Abstract
Study objectives
To examine the proportion of the recent decline in coronary heart disease (CHD) deaths in Ireland attributable to (a) “evidence based” medical and surgical treatments, and (b) changes in major cardiovascular risk factors.
Design setting
IMPACT, a previously validated model, was used to combine and analyse data on the use and effectiveness of specific cardiology treatments and risk factor trends, stratified by age and sex. The main data sources were published trials and meta‐analyses, official statistics, clinical audits, and observational studies.
Results
Between 1985 and 2000, CHD mortality rates in Ireland fell by 47% in those aged 25–84. Some 43.6% of the observed decrease in mortality was attributed to treatment effects and 48.1% to favourable population risk factor trends; specifically declining smoking prevalence (25.6%), mean cholesterol concentrations (30.2%), and blood pressure levels (6.0%), but offset by increases in adverse population trends related to obesity, diabetes, and inactivity (−13.8%).
Conclusions
The results emphasise the importance of a comprehensive strategy that maximises population coverage of effective treatments, and that actively promotes primary prevention, particularly tobacco control and a cardioprotective diet.
Keywords: coronary heart disease, mortality, Ireland, risk factor, treatment
Coronary heart disease (CHD) remains a leading cause of death and disability in Ireland, and mortality rates are still among the highest in Europe.1 However, CHD mortality rates have halved since the mid‐1980s, with steeper falls in younger age groups. This resulted in about 3765 fewer deaths in 2000 compared with 1985 in Ireland.1,2 The multinational MONICA study suggested that in countries with falling CHD mortality rates, about one third of the fall was attributable to improved case fatality (mostly treatment related) and two thirds to a reduction in event incidence (mostly attributable to risk factor reductions).3,4 It would be of benefit to determine the components that have resulted in the biggest decreases in mortality, to guide policy in the prevention of CHD, focus health promotion strategies, and target resources towards the most effective interventions in the populations with the greatest need.
Since 1996, Capewell and colleagues have progressively developed and refined a CHD mortality model called IMPACT.5,6,7 This model has been used to explore trends in CHD mortality in contrasting countries, and to comprehensively assess the potential contribution of cardiology treatments and risk factor changes. The model was validated against the actual CHD mortality falls seen in Scotland, England, New Zealand, and Finland5,6,7,8 before being used to assess substantial mortality increases seen in China.9 Results using the IMPACT model were generally consistent with other studies using diverse methodologies in different countries including the USA, New Zealand, Finland, and the Netherlands.10,11,12,13
This study aimed to use the IMPACT CHD model to examine the CHD mortality fall in Ireland between 1985 and 2000, and to determine how much of this fall could be attributed to “evidence based” medical and surgical treatments, and how much to changes in major cardiovascular risk factors.
Methods
The IMPACT model
The cell based mortality model in Microsoft Excel has been described in detail elsewhere.6 In brief, the number of CHD deaths prevented or postponed by each specific cardiac intervention and by each risk factor change was calculated for Ireland for the base year 1985, and again for the year 2000.
We identified and incorporated data for men and women aged 25 to 84 years in the Irish population of 3.8 million, stratified by age and sex, detailing:
CHD patient numbers, (ICD 9 codes 410–414) categorised by disease subgroup
Use of specific medical and surgical treatments,
Population trends in major cardiovascular risk factors (smoking, total cholesterol, hypertension, obesity, diabetes, and physical inactivity),
Effectiveness of specific cardiology treatments
Effectiveness of specific risk factor reductions.
All public and private patients were included. Those aged 85 years or over were excluded from the model, because of uncertainties regarding death certification accuracy.
Identification and assessment of relevant data (tables 1, 2)
Table 1 Deaths prevented or postponed by medical and surgical treatments in Ireland in 2000.
| Treatments | Number of eligible patients* | % Eligible patients treated† | Absolute risk reduction | Best estimate (number) | Best estimate (%) |
|---|---|---|---|---|---|
| Acute myocardial infarction (AMI) | 3970 | 166‡ | 4.4‡ | ||
| Community resuscitation | 49 | 0.110 | 12 | 0.3 | |
| Hospital resuscitation | 99 | 0.213 | 32 | 0.9 | |
| Thrombolysis | 39‡‡ | 0.038 | 60 | 1.6 | |
| Aspirin | 61‡‡ | 0.031 | 79 | 2.1 | |
| Primary angioplasty | 4‡‡ | 0.056 | 8 | 0.2 | |
| β blockers | 33 | 0.008 | 11 | 0.3 | |
| ACE inhibitors | 19‡‡ | 0.001 | 11 | 0.3 | |
| Total secondary prevention | 678§ | 18.0§ | |||
| Secondary prevention after infarction | 37245 | 449¶ | 11.9¶ | ||
| Aspirin | 64‡‡ | 0.010 | 127 | 3.4 | |
| β blockers | 33 | 0.012 | 92 | 2.4 | |
| ACE inhibitors | 21‡‡ | 0.012 | 53 | 1.4 | |
| Statins | 37‡‡ | 0.015 | 83 | 2.2 | |
| Warfarin | 4 | 0.008 | 9 | 0.2 | |
| Rehabilitation | 51 | 0.014 | 87 | 2.3 | |
| Secondary prevention after revascularisation | 24438 | 0.028 | 229** | 6.1** | |
| Chronic angina | 317 | 8.4 | |||
| CABG surgery | 18990 | 100 | 0.009 | 144 | 3.8 |
| Angioplasty | 11023 | 100‡‡ | 0.005 | 45 | 1.2 |
| Community angina (aspirin+statin) | 78873 | 75‡‡ | 0.002 | 128 | 3.4 |
| Unstable angina | 2432 | 33 | 0.9 | ||
| Aspirin and heparin | 59‡‡ | 0.012 | 17 | 0.5 | |
| Aspirin alone | 30‡‡ | 0.013 | 8 | 0.2 | |
| Platelet IIB/IIIA inhibitors | 48‡‡ | 0.007 | 8 | ||
| Heart failure | – | 340 | 9.1 | ||
| Hospital | 1715 | 28‡‡ | – | 150 | |
| Community | 12940 | 56‡‡ | 190 | 5.1 | |
| Hypertension treatment | 705648 | 37 | 0.001 | 59 | 1.6 |
| Statins for primary prevention | 915169 | 6‡‡ | 0.001 | 46 | 1.2 |
| Total treatment effects in 2000 | 1639/3763†† | 43.6 |
*Based on Hospital‐In‐Patient Enquiry, Central Statistics Office, and General Medical Payments Databases for the year 2000 only.23 †Treatment uptakes are weighted to sex and age groups by the year of death, and therefore not consistent with values in appendix III, and appendix III identifies the sources of treatment uptakes in Ireland for the year 2000 only. ‡This value does not include the additional 47 AMI deaths attributable to treatment effect of 1985. §This value equates to ¶ and ** together and does not include two additional deaths attributable to treatment effect of 1985. ††3763 is total observed fewer CHD deaths in 2000, and 1639 sums up all the individual bold font values. ‡‡These treatments were not generally available in 1985.
Table 2 Deaths prevented or postponed as a result of population risk factor changes in Ireland.
| Risk factors | Relative changes in risk factor* | β regression coefficients | Deaths prevented or postponed | |
|---|---|---|---|---|
| (%) | (%) | (number) | (%) | |
| Positive trends | ||||
| Smoking | −14.2† | 0.51 | 964 | 25.6 |
| Cholesterol | −4.6‡ | 2.46 | 1135 | 30.2 |
| Population BP | −7.2§ | 1.67 | 228 | 6.1 |
| Subtotals | +2327 | +61.9 | ||
| Adverse trends | ||||
| Relative risk | ||||
| Physical inactivity | +4.8¶ | 0.50 | −154 | −4.1 |
| Obesity | +195.1** | 1.57 | −131 | −3.5 |
| Diabetes | +48.0†† | 4.24 | −232 | −6.2 |
| Subtotals | −517 | −13.8 | ||
| Total risk factor effects in 2000 | 1810/3763‡‡ | +48.1 | ||
*Ratio of the absolute difference between 1985 and 2000 to the baseline year (1985), and then weighted to age and sex specific populations. †Smoking prevalence: 1985 (33.6%) and 2000 (28.8%). ‡Total mean cholesterol levels: 1985 (6.02 mmol/l) and 2000 (5.73 mmol/l). §Mean diastolic blood pressure levels: 1985 (81 mm Hg) and 2000 (75 mm Hg). ¶No Irish data available, so based on the UK prevalence data. **Obesity prevalence: 1985 (8%) and 2000 (24%). ††Diabetes prevalence: 1985 (1.7%) and 2000 (2.5%). ‡‡3763 is total observed CHD deaths in 2000, and 1810 is the sum of +2327 and −517 deaths.
Information was obtained from routine health statistics, mainly the Public Health Information System (PHIS),14 available from the Department of Health and Children, Ireland; the Hospital Inpatient Enquiry (HIPE) system available from the Economic and Social Research Institute15; and other surveys.16,17 However, HIPE data do not differentiate between first and recurrent events. Prescription data were obtained from the General Medical Services (GMS) payments board (http://www.gmspb.ie) and risk factor data from two population studies, the Kilkenny health project and the Cork and Kerry diabetes and heart disease study.18,19 Data on the effectiveness of therapeutic interventions and the mortality reduction from specific population cardiovascular risk factor changes came from published randomised controlled trials, meta‐analyses, and cohort studies.20,21,22 Further details on the identification and assessment of the relevant data can be found in appendices I‐III on the IMPACT web site.23
The fall in coronary heart disease deaths
The number of CHD deaths expected in 2000 if the mortality rates in 1985 had persisted was calculated by indirect age standardisation, using 1985 as the base year. The CHD deaths actually seen in 2000 were then subtracted to give the decrease in CHD deaths in 2000 compared with 1985 (3763 fewer deaths).
The model aimed to include all known medical and surgical treatments in 1985 and 2000. These interventions are listed in table 1, and included all the interventions considered in earlier versions of the IMPACT model, plus primary angioplasty including stenting for myocardial infarction, statins for primary prevention, platelet IIB/IIIA inhibitors and clopidogrel for unstable angina, plus spironolactone and β blockers for heart failure (table 1).
The mortality reduction for each treatment was calculated using the relative mortality reduction reported in published meta‐analyses and trials applied to the age specific case‐fatality rate seen in large unselected patient cohorts.6
Polypharmacy issues
The potential effect of multiple treatments in an individual patient was examined using the Mant and Hicks cumulative relative benefit approach24:
Relative benefit = 1 − [(1−treatment A) × (1−treatment B) × … etc
Potential overlaps between patient groups
Patient groups are seldom mutually exclusive. For example, about half the patients having CABG surgery have had a previous myocardial infarction, and about one fifth of myocardial infarction survivors develop clinical heart failure within 12 months. To avoid double counting, potential overlaps between different groups of patients were identified and adjustments were made using previously established methods.23
Treatment compliance
Compliance or concordance, the proportion of treated patients actually taking therapeutically effective levels of medication, was based on recent studies where available. The IMPACT model default assumptions for compliance were 100% in hospital patients, 70% in symptomatic community patients, and 50% in asymptomatic community patients.25
Deaths prevented or postponed
A number of effective therapies were already in limited use in 1985. These included CABG surgery, cardiopulmonary resuscitation, β blockers for acute myocardial infarction (AMI), diuretics for acute left ventricular heart failure, and therapy for moderate and severe hypertension (then defined as a diastolic blood pressure >105 mm Hg). Patient data for most of these interventions, such as CABG surgery, and eligible hypertensives, were obtained from the data sources detailed above.
Risk factor trends and mortality benefits
Data on risk factors were obtained for the years 1985 and 2000 only.
(a) Regression coefficients
For risk factor changes, the model uses multiple regression (β) coefficients obtained from meta‐analyses, large cohort studies, and MONICA analyses. Each β coefficient quantifies the independent relation between population change in a specific CHD risk factor, (such as smoking, cholesterol, or blood pressure) and the consequent change in population mortality rate from CHD using multiple regression analysis. These coefficients were recently reviewed and updated.6,20,21,22
The subsequent reduction in deaths produced by the fall in each major risk factor was then estimated as the product of three variables: the number of CHD deaths seen in the base year (1985), the relative reduction in that risk factor, and the β coefficient.
(b) Population attributable risk fraction
Given the absence of suitable β coefficients for obesity, diabetes, and physical activity, a separate, previously validated method was used. This was based on population attributable risk fraction (PARF), calculated using the conventional formula.6,23
The number of CHD deaths attributable to each specific risk factor was calculated for 1985 and for 2000. The difference between the two values then represented the deaths prevented or postponed because of the change in the risk factor in the population.
Model validation: comparison with observed mortality falls
The model estimate for the total deaths prevented or postponed by all treatments plus all risk factor changes was then summed and compared with the observed falls in mortality for men and women in each specific age‐sex group. On an a priori basis, any shortfall in the overall model estimate was then formally attributed to other, unmeasured and unidentified risk factors. In other industrialised countries, this has ranged from 3% to 9%.5,8
Sensitivity analyses
Because of the uncertainties surrounding many of the values, a multiway sensitivity analysis was performed using the analysis of extremes method.26 (Illustrative examples of specific analyses and calculations are shown in the appendices of the recent England and Wales model publication,6 and on the IMPACT web site23). This method does not entail any probabilistic interpretation as in confidence interval estimation.
Results
Between 1985 and 2000, CHD mortality rates in Ireland fell by 47% in men and in women aged 25–84. This resulted in 3763 fewer “observed” deaths in 2000 compared with the expected number given the rates in 1985 (8681 expected minus 4918 observed). Overall, the IMPACT model predicted 3449 fewer deaths, about 92% of the observed CHD mortality fall (93% in men and 88% in women). The remaining 8% of the mortality fall was attributed to other, unmeasured factors.
Medical and surgical treatments
Medical and surgical treatments together prevented or postponed about 1640 deaths (minimum estimate, 790; maximum estimate, 3150; table 1). This represented 43.6% of the total mortality decrease, after allowance for treatments applied in 1985 (table 1). Substantial contributions came from specific treatments for secondary prevention, heart failure and angina.
About 166 deaths were prevented or postponed by treatments for AMI in 2000 when an additional 47 AMI deaths were accounted for because of the treatment effect of 1985; the biggest contributions came from cardiopulmonary resuscitation (CPR), aspirin, and thrombolysis (table 1). CABG surgery and angioplasty were estimated to explain about 5% of the total mortality fall (table 1).
Adjustment for polypharmacy in individual patients
Applying the Mant and Hicks equation to the uptake of multiple medications in individual patients would have reduced the total deaths prevented or postponed by about 157 (14 in AMI, 56 in heart failure patients, and 87 in secondary prevention).24
Major cardiovascular risk factors
Changes in the major cardiovascular risk factors together produced a best estimate of 1810 fewer deaths (minimum estimate, 1505; maximum, 2425; table 2). This therefore accounted for 48.1% of the total mortality decrease between 1985 and 2000. The biggest contribution came from the decreases in serum total cholesterol levels, and reductions in smoking and blood pressure levels (table 2). Adverse trends were seen for physical activity, obesity, and diabetes; they together caused about 517 additional CHD deaths (table 2). The prevalence of obesity increased by 195% and diabetes prevalence increased by 48%. Indirect evidence suggested a 5% decrease in physical activity (table 2).
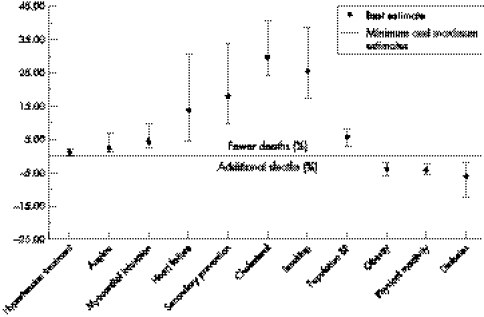
Sensitivity analyses, validation, and model fit
Figure 1 shows the results of the sensitivity analysis. Proportional contributions of specific treatments and risk factor changes to the CHD mortality reduction in Ireland are presented as best estimate, plus minimum and maximum estimates. The proportionate contribution of specific treatments and risk factor changes to the overall decrease in CHD mortality in Ireland between 1985 and 2000 remained comparatively consistent. For instance, considering the initial treatments of AMI, the best estimates were 4.4%, the minimum contribution was 2.5%, and the maximum 9.8%. Similarly, for risk factors, the best estimate for smoking for instance, was 25.6%, the minimum was 17.7%, and the maximum estimate was 38.3% (table 2).
Figure 1 Proportional contributions of specific treatments and risk factor changes to the CHD mortality reduction in Ireland: results of a sensitivity analysis.
Figure 2 shows the validation of the IMPACT model. The model estimates suggest a good fit with the observed CHD deaths across all age groups in both sexes.
Figure 2 Observed compared with model CHD deaths by sex and age groups.
Discussion
CHD mortality rates in Ireland halved between 1985 and 2000, with 3673 fewer observed CHD deaths in 2000. About 44% of this decrease was attributable to the combined effects of modern cardiology treatments and 48% to reduction in major risk factors, particularly smoking and cholesterol levels. Changes in the three classic cardiovascular risk factors (smoking, cholesterol, and blood pressure) contributed 61.9% of the total CHD mortality decrease, which is also consistent with studies in other developed countries6,7,8; where at least 80% of major CHD events in men can be attributed to these factors.27 The multinational MONICA study likewise suggested that about one third of the fall was attributable to improved case fatality (mostly treatment related) and two thirds to a reduction in event incidence (mostly attributable to risk factor reductions).3,4 This contribution is crucial, and current health promotion activities and public health policies are targeted at reducing these risk factors in the Irish population.
What this paper adds
About 44% of the decline in coronary heart disease mortality in Ireland can be attributed to medical treatments, particularly secondary preventative therapies and treatment of heart failure. Around 48% of the fall is attributable to changes in risk factors including substantial reductions in smoking and cholesterol, but offset by increases in obesity, diabetes, and physical inactivity.
What is already known
Two thirds of deaths due to cardiovascular disease can be attributed to three main risk factors; smoking, blood pressure, and cholesterol levels.
Risk factors
A significant contribution of the reduction in mortality attributable to risk factors reflected a moderate decrease in smoking prevalence, from 34% to 29% (a 5% absolute risk reduction). However, almost 30% of the mortality decrease came from a comparatively small reduction (4.6%) in population total cholesterol level. This is consistent with progressively healthier eating patterns among the general Irish population over the past decade. Furthermore, small cholesterol changes have big effects as recent meta‐analysis have shown.28,29 A recent Chinese study suggested that a 1 mmol/l rise in total cholesterol level was responsible for a 37% increase in CHD mortality,9 which has been replicated in the Asia Pacific cohort studies collaboration meta‐analyses.29 This emphasises the consistently large β coefficient quantified by Law and colleagues, (5.4 to 1.9 according to age,22 more recently 5.6 to 3.1 by age28), and highlights the potential gains that would come from more substantial cholesterol reductions in Ireland.
The smaller smoking contribution in Ireland may principally reflect the comparatively slow decline in Irish smoking prevalence between 1985–2000, averaging 14%, (half that seen in the UK and New Zealand over the same period).6,7 However, there is evidence of a steeper decline in smoking prevalence after the successful implementation of a ban on smoking in the workplace in Ireland in 2004.30
The adverse trends in obesity, diabetes, and physical inactivity together contributed over 500 additional deaths in 2000. These cancelled out over half the benefit from 15 years of cholesterol improvement. Furthermore, continuing deteriorations are expected, given the rising prevalence of childhood and adult obesity suggested by recent health and lifestyle surveys in Ireland, as elsewhere.31 In the Asia Pacific cohort studies collaboration a 2 kg/m2 reduction in population BMI decreased CHD risk by 11%.32
Policy implications
These results have major public health implications, particularly in relation to supporting the recent workplace smoking ban introduced in Ireland in March 2004.
We used comparatively conservative regression β coefficients for smoking (0.51), cholesterol (2.46), and blood pressure (1.67). All the β coefficients and relative risk values used in the model were independent, being obtained from multiple regression analyses. The interactions between the major risk factors should therefore have been accounted for. However, there may still be some overestimation as only a limited range of risk factors were used in the study. The MONICA study, for example, included smoking (yes or no), systolic blood pressure, total cholesterol, and body mass index.3
There was comparatively little space left in the model, for potential mortality benefits from other, unquantified factors, barely 8%. These other factors include deprivation, dietary consumption of fish oils, antioxidants, and alcohol, and life course factors. However, these and other novel risk factors such as homocysteine, apolipoprotein B, and C reactive protein are likely to be highly correlated with the major risk factors already included, and their independent contribution to future decline in CHD mortality may be modest.27 Some or all may thus contribute to the 8% of the mortality fall not explained by the model.
Interventions
Revascularisation by CABG surgery or angioplasty accounted for only 5% of the total mortality decrease, much as in Britain and the USA.6,10 This is a disappointingly small contribution given the large financial resources allocated to these interventions.33
The most substantial contributions in mortality decline attributable to treatments came from secondary prevention and heart failure treatments. However, although heart failure treatments resulted in over 300 (9%) of deaths prevented or postponed, this would gain few additional life years because of the comparatively short life expectancy in these patients.
Similarly, thrombolysis accounted for only about 1.6% of the deaths prevented or postponed. By contrast, aspirin therapy for patients with angina in the community (2.2%) prevented more than twice as many deaths as did treatment for unstable angina patients in hospitals (0.9%), principally reflecting the greater numbers involved (table 1).
Treatment uptake levels (the proportion of eligible patients actually receiving appropriate therapies) were variable and sometimes poor. Earlier work suggested that if even 80% of eligible patients had received appropriate therapy, about 21 000 additional deaths might have been prevented or postponed each year in England and Wales,34 equivalent to almost 2000 fewer deaths in Ireland.
In a previous study in 2002, we found that the uptake of statin therapy in those with established heart disease or diabetes was low at 44%.35 Encouragingly however, in a recently published report from the Irish Heartwatch programme, enrolling 10 500 patients with established CHD onto a primary care database, almost 74% were on some lipid lowering therapy at their first visit and 84% by their fourth visit.36
Limitations of the study
This study focused on the number of deaths rather than events incidence or improvements in case fatality.5,6 There are obvious limitations with this type of modelling study. It is very dependent on the quality and extent of data available on CHD risk factor trends and treatment uptakes. If the data are sparse or the quality poor then explicit assumptions and robust sensitivity analyses become essential when checking the validity of the model.
The model included only those aged 25 to 84 years old, because of very limited data in older groups. We considered only deaths from CHD and ignored “competing causes” such as cancer. However, we would expect that reductions in smoking would also decrease deaths from lung cancer and several other cancers. The IMPACT model assumes that estimates of efficacy from randomized controlled trials can usually be generalised to effectiveness in clinical practice.6,37 Although this seems reasonable, further development work is clearly needed.38 Risk factors and treatments were also considered to act independently in the model, but there is a paucity of literature on this issue. Finally, although lag times were not explicitly considered, they may be comparatively unimportant over 1.5 decades. Substantial mortality reduction occurs within one to four years of quitting smoking or reducing cholesterol levels.20,22
Explicit assumptions can then be tested by sensitivity analyses.26 Modelling studies provide a basis for assessing potential improvements in uptake of effective treatments, health promotion, and public health strategies.
In conclusion, about 48% of the recent CHD mortality decrease in Ireland was attributed to reductions in major risk factors, and 44% to medical and surgical therapies. Comprehensive CHD strategies should therefore maximise the population coverage of effective treatments and actively promote primary prevention.
Footnotes
Funding: the Irish Heart Foundation funded this project.
Competing interests: none declared.
References
- 1.Department of Health and Children Building healthier hearts: national cardiovascular health strategy. Dublin: Stationery Office, 1999
- 2.Department of Health and Children Ireland's changing heart: second report on the implementation of the cardiovascular health strategy. Dublin: Government Publications Sale Office, 2003
- 3.Tunstall‐Pedoe H, Vanuzzo D, Hobbs M.et al Estimation of contribution of changes in coronary care to improving survival, event rates, and coronary heart disease mortality across the WHO MONICA Project populations. Lancet 2000355675–687. [DOI] [PubMed] [Google Scholar]
- 4.Tunstall‐Pedoe H, Kuulasmaa K, Mahonen M.et al Contribution of trends in survival and coronary‐event rates to changes in coronary heart disease mortality: 10‐year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 19993531547–1557. [DOI] [PubMed] [Google Scholar]
- 5.Capewell S, Morrison C E, McMurray J J. Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart 199981380–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Unal B, Critchley J A, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 20041091101–1107. [DOI] [PubMed] [Google Scholar]
- 7.Capewell S, Beaglehole R, Seddon M.et al Explanation for the decline in coronary heart disease mortality rates in Auckland, New Zealand, between 1982 and 1993. Circulation 20001021511–1516. [DOI] [PubMed] [Google Scholar]
- 8.Laatikainen T, Critchley J, Vartiainen E.et al Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol 2005162764–773. [DOI] [PubMed] [Google Scholar]
- 9.Critchley J, Liu J, Zhao D.et al Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation 20041101236–1244. [DOI] [PubMed] [Google Scholar]
- 10.Hunink M G, Goldman L, Tosteson A N.et al The recent decline in mortality from coronary heart disease, 1980–1990. The effect of secular trends in risk factors and treatment. JAMA 1997277535–542. [PubMed] [Google Scholar]
- 11.Beaglehole R. Medical management and the decline in mortality from coronary heart disease. BMJ 198629233–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vartiainen E, Puska P, Pekkanen J.et al Changes in risk factors explain changes in mortality from ischaemic heart disease in Finland. BMJ 199430923–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bots M L, Grobbee D E. Decline of coronary heart disease mortality in the Netherlands from 1978 to 1985: contribution of medical care and changes over time in presence of major cardiovascular risk factors. J Cardiovasc Risk 19963271–276. [PubMed] [Google Scholar]
- 14.Department of Health and Children Public health information system (PHIS). Dublin: Information Management Unit, Department of Health and Children, 2001
- 15.HIPE and NPRS Unit Activity in acute public hospitals in Ireland 1990–1999. Dublin: The Economic and Social Research Institute, 2002
- 16.Lonergan M on behalf of the Irish Cardiac Surgery Group Irish cardiac surgery register report 1983–200. Dublin: Department of Health and Children, 2002
- 17.Doyle F, De La Harpe D, McGee H.et al Nine‐year comparison of presentation and management of acute coronary syndromes in Ireland: a national cross‐sectional survey. BMC Cardiovasc Disord 200555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shelley E and working group The Kilkenny health project: a community research and demonstration programme for cardiovascular disease prevention. Ir J Med Sci 1991160(suppl 9)1–54. [DOI] [PubMed] [Google Scholar]
- 19.Creagh D, Neilson S, Collins A.et al Established cardiovascular disease and CVD risk factors in a primary care population of middle‐aged Irish men and women. Ir Med J 200295298–301. [PubMed] [Google Scholar]
- 20.Critchley J A, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA 200329086–97. [DOI] [PubMed] [Google Scholar]
- 21.Lewington S, Clarke R, Qizilbash N.et al Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet 20023601903–1913. [DOI] [PubMed] [Google Scholar]
- 22.Law M R, Wald N J, Thompson S G. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ 1994308367–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.IMPACT http://www.liv.ac.uk/PublicHealth/sc/bua/IMPACT‐Model‐ Appendices pdf.
- 24.Mant J, Hicks N. Detecting differences in quality of care: the sensitivity of measures of process and outcome in treating acute myocardial infarction. BMJ 1995311793–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nichol M B, Venturini F, Sung J C. A critical evaluation of the methodology of the literature on medication compliance. Ann Pharmacother 199933531–540. [DOI] [PubMed] [Google Scholar]
- 26.Briggs A, Sculpher M, Buxton M. Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health Econ 1994395–104. [DOI] [PubMed] [Google Scholar]
- 27.Emberson J R, Whincup P, Morris R.et al Re‐assessing the contribution of serum total cholesterol, blood pressure and cigarette smoking to the aetiology of coronary heart disease: impact of regression dilution bias. Eur Heart J 2003241719–1726. [DOI] [PubMed] [Google Scholar]
- 28.Law M R, Wald N J, Rudnicka A R.et al Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta‐analysis. BMJ 20033261423–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Asia Pacific Cohort Studies Collaboration Cholesterol, coronary heart disease and stroke in the Asia Pacific region. Int J Epidemiol 200332563–572. [DOI] [PubMed] [Google Scholar]
- 30.Kabir Z, Clancy L. Preventive oncology. Lancet 20043631737. [DOI] [PubMed] [Google Scholar]
- 31.Dublin and Galway Health Promotion Unit, Centre for Health Promotion Studies, and Department of Public Health Medicine and Epidemiology The national health and lifestyles Survey. Dublin: Dublin and Galway Health Promotion Unit, 2003
- 32.Asia Pacific Cohort Studies Collaboration Body mass index and cardiovascular disease in the Asia‐Pacific region: an overview of 33 cohorts involving 305,000 participants. Int J Epidemiol 2004331–8. [DOI] [PubMed] [Google Scholar]
- 33.Liu J L, Maniadakis N, Gray A.et al The economic burden of coronary heart disease in the UK. Heart 200288597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Capewell S, Pell J P, Morrison C.et al Increasing the impact of cardiological treatments. How best to reduce deaths. Eur Heart J 1999201386–1392. [DOI] [PubMed] [Google Scholar]
- 35.Teeling M, Bennett K, Feely J. The influence of guidelines on the use of statins—analysis of prescribing trends 1998–2002. Br J Clin Pharmacol 200559227–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Department of Health and Children Heartwatch report. Ireland: Department of Health and Children, Health Boards, Irish College of General Practioners and Irish Heart Foundation, 2004
- 37.Unal B, Critchley J A, Fidan D.et al Life years gained from modern cardiological treatments and population risk factor changes in England and Wales. Am J Public Health 200595103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Critchley J A, Capewell S. Why model coronary heart disease? Eur Heart J 200223110–116. [DOI] [PubMed] [Google Scholar]