My career in physical therapy started over 40 years ago when in 1966 I graduated with my entry-level degree. In 1980, after 14 years of full-time clinical practice, I started graduate study, which culminated in 1988 in a PhD on the topic of functional vertebrobasilar insufficiency1. This was followed by an appointment as a professor of manual therapy at the Vrije Universiteit Brussel in Belgium and an appointment as a professor of allied health sciences at the Radboud University Nijmegen Medical Centre in the Netherlands. I had the opportunity to serve as a dissertation supervisor for 20 PhD students and am still actively involved as supervisor for an additional 14 students. I have been fortunate to be involved in interdisciplinary research in the areas of Parkinson disease, neuromuscular disorders, complex regional pain syndrome (CRPS) and whiplash syndrome, low back pain (LBP), motor dysfunction in premature children and children with Turner syndrome, facial paralysis, rheumatoid arthritis (RA), degenerative joint disease (DJD), lumbar disk herniation, repetitive strain injury (RSI), cervical pain, headache, dizziness, and chronic pain. This research has resulted in over 300 peer-reviewed publications in national and international journals. In addition I served as the scientific director of the Dutch Institute of Allied Health Care for almost 20 years. Recently I retired from all these appointments. This long and rather varied career in the field in a time when physical therapy has gone through turbulent developments has afforded me a perhaps unique perspective and was the reason why my former student and now editor of the Journal, Dr. Peter Huijbregts, invited me to share some insights in this guest editorial.
Early Days
From my early days in the field really up until the 1990s, opinion, authority, and experience-based knowledge dominated clinical care as exemplified by authorities such as Kaltenborn, Paris, McKenzie, Grieve, Maitland, and Maigne. Those trained in manual physical therapy (MPT) back then will undoubtedly remember the varied theoretical models and rationales later shown to be inconsistent with scientific data. Depending on the school of thought in which one was trained, certain theories, e.g., on the nature of intervertebral segment fixations, were elevated to dogma while competing rationales were summarily discarded. In the Netherlands, various schools within MPT vied for primacy, a situation certainly not unique to this country. I too was trained in this system where one apprenticed with an acknowledged “master” and despite the shortcomings of this educational model, to this day I consider myself blessed to have learned from people such as Henk Hesp, Freddy Kaltenborn, Professors Jan Bernards, Vladimir Janda, Karl Lewit, and Dr. Herbert Frisch.
However, it was inevitable that at the end of the last century, not only government, society, and third-party payers but also professional associations and individual therapists began to question the efficacy of MPT and the dogmatic belief in its underlying theoretical constructs. The field of MPT in the Netherlands owes an immense debt of gratitude to Professor Lex Bouter, now rector of the Vrije Universiteit Amsterdam, and to others following his lead, including Professors Bart Koes and Maurits van Tulder in that they offered the field the tools to do the required research resulting in a great many publications including a multitude of systematic reviews in first-tier international journals. Other countries have had their own influential colleagues mentoring the profession in the area of much needed scientific underpinning of the field. In this regard, Jules Rothstein, posthumously honored for his contributions to the field of physical therapy and MPT at the most recent WCPT conference in Vancouver, certainly deserves special mention.
The contrast between the beginning and end of my career is staggering. The prevailing paradigm within MPT has developed from authority and experience-based practice to evidence-based practice (EBP) with—in addition to patient values and clinician expertise—a role for data on diagnostic utility of clinical tests, results of randomized clinical trials (RCT), systematic reviews, clinical guidelines, and more recently, even systematic reviews of systematic reviews. However, despite the seeming promise held by EBP, there are issues related to research in MPT that affect the true and full implementation of this paradigm.
MPT Efficacy
Researchers have generally yet to establish MPT efficacy with the most obvious gap in evidence relating to support from systematic reviews based on RCTs2–4. Koes5 discussed the value but also drawbacks of the RCT as a means of gathering evidence on MPT, most notably the insufficient description of the content of MPT interventions studied in addition to methodological issues such as small sample size and lack of blinding. In a systematic literature review, article search strategy and inclusion and exclusion criteria are described meticulously allowing for replication and confirmation of the results. An important part of such a review is a methodological quality assessment of selected studies based on criterion lists such as the Maastricht-Amsterdam6, Cochrane7, and PEDro criterion lists8. In turn, systematic reviews are used to develop clinical practice guidelines9.
Systematic literature reviews are truly a double-edged sword. On the one hand, they promote adequate research methodology in future studies; on the other, they can impede progress because lack of evidence for efficacy may lead to premature restrictions imposed on clinicians by government or third-party payers. Results of systematic reviews have negatively impacted development and funding of MPT research despite emerging scientific evidence with regard to so-called non-specific health problems such as neck pain and LBP. This emerging evidence is exemplified by studies into MPT combined with a behavioral approach for patients with DJD of the knee and hip10,11, prognostic factors for patients with chronic neck and back pain12–15, the postoperative course of lumbosacral radiculopathy16, and the combined intervention of MPT and exercise therapy for patients with spinal pain. This shift in MPT content away from solely manual interventions so far has only been the subject of a few RCTs. Recently, Henschkel et al17 included these elements in a list of research priorities with regard to LBP, and in the Netherlands a national research agenda has been developed that includes MPT research.
MPT Diagnosis
Another issue relates to diagnostic utility of MPT tests. There are a multitude of MPT tests; the literature describes over 100 tests for the spine alone. However, Van Trijffel et al18 noted that, for example, interrater reliability of passive intervertebral segmental motion tests is poor to, at best, fair (κ=<0.00–0.40). Most diagnostic tests in MPT derive from a time when the diagnostic emphasis was on establishing tissue-specific impairments. The rationale was that diagnosis and treatment of this tissue-specific impairment would automatically lead to improved functioning. The main proponent of this systematic form of diagnosis aimed at identifying specific anatomical structures at fault was Dr. James Cyriax. In this context, we could use the example of a patient with shoulder pain, who in this paradigm might be diagnosed with, for example, tendinopathy of the supraspinatus. Ultimately, tissue-specific diagnosis is often not possible. In my opinion, this contributed to Green et al19 not being able to show between-group differences favoring MPT that consisted of a combination of ultrasound and deep friction massage aimed at specific anatomic structures in the shoulder over the control intervention. These and similar findings have led to a paradigm shift wherein tissue and pathology-specific diagnosis have been de-emphasized in favor of patient-specific and functional diagnosis. This shift is exemplified by the more frequent use of questionnaires to supplement diagnostic tests. Bot et al20 provided a review of questionnaires intended for patients with shoulder pain with an emphasis on limitations in activities and restrictions in participation. This patient-specific and functional diagnosis is arranged around five domains represented in the International Classification of Functioning, Disability and Health (ICF)21. This ICF provides a standardized terminology for expressing human functioning and alterations of the health state (Figure 1).
Fig. 1.
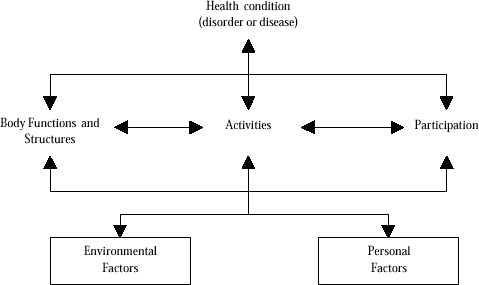
Interaction between the components of the International Classification of Functioning, Disability and Health (Adapted from World Health Organization, Geneva, 2001)
The ICF describes the interaction between different aspects of the health state (body structures and functions, activities, and participation) and external and personal factors. Diagnostic tests, outcome measures, and questionnaires have been classified according to the domain of the ICF they represent, e.g., for patients with rheumatoid conditions, confirming that the majority deal with the impairment rather than the activity or participation level22.
MPT Theory
Back when scientific study in the area of MPT was only just emerging, the prevailing sentiment was to stop asking how an intervention worked in favor of finding out if it worked. However, the questions as to how, with which patient, why, and under which circumstances an intervention is most effective indicate the need for a theoretical framework that provides a comprehensive description of underlying mechanisms. Outcome-based research does not provide answers to these types of questions. With our increasing knowledge of underlying mechanisms and prognostic factors, the time is ripe for a combination of outcome-based and theory-based research. Such research should incorporate new knowledge with regard to the physiology and psychology of chronic pain. Many health problems are labelled non-specific due to an absence of clear etiologic abnormality in anatomical structure; one need only consider non-specific low back, neck, and abdominal pain; chronic fatigue syndrome; and RSI. It is evident that for such health problems, the theoretical framework purely based on anatomy (but also including osteo- and arthrokinematics) falls short and that theory grounded in physiology and psychology is required to complement this anatomical structure-based framework.
The physiological theoretical framework suggested for use in MPT derives mainly from embryology and adaptation physiology of the locomotor systems. Adaptation physiology concerns itself with mechanisms for the dynamic equilibrium between load and load-bearing ability in the locomotor and other organ systems. Many of the above non-specific health problems can be better understood from a physiological than from an anatomical or structure-based theoretical framework. After all, people need to continually adapt to a changing environment in a physical, psychological, and social sense. This biopsychosocial model has permeated MPT as it has other areas of medicine23,24. In the Netherlands and in other European countries, I have had the opportunity to promote the biopsychosocial model within physical therapy and MPT together with Bernards and Hagenaars25,26. Together we introduced the terminology of local and general load adaptive capacity, adaptation process, and adaptation and segmental (dys)regulation within MPT.
The theoretical framework derived from psychology includes concepts such as self-efficacy, pain-related fear, somatization, catastrophizing, kinesiophobia, and willingness to alter behavior with regard to pain and movement; all these concepts are prognostic indicators for chronic pain that are increasingly supported by research14,15,27,28. After an initial period needed to determine the consequences that these initially foreign concepts might have for the daily clinical practice of MPT, the psychological theoretical framework has found a place within MPT: Therapists use behavioral principles to determine cooperatively with the patient the most appropriate movement strategy and they identify yellow flags that may indicate the need for referral to the general practitioner or a psychology consult.
Systematic Reviews and Knowledge Synthesis
With increasing frequency, earlier systematic reviews are summarized in a new systematic review with the goal of producing a best-evidence summary of systematic reviews29–31. Such reviews support research by way of summaries of relevant literature on a topic. However, external validity and clinical applicability of such reviews of reviews are often limited. Moore and Jull32 justifiably commented, “The systematic review of systematic reviews is an untested methodology at best and might take us even further away from the truth.” The main obstacles to clinical application of research findings reported in systematic reviews are the lack of information about patient characteristics, diagnostic process, clinically relevant treatment goals, the lack of specific description of MPT interventions used, and the variety of outcome measures used in RCTs.
Clinical Guidelines
In recent years, there has been important progress towards development, implementation, and evaluation of quality control systems in MPT. At the base of this initiative has been the development of clinical practice guidelines based on criteria of the Evidence-Based Guidelines Forum (Dutch: Evidence-Based Richtlijnen Overleg). Since 1993, this has led to the development of both process-related guidelines discussing, for example, standardization of clinical documentation, and clinical guidelines, such as the one on LBP. Currently, there are 18 such guidelines with many translated in English and made available at: http://www.fysionet.nl/index.html?dossier_id=81&dossiers=1. After initial resistance related to a perception of being forced to practice cookbook therapy, the growing awareness of the need for professionalization has resulted in increasing acceptance.
Of course, guideline development is pointless if there is no implementation of these guidelines. Guideline dissemination needs to lead to integration of guidelines in clinical practice, a process that has met with considerable resistance. Research into implementation has addressed both the most effective ways to disseminate and integrate guidelines into clinical practice and the effect of guidelines on the level of the clinician (does the clinician act according to the guidelines?) and on the level of the patient (does guideline-driven therapy result in better patient outcomes?). It is as of yet unclear which implementation strategy is most effective within MPT. Research into the effect of guidelines has addressed their effect on clinician actions but not much at all on patient outcome. Research has shown that after intensive training, therapists acted to a significantly greater degree according to the LBP guidelines but that patient outcome was not better as compared to the control group33. Currently, research showing superior efficacy of guideline-driven therapy is at best limited.
Electronic Health Records
Of course, as clinicians, we have an interest in monitoring patient progress during and after treatment. Currently, however, patient monitoring in the clinical MPT situation is not systematic or repeated. Outcome measures are collected but the type of data collected is inconsistent and often non-quantitative. The lack of normative data does not allow for comparison of the individual patient with a relevant normal population. Since 2001 in the Netherlands, data on physical therapy and MPT have been collected, analyzed, and interpreted nationwide by the Dutch Institute for Primary Care34, but in this context we should also mention the Web-Based-Medical-Electronic-Dossier (WEBMED) of the Centre for Evidence Based Physiotherapy (CEBP) of the University of Maastricht and the patient tracking system of the Programme Quality Indicators Physical Therapy of the Quality of Care Research Department of the Radboud University Nijmegen Medical Centre. However, a recent study on clinical databases available in various countries showed a paucity of clinical data, thereby not allowing for international comparisons on patient characteristics, diagnosis, and management35. I expect data collection in the form of an electronic health record to be a greater priority in the years to come, but I also acknowledge the need for a change in attitude within MPT with regard to the need for systematic documentation36.
Quality Indicators
The need for quality improvement in health care becomes evident with national and international studies showing that 30–50% of patients are not receiving care based on current best evidence. Quality indicators include process indicators (providing information on the care process), structure indicators (discussing organization and conditions for care), and outcome indicators (providing information on the outcomes of care provided). Quality indicators are new to the field of MPT where quality improvement had historically been based on self-regulation. This self-regulation has provided improvements in care but has not contributed to sufficient transparency of care delivered, this in a time when external pressures (government, third-party payers) are increasingly requiring justification of care based on valid quality indicators. In the Netherlands, this has led to the development of process and outcome indicators based on the existing clinical practice guidelines for the diagnosis and management of LBP33, hip and knee DJD37, whiplash syndrome38, and ankle injuries39. Although this has increased transparency of care to external parties, a documented adherence of 60% to guidelines clearly indicates that there is room for improvement. Of course, we need to acknowledge the ongoing discussion of the effect of public reporting of quality indicators; there is as yet little scientific evidence for the effect of reporting on the actual quality of care provided40,41.
I realize that solely identifying problems is only the first step in addressing the issues discussed above that plague the implementation of evidence-based practice within the field of MPT. The remainder of this editorial is, therefore, devoted to my suggested solutions to these problems.
Use of the “Inverse Evidence Pyramid”
As I have indicated above, applicability of findings in RCTs to the MPT clinical situation is often limited due to differences in patient characteristics. A further aspect limiting clinical applicability is the interactive, evolving nature of MPT intervention in the clinical situation as compared to the rigidly standardized intervention studied in an RCT. The question we need to ask at this point is not just whether the research done is of high methodological quality but also if it is in fact the correct type of research. On the occasion of accepting an honorary doctorate from the University of Amsterdam in 2006 one of the pioneers of systematic reviews, Sir Iain Chalmers asked why researchers do not answer clinical questions. He indicated that we have a great amount of evidence of sufficiently high methodological quality that is often irrelevant to physicians and their patients. In my opinion, the same applies to MPT. Research should answer the questions emanating from clinical practice. Although many still consider the RCT the gold standard for outcomes research, we need to understand that other study designs including cohort studies are excellent tools for generating clinically relevant information. We also discussed above how systematic reviews of the many RCTs performed within MPT have provided very limited research support for MPT. Despite a successful emphasis on improving the methodological quality of RCTs in MPT, fundamental questions as to who, what, when, why, and how remain unanswered. I suggest redirecting our research agenda to more clinically relevant research, including study designs other than the RCT, and including fundamental theory-based research to provide better understanding in the underlying mechanisms of our interventions.
One example of the above-mentioned fundamental research is how altered insights into the physiology and psychology of chronic pain should shift the research emphasis with regard to chronic pain management. Research in patients with lumbosacral radiculopathy42, shoulder pain43, and pelvic pain44 has shown no between-group differences in pain-related fear between graded activity and usual care groups. The new insights into the basic science underlying chronic pain imply that we should instead be comparing graded exposure to activities associated with pain-related fear to this current standard protocol of graded physical activity.
The question as to which study designs to use is less straightforward and is determined by the large variations in the extent to which portions of MPT clinical practice have been studied to date. One might be inclined to shoot for the highest level of evidence within the evidence pyramid and use an RCT design, but we have to realize that a large part of current medical knowledge was not derived by way of an RCT. Etiologic and prognostic questions cannot be answered by an RCT; it is unethical to expose subjects to potential pathogens or suspected adverse prognostic factors leaving only observational designs for these types of questions. The N=1-trial and also less methodologically rigorous case reports and case series are clinic-friendly designs that help construct our evidence pyramid. I have enjoyed reading the recent examples of this type of design published in JMMT45,46.
My suggestion is to critically evaluate the evidence pyramid for different areas of MPT. For every area of MPT, this should result in innovative research varying from case reports and case studies for one portion of the field, to cohort studies and even RCTs for another. For patients with DJD of the hip, for example, RCTs into efficacy and efficiency of MPT and systematic reviews of such trials seem indicated, because we have sufficient information on etiology, underlying mechanisms, diagnosis, and prognosis10. In less studied areas of MPT, I recommend not starting at the top of the evidence pyramid as has occurred with disappointing results in the past for some areas within MPT but rather that we systematically build our evidence pyramid starting with designs relevant to the current state of the research base.
Functional Outcome Measures
A large number of diagnostic tests and outcome measures have been developed and studied for reliability and validity. A current research emphasis is in the area of responsiveness of said tests and measures. However, with so many tests available, frequently the MPT clinician is at a loss as to which test or measure to use. Historically, MPT has concentrated on treating impairments. However, to the patient, the treatment goal of improving segmental spinal mobility is less relevant than a higher-level goal such as improving independent standing and walking. This requires that the clinician be able to measure not only at the impairment-level but also at the level of activity and participation. As a stand-alone intervention, MPT is less effective than MPT combined with exercise therapy, especially functional exercise therapy, i.e., at the level of activities and participation. With unique patient presentations and also with unique patient learning styles, standardized exercise programs are an impossibility requiring not only inventiveness and knowledge of motor learning from the MPT clinician but also functional outcome measures. These measures do not just consist of questionnaires quantifying functional tasks but should also include quantifiable movement tests specific to the patient and his unique environment.
ICF Core Sets
When assessing the literature, it becomes evident that different studies on similar populations have used a great variety of outcome measures. A good example of this is provided by research on patients with rheumatic conditions where aspects of pain have been measured with 40 different outcome measures22. This makes it impossible to statistically pool outcomes of multiple studies as would occur in a meta-analysis. In essence, every RCT then has its own unique outcome.
In addition to the great number of outcome measures used, one cannot help but notice their similarity in that most measures provide data at the level of impairments with only a few instruments measuring activities and participation. In contrast, there is an increasing clinical emphasis on defining treatment goals at these higher levels. Currently, there are no core sets of groups of tests and measures that provide information on all domains of human functioning. This again makes it difficult to compare RCTs and interpret their findings to MPT clinical practice. Based on ICF terminology, Stucki et al are coordinating international projects that, by way of Delphi analysis, are developing core sets of impairments, limitations in activities, and restrictions in participation for various patient groups47 including LBP48 and RA49. The next step is to select tests and measures with adequate psychometric properties that reflect these core sets: Sigl et al50 have done preliminary work on this for patients with LBP.
Clinical Prediction Rules
The development of clinical prediction rules that attempt to identify which patients have the greatest chance of success with a specific intervention is and will be a major breakthrough in research with regard to the identification of homogenous subpopulations in the larger group of patients with non-specific neck and LBP51–53. However, the validity of these clinical prediction rules is still a topic of discussion within the MPT community.
MPT: Standardization or Description?
Within MPT, there are a multitude of interventions. Heerkens et al54 described these techniques and identified some 10 variables including direction, amplitude, velocity, and force. International efforts to standardize the nomenclature of MPT interventions have been unsuccessful. Often descriptions in research are limited to mobilization or manipulation with some additional information with regard to amplitude and velocity. Hurley et al55 reviewed the description of MPT techniques in the scientific literature and indicated that the techniques studied are often identified with the name of their main proponent, such as Maitland techniques with the degree and direction of the technique.
Knowledge synthesis provides little information especially with regard to the rationale for choice and dosage of the MPT techniques studied. It is nearly impossible to comprehensively describe variations in MPT technique variables in any clinical visit, let alone in a research study involving a great number of subjects. The choice of technique variables (and technique) is made clinically in a cooperative manner with the patient, taking into account not only the best available evidence but also patient preference56. This greatly hampers the standardization of MPT techniques in a research setting and is in stark contrast to the much greater level of standardization that can be attained in pharmacological research. Instead, I suggest that any study on MPT include a description of the algorithm for choice of the specific MPT intervention without an overemphasis on standardization or technique description. Various attempts have been made to reach consensus on such algorithms, but an international consensus is lacking as of yet.
Conclusion
Above, I have discussed issues within MPT that are of concern to me but also some suggestions as to possible solutions. I would like to stress again that as a profession we need to continue to increase the research base at the basis of MPT not just with regard to interventions but also with regard to diagnosis. The emphasis needs to be placed on patient-based evidence that links individual patient characteristics to characteristics derived at the group level; one way to achieve this is to continue on the avenue of developing clinical prediction rules.
We need to think of an inverse evidence pyramid, by which I do not mean we have to value lower-level evidence over higher-level evidence but rather that we need to use study designs other than RCTs where appropriate, such as longitudinal non-experimental designs and fundamental theory-based research. The value of the case report and the case study as the basis for development of the field should not be underestimated. I agree wholeheartedly with Vandenbroucke57 in that innovation often requires that the hierarchy of evidence be turned upside-down, hence the mention of the “inverse” pyramid. Research also should not be limited to quantitative studies alone: The development of an internationally accepted nomenclature of MPT interventions, the development of ICF core sets, functional outcome measures, clinical practice guidelines, electronic health records and associated databanks, and quality of care indicators requires qualitative study designs as well.
I see the MPT clinician with scientific training as the most appropriate researcher in the field of MPT. Presently, many such colleagues have stepped up to the plate and are doing the clinical research or are on the track to doctoral degrees. Research projects also need the active cooperation of therapists involved in MPT clinical practice. The first generation of MPT researchers, of which I am one, is retiring. I feel confident that a new generation is ready to take over our work in continuing to build the evidence pyramid. It would seem that-in analogy to the great Egyptian pyramids-we should think in terms of generations rather than years when it comes to building the required evidence pyramid at the base of MPT clinical practice.
REFERENCES
- 1.Oostendorp RAB. Functionele Vertebrobasilaire Insuffciëntie: Diagnostiek en Behandeling in de Fysiotherapie en Manuele Therapie. Doctoral Thesis. Nijmegen, the Netherlands: Radboud University Nijmegen; 1988. [Google Scholar]
- 2.Clarke JA, Van Tulder MW, Blomberg, SEI, De Vet HCW, Van der Heijden GJMG, Bronfort G, Bouter L. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev 2007(2). Art. No.: CD003010. DOI: 10.1002/14651858.CD003010.pub4. [DOI] [PubMed]
- 3.Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. Cochrane Database Syst Rev. 2004;(1):CD000447. doi: 10.1002/14651858.CD000447.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Gross AR, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, Bronfort G. Cervical overview group: Manipulation and mobilisation for mechanical neck disorders. Cochrane Database Syst Rev 2004(1). Art. No.: CD004249. DOI: 10.1002/14651858.CD004249.pub2. [DOI] [PubMed]
- 5.Koes B.W. How to evaluate manual therapy: Value and pitfalls of randomized clinical trials. Man Ther. 2004;9:183–184. doi: 10.1016/j.math.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Verhagen AP, De Vet HC, De Bie RA, Kessels AG, Boers M, Bouter LM, Knipschild PG. The art of quality assessment of RCTs included in systematic reviews. J Clin Epidemiol. 2001;54:651–654. doi: 10.1016/s0895-4356(00)00360-7. [DOI] [PubMed] [Google Scholar]
- 7.Cochrane Methodology Review Group. About The Cochrane Collaboration (Cochrane Review Groups, CRGs) 2005(2). Art. No.: METHOD.
- 8.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;8:713–721. [PubMed] [Google Scholar]
- 9.Oostendorp RAB, Scholten-Peeters GGM, Swinkels RAHM, Heijmans MWFGJ, Huijbregts PA, Hendriks HJM. Evidence-based practice in physical and manual therapy: Development and content of Dutch national clinical guidelines for patients with non-specific low back pain. J Manual Manipulative Ther. 2004;12:21–31. [Google Scholar]
- 10.Veenhof C. The Effectiveness of Behavioral Graded Activity in Patients with Osteoarthritis of Hip and Knee. Doctoral Thesis. Amsterdam, the Netherlands: Vrije Universiteit Amsterdam; 2006. [Google Scholar]
- 11.Veenhof C, Köke AJ, Dekker J, Oostendorp RA, Bijlsma JW, Van Tulder MW, Van Ende CH. Effectiveness of behavioral graded activity in patients with osteoarthritis of the hip and/or knee: A randomized clinical trial. Arthritis Rheum. 2006;55:925–934. doi: 10.1002/art.22341. [DOI] [PubMed] [Google Scholar]
- 12.Hendriks EJ, Scholten-Peeters GG, Van der Windt DA, Neeleman-van der Steen CW, Oostendorp RAB, Verhagen AP. Prognostic factors for poor recovery in acute whiplash patients. Pain. 2005;114:408–416. doi: 10.1016/j.pain.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Swinkels-Meewisse IE, Roelofs J, Schouten EG, Verbeek AL, Oostendorp RAB, Vlaeyen JW. Fear of movement/(re)injury predicting chronic disabling low back pain: A prospective inception cohort study. Spine. 2006;31:658–664. doi: 10.1097/01.brs.0000203709.65384.9d. [DOI] [PubMed] [Google Scholar]
- 14.Den Boer JJ, Oostendorp RAB, Beems T, Munneke M, Evers AWM. Continued disability and pain after lumbar disc surgery: The role of cognitive-behavioral factors. Pain. 2006;123:45–52. doi: 10.1016/j.pain.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Den Boer JJ, Oostendorp RAB, Beems T, Munneke M, Evers AWM. Reduced work capacity after lumbar disc surgery: The role of cognitive-behavioral and work-related risk factors. Pain. 2006;123:72–78. doi: 10.1016/j.pain.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Johansson AC, Cornefjord M, Bergkvist L, Ohrvik J, Linton SJ. Psychosocial stress factors among patients with lumbar disc herniation, scheduled for disc surgery in comparison with patients scheduled for arthroscopic knee surgery. Eur Spine J. 2007;16:961–970. doi: 10.1007/s00586-007-0319-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henschkel N, Maher CG, Refshauge KM, Das A, McAuley JM. Low back pain research priorities: A survey of primary care practitioners. BMC Family Practice 2007;8:40 DOI:10.1186/1471–2296–8–40. [DOI] [PMC free article] [PubMed]
- 18.Van Trijffel E, Anderegg Q, Bossuyt PMM, Lucas C. Inter-examiner reliability of passive assessment of intervertebral motion in the cervical and lumbar spine: A systematic review. Man Ther. 2005;10:256–269. doi: 10.1016/j.math.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev 2003(2). Art. No.: CD004258. DOI: 10.1002/14651858.CD004258. [DOI] [PMC free article] [PubMed]
- 20.Bot SDM, Terwee CB, Van der Windt DAWM, Bouter LM, Dekker J, De Vet HCW. Clinimetric evaluation of shoulder disability questionnaires: A systematic review of the literature. Ann Rheum Dis. 2004;63:335–341. doi: 10.1136/ard.2003.007724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization International Classification of Functioning, Disability and Health. Geneva, Switzerland: Author; 2001. [Google Scholar]
- 22.Swinkels RA, Bouter LM, Oostendorp RAB, Van den Ende CHM. Impairment measures in rheumatic disorders for rehabilitation medicine and allied health care: A systematic review. Rheumatol Int. 2005;24:501–512. doi: 10.1007/s00296-005-0603-0. [DOI] [PubMed] [Google Scholar]
- 23.Butler CC, Evans M, Greaves D, Simpson S. Medically unexplained symptoms: The biopsychosocial model found wanting. J Royal Soc Med. 2004;97:219–222. doi: 10.1258/jrsm.97.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones M, Edwards I, Gifford L. Conceptual models for implementing biopsychosocial theory in clinical practice. Man Ther. 2007;7:2–9. doi: 10.1054/math.2001.0426. [DOI] [PubMed] [Google Scholar]
- 25.Bernards ATM, Hagenaars LHA, Oostendorp RAB. Het meerdimensionale belasting-belastbaarheidsmodel: Een conceptueel model voor de fysiotherapie. Ned Tijdschr Fysiother. 1999;109:58–65. [Google Scholar]
- 26.Hagenaars LHA, Bernards ATM, Oostendorp RAB. Het Meerdimensionaal Belasting-Belastbaarheidsmodel. Amersfoort, the Netherlands: Nederlands Paramedisch Instituut; 2000. [Google Scholar]
- 27.Landers MR, Creger RV, Baker CV, Stutelberg KS. The use of fear-avoidance beliefs and nonorganic signs in predicting prolonged disability in patients with neck pain. Man Ther (in press). [DOI] [PubMed]
- 28.Kent PM, Keating JL. Can we predict poor recovery from recent-onset nonspecific low back pain? A systematic review. Man Ther (in press). [DOI] [PubMed]
- 29.Ernst E, Canter PH. A systematic review of systematic reviews of spinal manipulation. J Royal Soc Med. 2006;99:192–196. doi: 10.1258/jrsm.99.4.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luijsterburg PAJ, Verhagen AP, Ostelo RWJG, Van Os TAG, Peul WC, Koes BW. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: A systematic review. Eur Spine J. 2007;16:881–899. doi: 10.1007/s00586-007-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smidt N, De Vet HC, Bouter LM, et al. Effectiveness of exercise therapy: A best-evidence summary of systematic reviews. Aust J Physiother. 2005;51:71–85. doi: 10.1016/s0004-9514(05)70036-2. [DOI] [PubMed] [Google Scholar]
- 32.Moore A, Jull G. The systematic review of systematic reviews has arrived! Man Ther. 2006;11:91–92. doi: 10.1016/j.math.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Bekkering GE, Van Tulder MW, Hendriks EJ, Koopmanschap MA, Knol DL, Bouter LM, Oostendorp RAB. Implementation of clinical guidelines on physical therapy for patients with low back pain: Randomized trial comparing patient outcomes after a standard and active implementation strategy. Phys Ther. 2005;85:544–555. [PubMed] [Google Scholar]
- 34.NIVEL Jaarboek LiPZ Fysiotherapie 2006. Utrecht, the Netherlands: Author; 2006. [Google Scholar]
- 35.Swinkels ICS, Van den Ende CHM, De Bakker D, et al. Clinical databases in physical therapy. Physiother Theory Pract. 2007;23:153–167. doi: 10.1080/09593980701209097. [DOI] [PubMed] [Google Scholar]
- 36.Vreeman DJ, Taggard SL, Rhine MD, Worrell TW. Evidence for electronic health records systems in physical therapy. Phys Ther. 2006;86:434–446. [PubMed] [Google Scholar]
- 37.Jansen MJ, Hendriks HJM, De Bie RA, Dekker J, Oostendorp RAB. Handelen volgens de KNGF-richtlijn Artrose heup-knie: Een prospectieve cohortstudie. Ned Tijdschr Fysiother. 2005;115:68–73. [Google Scholar]
- 38.Scholten-Peeters GGM, Neeleman-van der Steen CW, Van der Windt DA, Hendriks EJ, Verhagen AP, Oostendorp RAB. Education by general practitioners or education and exercises by physiotherapists for patients with whiplash-associated disorders? A randomized clinical trial. Spine. 2006;31:723–731. doi: 10.1097/01.brs.0000206381.15224.0f. [DOI] [PubMed] [Google Scholar]
- 39.Van der Wees PJ, Hendriks EJ, Jansen MJ, Van Beers H, De Bie RA, Dekker J. Adherence to physiotherapy clinical guideline acute ankle injury and determinants of adherence: A cohort study. BMC Musculoskel Disord. 2007:22. doi: 10.1186/1471-2474-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marshall MN, Brook RH. Public reporting of comparative information about quality of healthcare. Med J Aust. 2002;176:205–206. doi: 10.5694/j.1326-5377.2002.tb04373.x. [DOI] [PubMed] [Google Scholar]
- 41.Werner RM, Asch DA. The unintended consequences of public reporting quality information. JAMA. 2005;293:1239–1244. doi: 10.1001/jama.293.10.1239. [DOI] [PubMed] [Google Scholar]
- 42.Ostelo RW, De Vet HC, Vlaeyen JW, et al. Behavioral graded activity following first-time lumbar disc surgery: 1–year results of a randomized clinical trial. Spine. 2003;28:1757–1765. doi: 10.1097/01.brs.0000083317.62258.e6. [DOI] [PubMed] [Google Scholar]
- 43.Geraets JJ, Gossens ME, De Groot IJ, et al. Effectiveness of a graded exercise therapy program for patients with chronic shoulder complaints. Aust J Physiother. 2005;51:87–94. doi: 10.1016/s0004-9514(05)70037-4. [DOI] [PubMed] [Google Scholar]
- 44.Bastiaenen CH, De Bie RA, Wolters PM, et al. Effectiveness of a tailor-made intervention for pregnancy-related pelvic girdle and/or low back pain after delivery: Short-term results of a randomized clinical trial. BMC Musculoskel Disord. 2006;7:19. doi: 10.1186/1471-2474-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Issa TS, Hijbregts PA. Physical therapy diagnosis and management of a patient with chronic daily headache: A case report. J Manual Manipulative Ther. 2006;14:E88–E123. [Google Scholar]
- 46.Pinto D, Cleland J, Palmer J, Eberhart SL. Management of low back pain: A case series illustrating the pragmatic combination of treatment- and mechanism-based classification systems. J Manual Manipulative Ther. 2007;15:111–122. doi: 10.1179/106698107790819891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Finger ME, Cieza A, Stoll J, Stucki G, Huber EO. Identification of intervention categories for physical therapy, based on the International Classification of Functioning, Disability and Health: A Delphi exercise. Phys Ther. 2006;86:1203–1220. doi: 10.2522/ptj.20050134. [DOI] [PubMed] [Google Scholar]
- 48.Cieza A, Stucki G, Weigl M, et al. ICF Core sets for low back pain. J Rehabil Med. 2004;36(44S):69–76. doi: 10.1080/16501960410016037. [DOI] [PubMed] [Google Scholar]
- 49.Stucki G, Cieza A, Geyh S, et al. ICF Core sets for rheumatoid arthritis. J Rehabil Med. 2004;36(44S):87–93. doi: 10.1080/16501960410015470. [DOI] [PubMed] [Google Scholar]
- 50.Sigl T, Cieza A, Borckow T, Chatterji S, Kostanjsek N, Stucki G. Content comparison of low back pain-specific measures based on the International Classification of Functioning, Disability and Health (ICF) Clin J Pain. 2006;22:147–153. doi: 10.1097/01.ajp.0000155344.22064.f4. [DOI] [PubMed] [Google Scholar]
- 51.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: Use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 52.Childs JD, Cleland JA. Development and application of clinical prediction rules to improve decision making in physical therapist practice. Phys Ther. 2006;86:122–131. doi: 10.1093/ptj/86.1.122. [DOI] [PubMed] [Google Scholar]
- 53.Beattie P, Nelson R. Clinical prediction rules: What are they and what do they tell us? Aust J Physiother. 2006;52:157–163. doi: 10.1016/s0004-9514(06)70024-1. [DOI] [PubMed] [Google Scholar]
- 54.Heerkens YF, Van den Heuvel J, Van Klaveren AJJ. Classificatie Verrichtingen Paramedische Beroepen. Amersfoort. the Netherlands: Nederlands Paramedisch Instituut; 1995. [Google Scholar]
- 55.Hurley DA, McDonough SM, Baxter GD, Dempster D, Moore AP. A descriptive study of the usage of spinal manipulative therapy techniques within a randomized clinical trial in acute low back pain. Man Ther. 2005;10:61–67. doi: 10.1016/j.math.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 56.Freburger JK, Carey TS, Holmes GM. Management of back and neck pain: Who seeks care from physical therapists? Phys Ther. 2005;85:872–886. [PubMed] [Google Scholar]
- 57.Vandenbroucke JP. De N=1-trial, de meest ideale onderzoeksopzet die te weinig wordt gebruikt. Ned Tijdschr Geneesk. 2006;150:2794–2795. [PubMed] [Google Scholar]


