Abstract
Cervicogenic headache (CGH) is a common sequela of upper cervical dysfunction with a significant impact on patients. Diagnosis and treatment have been well validated; however, few studies have described characteristics of patients that are associated with outcomes of physical therapy treatment of this disorder. A retrospective chart review of patient data was performed on a cohort of 44 patients with CGH. Patients had undergone a standardized physical therapy treatment approach that included spinal mobilization/manipulation and therapeutic exercise, and outcomes of treatment were determined by quantification of changes in headache pain intensity, headache frequency, and self-reported function. Multiple regression analysis was utilized to determine the relationship between a variety of patient-specific variables and these outcome measures. Increased patient age, provocation or relief of headache with movement, and being gainfully employed were all patient factors that were found to be significantly (P<0.05) related to improved outcomes.
Key Words: Cervicogenic Headache, Physical Therapy, Treatment Characteristics, Manual Therapy
Although cervicogenic headache (CGH) has been described as a “final common pathway” of cervical spine dysfunction1, its true prevalence is difficult to determine due to inconsistent use of diagnostic criteria in the literature. Incidence of cervicogenic headache has been reported to range from 0.7% to as high as 13.8% in populations of patients suffering from headache disorders2. Others have reported cervicogenic origins of higher values (14% to 18%) in all chronic headaches3.
gThe anatomical basis for CGH is the convergence of the afferent input of the upper cervical spine nerve roots (C1-C3) with the afferent tracts of the trigeminal nerve in the trigeminocervical nucleus. This convergence results in cervical spine nociceptive input being expressed in the sensory distribution of the trigeminal nerve, most commonly the ophthalmic branch of the trigeminal nerve, which innervates the forehead, temple, and orbit and has its greatest topographic representation near the dorsal horns of spinal nerves C1-C34,5. Therefore, any structure innervated by C1, C2, or C3 spinal nerves can be implicated in the etiology of CGH. This includes the atlanto-occipital, median atlanto-axial, lateral atlanto-axial, and C2-3 zygapophyseal joints as well as the C2-3 intervertebral disc, suboccipital, upper posterior cervical, and upper paravertebral musculature, the trapezius and sternocleidomastoid muscles, upper cervical spinal dura mater, and the vertebral arteries4–6. Because of the ability of afferent nerves to travel up to three segments cephalically or caudally in the cervical spinal cord, bony and soft tissue structures of the middle and lower cervical spine cannot be excluded from contributing to CGH4,5.
The diagnosis of CGH has been a source of contention in the literature ever since the inception of the term by Sjaastad et al in 19837-9. Currently, two major sets of diagnostic criteria exist for CGH (Table 1). The International Headache Society (IHS) accepted the diagnosis of CGH in 1988 as a type of secondary headache and, at that time, included criteria for its diagnosis in the International Classification of Headache Disorders, which was most recently updated in 200410. However, the criteria established in 1990 by Sjaastad and the Cervicogenic Headache International Study Group (CHISG) and revised in 19981 are the most utilized clinically. The exception of the clinical utility of Sjaastad's criteria is Point II, which stipulates the use of a nerve block to diagnose CGH in scientific works. The use of a nerve block may be impractical for daily clinical practice, despite being the only means by which a structure in the cervical spine can truly be isolated as the pain generator5,11,12. Furthermore, although Point III of Sjaastad's criteria specifies unilaterality of symptoms, the presence of bilateral symptoms or “unilaterality on two sides” has been documented1,13. Differential diagnosis includes hemicrania continua, occipital neuralgia, migraine, and tension-type headache, with the differentiation of CGH from migraine and tension-type headache being the most challenging due to the overlap of many symptoms among these three disorders2,14.
TABLE 1.
Diagnostic criteria for cervicogenic headache
| CHISG Diagnostic Criteria (1) | IHS Diagnostic Criteria (10) |
|---|---|
|
|
| For a diagnosis of CGH to be appropriate, one or more aspects of Point I must be present, with Ia sufficient to serve as a sole criterion for positivity or Ib and Ic combined. For scientific work, Point II is obligatory, while Point III is preferably obligatory. | The presence of all four of these criteria is an indication that a diagnosis of CGH is appropriate. |
The reliability and validity of physical therapist diagnosis of CGH, specifically during manual cervical spine examination and evaluation that is necessitated by both sets of diagnostic criteria, have been well established11–13,15. Additionally, various physical therapy interventions including spinal manipulation or mobilization, therapeutic exercise, postural modification, or a combination of treatments have been validated in numerous reports as effective treatments of CGH12,16–18. In particular, several studies have found improved outcomes after combined spinal manipulation and therapeutic exercise treatment over either treatment alone for patients with mechanical neck dysfunction19 and for patients specifically with CGH17. However, when using spinal mobilization or manipulation patients with CGH, it becomes especially important to perform the appropriate pre-treatment screening procedures, particularly since headaches can be a symptom of disorders that contraindicate the use of these techniques such as vertebrobasilar insufficiency20.
In addition to the physical impairments of 1) increased pain, 2) decreased cervical range of motion21, 3) postural dysfunction22, and 4) decreased performance of deep cervical flexors22–24, symptoms of CGH have a demonstrable impact on patients' functioning and overall quality of life25. Although impairments associated with CGH are well documented, there remains a lack of evidence as to how impairments influence the outcome during physical therapy treatment. There are also few studies demonstrating if patient traits or characteristics positively or negatively affect treatment outcomes in physical therapy, although it has been reported that patients' individual experiences of cervical dysfunction play an important role in the prognosis of the condition26. Most published studies suggest inconsistency of predictors of positive outcomes of treatment of CGH17,27. Subsequently, the purpose of this study was to continue to examine various factors that are associated with improved overall function, decreased headache frequency, and decreased headache intensity after a consistent physical therapy intervention for CGH.
Methods and Materials
Design
The study involves a retrospective cohort chart review involving a population of patients with CGH. The study was performed under appropriate human ethics and institutional board approval of Ellis Hospital, Schenectady, New York, USA. The study received exempt status from the institutional review board.
Participants
The primary author of the paper reviewed consecutive charts of patients diagnosed with CGH seen for physical therapy from January 2003 through February 2006. Patients in this study were diagnosed clinically with CGH using both the CHISG and the IHS criteria (Table 1). Exclusion criteria for treatment included any contraindications to manual/manipulative therapy and/or exercise and a positive vertebrobasilar insufficiency test (VBI). All patients were cleared subjectively for any indication of VBI, and formal testing was performed, regardless of manual intervention.
Procedure
Charts were selected for review by performing a search of the primary author's computerized patient database by querying the diagnosis of headache (Figure 1). Additionally, the database was searched by referral source; the names of a neurologist and a neurological physician assistant were queried, as these persons were primary referral sources from a comprehensive headache treatment center located nearby the primary author's clinic. Charts were included if missing values were few, allowing extraction and transformation to a dataset. Charts were considered if the primary data of at least two sets (initial and discharge) of functional outcome data, headache frequency data, headache pain scores, and headache-duration data were present. Charts were excluded from the study if information regarding the second set of function and headache-specific outcome data was missing. Additionally, data regarding motor control, joint signs, history of neck pain/injury, and other relevant demographics were reported.
Figure 1.
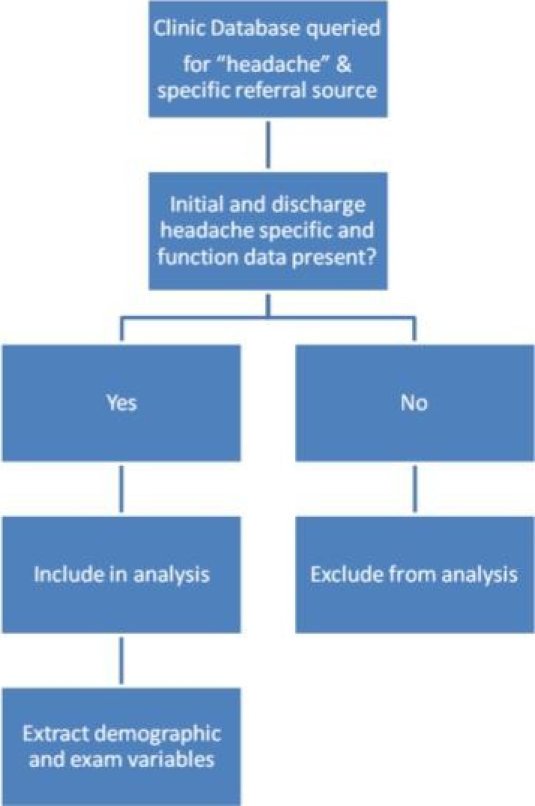
Flow Diagram of Chart Selection
Physical Therapy Patient History
Chart review data were extracted including standard questions regarding primary complaints, onset, and the overall history of the complaint. Additionally, because all patients had completed a medical screening questionnaire, including medications, this information was extracted and documented for each patient. Demographics such as age, work history, and gender were also reviewed. Report of 1) history of neck and/or head injury/trauma, 2) average number of headaches in 1 week, 3) historical duration of headache problem, 4) location of headache and/or neck pain, 5) specific aggravating and easing factors, 6) screening for any variables related to vertebral artery or cord compromise, 7) history of any dental or TMJ problems, and 8) headache pain (and neck pain if present) using a Numeric Pain Rating Scale (0-10) were collected. Because the same clinician originally examined all patients, consistent data were collected prospectively during patient care.
Physical Therapy Physical Examination
Report of findings from the physical examination was collected with a focus on identifying relevant physical impairments. Originally, the examination placed an emphasis on establishing physical impairments related to concordant signs. Data regarding 1) observation/postural faults; 2) active range of motion of the shoulders; 3) active range of motion of the cervical spine including retraction and overpressures as required; 4) supine palpation of the neck, upper back, and head; 5) passive physiological intervertebral movements (PPIVMS) of the cervical spine, including combined movements of the upper cervical spine; 6) assessment of relevant muscle length with particular focus on the scalene and levator scapulae; 7) palpation of soft tissues of the cervical and upper thoracic regions in prone; and 8) prone passive accessory intervertebral movements (PAIVMs), both central and unilateral of the cervical and upper thoracic regions, with particular emphasis on the upper three segments of the cervical spine11,17,28–30. Report of differentiation of C1-C3 was collected because of the propensity of mechanical dysfunction at these areas resulting in headache symptoms4,5,31.
Data regarding neurodynamics was examined only if the patient presented with more regionalized pain or radiating pain toward/into the upper extremity and/or scapular regions32,33. Information associated with motor control was collected generally from data of Visit 2 or 3, by recording neck flexor endurance measurements in neutral and inner range, along with examination of the cranio-cervical flexor synergy utilizing the Stabilizer (Stabilizer™, Chattanooga Group Inc., Chattanooga, TN). Data regarding the strength of the lower trapezius and serratus anterior were also assessed17.
Interventions
Data regarding interventions were based on determining relevant physical impairments found in the physical examination. Priority was placed on those impairments that were found to be related to the concordant signs and symptoms. An example of this would include a physical examination finding such as a unilateral passive-accessory posterior to anterior pressure to C2 reproducing the patient's headache. Treatment interventions were manual therapy and therapeutic exercise-based and frequently included passive accessory and/or passive physiologic movements of the cervical spine, with the purpose of reducing abnormal (concordant) symptoms and movement relevant to the patient's headache. Additionally, data regarding therapeutic exercises were based on identified impairments in active control of selected movements and related muscle groups. A typical intervention of active control training included methods designed to improve the recruitment and fatigability of the deep neck flexors of the cervical spine. Information involving a home exercise program that addressed the general mobility of the cervical spine region and control of selected active movements such as peri-scapular muscles or deep neck flexors was also recorded17,28.
Outcome Measures
All patient charts included a standard demographic and medical screening questionnaire. The data contained the Therapeutic Associates Outcomes System (TAOS)34 (now, the CareConnections Outcomes System), a comprehensive scale that is frequently used in the clinic where these patients received treatment and which provides clinicians access to a national database of outcomes information. The TAOS asked all patients to rate their perceived impairment in categories that included five descriptors of varying levels of impairment within a category, with 10 categories. Each category was scored using a 0-5 rating scale, 0 representing the most impairment within a category and 5 representing no impairment in that category. A total score was obtained by adding the scores of the 10 categories, then multiplying by two. Total scores ranged from 0-100, with 100 representing no functional impairment. This functional scale includes three questions that are related to a patient with headache: reading, headache frequency (based on a general pain level descriptor, e.g., “moderate”), and concentration. Examples of other categories include walking, personal care, lifting, driving, and recreation. This measure has not been validated in any specific patient populations; analysis of content validity and discriminate analysis were found to be adequate. This scale is modeled after the Oswestry Low Back Pain Disability Questionnaire and the Neck Disability Index34. The TAOS does contain questions specific to the cervical spine and headache and was utilized based on ease of access and clinician familiarity with standard use of the scale in clinical practice.
All charts selected included the primary outcomes measures of change in overall function using the TAOS as described above, headache intensity, and changes in headache frequency. Decrease in headache intensity was a clinically relevant indicator of positive outcome in this study, and it was measured using the Numeric Pain Rating Scale (NPRS), where the patient rates his/her pain from 0 to 10. This pain rating scale has been shown to be reliable and valid in a number of populations35,36. Although we are unaware of a study that has examined the NPRS solely in patients with cervical dysfunction or CGH, the measure has been validated as an outcomes measure for patients with chronic musculoskeletal pain37 and patients with other spine disorders38, and a change of two points on the NPRS has been found to be the minimal clinically important difference (MCID) in these populations39,40. Headache frequency was measured by the number of headache days in the past week, with a maximum of 28 headache days per month. According to the IHS guidelines, a reduction of 50% frequency is considered a clinically significant reduction27,39.
Statistical Analysis
All statistical analyses were performed using SPSS version 12.0. (Chicago, IL). Variables that were chosen for the analysis included demographic data as well as common examination procedures used in the examination of patients with complaints of CGH. Univariate statistics outlined the baseline characteristics of the cohort. Variables for report of function included rating of overall function from 0-100 per the TAOS, frequency of headache, and intensity of headache per the NPRS. Bivariate analysis and effect size scores were obtained for headache intensity, frequency, and function scores. Effect sizes were calculated by taking the difference between the mean and standard deviation changes in the primary outcome of headache frequency in the baseline and discharge groups, and dividing it by the standard deviation of the change score in the total population. An effect size of 0.2 was regarded as small, 0.5 as medium, and 0.8 as large40. Hierarchical multivariate statistics were used to outline which variables were associated with the change scores of frequency and intensity of function. Three linear regression analyses were performed, examining the change scores associated with report of function, frequency of report of headache, and report of intensity of headache. Significance was set at P<0.05.
Results
Initially, 62 charts were reviewed for inclusion, and 44 charts were included in the analysis. The majority of charts were removed from the study because information regarding the second set of function and headache-specific outcome data was missing. A number of patient charts lacked discharge data, and because the data of function and headache specific data were collected at baseline and discharge only, it was determined that the information was insufficient to remain in the retrospective analysis. Of the 44 charts included in the analysis, some were missing values. Seven charts were missing “strength” data and nine were missing “perceived improvement” data. An evaluation as to the reasons for the missing data revealed that patients with missing “strength” data revealed that the patient had presented with other physical impairments that took a clinical priority in the initial 2-3 treatment sessions so that these data were not collected within the noted time frame. As noted, the “strength” data presented in the analysis included only an assessment of the craniocervical flexor synergy as described by Jull17. The “perceived improvement” missing data appeared because the patient had not completed this section of the TAOS.
Of the remaining 44 patients from the charts retained in the review, the average age was 48.9 years (SD=20.3; range 14-71), and the majority was female (87%). The majority of participants worked full time (n=18) or were retired (n=13). The average duration of the headache was 46.3 weeks (SD=60.7) with a mean of 21.4 days per month in which the patients reported a headache. The baseline reported value for headache intensity was 7.7 (SD=1.6; range 4–10). Table 2 outlines the baseline characteristics of the study. Patients were seen for an average of 11.6 treatment sessions (range 3–25 sessions) for an average of 6.9 weeks (range 1–19 weeks).
TABLE 2.
Univariate analysis of study participants
| Item | Number | Mean/Median (SD) |
|---|---|---|
| Gender | 5 males | |
| 39 females | ||
| Age | 44 | 48.9/50.5 (20.3) |
| Employment Status | 18 = FT | |
| 2 = PT | ||
| 11 = Disabled/Unemployed | ||
| 13 = Retired | ||
| Function at Baseline | 44 | 65.7/66.0 (16.2) |
| Frequency of HA at Baseline | 44 | 21.4/24.0 (7.1) |
| Intensity of HA at Baseline | 44 | 7.7/8.0 (1.6) |
| Report of Previous Neck Problems | 23 = Yes | |
| 21 = No | ||
| Neural Provocation Testing (based on patient presentation) | 2 = Yes | |
| 4 = No | ||
| Number of Joint Signs | 44 | 4.3/4.0 (2.1) |
| HA Provoked/relieved with movement | 26 = Yes | |
| 16 = No | ||
| Duration of Symptoms | 44 | 46.3/NA (60.7) |
| Number of Total Visits | 44 | 11.6/12.0 (5.0) |
| Weeks of Total Treatment | 44 | 6.86/7.0 (3.2) |
HA = headache; FT = Full Time Employment; PT = Part Time Employment; NA = Not Available
There were significant differences in pre- and posttest scores for functional changes, changes in headache frequency, and headache intensity (P<0.0001). Effect size changes were 1.15 for the functional changes, 0.99 for changes in frequency, and 1.47 for changes in intensity. In all outcome variables, most patients demonstrated improvement from baseline. Out of 44 patients, 28 achieved a clinically significant decrease in headache frequency and 36 patients reported at least a minimally clinically significant change in headache pain intensity.
The model summary for the linear regression for change score of function was not significant (P=0.07). The R-square value for the 13 independent variables was 0.447, suggesting that the model explained 45% of the variance. Of the 13 predictor variables, only age (P=0.005) and employment (P = 0.004) were significant. The findings suggest that older patients were more inclined to report improvements in functional scores, as were individuals who were employed full time. Table 3 outlines the regression findings of functional change scores.
TABLE 3.
Regression analysis involving variables that affect change score for function
| Model | B | Std. Error | Beta | t | Significance |
|---|---|---|---|---|---|
| (Constant) | 29.09 | 25.01 | 1.16 | 0.254 | |
| Employment Status | −6.63 | 2.093 | −0.67 | −3.03 | 0.005* |
| Age | 0.32 | 0.11 | 0.53 | 2.88 | 0.007* |
| HA Provoked/Relieved with Movement | −6.43 | 3.92 | −0.26 | −1.64 | 0.111 |
| Gender | −6.51 | 6.38 | −0.17 | −1.02 | 0.316 |
| Frequency of HA at Baseline | 0.32 | 0.32 | 0.18 | 0.99 | 0.329 |
| Strength of Neck | −1.39 | 1.90 | −0.14 | −0.74 | 0.468 |
| Duration of Symptoms | 0.03 | 0.04 | 0.12 | 0.72 | 0.479 |
| Weeks of Total Treatment | −0.62 | 1.08 | −0.16 | −0.57 | 0.572 |
| Number of Joint Signs | −0.61 | 1.11 | −0.10 | −0.55 | 0.590 |
| Number of Total Visits | 0.231 | 0.71 | 0.09 | 0.33 | 0.747 |
| Neural Provocation | 0.85 | 5.15 | 0.03 | 0.17 | 0.870 |
| Intensity of HA at Baseline | −0.09 | 1.21 | −0.01 | −0.07 | 0.942 |
| History of Neck Problems | 0.02 | 4.31 | 0.00 | 0.00 | 0.997 |
Indicates significance at 0.05; HA = Headache
Table 4 outlines the multivariate analysis of changes in frequency. The model summary for the linear regression analysis of change scores for headache frequency was significant (P=0.001). The R-square value for the 13 independent variables was 0.637, and two of the 13 variables were significant. Older patients (increased age) were more inclined to report decreased headaches (P=0.001), as were patients who indicated their headaches were relieved or provoked with movement of the neck (P<0.0001).
TABLE 4.
Regression analysis involving variables that affect change score for frequency of headaches
| Model | B | Std. Error | Beta | t | Significance |
|---|---|---|---|---|---|
| (Constant) | 5.10 | 15.51 | 0.33 | 0.745 | |
| HA Provoked/Relieved with Movement | −10.81 | 2.38 | −0.55 | −4.54 | 0.000* |
| Age | 0.27 | 0.07 | 0.56 | 3.71 | 0.001* |
| Employment Status | −2.28 | 1.30 | −0.31 | −1.75 | 0.090 |
| Neural Provocation | 5.17 | 3.23 | 0.26 | 1.60 | 0.120 |
| Function at Baseline | 0.12 | 0.08 | 0.20 | 1.45 | 0.159 |
| Duration of Symptoms | −0.03 | 0.02 | −0.20 | −1.39 | 0.174 |
| Strength of Neck | −1.42 | 1.14 | −1.19 | −1.25 | 0.221 |
| Gender | −4.05 | 4.10 | −0.14 | −0.99 | 0.331 |
| Number of Total Visits | 0.37 | 0.46 | 0.20 | 0.81 | 0.424 |
| Intensity of HA at Baseline | 0.61 | 0.78 | 0.10 | 0.79 | 0.435 |
| History of Neck Problems | 1.91 | 2.70 | 0.10 | 0.71 | 0.484 |
| Weeks of Total Treatment | −0.48 | 0.69 | −0.16 | −0.70 | 0.490 |
| Number of Joint Signs | −0.29 | 0.70 | −0.06 | −0.42 | 0.681 |
Indicates significance at <0.001; HA = Headache
Lastly, the model summary for linear regression analysis of the change scores of intensity was also significant (P=0.031), and the R-square value for the 13 independent variables was 0.497. Age (P=0.004), headaches relieved or provoked with movement (P=0.003) of the neck, and employment (P=0.034) were significantly associated toward improvement in change scores of intensity. Table 5 outlines the findings associated with changes in intensity.
TABLE 5.
Regression analysis involving variables that affect change score for intensity of headaches
| Model | B | Std. Error | Beta | t | Significance |
|---|---|---|---|---|---|
| (Constant) | 12.78 | 4.25 | 3.01 | 0.005 | |
| HA Provoked/Relieved with Movement | −2.59 | 0.81 | −0.46 | −3.19 | 0.003* |
| Age | 0.08 | 0.02 | 0.57 | 3.14 | 0.004* |
| Employment Status | −0.99 | 0.46 | −0.47 | −2.22 | 0.034* |
| Strength of Neck | −0.61 | 0.39 | −0.28 | −1.58 | 0.125 |
| History of Neck Problems | −1.31 | 0.92 | −0.24 | −1.42 | 0.165 |
| Number of Joint Signs | −0.20 | 0.23 | −0.16 | −0.87 | 0.394 |
| Number of Total Visits | −0.13 | 0.15 | −0.24 | −0.85 | 0.401 |
| Function at Baseline | −0.02 | 0.03 | −0.10 | −0.59 | 0.559 |
| Weeks of Total Treatment | −0.13 | 0.23 | −0.16 | −0.59 | 0.560 |
| Neural Provocation | 0.51 | 1.09 | 0.09 | 0.46 | 0.647 |
| Gender | 0.39 | 1.38 | 0.05 | 0.28 | 0.780 |
| Duration of Symptoms | −0.00 | 0.01 | −0.03 | −0.19 | 0.847 |
| Frequency of HA at Baseline | 0.01 | 0.07 | 0.03 | 0.18 | 0.861 |
Indicates significance at 0.05; HA = Headache
Discussion
We endeavored to retrospectively examine various factors that are associated with improved overall function, decreased headache frequency, and decreased headache intensity after physical therapy intervention for CGH. Despite the wide variety of patient historical data that was examined in this study, only a few patient variables were associated with change scores after physical therapy intervention. This is despite the fact that the majority of patients met previously defined minimal clinically important differences for intensity of headache pain and frequency of headache. Our findings suggest that age, headaches that were provoked or relieved with movement, and work status during treatment were associated with positive patient outcomes.
Patients of a greater age were more likely, after physical therapy treatment, to demonstrate positive outcomes with respect to headache pain intensity and headache frequency. Among patients over the age of 50, the incidence of secondary headache, the category in which CGH falls, has been found to be more common than the incidence of primary headache41. However, most populations of patients with CGH that have been studied in the literature range in age from 18 up to 60 years of age17,42 with one study excluding patients over the age of 50 due to the range of motion lost and degenerative changes associated with increased age15. Although there is some evidence that suggests that younger patients with acute neck pain treated with spinal mobilization/manipulation have better outcomes of care than older patients43, others merely suggest that older age does not lead to negative outcomes of care of cervical spine dysfunction44 or CGH27. These results suggest that future prospective studies could not only include a sample of patients including those of older ages but also examine how patient age might influence treatment outcomes for this particular patient population.
Patients whose headaches were provoked or relieved with movement of the neck were associated with better outcomes of treatment, showing significantly decreased frequency of headache as well as significantly decreased reports of headache pain intensity. This finding is substantiated by a number of other existing studies that show manual interventions designed to increase mobility of the cervical spine, such as spinal mobilization and manipulation, are beneficial for patients with CGH17,19,45. Although the retrospective nature of this study precludes drawing a conclusion about the direct effect of patients' headache symptoms on functional outcomes after treatment, this finding does indicate that this relationship would be of interest to pursue in future research. In this way, these findings may have implications as to the use of the diagnostic criteria of CGH as not only able to indicate patients who have CGH but also to identify which patients among those with CGH would have greater benefit from physical therapy intervention1,10.
Additionally, 16 of the 44 patients were found not to have their headache provoked or relieved with movement during the initial examination. These patients were provisionally diagnosed with CGH as they did present with abnormal clinical signs of the cervical spine (i.e., reduced ROM and abnormal stiffness). These clinical signs did meet the inclusion criteria that are based on the aforementioned diagnostic criteria. These patients were treated based on these signs in an attempt to establish a relationship of these abnormal signs to the patients' complaints of headache. An analysis of these specific patient outcomes was not conducted. A future study may include the analysis of these types of presentations to establish whether abnormal cervical spine signs may temporarily be established as a CGH.
Maintaining gainful employment was significantly related to reports of reduced intensity of headaches and approached significance as being associated with reports of decreased frequency of headaches. Headache and cervical spine dysfunction have long been established as affecting quality-of-life measures and patient employment18,45–49. Headache specifically has a substantial effect on decreased productivity, being the most common cause of lost productive time at work, occurring in 5.4% of total respondents in a 2003 study and resulting in a loss of 19.6 billion dollars47. There is limited evidence on the particular effect of CGH on patients' employment status or quality of life, but the literature suggests that it has a unique psychosocial impact on quality of life compared with migraine and tension-type headache25. The results of this study suggest that future research could be directed at examining the effect of employment on patients with CGH and further establishing the distinctive set of psychosocial impairments that are found within this population.
This study has ventured to identify influential patient-specific variables that were associated with improved outcomes after physical therapy treatment of CGH with the intent of suggesting specific variables that would merit future research. Factors that influence prognosis of patients with CGH have not been widely studied. For clinicians, knowledge of patient-specific traits that could potentially affect patient treatment is important for numerous reasons. It allows clinicians to ascertain from the first treatment session whether a particular patient is likely to benefit from any treatment at all, leading to more effective patient management and clinical decision-making. Identification of factors that are implicated in patient prognosis also lead to more cost-effective treatment because it leads to earlier recognition of patients for whom particular treatments may not be appropriate. Furthermore, finding how these factors relate to outcomes of care is one of the first steps in the development of clinical prediction rules.
A recent study that offered a classification system for patients with neck pain named headache reduction as a specific subgroup of patients with neck pain45. The classification system dictates that examination findings are pertinent for early classification in the headache subgroup. We suggest that our findings may be beneficial in contributing to this collection of information, specifically the finding of improved outcomes associated with headache pain being provoked or relieved by neck movements. At the very least, identifying commonalities among demographic information and among physical impairments in populations of patients with CGH can lead to more effective, evidence-based management of patients with this disorder.
Limitations
There are methodological weaknesses to this study. The sample size would preferably have been larger and more diverse to improve the ability to extrapolate these results to the overall population. Reporting long-term effects of treatment would also have added strength to these results, as this is lacking in the literature on treatment of CGH. The retrospective nature of a chart review study design, while providing insightful data regarding patient care and outcomes, does not allow for conclusions to be drawn specifically linking the examined patient variables to the patient outcomes data, and it puts the study at risk for selection bias. Collecting data prospectively in a randomized controlled trial would be the ideal way to study this relationship between patient variables and outcomes; this is something that could be valuable to study in future research of this nature.
An additional limitation to consider that is associated with a retrospective study design is associated with data collection and control. It is difficult to ensure that data are consistently captured across subjects with this type of design. The data collection in this study was performed by a single clinician with 20 years experience, whose primary practice is limited to treatment of head and neck disorders. Based on this fact, the authors feel that using a single experienced clinician with a clinical practice focus related to the topic of the study to collect the data ensured a greater probability that the data were more consistent among patients and across the duration of the study time period.
The inclusion of 13 independent variables for this small sample resulted in another limitation of this study. The regression model was likely over-fit, inhibiting the achieving of statistical power and resulting in reaching significance for only two out of the three models. Since the two models of headache frequency and headache pain intensity did reach significance, the analysis was continued and the significant independent variables of increased age, headache provoked or relieved with movement, and having gainful employment indicate areas of interest that could be studied in future reports. Furthermore, the use of outcomes measures that have been validated in populations with CGH to measure outcomes of our dependent variables would lend more weight to these results because there would be evidence to support the fact that the measures that were used were appropriately detecting change in this sample of patients.
Conclusion
CGH has a vast impact on patients, as demonstrated by both physical and functional impairments, and thus it is important to increase efficacy of treatment by identifying patient-specific variables that are related to treatment prognosis. Increased age, provocation or relief of headache with movement, employment status, and potentially duration of symptoms were associated with improved physical and functional outcomes after a standardized physical therapy intervention that included spinal mobilization and manipulation, as well as a home exercise program. These findings build on the current knowledge base and suggest further research on outcomes of physical therapy treatment of CGH to provide more efficient and evidence-based care.
REFERENCES
- 1.Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: Diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. 1998;38:442–445. doi: 10.1046/j.1526-4610.1998.3806442.x. [DOI] [PubMed] [Google Scholar]
- 2.Martelletti P, van Suijlekom H. Cervicogenic headache: Practical approaches to therapy. CNS Drugs. 2004;18:793–805. doi: 10.2165/00023210-200418120-00004. [DOI] [PubMed] [Google Scholar]
- 3.Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther. 2006;11:118–129. doi: 10.1016/j.math.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Biondi DM. Cervicogenic headache: Mechanisms, evaluation, and treatment strategies. J Am Osteopathic Assoc. 2000;100(9Suppl):S7–S14. [PubMed] [Google Scholar]
- 5.Bogduk N. The neck and headaches. Neurologic Clinics. 2004;22(1):151–171. doi: 10.1016/S0733-8619(03)00100-2. [DOI] [PubMed] [Google Scholar]
- 6.Sizer PS, Phelps V, Brismee J. Diagnosis and management of cervicogenic headache and local cervical syndrome with multiple pain generators. J Man Manipulative Ther. 2002;10:136–152. [Google Scholar]
- 7.Leone M, D'Amico D, Grazzi L, Attanasio A, Bussone G. Cervicogenic headache: A critical review of the current diagnostic criteria. Pain. 1998;78(1):1–5. doi: 10.1016/S0304-3959(98)00116-X. [DOI] [PubMed] [Google Scholar]
- 8.Van Suijlekom HA, De Vet HC, Van Den Berg SG, Weber WE. Interobserver reliability in physical examination of the cervical spine in patients with headache. Headache. 2000;40:581–586. doi: 10.1046/j.1526-4610.2000.00090.x. [DOI] [PubMed] [Google Scholar]
- 9.Antonaci F, Bono G, Chimento P. Diagnosing cervicogenic headache. J Headache Pain. 2006;7:145–148. doi: 10.1007/s10194-006-0277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 11.Jull G, Zito G, Trott P, Potter H, Shirley D. Inter-examiner reliability to detect painful upper cervical joint dysfunction. Aust J Physiother. 1997;43:125–129. doi: 10.1016/s0004-9514(14)60406-2. [DOI] [PubMed] [Google Scholar]
- 12.Hanten WP, Olson SL, Ludwig GM. Reliability of manual mobility testing of the upper cervical spine in subjects with cervicogenic headache. J Man Manipulative Ther. 2002;10:76–82. [Google Scholar]
- 13.Antonaci F, Ghirmai S, Bono G, Sandrini G, Nappi G. Cervicogenic headache: Evaluation of the original diagnostic criteria. Cephalalgia. 2001;21:573–583. doi: 10.1046/j.0333-1024.2001.00207.x. [DOI] [PubMed] [Google Scholar]
- 14.Pollmann W, Keidel M, Pfaffenrath V. Headache and the cervical spine: A critical review. Cephalalgia. 1997;17:801–816. doi: 10.1046/j.1468-2982.1997.1708801.x. [DOI] [PubMed] [Google Scholar]
- 15.Schoensee SK, Jensen G, Nicholson G, Gossman M, Katholi C, Schoensee SK, et al. The effect of mobilization on cervical headaches. J Orthop Sports Phys Ther. 1995;21:184–196. doi: 10.2519/jospt.1995.21.4.184. [DOI] [PubMed] [Google Scholar]
- 16.Nilsson N, Christensen HW, Hartvigsen J. The effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther. 1997;20:326–330. [PubMed] [Google Scholar]
- 17.Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27:1835–1843. doi: 10.1097/00007632-200209010-00004. [DOI] [PubMed] [Google Scholar]
- 18.Bronfort G, Nilsson N, Haas M, Evans R, Goldsmith CH, Assendelft WJJ, et al. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database of Systematic Reviews. 2006:4. doi: 10.1002/14651858.CD001878.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Gross AR, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, et al. Manipulation and mobilisation for mechanical neck disorders. Cochrane Database of Systematic Reviews. 2006:4. doi: 10.1002/14651858.CD004249.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Magarey ME, Rebbeck T, Coughlan B, Grimmer K, Rivett DA, Refshauge K. Pre-manipulative testing of the cervical spine: Review, revision and new clinical guidelines. Man Ther. 2004;9:95–108. doi: 10.1016/j.math.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Zwart JA. Neck mobility in different headache disorders. Headache. 1997;37:6–11. doi: 10.1046/j.1526-4610.1997.3701006.x. [DOI] [PubMed] [Google Scholar]
- 22.Watson DH, Trott PH. Cervical headache: An investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13:272–284. doi: 10.1046/j.1468-2982.1993.1304272.x. [DOI] [PubMed] [Google Scholar]
- 23.Jull G, Barrett C, Magee R, Ho P. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia. 1999;19:179–185. doi: 10.1046/j.1468-2982.1999.1903179.x. [DOI] [PubMed] [Google Scholar]
- 24.Dumas JP, Arsenault AB, Boudreau G, Magnoux E, Lepage Y, Bellavance A, et al. Physical impairments in cervicogenic headache: Traumatic vs. nontraumatic onset. Cephalalgia. 2001;21:884–893. doi: 10.1046/j.1468-2982.2001.00264.x. [DOI] [PubMed] [Google Scholar]
- 25.van Suijlekom HA, Lame I, Stomp-van den Berg SG, Kessels AG, Weber WE, van Suijlekom HA, et al. Quality of life of patients with cervicogenic headache: A comparison with control subjects and patients with migraine or tension-type headache. Headache. 2003;43:1034–1041. doi: 10.1046/j.1526-4610.2003.03204.x. [DOI] [PubMed] [Google Scholar]
- 26.Cook CE, Richardson JK, Pietrobon R, Braga L, Silva HM, Turner D. Validation of the NHANES ADL scale in a sample of patients with report of cervical pain: Factor analysis, item response theory analysis, and line item validity. Disabil Rehabil. 2006;28:929–935. doi: 10.1080/09638280500404263. [DOI] [PubMed] [Google Scholar]
- 27.Jull GA, Stanton WR. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101–108. doi: 10.1111/j.1468-2982.2004.00811.x. [DOI] [PubMed] [Google Scholar]
- 28.Maitland G. Maitland's Vertebral Manipulation. Oxford, UK: Butterworth-Heinemann; 2001. [Google Scholar]
- 29.Kendall F, McCreary E. Muscles, Testing and Function. 3rd ed. Baltimore, MD: Williams and Wilkins; 1983. [Google Scholar]
- 30.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO: Mosby; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hall T, Robinson K. The flexion-rotation test and active cervical mobility: A comparative measurement study in cervicogenic headache. Man Ther. 2004;9:197–202. doi: 10.1016/j.math.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Butler D. The Sensitive Nervous System. Adelaide, Australia: Noigroup Publications; 2000. [Google Scholar]
- 33.Elvey RL. Physical evaluation of the peripheral nervous system in disorders of pain and dysfunction. J Hand Ther. 1997;10:122–129. doi: 10.1016/s0894-1130(97)80066-x. [DOI] [PubMed] [Google Scholar]
- 34.Schunk C, Rutt R. TAOS Functional Index: Orthopaedic rehabilitation outcomes tool. Therapeutic Associates Outcomes System. J Rehabil Outcomes Measurement. 1998;2:55–61. [Google Scholar]
- 35.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157–162. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- 36.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–392. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 37.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. European J Pain. 2004;8:283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30:1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- 39.Schoenen J. Guidelines for trials of drug treatments in tension-type headache. Cephalalgia. 1995;15:165. doi: 10.1046/j.1468-2982.1995.015003165.x. [DOI] [PubMed] [Google Scholar]
- 40.Portney L, Watkins M. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, NJ: Prentice-Hall; 2000. [Google Scholar]
- 41.Biondi DM, Saper JR. Geriatric headache: How to make the diagnosis and manage the pain. Geriatrics. 2000;55:43–45. 40, 48–50. [PubMed] [Google Scholar]
- 42.Hanten WP, Olson SL, Lindsay WA, Lounsberry KA, Stewart JK. The effect of manual therapy and a home exercise program on cervicogenic headaches: A case report. J Man Manipulative Ther. 2005;13:35–43. [Google Scholar]
- 43.Koes BW, Bouter LM, van Mameren H, Essers AH, Verstegen GJ, Hofhuizen DM, et al. A randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints: Subgroup analysis and relationship between outcome measures. J Manipulative Physiol Ther. 1993;16:211–219. [PubMed] [Google Scholar]
- 44.Donelson R, Silva G, Murphy K, Donelson R, Silva G, Murphy K. Centralization phenomenon: Its usefulness in evaluating and treating referred pain. Spine. 1990;15:211–213. [PubMed] [Google Scholar]
- 45.Childs JD, Fritz JM, Piva SR, Whitman JM. Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther. 2004;34:686–696. doi: 10.2519/jospt.2004.34.11.686. discussion 97–100. [DOI] [PubMed] [Google Scholar]
- 46.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 47.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 48.Gesztelyi G, Bereczki D. Determinants of disability in everyday activities differ in primary and cervicogenic headaches and in low back pain. Psychiat Clin Neuros. 2006;60:271–276. doi: 10.1111/j.1440-1819.2006.01501.x. [DOI] [PubMed] [Google Scholar]
- 49.Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status. Spine. 2003;28:2030–2035. doi: 10.1097/01.BRS.0000083325.27357.39. [DOI] [PubMed] [Google Scholar]


