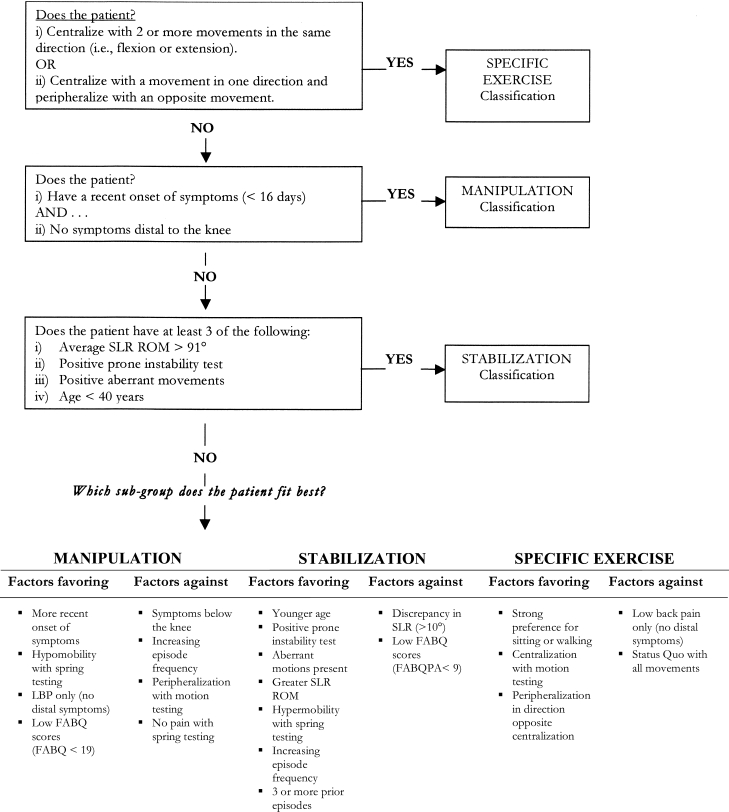
Delitto et al6 have proposed a treatment-based classification system to categorize patients with acute LBP; this system has subsequently been supported in the literature10, 11. Specific findings based on patient history, symptom behavior, and clinical signs serve to facilitate classification of the patient into a subgroup that then receives treatment from which they are most likely to benefit. Although Delitto et al6 originally based this system on the limited available evidence and expert opinion at the time, recent randomized trials10, 11 have supported the use of this classification-based treatment approach in the management of patients with LBP. Classification-based treatment has been shown to be more effective in improving patient outcomes than management strategies that are based on practice guidelines and treatment not matched to a specific subgroup10, 11. Fritz et al12 have refined the classification system proposed by Delitto et al6 and have constructed a decision-making algorithm that divides subjects into a manipulation, specific exercise, or stabilization subgroup (Figure 1).
Fig. 1.
Decision-making algorithm used by clinicians in this study to identify appropriate subgrouping of patients
SLR- straight leg raise; ROM- range of motion; LBP- low back pain; FABQ- Fear Avoidance Beliefs Questionnaire; FABQPA-Fear Avoidance Beliefs Questionnaire Physical Activity Subscale
The importance of matching patient treatment to a specific subgroup has continued to receive widespread attention13, 14. Flynn et al15 established a clinical prediction rule (CPR) to accurately identify subgroups of patients likely to benefit from thrust spinal manipulation. An increase in likelihood of success with manipulation, from 45% to 95%, occurred when patients satisfied four of the five criteria comprising the CPR. The five variables included duration of symptoms < 16 days; Fear Avoidance Beliefs Questionnaire (FABQ) work subscale score < 19; at least one hip with > 35° internal rotation; hypomobility in the lumbar spine, and no symptoms distal to the knee15. More recently, this CPR was validated through a multi-center randomized clinical trial16.
Long et al17 investigated a subgroup of patients expected to respond to a specific exercise preference. Patients found to have a directional preference through examination were randomized into matched direction, opposite direction, and general exercises. Those treated in the matched direction group reported significant improvements with regard to back pain intensity, leg pain intensity, Roland-Morris Disability score, medication use, and interference with activity when compared to both other groups.
Hicks et al18 developed a preliminary CPR to identify patients likely to respond favorably to specific stabilization exercises. The four variables indicative of success included age < 40 years old; average straight leg raise > 91°; the presence of aberrant movements; and a positive prone instability test. The presence of three or more of these four variables indicated the best prognosis for success with specific stabilization exercise. Brennan et al11 also demonstrated that patients with LBP achieved greater and more rapid functional improvement if they received intervention strategies matched to their specific subgroup.
Each of the aforementioned studies investigated the treatment of non-specific LBP within subgroups using a treatment-based classification system. With the exception of the study by Brennan et al11, each of these studies used a matched versus unmatched treatment approach. In contrast, Brennan et al11 used a more pragmatic approach to more closely mimic clinical practice. In their study, a randomized treatment group decision determined the initial intervention, and if the patient progressed into a second, sub-acute stage, a more general approach was used. In this sub-actue stage progression of treatment was permitted to more accurately reflect clinical practice in which treatment is typically altered and advanced as improvements are made. Clinicians were able to use the mechanism-based classification approach to address impairments in muscle length as they saw fit.
In clinical practice, therapists often combine treatment- and mechanism-based classification systems. This case series describes a dynamic pragmatic management approach combining a treatment-based and mechanism-based classification system in four patients referred to physical therapy with a chief complaint of LBP.
Examination and Classification
To be eligible to participate in this case series, patients had to present to one of two physical therapy clinics (Rehabilitation Services of Concord Hospital, Concord, NH, or Rehabilitation Services of the Regional Transportation District, Denver, CO) with a primary report of pain and/or numbness in the lumbar spine, buttock, and/or lower extremity. They also had to be between 18 and 80 years of age. Patients were excluded from the study if red flags were noted in the participant's general medical screening questionnaire (e.g., tumor, metabolic diseases, rheumatoid arthritis, osteoporosis, prolonged history of steroid use, etc.), current pregnancy, medical history of osteoporosis or spinal compression fracture, or signs consistent with nerve root compression. The operational definition of such signs included reproduction of low back or leg pain with straight leg raise at < 45°; muscle weakness involving a major muscle group of the lower extremity; diminished lower extremity muscle stretch reflex (quadriceps or Achilles tendon); or diminished or absent sensation to pinprick in any lower extremity dermatome. This case series was approved by the Human Investigations Committee of Concord Hospital, Concord, NH, and the Institutional Review Board of Franklin Pierce College, Concord, NH.
Enrollment occurred if patients met inclusion criteria and were negative on the exclusion criteria, agreed to participate, and signed the informed consent. On initial evaluation, the patients completed self-report measures including a body diagram, numeric pain rating scale (NPRS), modified Oswestry Disability Index (ODI), FABQ, and—at follow-up examinations—the Global Rating of Change (GROC). The initial evaluation also included a physical examination conducted by one of two physical therapists with 3 and 3.5 years of experience, respectively, or a student physical therapist in the last semester of a Master's of Physical Therapy program. Demographic data collected included age, gender, employment status, and medical history.
We used a body diagram to assess distribution of symptoms. Location of symptoms was categorized as low back, buttock, thigh, and/or leg (distal to knee). Werneke et al19 reported high interrater reliability (κ=0.96) for this method of scoring the body diagram.
The 11-point NPRS ranges from 0 (“no pain”) to 10 (“worst pain imaginable”). We used the NPRS to have patients indicate the intensity of current pain and at its lowest and highest level over the last 24 hours18. These three ratings were averaged to arrive at an overall pain score. The scale has been shown to have adequate reliability, validity, and responsiveness in patients with LBP; its minimal clinically important difference (MCID) has been identified as two points16.
The ODI is a condition-specific disability scale for patients with LBP, consisting of 10 items addressing different aspects of function, each scored from 0-5 with higher values representing greater disability. The ODI used in this study was a version that was modified to improve compliance by replacing the section on sex life with one regarding employment/home-making. This modified ODI has been found to have high levels of reliability, validity, and responsiveness19. The MCID for the ODI has been identified at six points6.
Patients completed the FABQ Work Subscale (FABQW), a 7-item scale measure assessing fear-avoidance beliefs about the influence of work activities on back pain predictive of work loss and long-term disability19, 20. Each item is scored from 0–6 with possible total scores ranging between 0–42 and higher scores representing increased fear-avoidance beliefs.
At follow-up examinations, we used the GROC. This scale ranges from –7 (a very great deal worse) with zero as the midpoint (about the same) to +7 (a very great deal better). Intermediate descriptors of worsening or improving are assigned values from –1 to –6 and +1 to +6, respectively. Jaeschke et al21 recommended that scores on the GROC between ±1 and ± 3 represent small changes, ± 4 and ± 5 moderate changes, and scores of ±6 and ±7 large changes.
Following completion of these self-report measures, each patient underwent a standard history and physical examination. Patient history included questions involving duration of symptoms, mechanism of injury, location of symptoms, prior episodes of LBP, and the effect of any treatments received for current or past episodes. The physical examination included neuroconductive tests, posture assessment, neurodynamic tests, and lumbar joint movement and mobility tests.
The neuroconductive examination consisted of L1-S1 myotomal manual muscle testing, L1-S1 dermatomal pinprick sensation testing, and quadriceps and Achilles deep tendon reflexes. McCombe et al22 reported κ-values of 0.1-0.85 for interrater reliability of lower extremity manual muscle testing in patients with LBP. Katz et al23 reported a sensitivity of 0.47 and a specificity of 0.81 for identifying the presence of neurological impairment for sensation assessment using a pinprick test. The interrater reliability of ankle reflex testing has been found to be low to moderate, with κ-values ranging from 0.39 to 0.5024.
Posture was assessed in a standing position according to the description provided by Kendall25. Although some investigators have examined the reliability of postural measurements using photography or radiography, the reliability of postural observations have not been extensively investigated. Griegel-Morris et al26 studied the reliability of judgments of postural deviations from a plumb line on a 0–5 scale and reported a high degree of reliability (κ=0.83); however, individual postural deviations were not assessed. Studies judging the reliability of individual postural observations in the lumbar spine have not shown high levels of reliability (κ=0.32–0.50)9.
The neuroconductive examination consisted of the straight leg raise, prone knee bend, and slump test27. The interrater reliability for detecting a positive slump test has been shown to be high (κ=0.83)28.
Movement testing of the lumbar spine included range of motion (ROM), observation for aberrant movement, and quadrant testing. Fritz et al29 studied interrater reliability of single inclinometer lumbar flexion and extension ROM measures in 49 patients with LBP referred for flexion-extension radiographs; intraclass correlation coefficients were 0.60 and 0.61 for flexion and extension, respectively. Aberrant movements have been described as a painful arc in flexion or on return from flexion, an instability catch, Gower's sign, and reversal of lumbopelvic rhythm31. Observation of aberrant movements during trunk flexion has shown moderate levels of interrater reliability (κ=0.60)30. Haswell31 studied interrater reliability of quadrant testing and reported κ-values for the provocation of pain at 0.39 for the positions of flexion, sidebending, and rotation, and values of 0.29 for the positions of extension, sidebending, and rotation31.
Joint mobility testing was performed to the lumbar spine using the spring test32. The stiffness at each segment was judged on a 3-point scale as normal, hypomobile, or hypermobile, and symptom response was recorded. Interrater identification of specific lumbar segments has shown poor reliability33. Despite the lack of reliability, assessing segmental mobility has been found to be beneficial for identifying patients with LBP who are likely to respond to manipulation or stabilization intervention strategies29.
The therapists then used the data collected from the self-report questionnaires, the standard history, and the physical examination to classify a patient into a specific subgroup according to the algorithm reported by Fritz et al12 (Figure 1). If the patient did not accurately fit into one classification, the evaluating therapist utilized clinical judgment to determine the subgroup that most accurately represented the patient's condition.
Case Reports
Patient #1
History
Patient #1 was a 46-year-old male with reports of left-sided low back and groin pain. Onset of symptoms was 13 days prior to the physical therapy examination and occurred suddenly after getting up from the floor. The patient was able to continue work as a systems programmer; pain limited his workout routine and occurred when getting into and out of his car. No diagnostic imaging was performed. The patient reported a history of three to five previous episodes of LBP with increasing frequency. He had received many conservative treatments including medication and exercise, but manipulation seemed to be the only treatment that had produced a beneficial effect in the past. Demographic data can be found in Table 1.
TABLE 1.
Demographic data for all patients included in this case series.
| Demographics and History | ||||
|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
| Age | 46 | 44 | 51 | 56 |
| Gender | Male | Female | Male | Male |
| Chief complaint | Left-sided low back and groin pain | Left buttock pain and pins and needles down the left medial leg | Right-sided buttock pain | Right-sided lumbosacral pain |
| Onset of symptoms | Occurred suddenly after getting up off of the floor | Gradual onset of symptoms | Sudden onset after 18-hour work day | Sudden onset after performing trunk flexion and rotation while lifting 40# box |
| Time between onset of symptoms and physical therapy evaluation | 13 days | 6 weeks | 4 days | 3 days |
| Categorization of postures | ||||
| Best | Standing, walking | Walking, lying supine | Standing, walking | Lying, sitting |
| Worst | Flexion/right sidebending | Standing, sitting | Sitting | Bending, walking, standing, transitioning |
| Prior history of back pain | 3-5 episodes becoming more frequent | 2 episodes | 5 episodes increasing in frequency | 10-year history of LBP episodes |
| Treatment received for prior episodes | Responded favorably to manipulation in the past | Responded favorably to medication | Responded favorably to physical therapy in the past | Responded favorably to manipulation in the past |
| No effect from manipulation | ||||
LBP–low back pain
Physical Examination
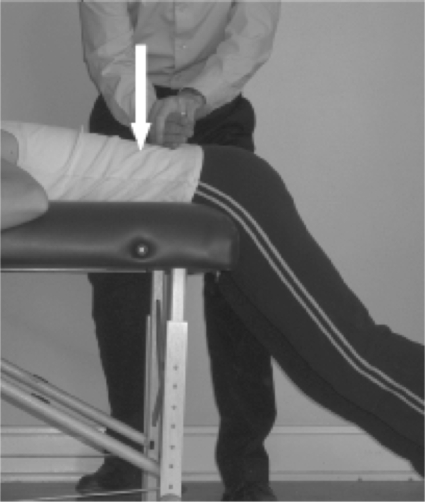
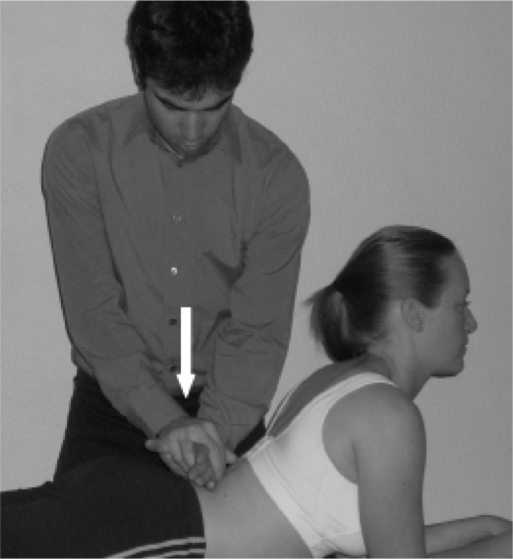
No deviations were noted during postural observation. The neurological examination revealed sensory, motor, and muscle stretch reflexes within normal limits. Range of motion was symmetric and full with the exception of a painful arc on return from a flexed trunk position and pain with right sidebending. Spring testing of the lumbar vertebrae indicated hypomobility at the levels L2–L5. The prone instability test was negative (Figures 2A and 2B). Specific findings of the examination can be found in Table 2.
Fig. 2.
Prone instability test, part one: Painful posteroanterior pressure while feet are on floor, erector spinae relaxed. Prone instability test, part two: Painless posteroanterior pressure with legs elevated from floor, erector spinae tense.
TABLE 2.
Clinical examination findings for all patients in this case series.
| Examination | ||||
|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
| Observation | No deformity noted
Normal gait |
Reduction in the lordotic lumbar curve and antalgic gait | Reduction in the lumbar lordotic curve
Normal gait |
Increased anterior pelvic tilt and antalgic gait |
| Neurological examination | No deficits in sensation | No deficits in sensation | No deficits in sensation | No deficits in sensation |
| No deficits in LE strength | Diminished left quadriceps | No deficits in reflexes | No deficits in reflexes | |
| No deficits in reflexes | No deficits in LE strength | No deficits in LE strength Positive femoral nerve tension test bilateral | No deficits in LE strength | |
| Movement testing | Painful arc on return from a flexed trunk position and pain with right sidebending | Increased pain with flexion and decreased pain with centralization of symptoms in extension | Painful right sidebending and extension | Increased pain with all movements, extension most significantly limited |
| Spring testing | Hypomobility at the levels L2-L5 | Hypomobility at L4 | Hypomobility lumbar spine | Hypomobility at L4/5 |
| Prone instability test | Negative | Negative | Negative | Negative |
| Aberrant movement | Positive | Positive | Positive | Positive |
| Oswestry score | 12% | 26% | 30% | 68% |
LE-lower extremity
Classification and Intervention
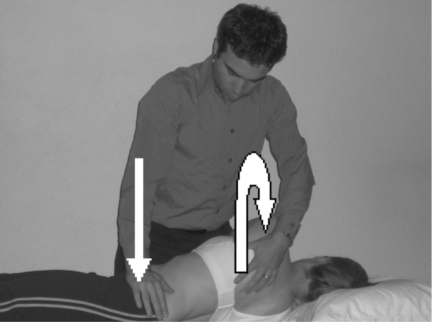
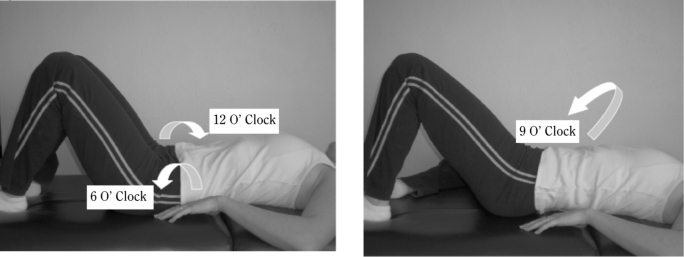
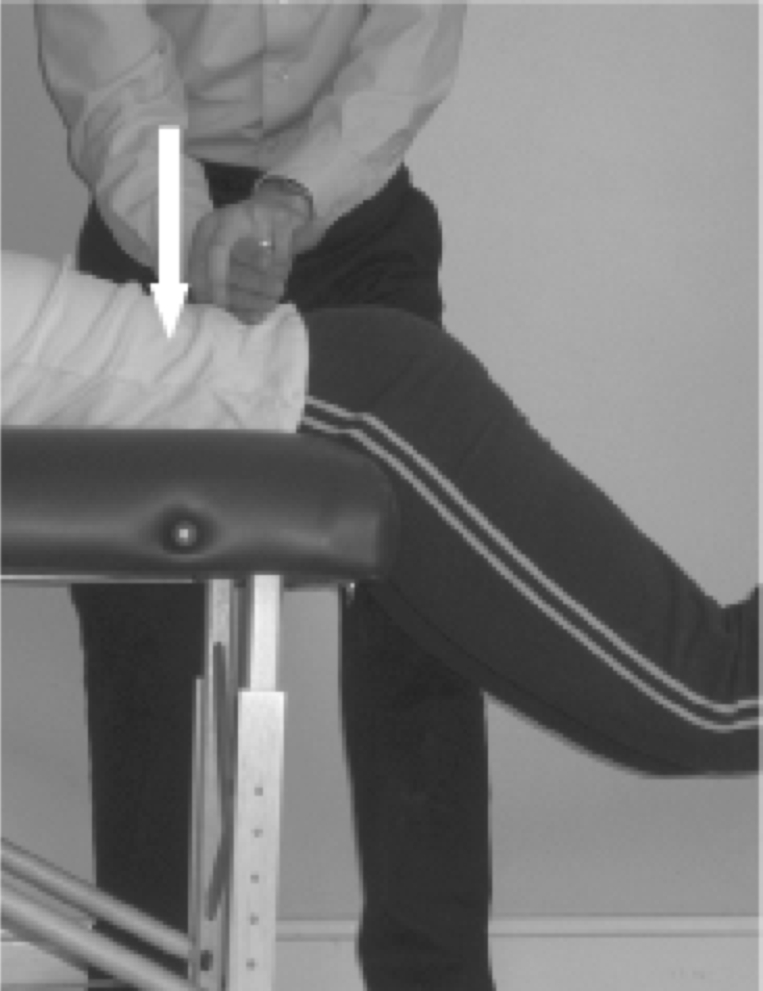
The treating therapist determined the patient would best fit in the mobilization/manipulation category as the patient satisfied four of five criteria for this subgroup (Figure 1). Treatment was initiated as suggested by the classification system and it focused on central and unilateral posteroanterior mobilizations directed at segments L2–L5. Sidelying rotational mobilizations and thrust manipulations directed at the lumbar spine (Figure 3) and lumbopelvic spine (Figure 4), and a basic pelvic range of motion exercise were also administered (Figures 5A and 5B). Treatment continued in this fashion for two sessions.
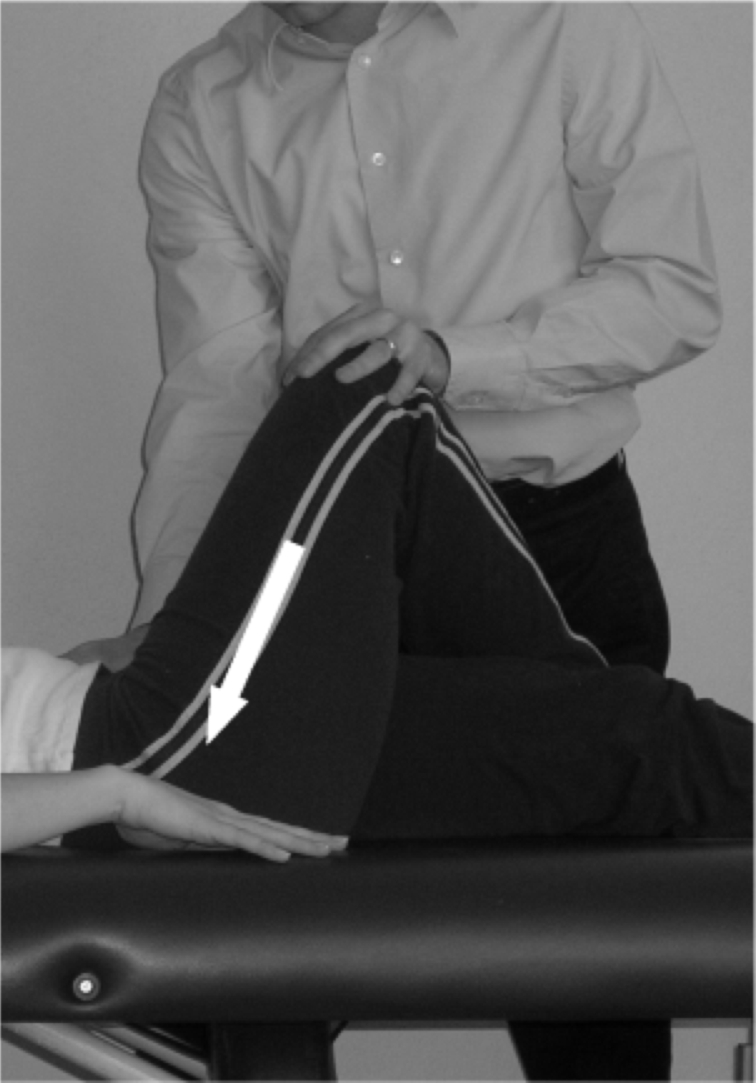
Fig. 3.

Lumbar side lying rotational mobilizations and thrust manipulations used in this case series.
Fig. 4.
Lumbopelvic thrust manipulation technique used in this case series.
Fig. 5.
Pelvic clock: 12 O'clock and 6 O'clock. Pelvic clock toward 9 O'clock.
Outcomes
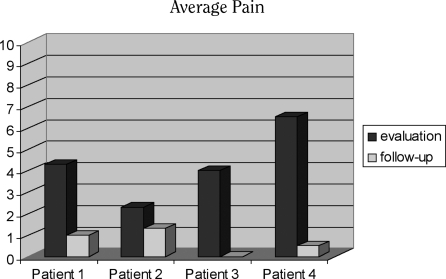
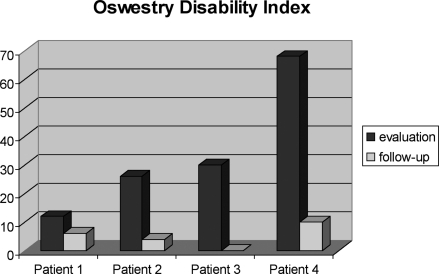
At the time of the third treatment, the patient's ODI score had decreased by half from a baseline score of 12% to 6%. On the GROC, the patient indicated that he was “a great deal better” from the time he began treatment. The patient reported no longer experiencing symptoms in the groin. The pain in his lower right lumbar spine decreased from an average of 4.25/10 to 1/10 on the NPRS. At this time the patient was able to get out of his car without groin pain and with only minimal LBP.
The treating clinician then focused the subsequent sessions on impairments found during examination. Hypomobility of the posterior hip joint was addressed with grade III–IV posterior femoroacetabular mobilizations32 (Figure 6). Whitman et al34 have demonstrated favorable outcomes in patients with LBP and spinal stenosis who received treatment of underlying impairments distal to the low back, including joint mobilization applied to the hip joint. Hip flexion weakness at the end of ROM was addressed with strengthening exercises at the end range of hip flexion. Lumbopelvic hypomobility was further treated using a muscle energy technique35. These treatments were performed for the next two visits, and the strengthening exercises were prescribed as part of the home exercise program. The patient was then discharged from physical therapy with a full return to all functional activities. Pre- and post-test scores for pain and disability for this patient can be found in Figures 7 and 8.
Fig. 6.
Posterior femoroacetabular mobilizations
Fig. 7.
Pre and post test scores for pain for all patients.
Fig. 8.
Pre and post test scores for disability for all patients.
Patient #2
History
Patient #2 was a 44-year-old female employed as an engineering technician with complaints of left buttock pain and “pins and needles” in the left medial leg. She reported a gradual onset of symptoms approximately six weeks prior to her initial examination. Symptoms increased with standing or sitting and improved with walking or lying supine. Her functional deficits included sitting or standing for greater than one hour, dressing her lower body, and bathroom mobility. The patient had a history of two episodes of LBP. Previous treatments included medication that improved symptoms and manipulation that had had no effect on her complaint. Demographic data can be found in Table 1.
Physical Examination
Postural observation revealed a reduction in the lordotic lumbar curve. The neurological examination revealed normal sensory and motor testing with the exception of a diminished muscle stretch reflex at the left quadriceps muscle. Movement testing revealed increased pain with flexion and a painful arc on return from flexion. Repeated extension decreased pain and centralized symptoms to her low back. Spring testing of the lumbar vertebrae indicated hypomobility at L4. Hip internal rotation tested at 0° was measured at 30° on the right and 40° on the left. Specific findings of the examination can be found in Table 2.
Classification and Intervention
Based on the findings during the clinical examination, the treating therapist determined the patient most accurately fit the specific exercise classification because the patient had a preference for one posture and centralization of symptoms with repeated lumbar movement testing. On the day of the initial evaluation, the patient was prescribed a home exercise program consisting of prone and standing extension exercises (Figures 9A and 9B). The patient received treatment two times a week for three weeks. The treatments focused on progression of the extension exercises and joint mobilizations directed at hypomobile segments while prone on elbows (Figure 10). Browder et al36 demonstrated that patients whose symptoms centralized with extension benefited from extension exercises combined with lumbar spine postero-anterior joint mobilizations. On the sixth visit, the patient reported that her symptoms were “moderately better” on the GROC. Her symptoms centralized to her left buttock region, and her pain decreased from an average of 2.25/10 to 1.25/10 on the NPRS. Her ODI score decreased from 26% to 4%. She no longer fit the specific exercise classification, as her symptoms were no longer altered by single or repeated lumbar movements. Pre- and post-test scores for pain and disability can be found in Figures 7 and 8. The treating physical therapist included specific stabilizing exercises for an additional two visits. Specific stabilizing exercises have been shown to reduce the recurrence rate in first-time LBP patients and to decrease pain and functional disability levels in chronic LBP patients37. The exercises used were selected from exercises as used by Hicks et al18.
Fig. 9.

Home exercise programs of prone and standing extension used with patient #2.
Fig. 10.
Postero-anterior joint mobilizations used in this case series.
Patient # 3
History
Patient #3 was a 51-year-old male who reported to physical therapy with a four-day history of right-sided buttock pain. The patient's symptoms began after working an 18-hour day in his bakery. Symptoms increased with sitting and improved with standing or walking. The patient was unable to continue working at full capacity since he could not stand for long periods as a result of his symptoms. Medical history revealed a history of LBP that had resulted in a multilevel spinal fusion at L4-L5 four years prior to this episode.
Physical Examination
Postural observation revealed a decrease in the lumbar lordotic curve. Neurological screening revealed normal sensation, muscle stretch reflexes, and myotomal strength tests. During motion testing, the patient demonstrated aberrant movement; trunk extension and sidebending right increased his symptoms. Repeated extension and flexion did not change the symptoms. Central lumbar spring testing revealed hypomobile segments from L1 to L3. Hip internal rotation tested at 0° was 60° on the right and 70° on the left. Specific findings of the examination can be found in Table 2.
Classification and Intervention
The treating therapist determined that the patient would best fit the stabilization classification due to the presence of aberrant movements and > 3 prior episodes of LBP (Figure 1). Treatment focused on progressive trunk stabilization exercises and was advanced at the treating therapist's discretion.
On treatment session three (12 days after the examination), the patient's ODI score decreased from 30% to 4%. On the GROC, the patient indicated he was “a very great deal better,” and his average buttock pain decreased from 4/10 to 0.5/10 on the NPRS. At this time, he could perform all work duties and was no longer experiencing any functional limitations. On his next visit, he reported no pain and an ODI score of 0%; he was discharged from physical therapy with instructions to continue his exercise program. Pre-and post-test scores for pain and disability can be found in Figures 7 and 8.
Patient #4
History
Patient #4 was a 56-year-old male who reported to physical therapy with complaints of posterior LBP (right greater than left-sided) three days after an injury at work. The patient reported rotating and flexing his trunk, while attempting to lift a 40-pound tub of supplies from the back of a sport utility vehicle. He noticed a “shift” in his back and “knew that he did something bad.” Tying his shoes, bending, walking, lifting, and standing aggravated his symptoms. He was unable to return to work due to his injury. The patient reported a chronic history of LBP for “at least ten years,” for which he indicated manipulation had been helpful. Specific historical findings can be found in Table 1.
Physical Examination
Postural observation revealed a lateral shift to the left. Neurological screening revealed normal sensation, muscle stretch reflexes, and myotomal strength tests. Range-of-motion assessment revealed significant limitations in all directions. Specific findings of the examination can be found in Table 2.
Classification and Intervention
The treating therapist determined the patient would best fit in the mobilization/manipulation classification based on presentation. The patient satisfied three of five criteria for lumbosacral manipulation: lumbar spine hypomobility at L4–L5; < 16 days since onset of injury; and no symptoms distal to the knee. After the initial examination, the patient received manipulation directed at the lumbopelvic region and was instructed in the performance of pelvic clock exercises at home.
During the second treatment session the patient reported a decrease in average pain from 6.5/10 to 6/10 on the NPRS. His pain distribution changed to include pain in the proximal to middle medial right thigh. His symptoms centralized with repeated lumbar extension. He was instructed in lateral shift correction exercises and extension-based exercises to be performed 10 times per hour. The patient was also instructed to continue performing his pelvic clock exercises from three o’clock to nine o’clock and to six o’clock but to eliminate the performance of pelvic tilts to 12 o’clock. The pelvic tilt toward 12 o’clock was eliminated because it increased his pain. By the third session, the patient's average pain level was reduced to 3.5/10 on the NPRS. He no longer had complaints of thigh symptoms. His ODI score decreased from 68% to 42%. He was instructed in proper posture when sitting, as this was a major function of his job. During the fourth session, the patient was manipulated again because he still fit in the mobilization/manipulation category and he was not demonstrating continued progress with the utilization of repeated movements. By the fifth session, his ODI score decreased to a 32%. During the fifth session, he was instructed in general stabilization exercises because of his ten-year history of LBP. On the sixth visit, one week following the patient's return to work, his ODI score was further reduced to 10% and average pain level was 0.5/10 on the NPRS. Pre- and post-test scores for disability and pain can be found in Figures 7 and 8. He rated the GROC as “quite a bit better.” The patient also reported that he had received spinal manipulation by a different provider during the week between the fifth and sixth visits. Prior to being discharged from PT, his stabilization exercise program was reviewed and he was instructed in exercise progression principles.
Discussion
The origin of LBP is difficult to establish, complicating the use of the pathoanatomical model to guide appropriate management38. In addition, there is conflicting evidence on the effectiveness of mechanism-based treatment for the management of LBP38. The treatment-based system for the treatment of LBP has demonstrated significant improvements when patient treatment is matched with subgroup classification. The treatment-based system is designed to place patients in a treatment category and to provide them with the treatment most likely to be successful. In this case series, the treating therapists were given the freedom to use treatment principles from multiple subgroups if patients fit into more than one subgroup. They were also free to use mechanism-based treatment after classifying patients into a subgroup and beginning treatment accordingly. The treating therapists in this study were novice clinicians, all with ≤ 3.5 years experience, and one was still a student in a graduate physical therapy program at the time this case series was completed. While some might consider the lack of experience as a limitation, it has been demonstrated that there is no difference in reliability between novice and expert clinicians in the use of the treatment-based classification system for the low back12.
A 6-point change on the ODI39 and a 2-point change on the NPRS40 represent the MCID for these tools. This case series further illustrates the effectiveness of a treatment-based classification, as all patients in this study achieved results exceeding these clinically meaningful changes. Patient #1 had a 3.25-point decrease in his average NPRS and a 6-point decrease in his ODI over the course of three physical therapy visits. After six physical therapy visits, patient #2 reported only a 1-point change in her LBP and a 12-point reduction in her ODI score. The authors hypothesize that the small magnitude of change in pain intensity could have been affected by the low pain level originally reported possibly resulting in a floor effect. Patient #3 achieved a 3.5-point improvement on his NPRS and a 30-point improvement in his ODI in four visits. Patient #4 had a 58-point improvement on his ODI after five visits. He also had a 6.5-point change on NPRS.
The treatment-based classification system utilized in this case series is a dynamic process. The patient may fit into one or more categories on the initial examination. As the patient's clinical presentation changes, the original classification may no longer be accurate, and the clinician must reassess the patient to determine whether another category is more appropriate. Additionally, after the patient progresses out of a particular subgroup, the clinician may find that a mechanism-based approach is more beneficial11. For example, Patient #1 no longer improved with the treatment recommended in the manipulation/mobilization category at treatment session three; therefore, the clinician decided to address impairments identified on reexamination. Patient #2 was classified into the subgroup that includes specific extension exercises. Her symptoms centralized by the sixth visit; she no longer satisfied the criteria of the extension group. The clinician determined that the patient would benefit from stabilization exercises; she continued to improve and was discharged from physical therapy three visits later. Patient #3 fit the criteria for the manipulation subgroup; however, the treating clinician did not believe that introducing motion into the lumbar spine would be advantageous as a result of the prior spinal fusion. The therapist determined that the next classification the patient most accurately satisfied was the stabilization group. The patient remained in this subgroup for four visits after which he reported no pain or disability and was discharged from physical therapy. Patient #4 was deemed appropriate for manipulation by satisfying three of the five criteria for that subgroup. The patient's presentation changed on his second visit. With less pain overall and more mobility, he was found to improve with repeated movements into extension. On his fourth visit, he appeared to no longer benefit from repeated extension. Acknowledging that he still fit into the manipulation group, the treating physical therapist manipulated his lumbopelvic region for a second time. On the fifth visit, he was experiencing minimal pain. Due to his long history of LBP, he was instructed in stabilization exercises. This patient was also instructed in proper posture while sitting due to prolonged periods of sitting while performing his job. After one week at work, the patient arrived for his final physical therapy visit. The patient reported that he had gone to a chiropractor because of difficulty rotating while sitting in his car. Although this complicates the assessment of treatment outcome, manipulation was compatible with the patient's treatment-based classification making it irrelevant whether this appropriate intervention was performed by his treating physical therapist or by another practitioner.
Due to the inherent limitations of a case series, a cause-and-effect relationship cannot be inferred. However, the intention of this series is to describe the clinical reasoning process of clinicians when deciding how to classify patients into subgroups and to provide examples for treating impairments within a subgroup. It has been demonstrated that patients receiving treatment matched to their classification will experience improved outcomes as compared to those who receive unmatched treatment11.
A further limitation of this case series is that only short-term outcomes for disability and pain were captured. However, despite its limitations, this case series may serve to illustrate that the classification system is a dynamic process in that the patient's classification may change throughout the course of treatment. In addition, outcomes may be further improved if clinicians address impairments while continuing to treat within a particular classification subgroup as illustrated in this case series.
Conclusion
As costs for treating LBP continue to rise, it is imperative that clinicians maximize the patient's likelihood of achieving a successful outcome. This case series illustrates the pragmatic combination of a treatment-based classification approach with a mechanism-based classification system in the diagnosis and management of patients with LBP. Additional research is indicated to further define the usefulness of this approach to the treatment of patients with LBP.
REFERENCES
- 1.Frymoyer JW. Predicting disability from low back pain. Clin Orthop. 1992;9:101–109. [PubMed] [Google Scholar]
- 2.Bhargava A, Gelb D, Ludwig S, DePalma MJ. Physical therapy for low back pain. Curr Opin Orthop. 2006;17:207–211. [Google Scholar]
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 4.Riddle DL. Classification and low back pain: A review of the literature and critical analysis of selected systems. Phys Ther. 1998;78:708–737. doi: 10.1093/ptj/78.7.708. [DOI] [PubMed] [Google Scholar]
- 5.Abenhaim L, Rossignol M, Gobeille D, Bonvalot Y, Fines P, Scott S. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine. 1995;20:791–795. doi: 10.1097/00007632-199504000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: Identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–485. doi: 10.1093/ptj/75.6.470. [DOI] [PubMed] [Google Scholar]
- 7.McKenzie R. Mechanical diagnosis and therapy for disorders of the low back. In: Twomey L, Taylor J, editors. Physical Therapy of the Low Back. Philadelphia, PA: Churchill Livingstone; 2000. pp. 141–165. [Google Scholar]
- 8.Dankaerts W, O'Sullivan PB, Straker LM, Burnett AF, Skouen JS. The inter-examiner reliability of a classification method for non-specific chronic low back pain patients with motor control impairment. Man Ther. 2006;11:28–39. doi: 10.1016/j.math.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78:979–988. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- 10.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: A randomized clinical trial. Spine. 2003;28:1363–1371. doi: 10.1097/01.BRS.0000067115.61673.FF. [DOI] [PubMed] [Google Scholar]
- 11.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: Results of a randomized clinical trial. Spine. 2006;31:623–631. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 12.Fritz JM, Brennan GP, Clifford SN, Hunter SJ, Thackeray A. An examination of the reliability of a classification algorithm for subgrouping patients with low back pain. Spine. 2006;31:77–82. doi: 10.1097/01.brs.0000193898.14803.8a. [DOI] [PubMed] [Google Scholar]
- 13.Bouter LM, van Tulder MW, Koes BW. Methodologic issues in low back pain research in primary care. Spine. 1998;23:2014–2020. doi: 10.1097/00007632-199809150-00019. [DOI] [PubMed] [Google Scholar]
- 14.Delitto A. Clinicians and researchers who treat and study patients with low back pain: Are you listening? Phys Ther. 1998;78:705–707. doi: 10.1093/ptj/78.7.705. [DOI] [PubMed] [Google Scholar]
- 15.Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27:2835–2843. doi: 10.1097/00007632-200212150-00021. [DOI] [PubMed] [Google Scholar]
- 16.Childs JD, Fritz JM, Flynn TW, et al. A clinical prediction rule to identify patients likely to benefit from spinal manipulation: A validation study. Ann Intern Med. 2004;141:920–928. doi: 10.7326/0003-4819-141-12-200412210-00008. [DOI] [PubMed] [Google Scholar]
- 17.Long AL, Donelson R, Fung T. Does it matter which exercise? Spine. 2004;29:2593–2602. doi: 10.1097/01.brs.0000146464.23007.2a. [DOI] [PubMed] [Google Scholar]
- 18.Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86:1753–1762. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 19.Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: Relationships with current and future disability and work status. Pain. 2001;94:7–15. doi: 10.1016/S0304-3959(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 20.Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine. 1992;17:617–628. doi: 10.1097/00007632-199206000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Jaeschke R, Singer J, Guyatt G. Measurement of health status: Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 22.McCombe PF, Fairbank JC, Cockersole BC, Pynsent PB. Reproducibility of physical signs in low-back pain. Spine. 1989;14:908–918. doi: 10.1097/00007632-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Katz J, Dalgas M, Stucki G, Katz N, Bayley J, et al. Degenerative lumbar spinal stenosis: Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236–1241. doi: 10.1002/art.1780380910. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz RS, Morris JG, Crimmins D, et al. A comparison of two methods of eliciting the ankle jerk. Aust N Z J Med. 1990;20:116–119. doi: 10.1111/j.1445-5994.1990.tb01286.x. [DOI] [PubMed] [Google Scholar]
- 25.Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. 4th ed. Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- 26.Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther. 1992;72:425–431. doi: 10.1093/ptj/72.6.425. [DOI] [PubMed] [Google Scholar]
- 27.Butler DS. Mobilisation of the Nervous System. 1st ed. Melbourne, Australia: Churchill Livingstone; 1991. [Google Scholar]
- 28.Philip K, Lew PC, Matyas T. The inter-therapist reliability of the slump test. Aust J Physiother. 1989;35:89–94. doi: 10.1016/S0004-9514(14)60499-2. [DOI] [PubMed] [Google Scholar]
- 29.Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: An examination of validity for determining intervention strategies in patients with low back pain. Arch Phys Med Rehabil. 2005;86:1745–1752. doi: 10.1016/j.apmr.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 30.Hicks G, Fritz J, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84:1858–1864. doi: 10.1016/s0003-9993(03)00365-4. [DOI] [PubMed] [Google Scholar]
- 31.Haswell K. Interexaminer reliability of symptom-provoking active sidebend, rotation, and combined movement assessments of patients with low back pain. J Manual Manipulative Ther. 2004;12:11–20. [Google Scholar]
- 32.Maitland G, Hengeveld E, Banks K, English K. Maitland's Vertebral Manipulation. 6th ed. Oxford, UK: Butterworth-Heinemann; 2000. [Google Scholar]
- 33.Binkley J, Stratford PW, Gill C. Interrater reliability of lumbar accessory motion mobility testing. Phys Ther. 1995;75:786–792. doi: 10.1093/ptj/75.9.786. [DOI] [PubMed] [Google Scholar]
- 34.Whitman JM, Flynn TW, Childs JD, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: A randomized clinical trial. Spine. 2006;31:2541–2549. doi: 10.1097/01.brs.0000241136.98159.8c. [DOI] [PubMed] [Google Scholar]
- 35.Greenman P. Principles of Manual Medicine. 2nd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 1996. [Google Scholar]
- 36.Browder DA, Childs JD, Cleland JA, Fritz JM. Effectiveness of an extension oriented treatment approach in a subgroup of patients with low back pain: A randomized clinical trial. Phys Ther; In Review. [DOI] [PubMed]
- 37.Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26:E243–E248. doi: 10.1097/00007632-200106010-00004. [DOI] [PubMed] [Google Scholar]
- 38.Jull G. Editorial-Classification systems in clinical practice. Physiother Res Int. 2004;9:iii–iiv. doi: 10.1002/pri.317. [DOI] [PubMed] [Google Scholar]
- 39.Fritz JM, Irrang JJ. A comparison of a modified Oswestry Low Back Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 40.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30:1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]