Abstract
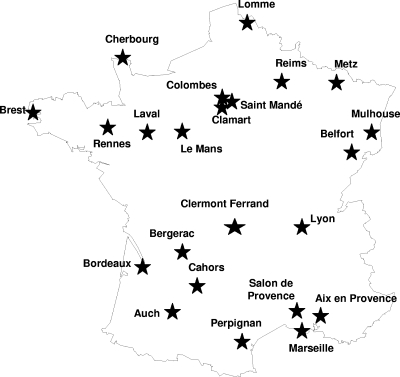
We conducted a prospective multicenter study of methicillin-resistant Staphylococcus aureus (MRSA) isolates, including the first five consecutive clinical isolates, collected between September 2006 and February 2007 in 23 hospitals located throughout France (Fig. 1). The 111 isolates were tested for their antibiotic susceptibility patterns and were extensively characterized by screening for drug resistance and agr alleles, multilocus sequence typing (ST), staphylococcal cassette chromosome mec (SCCmec) typing, spa typing, and PCR profiling of 21 toxin genes. Clones were designated by their ST followed by their SCCmec type (I to VI). The Lyon clone ST8-IV or ST8-IVvariant (n = 77; 69.4%) was widely distributed. Four minor clones were also detected, namely, the “classical” Pediatric clone ST5-IV (n = 9; 8.1%), the “new” Pediatric clone ST5-VI (n = 8; 7.2%), the clone Geraldine ST5-Itruncated (n = 7; 6.3%), and the European clone ST80-IV (n = 4; 3.6%). The six other isolates were related to five rare clones. Relative to that of other European countries, the situation in France is marked by the predominance of a specific major clone and the worrying emergence of minor clones with enhanced virulence and new antibiotic susceptibility profiles.
A thorough knowledge of the epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) isolates is needed to prevent their spread, to determine the clinical spectrum of MRSA disease, and to optimize treatment. Many molecular techniques have been developed to allow the unambiguous assignment of each isolate to previously described or new MRSA clones (8, 15, 26, 29), and these techniques have helped to monitor the evolutionary process of the emergence and temporal and geographical spread of pandemic clones (1, 8, 38).
Several epidemic healthcare-associated MRSA clones (HA-MRSA) have emerged since the 1970s. During the last decade, five major pandemic clones, named Iberian, Brazilian, Hungarian, New York/Japan, and Pediatric, have been identified (1, 35, 36), while other new or preexisting clones emerged in some specific areas. The recent worldwide spread of several community-acquired MRSA (CA-MRSA) clones made even more complex the understanding of this epidemiology (42).
In France, several new MRSA clones have been described in the last decade (5, 16, 28), but the current epidemiology of MRSA is poorly documented. The aim of this study was to characterize MRSA isolates collected during a 6-month prospective multicenter study in representative French hospitals. The isolates were extensively typed by accessory gene regulator (agr) allele determination, multilocus sequence typing (MLST), spa typing, structural analysis of the staphylococcal cassette chromosome mec (SCCmec) element, toxin profiling, and antimicrobial resistance phenotyping.
MATERIALS AND METHODS
We conducted a prospective multicenter study of MRSA isolates collected between September 2006 and February 2007 by 23 representative randomly selected French hospital laboratories. The first five isolates, obtained from different patients by invasive sampling (blood or fluid from a normally sterile site; one isolate per patient) were sent to the French National Reference Center for Staphylococci (Lyon, France). Isolates were considered to be community acquired if a sample obtained within 48 h after admission was culture positive and hospital acquired if obtained later. Antimicrobial susceptibility was determined by each participating laboratory as recommended by the French Society for Microbiology (17).
The identification of the 111 isolates was confirmed by multiplex PCR amplification of the agr (25) and by determining the agr allelic group. The isolates were fully typed by the French National Reference Center for Staphylococci (Lyon, France) and were screened for genes encoding methicillin resistance (mecA), staphylococcal enterotoxins (se) A, B, C, D, H, K, L, M, O, P, Q, and R (sea to sed, seh, sek to sem, and seo to ser), toxic shock syndrome toxin 1 (tst), exfoliative toxins A, B, and D (eta, etb, and etd), Panton-Valentine leukocidin (PVL; luk-PV), class F LukM leukocidin (lukM), beta-hemolysin (hlb), and epidermal cell differentiation inhibitor (edinA, edinB, and edinC), as previously described (25, 43). spa typing was performed with the Ridom Staph Type standard protocol (www.ridom.com) and by using the Ridom SpaServer, which automatically analyses spa repeats and assigns spa types (http://spa.ridom.de/index.shtml). MLST was performed as described elsewhere (14) for all isolates carrying agr-2 or agr-3 and for 54 of 81 agr-1 isolates representative of all toxin types, susceptibility profiles, and SCCmec types detected within this subgroup. SCCmec types were determined by PCR with a simplified version of Kondo's typing system, including M-PCR-1 and M-PCR-2, without determining differences in the junkyard region (26). In specific cases, SCCmec typing was also performed as recommended by Oliveira et al. (33) and ccrB gene sequencing was performed as previously described (33). We use the classification of Ito et al. (24) and Ma et al. (30) for SCCmec elements.
RESULTS AND DISCUSSION
The results of molecular typing methods indicated that one major clone and four minor clones of MRSA are currently predominant in France. A total of 111 different MRSA isolates were examined. They were isolated by culture of blood (n = 82; 74%), puncture fluid from a sterile cavity (n = 28; 25%), or cerebrospinal fluid (one case). The patients were hospitalized in intensive care units (n = 26, 23.4%), daycare units (n = 62; 55.9%), or outpatient departments (n = 23; 20.7%). Sixty-seven isolates (60.3%) were hospital acquired. All isolates with the same ST and identical or variant SCCmec elements were considered to belong to the same clone.
A first major clone, comprising 77 strains (69.4% of all isolates), was related to the Lyon clone (16). Since the 1990s, the Lyon clone has gradually replaced the gentamicin-resistant Iberian clone (ST247; SCCmec type I) that predominated in France in the 1990s (28). In our study, the Lyon clone was isolated in 22 of the 23 participating hospitals, confirming its wide dissemination all over France, and was mainly hospital acquired (48 hospital-acquired and 31 community-acquired isolates). The characteristics shared by these isolates corresponded largely to those reported by Ferry et al. (16), namely, agr allele 1, ST8, spa type t008 and related, SCCmec type IV (n = 70) or type IVvariant (n = 7) with mec gene complex class B, and ccrAB allotype 2, associated with a supplementary ccr gene in variants. Nevertheless, the strains were more diverse than initially reported (16). The sea gene was found in only 88% of isolates (68 out of 77), sed in 49% (38 out of 77), ser in 49% (38 out of 77), and hlb in 12.7% (10 out of 77 isolates). The most-common toxin types were sea alone (43.6%) and sea plus sed and ser (41%). Although these isolates were consistently resistant to methicillin and fluoroquinolones, the antimicrobial susceptibility profiles were highly variable (more than 20 antibiotypes). This points to frequent acquisition and loss of toxin-carrying and resistance-carrying mobile genetic elements, such as bacteriophages, plasmids, or transposons, even if some changes in antibiotic susceptibility are due to point mutations. This confirms that the horizontal mobility of such genetic elements in MRSA is probably greater than previously believed (23, 37). Moreover, in addition to the classical ccrAB allotype 2 of SCCmec type IV, a supplementary recombinase locus (ccrC in two cases and ccrAB4 in five cases) was detected in seven isolates belonging to the Lyon clone and confirmed in single isolated colonies. Except in strains harboring SCCmec type III (with ccrAB3), which is always associated with SCCmercury (with ccrC) (8), the combination of two ccr genes (ccrAB with ccrC or two ccrC genes) has rarely been reported (8, 21, 41). To our knowledge, the combination of two ccrAB genes (ccrAB2 and ccrAB4) has not previously been reported in an S. aureus strain and has only been reported once in a Staphylococcus epidermidis strain (20). It remains to be determined whether the different ccrs are located within the SCCmec element or outside the cassette in the chromosome, as previously described for mecA-negative strains. Further structural studies of these SCCmec elements are under way. Full sequencing of the cassette, cohybridization, or artificial excision with a high-copy-number plasmid harboring an excisionase will probably help to resolve this issue. Finally, this clone shared some features (ST8 and SCCmec IV) with USA300, an epidemic CA-MRSA clone in the United States (42), but these two clones are very different according to their resistance profiles and their toxin profiles, and no relation has been established between these two clones. Moreover, USA300 was initially described as a CA-MRSA clone (even if this clone has now invaded U.S. hospitals), while the Lyon clone is typically a French HA-MRSA clone.
The first minor clone found here (n = 7), the Geraldine clone, had already been identified during a passive French survey of S. aureus infections in 2002 and 2003 (12). This tst-MRSA clone caused both toxic shock syndrome and suppurative infections. It was described as agr-2, ST5, spa type t002 or related, and SCCmec type IV. In our study, seven isolates (6.3%) from six hospitals located throughout France matched these molecular characteristics. As previously reported, the infections were both community acquired (n = 3) and hospital acquired (n = 4). However, our patients had a median age of 74 years, compared to only 3 years in Durand's study (12). As also described by Durand et al., we observed a specific toxinotype in which the tst, sec, sed, sel, sem, seo, and ser genes were always present, with the exception of one strain that was negative for tst, sec, and sel (Table 1). This latter strain probably arose through the loss of the SaPI mobile genetic element known to harbor these three toxin genes. The antibiotic susceptibility pattern of this clone was characteristic, with resistance to methicillin and fusidic acid in every case and to kanamycin and tobramycin in five of the seven isolates. The main difference relative to the previous description of this clone concerned the type of SCCmec cassette. It was initially identified as type IV in Oliveira's typing system (33), because PCR was positive for locus D but negative for locus A (corresponding to the pls fragment). The use of Kondo's typing system (26) revealed that it displayed features associated with SCCmec type I (mec gene complex class B and ccrAB allotype 1) as previously reported (29). We therefore assume that this clone harbors a new subtype of the SCCmec type I element, characterized by deletion of the pls fragment, and therefore propose to name it “truncated SCCmec type I”.
TABLE 1.
Characteristics of the most frequent MRSA clones isolated in Francea
| Characteristic or parameter | Lyon clone | Geraldine Clone | Pediatric clone
|
European ST80 clone | |
|---|---|---|---|---|---|
| “Classical” subtype | “New” subtype | ||||
| No. of isolates (%) | 77 (69.4) | 7 (6.3) | 9 (8.1) | 8 (7.2) | 4 (3.6) |
| No. of health care-associated isolates (%) | 47 (61) | 4 (57) | 6 (66) | 6 (75) | 3 (75) |
| No. of hospitals (out of 23) | 22 | 6 | 5 | 5 | 3 |
| Molecular characteristics | |||||
| agr allelic group | 1 | 2 | 2 | 2 | 3 |
| ST | 8 | 5 | 5 | 5 | 80 |
| Clonal complex ST | 8 | 5 | 5 | 5 | 80 |
| spa type | t008 and related | t002 and related | t002 and related | t777 | t044 |
| SCCmec type | IV (n = 70) or IVvariant (n = 7) | Itruncated | IV | VI | IV |
| mec complex | B | A | B | B | B |
| ccr allotype | AB2 with or without AB4 (n = 5) or C (n = 2) | AB1 | AB2 | AB4 | AB2 |
| Toxin genes | |||||
| Always positive | tst, sec, sed, sel, sem, seo, serb | sem, seo | sed, sem, seo, ser | luk-PV, etd, edin | |
| Always negative | seb, sec, seh, sek, sel, sem, seo, tst, eta, etb, etd, luk-PV, lukM, edin | sea, seb, seh, sek, sel, sep, eta, etb, etd, luk-PV, lukM, edin, hlb | sea, sec, seh, sek, seq, tst, eta, etb, etd, luk-PV, lukM, edin | sea, seb, sec, sek, sel, eta, etb, luk-PV, lukM, edin | sea, seb, sec, sed, seh, sek, sel, sem, seo, sep, seq, tst, eta, etb, lukM, edin |
| Variably positive (%) | sea (86), sed (49), ser (49), hlb (13) | seb (22), sed (66), sep (44), ser (66), hlb (11) | sep (87), hlb (25) | ||
| Susceptibility pattern | |||||
| Always resistant | Pen, Met, Flq | Pen, Met, Fus | Pen, Met, Flq | Pen, Met, Flq | Pen, Met, Kan, Fus |
| Variably resistant (% resistant) | Kan (75.3), Tob (75.3), Gen (2.6), Ery (50.6), Lin (53.2), Pri (7.8), Rif (1.3), Fos (9.1), Fus (9.1), Sxt (96.1) | Kan (28), Tob (28), Ery (14) | Kan(33), Tob (33), Ery (11) | Ery (12), Lin (12) | Ery (25) |
| Always susceptible | Tec, Van | Gen, Flq, Lin, Pri, Rif, Fos, Sxt, Tec, Van | Gen, Lin, Pri, Fus, Rif, Fos, Sxt, Tec, Van | Kan, Tob, Gen, Pri, Fus, Rif, Fos, Sxt, Tec, Van | Tob, Gen, Flq, Lin, Pri, Rif, Fos, Sxt, Tec, Van |
spa, staphylococcal protein A; ccr, cassette chromosome recombinase; tst, toxic shock syndrome toxin 1 gene; luk, staphylococcal leukocidin; hlb, beta-hemolysin; edin, epidermal cell differentiation inhibitor; eta, exfoliatin A; etb, exfoliatin B; etd, exfoliatin D; Pen, penicillin; Met, methicillin; Kan, kanamycin; Tob, tobramycin; Gen, gentamicin; Ery, erythromycin; Lin, lincomycin; Pri, pristinamycin; Rif, rifampin; Fos, fosfomycin; Van, vancomycin; Tec, teicoplanin; Sxt, trimethoprim-sulfamethoxazole; Fus, fusidic acid; Flq, fluoroquinolone.
One Geraldine clone isolate was negative for tst, sec, and sel.
Another minor clone was the Pediatric clone (n = 17), first identified in a pediatric hospital in Portugal in 1992 (40) and subsequently detected in Poland, Argentina, Colombia, and the United States (19, 32, 40). This clone was recently subdivided into two clones on the basis of a different ccrAB allotype and J1 region of the genetic SCCmec element (34). The first, referred to here as the “classical” Pediatric clone, had SCCmec type IV with ccrAB2 and represented most strains belonging to the original Pediatric clone identified in Portugal and internationally (40). The second, referred to here as the “new” Pediatric clone, had SCCmec type VI with ccrAB4 and was restricted to a few Portuguese hospitals (34). We detected both these clones in this study. Nine isolates (8.1% of all MRSA isolates) collected from five hospitals matched the characteristics of the “classical” Pediatric clone, with the agr-2 allele, ST5, spa type related to t311 (t045, t067, t509, t2173, or t1818), and SCCmec type IV (mec gene complex class B and ccrAB allotype 2). These isolates were also characterized by the presence of sem and seo and by resistance to methicillin and fluoroquinolones (Table 1). Eight other isolates (7.2%) were related to the “new” Pediatric clone. They possessed the agr-2 allele, ST5, a unique spa type t777, and SCCmec type VI (mec gene complex class B and ccrAB type 4). The sed, sem, seo, and ser genes were always present, and the isolates were resistant to methicillin and fluoroquinolones and susceptible to all aminoglycosides. This is the first description of the “new” Pediatric clone outside of Portugal. Interestingly, it was as frequent as the “classical” Pediatric clone that represents a specific and unusual epidemiology.
The last minor clone was the European ST80 clone, which is one of the CA-MRSA clones most widespread in Europe (10, 22, 31, 42, 45). It expresses PVL and can cause severe skin and soft-tissue infections, as well as rapidly fatal pneumonia and extensive bone and joint infections (11, 18). The prevalence of this clone in France was estimated at less than 1% in 2004 (39). In the present study, four isolates (3.6%), three of which were community acquired, presented the specific profile of this clone, namely the agr-3 allele, ST80, and SCCmec type IV (mec gene complex class B and ccrAB type 2), that is associated with a specific antibiotic-susceptibility pattern, including resistance to methicillin, kanamycin, and fusidic acid. All the isolates had the same spa type (t044) and the same toxinotype (luk-PV, etd, and edin). They were collected from three hospitals that are distant from one another, highlighting the widespread dissemination of this clone. Our results indicate a slow but worrying emergence of this clone (39) that should be watched closely in coming years.
Finally, we collected six sporadic isolates: one agr-1, ST1041 with SCCmec type V harboring luk-PV; one agr-1, ST1042 with SCCmec type III; two agr-1, ST247 with SSCmec type I; one agr-2, ST5 with SCCmec type I; and one agr-3, ST88 with SCCmec type I.
This study provides an overview of the invasive MRSA clones currently circulating in France. The pattern of MRSA clonal lineages is very different from that observed in neighboring countries, where, according to the most-recent data, the predominant clones are ST45-SCCmec type IV and ST8-SCCmec type IV in Belgium (9), ST22-SCCmec type IV in the United Kingdom (13), ST225-SCCmec type I and ST22-SCCmec type IV in Germany (27), ST228-SCCmec type I in Italy (7), and ST125-SCCmec type IV in Spain (4). No isolates belonging to these different clones were isolated in our study, and conversely, the Lyon clone seems to be infrequent in these countries (except in Belgium, where the Lyon clone shared the first place with ST45-SCCmec type IV (37% and 34% of all MRSA isolates, respectively) (9). Possible explanations are geographic segregation and/or differences in antimicrobial chemotherapy or antisepsis. In the same way, we confirm the complete disappearance of the gentamicin-resistant Iberian clone (ST247-SCCmec type I, spa t008, and related) that was by far the most-frequent French clone in the 1990s (5, 28) and its replacement by the Lyon clone. Several similar reports have been published, with the Iberian clone in a hospital setting in two cases (2, 38) or with other epidemic clones (3, 6). Various genetic factors have been proposed to explain such rapid evolution and the dissemination of particular epidemic clones. One characteristic of the Lyon clone is the presence of sea (87% of the isolates), and it was recently demonstrated that this gene is part of an immune evasion cluster carried by a phage and harboring a collection of virulence factors able to modulate the human immune system, namely SEA, SCIN (staphylococcal complement inhibitor), CHIPS (chemotaxis inhibitory protein of S. aureus), and SAK (staphylokinase) (44). This pathogenicity island could be involved in the success of the Lyon clone and in its ability to cause invasive infections. Finally, it must be noted that the two major clones isolated during this study, the Lyon clone and the “classical subtype” of the Pediatric clone, are both typically HA-MRSA (16, 34, 40), although they harbor SCCmec type IV that is usually considered a CA-MRSA marker.
We found that variable traits, such as toxin production and antibiotic susceptibility encoded by mobile genetic elements, were more variable than expected. Care should thus be taken when using such characteristics to define or even to identify MRSA clones circulating in a given area. However, they could be useful for monitoring the evolution of these clones and their potent pathogenicity profiles and for adapting empirical antimicrobial chemotherapy.
Finally, the results of this study indicate the emergence and spread of new MRSA clones in France, namely, the Geraldine clone, the European ST80 clone, and the “new” Pediatric clone. The dissemination of clones producing PVL has been extensively reported, but the emergence of a tst-positive MRSA clone is new. The spread of such clones with potent superantigenic activity (TSST-1) or the capacity to cause invasive disease (through PVL production) is of major concern. Even if their prevalence is currently low, the possibility of rapid spread, as recently reported for the USA300 clone, should be kept in mind. These clones with enhanced virulence thus represent a new threat in terms of pathogenicity, treatment, and the prevention of transmission and should be closely monitored in coming years.
FIG. 1.
Geographical distribution of the 23 French hospitals that participated in this study.
Acknowledgments
We thank our colleagues who sent us French MRSA isolates from the indicated towns: H. Chardon (Aix en Provence), D. Pierrejean (Auch), G. Julienne (Belfort), C. Fabe (Bergerac), C. Moratte (Bordeaux), G. Lelay (Brest), N. Wilheim (Cahors), F. Beisse (Cherbourg), C. Solere (Clamart), R. Bonnet (Clermont Ferrand), C. Branger (Colombes), D. Jan (Laval), A. Marmonnier (Le Mans), A. Decoster (Lomme), S. Vedy (Marseille), J. Puyhardy (Metz), J. M. Delarbre (Mulhouse), E. Lecaillon (Perpignan), V. Vernet (Reims), P. Y. Donnio (Rennes), P. Rousselier (Salon de Provence), and J. D. Cavallo (Saint Mande). We thank C. Courtier, C. Gardon, C. Spinelli, C. Bouveyron, A. Martra, and M. Rougier for technical help and David Young for editorial assistance.
This work was part of a larger European study (EARSS) coordinated by Hajo Grundmann, to whom we are grateful.
Footnotes
Published ahead of print on 30 July 2008.
REFERENCES
- 1.Aires de Sousa, M., and H. de Lencastre. 2004. Bridges from hospitals to the laboratory: genetic portraits of methicillin-resistant Staphylococcus aureus clones. FEMS Immunol. Med. Microbiol. 40101-111. [DOI] [PubMed] [Google Scholar]
- 2.Amorim, M. L., M. Aires de Sousa, I. S. Sanches, R. Sa-Leao, J. M. Cabeda, J. M. Amorim, and H. de Lencastre. 2002. Clonal and antibiotic resistance profiles of methicillin-resistant Staphylococcus aureus (MRSA) from a Portuguese hospital over time. Microb. Drug Resist. 8301-309. [DOI] [PubMed] [Google Scholar]
- 3.Amorim, M. L., N. A. Faria, D. C. Oliveira, C. Vasconcelos, J. C. Cabeda, A. C. Mendes, E. Calado, A. P. Castro, M. H. Ramos, J. M. Amorim, and H. de Lencastre. 2007. Changes in the clonal nature and antibiotic resistance profiles of methicillin-resistant Staphylococcus aureus isolates associated with spread of the EMRSA-15 clone in a tertiary care Portuguese hospital. J. Clin. Microbiol. 452881-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Argudin, M. A., C. Mendoza, F. Vazquez, M. C. Martin, and M. R. Rodicio. 2008. Diversity of the virulence and genomic backgrounds in clinical isolates of Staphylococcus aureus collected in a Spanish hospital 1992 to 2006, abstr. P1409, p.126. Abstr. 18th Eur. Congr. Clin. Microbiol. Infect. Dis.
- 5.Aubry-Damon, H., P. Legrand, C. Brun-Buisson, A. Astier, C. J. Soussy, and R. Leclercq. 1997. Reemergence of gentamicin-susceptible strains of methicillin-resistant Staphylococcus aureus: roles of an infection control program and changes in aminoglycoside use. Clin. Infect. Dis. 25647-653. [DOI] [PubMed] [Google Scholar]
- 6.Aucken, H. M., M. Ganner, S. Murchan, B. D. Cookson, and A. P. Johnson. 2002. A new UK strain of epidemic methicillin-resistant Staphylococcus aureus (EMRSA-17) resistant to multiple antibiotics. J. Antimicrob. Chemother. 50171-175. [DOI] [PubMed] [Google Scholar]
- 7.Campanile, F., D. Bongiorno, S. Borbone, G. Mongelli, S. Jeddari, and S. Stefani. 2008. Looking back, current status, and future trends of MRSA clones in Italy, abstr. P-1426, p. 127. Abstr. 18th Eur. Congr. Clin. Microbiol. Infect. Dis.
- 8.Chongtrakool, P., T. Ito, X. X. Ma, Y. Kondo, S. Trakulsomboon, C. Tiensasitorn, M. Jamklang, T. Chavalit, J.-H. Song, and K. Hiramatsu. 2006. Staphylococcal cassette chromosome mec (SCCmec) typing of methicillin-resistant Staphylococcus aureus strains isolated in 11 Asian countries: a proposal for a new nomenclature for SCCmec elements. Antimicrob. Agents Chemother. 501001-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delplano, A., O. Denis, M. Hallin, S. Rottiers, R. De Ryck, E. Hendrickx, H. Grundmann, and M. J. Struelens. 2008. Clonal distribution of methicillin-resistant and susceptible Staphylococcus aureus invasive isolates in Belgium, EARSS/SeqNet study, 2006-2007, abstr. P-1431, p.127. Abstr. 18th Eur. Congr. Clin. Microbiol. Infect. Dis.
- 10.Denis, O., A. Deplano, H. De Beenhouwer, M. Hallin, G. Huysmans, M. G. Garrino, Y. Glupczynski, X. Malaviolle, A. Vergison, and M. J. Struelens. 2005. Polyclonal emergence and importation of community-acquired methicillin-resistant Staphylococcus aureus strains harboring Panton-Valentine leucocidin genes in Belgium. J. Antimicrob. Chemother. 561103-1106. [DOI] [PubMed] [Google Scholar]
- 11.Dohin, B., Y. Gillet, R. Kohler, G. Lina, F. Vandenesch, P. Vanhems, D. Floret, and J. Etienne. 2007. Pediatric bone and joint infections caused by Panton-Valentine leukocidin-positive Staphylococcus aureus. Pediatr. Infect. Dis. J. 261042-1048. [DOI] [PubMed] [Google Scholar]
- 12.Durand, G., M. Bes, H. Meugnier, M. C. Enright, F. Forey, N. Liassine, A. Wenger, K. Kikuchi, G. Lina, F. Vandenesch, and J. Etienne. 2006. Detection of new methicillin-resistant Staphylococcus aureus clones containing the toxic shock syndrome toxin 1 gene responsible for hospital- and community-acquired infections in France. J. Clin. Microbiol. 44847-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellington, M. J., I. McCormick Smith, M. Warner, M. Ganner, B. D. Cookson, R. L. Hill, A. P. Johnson, and A. M. Kearns. 2008. EARRS-SEQNET surveillance of S. aureus associated with bacteraemia in the UK during 2006, abstr. P-1418, p.126. Abstr. 18th Eur. Congr. Clin. Microbiol. Infect. Dis.
- 14.Enright, M. C., N. P. Day, C. E. Davies, S. J. Peacock, and B. G. Spratt. 2000. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 381008-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faria, N. A., J. A. Carrico, D. C. Oliveira, M. Ramirez, and H. de Lencastre. 2008. Analysis of typing methods for epidemiological surveillance of both methicillin-resistant and methicillin-susceptible Staphylococcus aureus strains. J. Clin. Microbiol. 46136-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferry, T., M. Bes, O. Dauwalder, H. Meugnier, G. Lina, F. Forey, F. Vandenesch, and J. Etienne. 2006. Toxin gene content of the Lyon methicillin-resistant Staphylococcus aureus clone compared with that of other pandemic clones. J. Clin. Microbiol. 442642-2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.French Society for Microbiology. 2007. Recommandations du Comité de l'Antibiogramme de la Société Française de Microbiology. http://www.sfm.asso.fr/nouv/general.php?pa=2.
- 18.Gillet, Y., B. Issartel, P. Vanhems, J. C. Fournet, G. Lina, M. Bes, F. Vandenesch, Y. Piemont, N. Brousse, D. Floret, and J. Etienne. 2002. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359753-759. [DOI] [PubMed] [Google Scholar]
- 19.Gomes, A. R., I. S. Sanches, M. Aires de Sousa, E. Castaneda, and H. de Lencastre. 2001. Molecular epidemiology of methicillin-resistant Staphylococcus aureus in Colombian hospitals: dominance of a single unique multidrug-resistant clone. Microb. Drug Resist. 723-32. [DOI] [PubMed] [Google Scholar]
- 20.Hanssen, A. M., and J. U. Sollid. 2007. Multiple staphylococcal cassette chromosomes and allelic variants of cassette chromosome recombinases in Staphylococcus aureus and coagulase-negative staphylococci from Norway. Antimicrob. Agents Chemother. 511671-1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heusser, R., M. Ender, B. Berger-Bachi, and N. McCallum. 2007. Mosaic staphylococcal cassette chromosome mec containing two recombinase loci and a new mec complex, B2. Antimicrob. Agents Chemother. 51390-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes, A., M. Ganner, S. McGuane, T. L. Pitt, B. D. Cookson, and A. M. Kearns. 2005. Staphylococcus aureus isolates carrying Panton-Valentine leucocidin genes in England and Wales: frequency, characterization, and association with clinical disease. J. Clin. Microbiol. 432384-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holtfreter, S., D. Grumann, M. Schmudde, H. T. Nguyen, P. Eichler, B. Strommenger, K. Kopron, J. Kolata, S. Giedrys-Kalemba, I. Steinmetz, W. Witte, and B. M. Broker. 2007. Clonal distribution of superantigen genes in clinical Staphylococcus aureus isolates. J. Clin. Microbiol. 452669-2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ito, T., Y. Katayama, K. Asada, N. Mori, K. Tsutsumimoto, C. Tiensasitorn, and K. Hiramatsu. 2001. Structural comparison of three types of staphylococcal cassette chromosome mec integrated in the chromosome in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 451323-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jarraud, S., C. Mougel, J. Thioulouse, G. Lina, H. Meugnier, F. Forey, X. Nesme, J. Etienne, and F. Vandenesch. 2002. Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect. Immun. 70631-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kondo, Y., T. Ito, X. X. Ma, S. Watanabe, B. N. Kreiswirth, J. Etienne, and K. Hiramatsu. 2007. Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob. Agents Chemother. 51264-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kresken, M., J. Brauers, B. Strommenger, and W. Witte. 2008. Spread of MRSA clones in German hospitals and in vitro activity of tigecycline, abstr. P-1433, p.127. Abstr. 18th Eur. Congr. Clin. Microbiol. Infect. Dis.
- 28.Lelievre, H., G. Lina, M. E. Jones, C. Olive, F. Forey, M. Roussel-Delvallez, M. H. Nicolas-Chanoine, C. M. Bebear, V. Jarlier, A. Andremont, F. Vandenesch, and J. Etienne. 1999. Emergence and spread in French hospitals of methicillin-resistant Staphylococcus aureus with increasing susceptibility to gentamicin and other antibiotics. J. Clin. Microbiol. 373452-3457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lina, G., G. Durand, C. Berchich, B. Short, H. Meugnier, F. Vandenesch, J. Etienne, and M. C. Enright. 2006. Staphylococcal chromosome cassette evolution in Staphylococcus aureus inferred from ccr gene complex sequence typing analysis. Clin. Microbiol. Infect. 121175-1184. [DOI] [PubMed] [Google Scholar]
- 30.Ma, X. X., T. Ito, C. Tiensasitorn, M. Jamklang, P. Chongtrakool, S. Boyle-Vavra, R. S. Daum, and K. Hiramatsu. 2002. Novel type of staphylococcal cassette chromosome mec identified in community-acquired methicillin-resistant Staphylococcus aureus strains. Antimicrob. Agents Chemother. 461147-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maier, J., H. Melzl, U. Reischl, I. Drubel, W. Witte, N. Lehn, and H. Linde. 2005. Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus in Germany associated with travel or foreign family origin. Eur. J. Clin. Microbiol. Infect. Dis. 24637-639. [DOI] [PubMed] [Google Scholar]
- 32.McDougal, L. K., C. D. Steward, G. E. Killgore, J. M. Chaitram, S. K. McAllister, and F. C. Tenover. 2003. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: establishing a national database. J. Clin. Microbiol. 415113-5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oliveira, D. C., and H. de Lencastre. 2002. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 462155-2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oliveira, D. C., C. Milheirico, and H. de Lencastre. 2006. Redefining a structural variant of staphylococcal cassette chromosome mec, SCCmec type VI. Antimicrob. Agents Chemother. 503457-3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oliveira, D. C., A. Tomasz, and H. de Lencastre. 2001. The evolution of pandemic clones of methicillin-resistant Staphylococcus aureus: identification of two ancestral genetic backgrounds and the associated mec elements. Microb. Drug Resist. 7349-361. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira, D. C., A. Tomasz, and H. de Lencastre. 2002. Secrets of success of a human pathogen: molecular evolution of pandemic clones of methicillin-resistant Staphylococcus aureus. Lancet Infect. Dis. 2180-189. [DOI] [PubMed] [Google Scholar]
- 37.Peacock, S. J., C. E. Moore, A. Justice, M. Kantzanou, L. Story, K. Mackie, G. O'Neill, and N. P. Day. 2002. Virulent combinations of adhesin and toxin genes in natural populations of Staphylococcus aureus. Infect. Immun. 704987-4996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perez-Roth, E., F. Lorenzo-Diaz, N. Batista, A. Moreno, and S. Mendez-Alvarez. 2004. Tracking methicillin-resistant Staphylococcus aureus clones during a 5-year period (1998 to 2002) in a Spanish hospital. J. Clin. Microbiol. 424649-4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robert, J., J. Etienne, and X. Bertrand. 2005. Methicillin-resistant Staphylococcus aureus producing Panton-Valentine leukocidin in a retrospective case series from 12 French hospital laboratories, 2000-2003. Clin. Microbiol. Infect. 11585-587. [DOI] [PubMed] [Google Scholar]
- 40.Sá-Leão, R., I. Santos Sanches, D. Dias, I. Peres, R. M. Barros, and H. de Lencastre. 1999. Detection of an archaic clone of Staphylococcus aureus with low-level resistance to methicillin in a pediatric hospital in Portugal and in international samples: relics of a formerly widely disseminated strain? J. Clin. Microbiol. 371913-1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takano, T., W. Higuchi, T. Otsuka, T. Baranovich, S. Enany, K. Saito, H. Isobe, S. Dohmae, K. Ozaki, M. Takano, Y. Iwao, M. Shibuya, T. Okubo, S. Yabe, D. Shi, I. Reva, L. J. Teng, and T. Yamamoto. 2008. Novel characteristics of community-acquired methicillin-resistant Staphylococcus aureus strains belonging to multilocus sequence type 59 in Taiwan. Antimicrob. Agents Chemother. 52837-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tristan, A., M. Bes, H. Meugnier, G. Lina, B. Bozdogan, P. Courvalin, M. E. Reverdy, M. C. Enright, F. Vandenesch, and J. Etienne. 2007. Global distribution of Panton-Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus, 2006. Emerg. Infect. Dis. 13594-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tristan, A., L. Ying, M. Bes, J. Etienne, F. Vandenesch, and G. Lina. 2003. Use of multiplex PCR to identify Staphylococcus aureus adhesins involved in human hematogenous infections. J. Clin. Microbiol. 414465-4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van Wamel, W. J., S. H. Rooijakkers, M. Ruyken, K. P. van Kessel, and J. A. van Strijp. 2006. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J. Bacteriol. 1881310-1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Witte, W., C. Braulke, C. Cuny, B. Strommenger, G. Werner, D. Heuck, U. Jappe, C. Wendt, H. J. Linde, and D. Harmsen. 2005. Emergence of methicillin-resistant Staphylococcus aureus with Panton-Valentine leukocidin genes in central Europe. Eur. J. Clin. Microbiol. Infect. Dis. 241-5. [DOI] [PubMed] [Google Scholar]