Abstract
Background
Performing a lumbar puncture in an unwell child can cause anxiety in both the parent and the junior doctor. There is increasing evidence of post‐lumbar‐puncture complications in this age group.
Aims
To improve the documentation, consent for and technical performance of paediatric lumbar punctures to 100% of the required standard within 3 months.
Setting
The paediatric emergency department of a the Royal North Shore Hospital (University of Sydney, Sydney, Australia).
Participants
Paediatric emergency staff, including residents, registrars and consultants.
Methods
Medical records of 40 consecutive children who had undergone a lumbar puncture in the 6 months before the introduction of the lumbar‐puncture proforma were reviewed. After introduction of the proforma, the records of 25 consecutive patients were reviewed to assess changes in the outcome measures. Before introduction of the proforma, junior medical staff were instructed in the procedure using specialised lumbar puncture manikins (Baby Stap; Laerdel, USA).
Results
Before introduction of the proforma, the median number of documented indicators was 4, out of a maximum of 12. There was almost no documentation of parental consent, patient complications and analgesia. Introduction of the proforma resulted in a highly marked increase to a median of 12 documented indicators per patient (p<0.01, 95% confidence interval 6 to 8).
Conclusions
The introduction of a lumbar‐puncture proforma and formal teaching sessions using a paediatric manikin led to a marked improvement in the documentation of paediatric lumbar‐punctures. Lumbar‐punctures can be performed only by accredited medical officers who have achieved competency on the lumbar‐puncture teaching manikin.
Royal North Shore Hospital is a large teaching hospital of The University of Sydney, Sydney, Australia. The emergency department treats 45 000 patients every year, of whom nearly 15 000 are children <18 years of age. The department has separate paediatric and adult facilities. This study focused on all junior staff of the paediatric emergency department (residents, senior residents, and registrars) and consultants.
Outline of the problem
The performance of a lumbar‐puncture in an unwell child can cause anxiety to the parent, the child and the junior doctor. Despite the fact that it is a relatively common procedure in paediatrics, there is a paucity of data in the area of procedural documentation and complications.1,2 Post‐lumbar‐puncture complications, particularly postdural headaches, are well recognised in adults.3,4,5 Until recently, there has been little information available on post‐lumbar‐puncture complications in children, and these were thought to be rare.1,6,7
However, more recent studies on patients in paediatric oncology 8,9 and general paediatric departments1,2,6 have reported marked rates of headache (8–27%) and backache (40%) after lumbar‐puncture.1 The consensus is that the rate of complications increases with increasing age, particularly in post‐pubertal girls.1,2,3,6,8,9 No data are available on the incidence of neck stiffness, nausea and vomiting in children post‐lumbar‐puncture.
Before this study, documentation in the paediatric emergency department was thought to be of a poor standard, rendering assessment of lumbar‐puncture complications difficult. Medical staff had a wide range of ability and experience in the performance of technical procedures, making the assessment of an individual's procedural proficiency also difficult. Senior medical staff had repeatedly raised concerns about the haphazard and incomplete consent process. They believed that parents were not being made aware of potential post‐lumbar‐puncture complications.
Aim
Our study aimed to measure the effect of introducing a mandatory lumbar‐puncture adhesive sticker proforma, a parent fact sheet and compulsory teaching for all junior staff using a lumbar‐puncture manikin. It was hoped that the documentation of parental consent and technical performance of lumbar‐punctures would improve to 100% of the required departmental standard within 3 months. Our newly updated guideline on paediatric lumbar‐puncture was reviewed, and was considered the ideal standard for lumbar‐punctures performed in our department. The guideline set out the minimum requirements in terms of consent, documentation, sterility and technical performance, among others. The team agreed that appropriate completion of the indicators on the sticker would meet the departmental requirements relating to documentation. Local ethical approval was obtained for this study.
Methods
Design of study
A multidisciplinary project team with fundamental knowledge was formed to investigate the extent of the problem. Using clinical practice improvement methods and the sequential “plan, do, study and act” cycle, we implemented and tested changes to achieve our improvement goal.9
The project team met and developed a list of 12 indicators that we thought were important in the documentation and performance of a paediatric lumbar‐puncture (box 1). Using this agreed set of indicators, we then audited the medical records of 40 consecutive children who had had a lumbar‐puncture performed in the paediatric emergency department in the 6 months before the start of the study. These records were obtained by cross referencing the medical record numbers of all paediatric lumbar‐puncture specimens that had been received by the microbiology laboratory during the relevant time period. There may in fact have been more lumbar‐punctures performed than we were aware of, as those abandoned after numerous unsuccessful attempts would not have had a specimen received in the microbiology laboratory.
Box 1 Lumbar‐puncture indicators
Is the indication for lumbar‐puncture documented?
Was consent obtained?
Was consent documented?
Is the procedure documented as per departmental guidelines?
Is the date, time and operator clearly documented?
How many attempts were made?
Any documented complications with the procedure?
Any documented patient complications?
Any documented analgesia used during the procedure?
Are the results documented?
Has the appropriate management plan been instituted as per the results?
Is there documentation that parents have been notified of the results?
Interventions
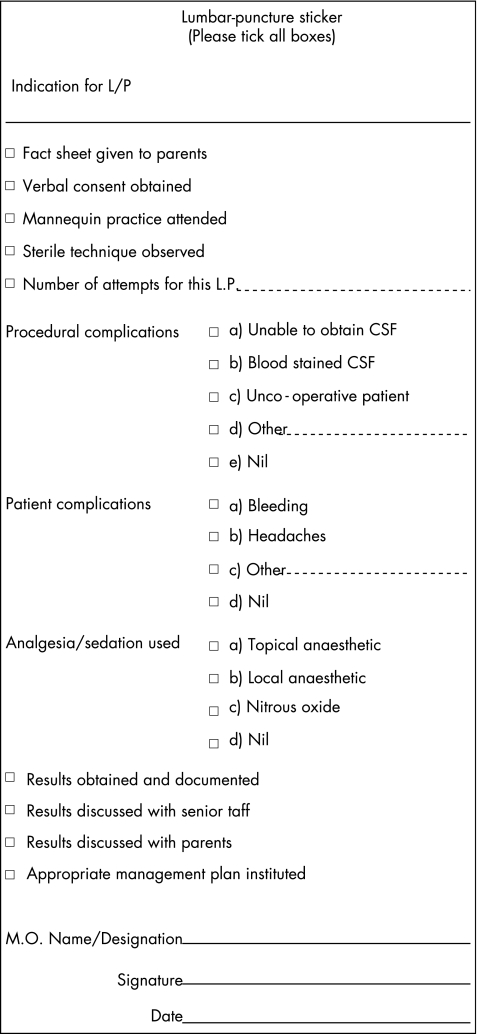
The study group modified a locally available parent information sheet for lumbar‐puncture and developed a proforma sticker based on the agreed indicators (fig 1). The sticker was to replace the medical record for the documentation of paediatric lumbar‐punctures.
Figure 1 Lumbar‐puncture sticker.
Before the study, all staff attended a training session in lumbar‐puncture procedure using lumbar‐puncture teaching manikins (Baby Stap, Laerdel, USA). All junior staff had to attend the training sessions and demonstrate competency on lumbar‐puncture procedures before being accredited to perform them in the paediatric emergency department. During the orientation sessions, all new junior staff were shown an ideal lumbar‐puncture by a senior staff member using the manikin. Special emphasis was be placed on positioning, technique and sterility. In some of the sessions a nurse would assist by “holding” the patient. We did not have a parent present as we thought this might be too stressful for the junior staff. After the demonstration, each new doctor was required to perform a lumbar‐puncture to the satisfaction of the senior supervisor. A tick chart was used to score each junior doctor. Our end point for accreditation was success in obtaining fluid from the manikin, provided the correct technique had been demonstrated. Junior doctors unsuccessful at their first attempt were given further supervised opportunities before being retested.
For the purposes of this study a lumbar‐puncture attempt was defined as the passage of a lumbar‐puncture needle into the lumbar space of a child by a doctor, with the aim of obtaining cerebrospinal fluid. A successful attempt results in cerebrospinal fluid being obtained and an unsuccessful attempt results in failure to do so. Fisher's exact tests were used to compare the frequency of documented indicators and Mann–Whitney U tests were used to compare overall indicators documented. Statistical analysis was carried out using a commercial software package (Minitab 14, Minitab).
Results
Results of assessment
On completion of the 3‐month study, the records of 25 children who had undergone a lumbar‐puncture in the emergency department were reviewed. These records were audited using the 12 indicators displayed. (box 1).
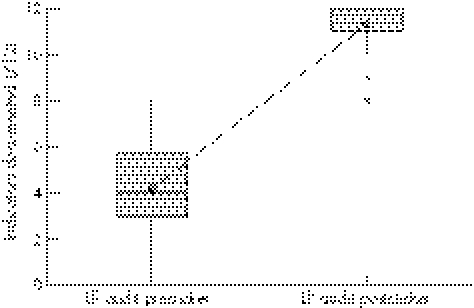
Before the study, the median number of documented indicators was 4 out of a maximum of 12 (fig 2). One child had undergone a lumbar‐puncture, with no documentation evident in the clinical record. Only 10% of records showed evidence that parental consent had been obtained. We found no documentation of the use of analgesia for the performance of a lumbar‐puncture or post‐lumbar‐puncture complications. Documentation was better for the following indicators: indication for lumbar‐puncture (70%), number of lumbar‐puncture attempts (78%) and lumbar‐puncture results (78%; table 1).
Figure 2 Box plot of indicators documented before and after introduction of lumbar‐puncture (LP) sticker.
Table 1 Indicators documented before and after introduction of lumbar‐puncture sticker.
| Documented indicator | Before (%) | After (%) | p Value |
|---|---|---|---|
| 1. Indication for lumbar‐puncture documented? | 70 | 100 | 0.002 |
| 2. Consent obtained? | 10 | 100 | <0.001 |
| 3. Consent documented? | 10 | 100 | <0.001 |
| 4. Procedure documented as per guidelines? | 35 | 100 | <0.001 |
| 5. Date, time and operator documented? | 18 | 96 | <0.001 |
| 6. Number of attempts documented? | 78 | 100 | 0.010 |
| 7. Documented complications with procedure? | 30 | 96 | <0.001 |
| 8. Documented patient complications? | 0 | 96 | <0.001 |
| 9. Documentation of analgesia used? | 0 | 96 | <0.001 |
| 10. Results documented? | 78 | 92 | 0.181 |
| 11. Appropriate management plan instituted? | 85 | 96 | 0.235 |
| 12. Documentation of parents having been notified? | 8 | 56 | <0.001 |
| Blood‐stained lumbar‐puncture samples | 55 | 40 | 0.310 |
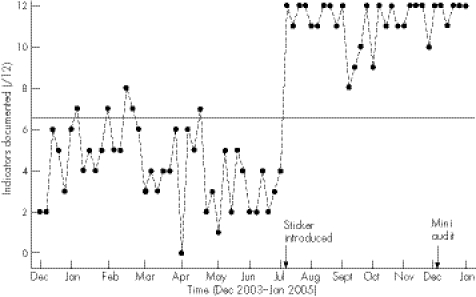
Figure 3 Run chart of indicators documented before and after introduction of lumbar‐puncture sticker.
In the pre‐study cohort, 22 of 40 lumbar‐punctures (55%) were reported as bloodstained by our laboratory. We are unable to make a comment on the lumbar‐puncture failure rate and bleeding complications in the pre‐study group as the medical documentation was insufficient.
Results of interventions
Introduction of the proforma (fig 2) resulted in a highly significant increase in the number of indicators documented for each patient from a median of 4 to 12 (p<0.01, 95% confidence interval 6 to 8).
All categories of documentation were much improved. In all 25 cases junior doctors ticked the box that stated that they had given the fact sheet to the parents, had obtained consent and that this was documented in the medical record. Only the documentation of parental notification of lumbar‐puncture results was unsatisfactory (table 1).
The number of bloodstained taps remained high at 10 of 25 (40%) and had not decreased significantly (p = 0.31). The study group was concerned about the continued high rate of bloody taps and is considering further quality improvement strategies to specifically target this outcome. Decreasing the number of attempts may not reduce the number and severity of complications such as post‐lumbar‐puncture headache, but may increase the confidence of junior doctors and alleviate some parental anxiety.
A method of assessing clinical competence and establishing ongoing learning curves of individual trainees and clinicians is by cumulative‐summation analysis.11,12 This audit method provides useful information about individual performance after initial training as well as ongoing surveillance. High failure rates or declining performance on a cumulative‐summation graph signal a need for retraining.13 Insufficient documentation on individual performance was available before this study to assess the effect of training on lumbar‐puncture attempts. With improved documentation of lumbar‐punctures after this study, a system of ongoing surveillance using performance indicators such as the number of lumbar‐puncture attempts and the quality of samples retrieved will establish the effectiveness of competence training in maintaining the high standards put forward in local guidelines.
We acknowledge that the complication of headache would not be detectable at the time of the lumbar‐puncture, and our second‐generation proforma will be divided into early and late complications of the lumbar‐puncture. The late‐complication proforma will be completed only before the discharge of the patient. We found no reported bleeding complications or failed lumbar‐punctures in the post‐study group. The patchy documentation in the pre‐study group made comparison of patient cooperation during the lumbar‐puncture procedure difficult.
A random audit of five paediatric lumbar‐punctures was performed 3 months after the study was completed. This mini audit showed that improvements were sustained, with a median of 12 documented indicators. Four of the five lumbar‐punctures in the mini audit were successful at the first attempt. Only one was reported as bloodstained.
Lessons and messages
The introduction of a lumbar‐puncture proforma led to a large improvement in the documentation of paediatric lumbar‐punctures in this hospital. Obtaining and documenting parental consent for a lumbar‐puncture improved markedly. Junior staff was instructed to tick the consent box only after the parents had had time to read and understand the contents of the parent fact sheet on lumbar‐punctures and to have an informed discussion of the risks and benefits of the procedure with the doctor. Although it was hoped that this intervention would improve the quality of the consent process, we cannot be certain that all doctors followed these instructions before ticking the consent box.
Feedback from the junior staff questionnaire was that the proforma was less time consuming than writing notes and that it was easily available and user‐ friendly. A key factor in sustainability of this intervention is the ready availability of the sticker in the treatment room. There are also visible reminders in the emergency department treatment room about the sticker and parent fact sheet. Monthly run charts with up‐to‐date information on junior staff performance are placed in the tearoom to remind junior staff of their success in this project. We are able to monitor progress, and if performance deteriorates we will be able to deal with this appropriately.
The authors acknowledge the mitigating Hawthorne effect created by maintaining a system whereby regular auditing of lumbar‐puncture performance is made possible by documentation of indicators on a proforma.14 By creating a proforma, a trainee is committed to improving performance on documentation for lumbar‐puncture and, in doing so, reaches a high standard of documentation for a complex clinical procedure. This “Hawthorne strategy” reinforces the initial lumbar‐puncture training on an ongoing basis. This is having a positive effect on the training, achieving and maintaining of high standards in junior doctors.15
Another factor that ensures sustainability of the project is that the lumbar‐puncture teaching sessions have become an essential part of junior staff orientation. Each term, medical staff must attend the lumbar‐puncture teaching sessions and achieve competency, as outlined earlier, at these teaching sessions before being accredited to perform a lumbar‐puncture in the paediatric emergency department. This will hopefully continue to create an awareness of the importance of lumbar‐puncture performance and documentation. Finally, the results of this study have convinced us to make our second‐generation lumbar‐puncture adhesive proforma and parent fact sheet mandatory for all paediatric lumbar‐punctures performed at our hospital. It has also highlighted that a reduction in blood stained taps remains a priority quality improvement challenge for our hospital.
Footnotes
Competing interests: None declared.
References
- 1.Ebinger F, Kosel C, Pietz J.et al Headache and backache after lumbar puncture in children and adolescents: a prospective study. Paediatrics 20041131588–1592. [DOI] [PubMed] [Google Scholar]
- 2.Ebinger F, Kosel C, Pietz J.et al Strict bed rest following lumbar puncture in children and adolescents is of no benefit. Neurology 2004621003–1005. [DOI] [PubMed] [Google Scholar]
- 3.Wee L. The incidence of postdural puncture headache in children. Anaesthesia 1996511164–1166. [DOI] [PubMed] [Google Scholar]
- 4.Lybecker H, Djernes M, Schmidt J. Postdural puncture headache (PDPH): onset, duration, severity and associated symptoms. An analysis of 75 consecutive patients with PDPH. Acta Anaesthesiol Scand 199539605–612. [DOI] [PubMed] [Google Scholar]
- 5.Vilmig S, Kloster R, Sandvik L. The importance of sex, age, needle size, height and body mass index in post‐lumbar puncture headache. Cephalalgia 200121738–743. [DOI] [PubMed] [Google Scholar]
- 6.Ylonen P, Kokki H. Management of postdural puncture headache with epidural blood patch in children. Paediat Anaesth 200212526–529. [DOI] [PubMed] [Google Scholar]
- 7.Adler M, Comi A, Walker A. Acute hemorrhagic complication of diagnostic lumbar puncture. Pediatr Emerg Care 200117184–188. [DOI] [PubMed] [Google Scholar]
- 8.Ramamoorthy C, Geiduschek J, Bratton S.et al Postdural puncture headache in Paediatric oncology patients. Clin Pediatr 199837247–251. [DOI] [PubMed] [Google Scholar]
- 9.Bolder P. Postlumbar puncture headache in Pediatric oncology patients. Anesthiology 198665696–698. [DOI] [PubMed] [Google Scholar]
- 10.Langley G J, Nolan K M, Nolan T W.et al A model for improvement. In: The improvement guide: a practical approach to enhancing organization performance. San Francisco: Jossey Bass, 19963–11.
- 11.Bolsin S, Colson M. The use of the Cusum technique in the assessment of trainee competence in new procedures. Int J Qual Health Care 200012433–438. [DOI] [PubMed] [Google Scholar]
- 12.Bolsin S. Routes to quality assurance: risk adjusted outcomes and personal professional monitoring. Int J Qual Health Care 200012367–369. [DOI] [PubMed] [Google Scholar]
- 13.Naik V N, Devito I, Halplumbar punctureern S H. Cusum analysis is a useful tool to assess resident proficiency at insertion of labour epidurals. Can J Anaesth 200350694–698. [DOI] [PubMed] [Google Scholar]
- 14.Franke R H, Kaul J D. The Hawthorne experiments: first statistical interpretation. Am Sociol Rev 197843623–643. [Google Scholar]
- 15.Lied T R, Kazandjian V A. A Hawthorne strategy: implications for performance measurement and improvement. Clin Perform Qual Health Care 19986201–204. [PubMed] [Google Scholar]