Abstract
Psychological and behavioral adaptation to HIV is integral to long-term survival. Although most research on coping with HIV has focused on factors associated with poor adaptation, recent research has expanded to include positive concomitants of adaptation, such as benefit finding. This study examined the occurrence of benefit finding among HIV+ men and women and evaluated the potential relevance of benefit finding to positive health behavior and psychosocial adaptation. HIV+ participants (N = 221) recruited during outpatient care completed self-report assessments of benefit finding, social support, depression, HAART adherence, substance use, and physical activity. In a series of multivariate analyses that controlled for demographic and health status variables, benefit finding was associated with lower depression scores, greater social support, and more physical activity, but showed no association to HAART adherence or substance use. The association of benefit finding to depression was partially mediated by differences in social support. Thus, benefit finding may improve psychological adjustment by motivating patients who experience stress-related growth to seek improved social support.
The success of highly active antiretroviral treatments (HAART) has dramatically improved the health outlook for people living with HIV (Volberding, 2003). Indeed, life expectancy estimates for persons living with HIV now mirror those seen among patients with type 1 diabetes (Lohse et al., 2007). However, HIV remains a highly stigmatized illness (Vanable, Carey, Blair, & Littlewood, 2006) and maintaining optimal health requires that patients manage multiple challenges and stressors. Within this context, research on coping with HIV has focused on factors associated with poor adaptation, including studies examining risk factors for depression, anxiety, and substance abuse disorders (Bing et al., 2001; Cruess et al., 2003). However, several studies indicate that a subset of HIV+ men and women perceive benefit accruing from their HIV-related experiences (Dunbar, Mueller, Medina, & Wolf, 1998; Mosack, Abbott, Singer, Weeks, & Rohena, 2005; Schwartzberg, 1993; Siegel & Schrimshaw, 2000).
“Benefit finding” refers to the efforts that individuals make to look for the positive aspects in their life while experiencing stressors and to look for good things that can be learned from that experience (Tennen & Affleck, 2002). Findings from research with other medical populations suggest that benefit finding in the context of a major medical stressor may be associated with improved psychosocial and behavioral adaptation (Affleck, Tennen, Croog, & Levine, 1987; Antoni et al., 2001; Carver & Antoni, 2004; Mohr et al., 1999; Pakenham, 2005; Petrie, Buick, Weinman, & Booth, 1999; Sears, Stanton, & Danoff-Burg, 2003; Tomich & Helgeson, 2004). Research on benefit finding in the context of HIV is limited so, in the present study, we clarify the relevance of benefit finding to health behavior adaptation and adjustment among people living with HIV disease.
Several theoretical frameworks address how some individuals may derive benefits from a life-threatening medical illness. For example, the theory of cognitive adaptation (Taylor, 1983; Taylor, Kemeny, Reed, Bower, & Gruenewald, 2000) proposes that perceiving benefits in response to a chronic stressor such as HIV can be viewed as a cognitive strategy used to counteract the negative impact of the disease; benefit finding can help a person to find meaning, gain mastery, and maintain self-esteem in the face of a serious illness (Taylor, 1983; Taylor et al., 2000). On this basis, the theory posits that cognitive adaptation in the form of benefit finding may minimize adverse health outcomes by reducing distress, which may in turn affect the physiological underpinnings of disease and improve health behaviors (Taylor et al., 2000). Thus, benefit finding may in part represent an “adaptive illusion” that serves to lessen the emotional impact of traumatic life events. In the context of HIV disease, a case can be made that an HIV diagnosis may also lead to actual as well as subjectively perceived life improvements. For example, prior to their HIV diagnosis, many HIV+ individuals face disadvantages stemming from poverty, psychiatric illness, drug addiction, unemployment, and housing difficulties. By entering into care for HIV, a subset of newly diagnosed individuals may, for the first time, gain access to regular medical care, social services, and disability benefits. Thus, consistent with the conservation of resources theory (Hobfoll, 1989, 2002), an HIV diagnosis may lead to the acquisition of tangible resources and positive changes, particularly for individuals whose life circumstances made them vulnerable to HIV in the first place. Whether benefit finding occurs through acquisition of tangible resources, a process of positive reappraisal, or a combination of both, individuals who perceive HIV as having some positive impact on their lives may be less distressed and more motivated to pursue adaptive health behaviors.
Health behavior changes (e.g., reduced substance use, improved diet) are commonly endorsed as positive changes that result from an HIV diagnosis (Siegel & Schrimshaw, 2000) and several studies note an association between benefit finding and improved health among HIV+ people (Bower, Kemeny, Taylor, & Fahey, 1998; Milam, 2006b). There is some evidence suggesting that benefit finding is related to initiation of HAART, possibly through improvements in health status (e.g., Judd et al., 2000; Rabkin, Ferrando, Lin, Sewell, & McElhiney, 2000), but few studies have explored the possibility that benefit finding promotes adherence to HAART. To date, findings from research investigating the association of benefit finding to specific health behaviors among HIV+ people have been mixed. Milam (2006b) found a small inverse association of perceived growth to alcohol and drug use, but no association of benefit finding to HIV medication adherence or physical activity. In an earlier study, benefit finding was associated with lower levels of alcohol use and more healthful eating (Milam, 2004), but showed no association to smoking, exercise, or illicit drug use. Research involving HIV+ women (Weaver et al., 2005) and HIV/AIDS clinic patients in India (Luszczynska, Sarkar, & Knoll, 2007) provides support for a positive association between benefit finding and adherence to HAART. In the present study, we sought to clarify the relevance of benefit finding to health behavior adaptation by characterizing the association of benefit finding to HAART adherence, physical activity, cigarette and alcohol use, and drug abuse problems. We propose that patients who perceive benefits and opportunities for personal growth stemming from their illness will be more motivated to adopt behavior changes that promote long-term survival, such as adherence to prescribed HIV medications.
Benefit finding may also have important implications for psychological adjustment among HIV+ men and women. A recent meta-analysis suggests that benefit finding in response to traumatic stress is associated with fewer depressive symptoms across a variety of medical and non medical populations (Helgeson, Reynolds, & Tomich, 2006). However, average effect sizes were small (r = −.09) and there was considerable heterogeneity in findings across studies. Further, only two of the 17 studies that assessed depression involved HIV+ patients. One of those studies (Milam, 2004) found no association between baseline levels of benefit finding and depression levels over time whereas the other found a negative association of benefit finding and depression in a sample of HIV+ women (Updegraff, Taylor, Kemeny, & Wyatt, 2002). A third more recently published study confirmed a cross-sectional association between perceived growth and depression in a sample of HIV+ men and women (Milam, 2006b). Additional research is warranted to clarify the strength of the association between benefit finding and psychological adjustment and to explore potential mechanisms linking benefit finding to improved mental health outcomes.
One way in which benefit finding may promote improved emotional adjustment is through changes in social support. Patients from a variety of medical populations, including HIV, frequently endorse “improved relationships” as a positive outcome of their illness experience (Dunbar et al., 1998; Petrie et al., 1999; Siegel & Schrimshaw, 2000; Thornton, 2002; Updegraff et al., 2002). Although a substantial body of research indicates that social support is associated with better psychological adjustment and use of adaptive coping strategies among HIV+ patients (Hall, 1999; Pakenham & Rinaldis, 2001; Serovich, Kimberly, Mosack, & Lewis, 2001), only two studies have examined the relationship between social support and benefit finding. In a small sample of HIV+ women recruited via community outreach, emotion-focused social support was found to be associated with stress-related growth (Siegel, Schrimshaw, & Pretter, 2005). Similarly, social support (i.e., emotional, informational, and instrumental) was associated with greater benefit finding among HIV+ patients recruited from three HIV treatment clinics in India (Luszczynska et al., 2007). An additional goal of the present study was to characterize the association of benefit finding to perceived social support and to test the hypothesis that the association of benefit finding to depression is mediated by differences in perceived social support.
To summarize, benefit finding may have important implications for understanding health behavior adaptation, psychosocial adjustment, and health outcomes among HIV+ individuals. Accordingly, in the present study we: (a) characterize the occurrence of benefit finding in a clinic based sample of HIV+ men and women; (b) describe the association of benefit finding to demographic and health status variables; and (c) present bivariate and multivariate analyses concerning the association of benefit finding to health behaviors (HAART adherence, substance use, and physical activity) and psychosocial adjustment (social support, and depression). We used a cross-sectional design to test the hypothesis that HIV+ patients who perceive benefits and opportunities for personal growth stemming from their illness would report better HAART adherence, more physical activity, less substance use, and fewer depressive symptoms. In addition, we predicted that the association of benefit finding to depression would be mediated by differences in social support.
Method
Participants
Participants were recruited from a university-based Infectious Disease Clinic in central New York State during a 16 month period beginning in July, 2001. A patient was eligible for the study if she or he was 18 years of age or older, HIV+, English speaking, and capable of providing informed consent. A total of 314 patients met eligibility criteria and were invited to participate. Among eligible participants, 76% consented to participate (N = 240). A subset of consenting participants were excluded due to poor data quality or early withdrawal from the study, yielding a final study N of 221 (44% female).
The mean age of participants was 40 years old (range 22–59). Of these, 42% self-identified as African-American, 46% Caucasians, 4% Native American, 4% Asian/Pacific Islander, and 4% “other.” Most participants reported that they were unemployed (67%), and 62% reported a yearly income under $10,000. Thirty-seven percent of participants had less than a high school diploma, 37% graduated high school, and 27% had completed some college. The average time since testing positive was 7 years, 37% had an undetectable viral load, and the mean CD4+ count was 500. The mean number of HIV-related symptoms reported was 13 out of a possible 20 and the mean discomfort score was 1.4. Seventy-eight percent of participants were currently taking HAART.
Procedure
A clinic nurse informed patients about the study and obtained verbal consent from the patient regarding his or her willingness to be introduced to a research assistant (RA). Patients who provided verbal consent were introduced to the RA, who informed the patient of the study goals and procedures. Patients were told that they would be asked to respond to sensitive questions about their health behaviors, mental health, and substance use, and were informed that they would receive $10 for participation. In addition, participants consented to allow research staff to access their medical records in order to obtain data points for current health status. All research participants provided written informed consent prior to the start of the study.
Literacy difficulties are common among persons in care for HIV (Kalichman & Rompa, 2000). To reduce survey administration difficulties related to literacy limitations, data collection for low-literacy participants (those scoring below the 9th grade reading level on the Rapid Estimate of Adult Literacy in Medicine; Davis et al., 1993) and participants for whom clinic or research staff expressed concerns about their capacity to understand the written questionnaire was completed using either an audio computer-assisted self-interview (n = 19; ACASI) or a face-to-face interview with an RA (n = 15). Interview administration was used in instances when the computer was unavailable (i.e., the assessment room equipped with the computer was already being used).
Measures
Demographics
Descriptive information, including age, employment status, ethnicity, education, and income was assessed using standardized questions developed in previous research with the population.
Medical records data
Patients’ medical records were accessed to obtain data on health status and clinic attendance for the past year. Data reported in the current study consisted of viral load (detectable vs. undetectable) and CD4+ count at the time of study participation, and AIDS diagnosis (yes/no).
HIV-related symptoms
A validated self-report measure of HIV-related symptoms assessed both physical and cognitive symptoms associated with HIV disease and treatment (Justice et al., 2001). The questionnaire includes a list of 20 common symptoms, and requires the patient to rate the degree to which each symptom has been bothersome to them within the last month on a 5-point Likert scale (0–4) with higher scores indicative of greater symptom severity. An HIV symptom discomfort score was computed based on participants’ mean response across the 20 items. In addition, a sum score of the number of HIV-related symptoms endorsed (symptoms rating > 0) was computed. In the current sample, this measure displayed high internal consistency (α = .91).
Depressive symptoms
Symptoms of depression were assessed using the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977). This 20-item questionnaire assesses the occurrence of cognitive, affective, motivational, and somatic symptoms within the last week and has been used extensively in both the general population and with samples of HIV+ men and women. Studies employing the CES-D to assess depressive symptoms among HIV+ individuals reveal average scores around 25, with a majority of participants scoring above the usual cut-off of 16 (Catz, Gore-Felton, & McClure, 2002; Farber, Mirsalimi, Williams, & McDaniel, 2003). In the current study, scores on the CES-D were treated as a continuous variable (α = .92 in the current sample).
Social Support
Perceived social support was measured across five domains related to living with HIV: assistance with financial problems, help with daily chores, talking about your illness, emotional support, and help with taking HIV medications (Alferi, Carver, Antoni, Weiss, & Duran, 2001). Participants reported on the extent to which they felt they could count on their (a) significant other, (b) family members, and (c) friends for support in each domain. The same items were asked for each support source and were rated on a five-point scale with three anchors: (1) not at all, (3) somewhat, and (5) a lot. This scale was scored by averaging items, with higher scores indicating greater perceived social support (α = .91 in the current sample). For patients without a spouse or partner (50%), an average score was computed based on data from the friends and family member items so that all participants had a social support score.
Physical activity
Two items assessed the frequency with which participants engaged in moderate (e.g., walking more that a couple of blocks) and vigorous (e.g., jogging) physical activity. Response options for each item were ‘never’, ‘a few times a month’, ‘a few times a week’, or ‘nearly every day.’ A composite physical activity score was computed based on the mean response for the two items.
Substance use
Current cigarette and alcohol use were also assessed. To assess tobacco use, participants were asked: “Over the past month, how many cigarettes have you smoked on the average day?” To assess alcohol consumption, two questions requested that participants indicate: (a) the average number of days during a week when they consumed one or more drinks, and (b) the typical quantity of alcohol consumed per day. As an indicator of global drinking patterns, the average number of days drinking alcohol per week was multiplied by the typical number of drinks consumed (Sobell & Sobell, 2003). For the smoking and alcohol use variables, outliers were defined as values in the distribution of observed scores that lie more than three standard deviations from the mean (i.e., z > 3.29). To ensure that the normality assumption was not violated in subsequent analyses, outliers were adjusted to one more than largest value in the distribution that corresponds to a z-score less than 3.29 (Schroder, Carey, & Vanable, 2003a; Tabachnick & Fidell, 2001).
Drug abuse
To assess for the presence of drug-related problems, the Drug Abuse Screening Test (DAST–10; Skinner, 1982) was administered. The DAST is a validated 10-item screening test developed to identify drug-use related problems in the previous year. A single summary score (range = 0–9) reflects the number of drug abuse items endorsed. Coefficient alpha in the current sample was .87.
HAART adherence
The 4-item medication adherence questionnaire used in this study was adapted from previously validated measures (Catz, Heckman, Kochman, & DiMarco, 2001; Chesney et al., 2000). Because recall accuracy is highest for short recall periods (e.g., Schroder, Carey, & Vanable, 2003b), we assessed adherence difficulties for the past seven days. Participants indicated the frequency of missed doses, frequency of late doses, and frequency of ignoring special instructions using a 6-point rating scale (‘more than once a day’ to ‘never during the past week’). In addition, participants indicated when the last time was that they skipped taking any of their HIV medication using a 6-point frequency scale (‘within the past week’ to ‘never’). To reduce socially desirable responding, the instructions on the assessment included phrases that attempted to normalize imperfect adherence and emphasized the importance of honest reporting. Summary scores were computed based on the mean of responses across the four-item adherence scale (α = .80).
Benefit finding
Benefit finding was assessed using a 17-item, single factor scale adapted from Antoni et al. (2001). The measure was originally developed for use with cancer patients. The measure was adapted for use in the present study by prefacing each item with the stem “Having had HIV disease…”. Response were rated using a 5-point Likert scale ranging from 1 (“not at all”) to 5 (“extremely”). Sample items include: “Having had HIV disease has brought my family closer together,” “Having had HIV disease has led me to deal better with stress and problems,” and “Having had HIV disease has helped me become more focused on priorities, with a deeper sense of purpose in life.” A single score was computed by averaging responses across the 17 items, with higher scores indicating greater benefit finding. Consistent with Antoni et al. (2001), factor analysis using data from the present sample yielded a single factor solution (Eigenvalue = 8.9) and the scale demonstrated good internal reliability (α = .94). Antoni et al. (2001) report evidence of convergent validity for the benefit finding measure and optimism (r = .23), discriminant validity between benefit finding and a POMS-derived index of distress (r = −.25), and benefit finding scores were relatively stable throughout the 12-month study period (r = .75 to .91).
Overview of Analyses
First, we present descriptive data on benefit finding among participants. Next, analyses are presented to characterize the association of benefit finding to demographic characteristics, subjective ratings of HIV-related symptoms, and objective indices of current health, and to test for hypothesized associations between benefit finding and indices of positive health behavior adaptation and psychosocial adjustment. The association of benefit finding to demographic characteristics and objective indices of current health status were examined using t-tests, analysis of variance (ANOVA), and Pearson’s product-moment correlations. To characterize the association of benefit finding with each of the hypothesized dependent variables, a series of regression equations were computed with significant demographic and health status correlates entered at Step 1 and benefit finding entered at Step 2. Supplemental analyses were also conducted to determine whether demographic or health status characteristics moderate the association between benefit finding and the dependent variables. We first computed an interaction term for benefit finding and the standardized or dummy coded scores for selected moderators (i.e., gender, ethnicity, time since HIV diagnosis, AIDS diagnosis, and HIV symptoms). Then, separate regression analyses were computed, with the main effects of benefit finding and each relevant moderator variable entered at Step 1 and the interaction term entered at Step 2. Finally, to test whether social support mediates the hypothesized association between benefit finding and depression, Baron and Kenny (1986) procedures were employed.
Results
Descriptive Findings
Averaging across benefiting finding items, the mean response was 3.6 (SD = .95), indicating moderate to high levels of agreement. Among the highest rated items were “Having had HIV disease has taught me how to adjust to things I cannot change” (M = 3.9, SD = 1.2) and “Having had HIV disease has helped me become more focused on priorities, with a deeper sense of purpose in life” (M = 3.7, SD = 1.4). Among the lowest rated items on the measure were “Having had HIV disease has brought my family closer together” (M = 2.7, SD = 1.5) and “Having had HIV disease has led me to meet people who have become some of my best friends” (M = 2.9, SD = 1.5).
Bivariate Association of Benefit Finding to Demographic and Health Status Variables
Benefit finding scores differed by gender, such that women scored higher than men (M = 3.8 vs. 3.5), t(220) = 2.61, p < .01, and for ethnicity, such that African-American participants scored higher than other participants (M = 3.8 vs. 3.5), t(220) = 2.53, p < .02. Benefit finding scores did not vary as a function of age, education, employment status, income, sexual orientation, or relationship status (all ps > .05).
Benefit finding was associated with current AIDS diagnosis, such that participants diagnosed with AIDS reported greater benefit finding (M = 3.8 vs. 3.5), t(219) = −2.31, p < .05. Whereas benefit finding was more common among those with an AIDS diagnosis, self-reported HIV-related symptoms were negatively associated with benefit finding (r = −.14, p < .05), indicating greater benefit finding among patients with fewer symptoms. Benefit finding was not associated with current viral load (detectable vs. undetectable), average CD4+ count, or time since HIV diagnosis (all ps > .05).
Association of Benefit Finding to Health Behavior Adaptation and Psychosocial Adjustment
Bivariate associations between benefit finding and primary study variables are presented in Table 1. Primary hypotheses concerning the association of benefit finding to health behavior adaptation and psychological adjustment were tested with multiple regression analyses. Because gender, ethnicity, AIDS diagnosis, and HIV-related symptoms were associated with benefit finding in bivariate analyses, these variables were entered as covariates in Step 1 of each regression analysis, followed by the benefit finding score in Step 2. Significant results from hierarchical regression models conducted for each dependent variable are presented in Table 2.
Table 1.
Intercorrelations, Means, and Standard Deviations of Primary Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M | SD | Range |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Benefit Finding | 3.6 | .95 | 1–5 | |||||||
| 2. Depression | −.24** | 19.6 | 12.7 | 0–40 | ||||||
| 3. Social Support | .31** | −.32** | 3.0 | 1.1 | 1–5 | |||||
| 4. Adherence | −.07 | .19* | −.15* | 4.6 | 1.3 | 1–6 | ||||
| 5. Physical Activity | .25** | −.17* | .12 | −.08 | 1.4 | 1.5 | 0–3 | |||
| 6. Cigarettes/Day | −.01 | .17* | −.06 | .13 | −.04 | 10 | 10 | 0–41 | ||
| 7. Alcohol Use | −.11 | .02 | −.01 | .07 | .06 | .14* | 3.5 | 9.1 | 0–77 | |
| 8. DAST | −.04 | .19** | −.09 | .23* | .14* | .14* | .02 | 1.7 | 2.4 | 0–9 |
Note. p < .05.
p < .01.
Table 2.
Hierarchical Multiple Regression Results for Association Between Benefit Finding and Indices of Psychosocial and Behavioral Adaptation to HIV
| Health Behavior and Psychosocial Outcome Variables
|
||||||
|---|---|---|---|---|---|---|
| Physical Activity
|
Depressive Symptoms
|
Social Support
|
||||
| Block and predictor | β | Model R2 | β | Model R2 | β | Model R2 |
| Step 1 | .04 | .37*** | .05* | |||
| Gender | .09 | −.07 | .08 | |||
| Ethnicity | −.05 | −.02 | .02 | |||
| AIDS Diagnosis | .05 | −.12** | −.03 | |||
| HIV Symptoms | −.14* | .57*** | −.20** | |||
| Step 2 | .09*** | .39*** | .16*** | |||
| Benefit Finding | .25*** | −.17** | .35*** | |||
Note. p < .05.
p < .01.
p < .001.
With respect to the indices of positive health behavior adaptation, the hypothesized associations with benefit finding were partially supported. As predicted, physical activity was significantly associated with benefit finding in the final step of the regression model, after controlling for relevant background variables, F(5, 219) = 4.26, p < .001. Contrary to expectation, the hypothesized associations between benefit finding and HAART adherence, alcohol use, drug abuse, and smoking were not supported (all ps > .05). As shown in Table 3, benefit finding was associated with both indices of psychosocial adaptation. After controlling for relevant health status and demographic variables, benefit finding was inversely related to current depressive symptoms, F(5, 218) = 27.55, p < .001, and positively associated with social support, F(5, 217) = 8.14, p < .001.
Supplemental analyses were conducted to determine whether demographic or health status characteristics (i.e., gender, ethnicity, time since HIV diagnosis, AIDS diagnosis, or HIV symptoms) moderate the association between benefit finding and each dependent variable. Results (not tabled) confirmed that the association of benefit finding to depression, social support, adherence, activity level, smoking, alcohol use index, and drug problems did not vary as a function of demographic or health status characteristics.
Does Social Support Mediate the Association of Benefit Finding to Depression?
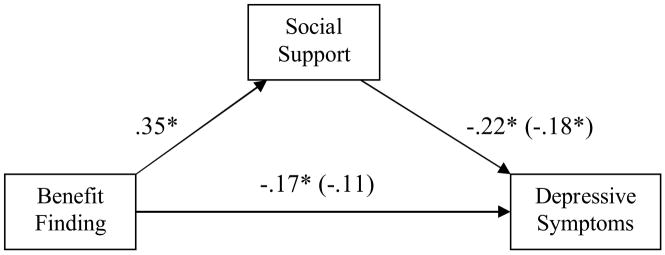
Based on the observed associations between benefit finding, depression, and social support, follow-up analyses tested the hypothesis that social support would mediate the association of benefit finding with depressive symptoms. Following the recommendations of Baron and Kenny (1986), we first established that the conditions for mediation were met using a series of multiple regression analyses that controlled for relevant covariates. As illustrated in Figure 1, the direct effect of benefit finding on depression was significant (β = −.17, ΔR2 = .03, p < .01), satisfying the first criterion for mediation. Second, benefit finding was associated with the hypothesized mediating variable, social support (β = .35, , ΔR2 = .11, p < .0001). Satisfying the third criterion, social support was related to depression while controlling for benefit finding (β = −.18, ΔR2 = .06, p < .01). Finally, when all the variables were entered in one regression equation with depression as the dependent variable, the beta weight (−.11) for benefit finding was non-significant (p > .05) and the beta weight for social support (−.18) remained significant (p < .01). To confirm that the relation between benefit finding and depression is significantly smaller with social support entered as a predictor, a formal test of the significance of the observed indirect effect was conducted (Frazier, Tix, & Barron, 2004; Preacher & Hayes, 2004). The relation between benefit finding and depression decreased significantly when social support was included in the equation (Sobel test statistic z = −3.01, p < .01). Given that the association between benefit finding and depression decreased significantly (but not to zero) with the inclusion of social support, we conclude that social support partially mediated the association of benefit finding to depression.
Figure 1.
Social support mediates the association between benefit finding and depressive symptoms. Numbers in parentheses are standardized beta coefficients that represent indirect effects when social support was included in the model (* p < .01).
Discussion
Although there is now a broad literature indicating that benefit finding is commonly experienced in response to a variety of traumatic stressors, research has only recently begun to explore the ways in which benefit finding may influence the lives of men and women living with HIV. The present study sought to describe interrelations among physical health status, psychosocial adjustment, and health behavior adaptation in a clinic sample of HIV+ men and women. In addition to the goal of characterizing the extent to which HIV+ individuals attribute positive changes to their experience of living with HIV, it was hypothesized that benefit finding would be associated with psychosocial and behavioral adaptation, as assessed by indicators of current HAART adherence, substance use, physical activity, depressive symptoms, and social support. Several noteworthy findings emerged.
Positive changes across a variety of life domains were frequently attributed to the experience of having HIV. Indeed, the majority of participants endorsed moderate to high levels of agreement with statements indicative of a major shift in perspective, priorities, and personal growth. Thus, consistent with findings from populations of bereaved individuals (Davis, Nolen-Hoeksema, & Larson, 1998), heart attack survivors (Affleck et al., 1987; Petrie et al., 1999), multiple-sclerosis patients (Mohr et al., 1999; Pakenham, 2005), and cancer patients (Antoni et al., 2001; Carver & Antoni, 2004; Sears et al., 2003; Tomich & Helgeson, 2004), many HIV+ individuals report gains in the context of coping with a chronic, incurable illness. The tendency to perceive benefits in the context of being HIV+ was more common among African-American and female participants, relative to Caucasian and male participants. Although benefit finding was not associated with objective markers of viral load and CD4+ count, benefit finding was associated with having been diagnosed with AIDS and negatively correlated with self-reported HIV-related symptoms. Although these findings may appear contradictory, they should be considered within the context of the classification criteria used to establish an AIDS diagnosis. Current guidelines specify that a person is classified as having AIDS if their CD4+ counts drop below 200 or if a patient has had one of several AIDS defining illnesses; these guidelines do not allow for revocation of AIDS diagnosis even if the patient no longer meets criteria for AIDS. In our sample, the mean CD4+ count for patients with an AIDS diagnosis was 322 and 39% of patients diagnosed with AIDS had an undetectable viral load. Thus, it is conceivable that higher benefit finding among patients with AIDS may have been influenced by the subset of patients who recovered to the point where their immune functioning resembles that of an asymptomatic individual.
Consistent with other recent reports in the literature (Farber et al., 2003; Luszczynska et al., 2007; Milam, 2004, 2006b; Siegel & Schrimshaw, 2000; Weaver et al., 2005), findings from the present study suggest that benefit finding may decrease HIV+ patients’ vulnerability to psychological adjustment difficulties. In analyses that controlled for relevant demographic and health status variables, benefit finding was associated with fewer depressive symptoms and greater perceived social support. The association between benefit finding and depressive symptoms is particularly noteworthy, given the high rates of depression observed in the current sample (CES-D, M = 19.6) and in other community-dwelling samples of persons living with HIV (Bing et al., 2001).
To clarify potential mechanisms linking benefit finding to depressive symptoms, our study also tested the hypothesis that social support would mediate the association of benefit finding with depression. Findings confirmed that social support and depression were correlated with one another and each were associated with benefit finding. Consistent with our mediational hypothesis, when both social support and benefit finding were included in the regression model, only social support remained as a significant predictor of depression scores. Thus, findings suggest that participants who reported greater benefit finding may have fewer depressive symptoms, in part because they perceive themselves as receiving more support in dealing with their illness. This finding has important clinical implications. Patients who experience benefit finding in the context of adapting to HIV may well be emboldened to seek out social support from friends, partners, and family. In turn, the presence of supportive others may serve to buffer patients’ vulnerability to depression or related difficulties. Because findings are based on cross-sectional data, an important goal for future research will be to clarify the directionality and temporal sequencing of changes in benefit finding, social support, and depression using a longitudinal research design.
Study results provided only modest support for an association of benefit finding to health behaviors. Benefit finding was associated with physical activity, as measured by items assessing the frequency of both moderate and vigorous exercise. The observed association of benefit finding to exercise warrants additional investigation, particularly given recent data suggesting that physical activity is associated with improved health among persons with HIV (Bopp et al., 2004; Mustafa et al., 1999). However, benefit finding was not associated with HAART adherence, nor was there an association of benefit finding to tobacco use, alcohol use, or drug abuse problems. The absence of an association between benefit finding and HAART adherence was also observed by Milam (2006b) and suggests that any improvements in health associated with benefit finding are not mediated by better adherence to HAART.
An important focus for research is to disentangle the extent to which cognitive adaptation and acquisition of actual benefits explain the development of benefit finding. Although findings from the current study are not inconsistent with either of the proposed mechanisms, the occurrence of cognitive adaptation or the acquisition of tangible benefits (e.g., housing subsidies) resulting from receiving an HIV or AIDS diagnosis were not directly assessed in this study. Further investigation of these mechanisms would help to clarify the way in which benefit finding is linked to lower levels of depressed mood. For example, if benefit finding is a product of cognitive adaptation (Taylor et al., 2000), the tendency to perceived benefits may co-vary along a continuum of psychological adaptation, where distress is inversely related to benefit finding. Alternatively, if benefit finding stems primarily from the acquisition of tangible resources, acquisition of resources would presumably lessen a patient’s future vulnerability to depressed mood. Indeed, some have argued that it is the successful integration of contrasting states (e.g., distressed mood associated with traumatic illness and the perception of benefits) that brings about eventual psychological adjustment among patients coping with a traumatic illness such as HIV (e.g., Milam, 2006a).
Closely related to these conceptual challenges are the methodological limitations introduced by the use of a cross-sectional research design. Indeed, the cross-sectional design of this study precludes definitive interpretation of the nature and direction of the observed relationships among study variables. As with other aspects of adaptation to HIV, it is likely that the extent to which one is able to identify benefits associated with being HIV+ will fluctuate over time as a function of disease progression, treatment response, and other psychosocial factors. Given the importance of psychological adjustment and health behaviors to long-term survival, prospective studies that examine the relevance of benefit finding over time to long-term adaptation and health are warranted. For example, while perceived social support has been linked to fewer depressive symptoms in HIV+ samples (e.g., Hays, Turner, & Coates, 1992), prospective research is needed to clarify how perceived benefits associated with medical illness interact with social support in predicting psychological adjustment.
Limitations associated with the use of self-report measures, including memory biases, social desirability, and both willful and unwitting distortion of responses, should also be considered (Rand, 2000). Given that self-report assessments of HAART adherence may be influenced by self-report biases or inaccurate responding (Simoni et al., 2006), steps were taken to reduce the potential for biased responding in the present study. However, future studies may consider incorporating an objective measure of HAART adherence in order to reduce the potential for biased responding.
This study extends the base of knowledge on the contribution of benefit finding to psychosocial adjustment and health behavior adaptation in a diverse sample of HIV+ individuals. Given that most patients reported experiencing benefits in the context of being HIV+ and that such benefits were associated with better psychological adaptation and more frequent physical activity, an important direction for future research concerns the application of findings to the development of effective coping interventions. Indeed, several interventions designed to improve adaptation in the context of coping with a medical stressor have shown promising results (Antoni et al., 2001; Chesney, Chambers, Taylor, Johnson, & Folkman, 2003; McGregor et al., 2004; Stanton et al., 2002). Further, several studies suggest that benefit finding is amenable to change through cognitive-behavioral (Antoni et al., 2001; Carver & Antoni, 2004) and expressive writing (Stanton et al., 2002) interventions. Interventions that facilitate benefit finding may prove helpful in reducing distress and improving quality of life.
Relative to other health conditions, patients’ reports of benefit finding in the context of HIV disease are striking, given the degree to which people continue to experience stigma and discrimination because of HIV disease (Vanable et al., 2006). Although benefit finding is a topic of relevance across a wide variety of health and other stress-related events (Linley & Joseph, 2004), it is noteworthy that benefit finding in the context of HIV disease has only recently received empirical attention. Indeed, prior to the advent of HAART, HIV+ patients may have been hard-pressed to identify positive changes associated with having such a highly stigmatized, deadly disease. Even with improved life expectancies, persons living with HIV continue to struggle with a host of stressors (e.g., poverty, stigma, discrimination, depression, and substance dependence) in addition to the demands of managing their illness. Given all the challenges faced by persons living with HIV, it is remarkable that the experience of having HIV is associated with such positive changes. Whether such changes reflect perceived rather than objective life improvement is a topic of continuing debate. In either case, given the growing evidence that benefit finding is associated with better adjustment among patients experiencing traumatic illnesses, benefit finding remains a compelling construct worthy of further theoretical development and empirical investigation.
Acknowledgments
This work was supported by the National Institute of Mental Health Grant R21-MH65865. The authors thank the staff at University Hospital for their support of this work. Special thanks are extended to Missy Albert, Linda Bartlett, Jennifer Brown, Mary Beth Cavalieri, Kelley Flood, Lois Needham, Paul Preczewski, Pamela Wickham, Judy Rees, Craig Withers, and Jennifer Wuilliez for their assistance.
Footnotes
Rae A. Littlewood, Peter A. Vanable, and Michael P. Carey, Department of Psychology and Center for Health and Behavior, Syracuse University, Syracuse, NY. Donald Blair, Department of Medicine, SUNY Upstate Medical University.
References
- Affleck G, Tennen H, Croog S, Levine S. Causal attribution, perceived benefits, and morbidity after a heart attack: an 8-year study. Journal of Consulting and Clinical Psychology. 1987;55(1):29–35. doi: 10.1037//0022-006x.55.1.29. [DOI] [PubMed] [Google Scholar]
- Alferi SM, Carver CS, Antoni MH, Weiss S, Duran RE. An exploratory study of social support, distress, and life disruption among low-income Hispanic women under treatment for early stage breast cancer. Health Psychology. 2001;20(1):41–46. doi: 10.1037//0278-6133.20.1.41. [DOI] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry. 2001;58(8):721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Bopp CM, Phillips KD, Fulk LJ, Dudgeon WD, Sowell R, Hand GA. Physical activity and immunity in HIV-infected individuals. AIDS Care. 2004;16(3):387–393. doi: 10.1080/09540120410001665385. [DOI] [PubMed] [Google Scholar]
- Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. Journal of Consulting and Clinical Psychology. 1998;66(6):979–986. doi: 10.1037//0022-006x.66.6.979. [DOI] [PubMed] [Google Scholar]
- Carver CS, Antoni MH. Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychology. 2004;23(6):595–598. doi: 10.1037/0278-6133.23.6.595. [DOI] [PubMed] [Google Scholar]
- Catz SL, Gore-Felton C, McClure JB. Psychological distress among minority and low-income women living with HIV. Behavioral Medicine. 2002;28(2):53–60. doi: 10.1080/08964280209596398. [DOI] [PubMed] [Google Scholar]
- Catz SL, Heckman TG, Kochman A, DiMarco M. Rates and correlates of HIV treatment adherence among late middle-aged and older adults living with HIV disease. Psychology, Health, and Medicine. 2001;6(1):47–58. [Google Scholar]
- Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: Results from a randomized clinical trial testing a group-based intervention. Psychosomatic Medicine. 2003;65(6):1038–1046. doi: 10.1097/01.psy.0000097344.78697.ed. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. AIDS Care. 2000;12(3):255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Cruess DG, Evans DL, Repetto MJ, Gettes D, Douglas SD, Petitto JM. Prevalence, diagnosis, and pharmacological treatment of mood disorders in HIV disease. Biological Psychiatry. 2003;54(3):307–316. doi: 10.1016/s0006-3223(03)00318-4. [DOI] [PubMed] [Google Scholar]
- Davis CG, Nolen-Hoeksema S, Larson J. Making sense of loss and benefiting from the experience: Two construals of meaning. Journal of Personality and Social Psychology. 1998;75(2):561–574. doi: 10.1037//0022-3514.75.2.561. [DOI] [PubMed] [Google Scholar]
- Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Family Medicine. 1993;25(6):391–395. [PubMed] [Google Scholar]
- Dunbar HT, Mueller CW, Medina C, Wolf T. Psychological and spiritual growth in women living with HIV. Social Work. 1998;43(2):144–154. doi: 10.1093/sw/43.2.144. [DOI] [PubMed] [Google Scholar]
- Farber EW, Mirsalimi H, Williams KA, McDaniel JS. Meaning of illness and psychological adjustment to HIV/AIDS. Psychosomatics. 2003;44(6):485–491. doi: 10.1176/appi.psy.44.6.485. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology. 2004;51(1):115–134. [Google Scholar]
- Hall VP. The relationship between social support and health in gay men with HIV/AIDS: An integrative review. Journal of the Association of Nurses in AIDS Care. 1999;10(3):74–86. doi: 10.1016/S1055-3290(05)60121-5. [DOI] [PubMed] [Google Scholar]
- Hays RB, Turner H, Coates TJ. Social support, AIDS-related symptoms, and depression among gay men. Journal of Consulting and Clinical Psychology. 1992;60(3):463–469. doi: 10.1037//0022-006x.60.3.463. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44:513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Social and psychological resources and adaptation. Review of General Psychology. 2002;6(4):307–324. [Google Scholar]
- Judd FK, Cockram AM, Komiti A, Mijch AM, Hoy J, Bell R. Depressive symptoms reduced in individuals with HIV/AIDS treated with highly active antiretroviral therapy: a longitudinal study. Australian & New Zealand Journal of Psychiatry. 2000;34(6):1015–1021. doi: 10.1080/000486700278. [DOI] [PubMed] [Google Scholar]
- Justice AC, Holmes W, Gifford AL, Rabeneck L, Zackin R, Sinclair G, et al. Development and validation of a self-completed HIV symptom index. Journal of Clinical Epidemiology. 2001;54:S77–90. doi: 10.1016/s0895-4356(01)00449-8. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. Functional health literacy is associated with health status and health-related knowledge in people living with HIV-AIDS. Journal of Acquired Immune Deficiency Syndrome. 2000;25(4):337–344. doi: 10.1097/00042560-200012010-00007. [DOI] [PubMed] [Google Scholar]
- Linley PA, Joseph S. Positive change following trauma and adversity: A review. Journal of Traumatic Stress. 2004;17(1):11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e. [DOI] [PubMed] [Google Scholar]
- Lohse N, Hansen AB, Pedersen G, Kronborg G, Gerstoft J, Sorensen HT, et al. Survival of persons with and without HIV infection in Denmark, 1995–2005. Annals of Internal Medicine. 2007;146(2):87–95. doi: 10.7326/0003-4819-146-2-200701160-00003. [DOI] [PubMed] [Google Scholar]
- Luszczynska A, Sarkar Y, Knoll N. Received social support, self-efficacy, and finding benefits in disease as predictors of physical functioning and adherence to antiretroviral therapy. Patient Education and Counseling. 2007;66(1):37–42. doi: 10.1016/j.pec.2006.10.002. [DOI] [PubMed] [Google Scholar]
- McGregor BA, Antoni MH, Boyers A, Alferi SM, Blomberg BB, Carver CS. Cognitive-behavioral stress management increases benefit finding and immune function among women with early-stage breast cancer. Journal of Psychosomatic Research. 2004;56(1):1–8. doi: 10.1016/S0022-3999(03)00036-9. [DOI] [PubMed] [Google Scholar]
- Milam J. Posttraumatic growth among HIV/AIDS patients. Journal of Applied Social Psychology. 2004;34(11):2353–2376. [Google Scholar]
- Milam J. Positive changes attributed to the challenge of HIV/AIDS. In: Calhoun LG, Tedeschi RG, editors. Handbook of post-traumatic growth: Research and practice. Mahwah, NJ: Erlbaum; 2006a. pp. 214–224. [Google Scholar]
- Milam J. Posttraumatic growth and HIV disease progression. Journal of Consulting and Clinical Psychology. 2006b;74(5):817–827. doi: 10.1037/0022-006X.74.5.817. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Dick LP, Russo D, Pinn J, Boudewyn AC, Likosky W, et al. The psychosocial impact of multiple sclerosis: Exploring the patient’s perspective. Health Psychology. 1999;18(4):376–382. doi: 10.1037//0278-6133.18.4.376. [DOI] [PubMed] [Google Scholar]
- Mosack KE, Abbott M, Singer M, Weeks MR, Rohena L. If I didn’t have HIV, I’d be dead now: illness narratives of drug users living with HIV/AIDS. Qualitative Health Research. 2005;15(5):586–605. doi: 10.1177/1049732304271749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafa T, Sy FS, Macera CA, Thompson SJ, Jackson KL, Selassie A, et al. Association between exercise and HIV disease progression in a cohort of homosexual men. Annals of Epidemiology. 1999;9(2):127–131. doi: 10.1016/s1047-2797(98)00043-x. [DOI] [PubMed] [Google Scholar]
- Pakenham KI. Benefit finding in multiple sclerosis and associations with positive and negative outcomes. Health Psychology. 2005;24(2):123–132. doi: 10.1037/0278-6133.24.2.123. [DOI] [PubMed] [Google Scholar]
- Pakenham KI, Rinaldis M. The role of illness, resources, appraisal, and coping strategies in adjustment to HIV/AIDS: The direct and buffering effects. Journal of Behavioral Medicine. 2001;24(3):259–279. doi: 10.1023/a:1010718823753. [DOI] [PubMed] [Google Scholar]
- Petrie KJ, Buick DL, Weinman J, Booth RJ. Positive effects of illness reported by myocardial infarction and breast cancer patients. Journal of Psychosomatic Research. 1999;47(6):537–543. doi: 10.1016/s0022-3999(99)00054-9. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Rabkin JG, Ferrando SJ, Lin SH, Sewell M, McElhiney M. Psychological effects of HAART: a 2-year study. Psychosomatic Medicine. 2000;62(3):413–422. doi: 10.1097/00006842-200005000-00015. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rand CS. “I took the medication like you told me, doctor”: Self-report of adherence with medical regimens. In: Stone A, Turkkan J, Bachrach C, Jobe J, Kurtzman H, Cain V, editors. The science of self-report: Implications for research and practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: I. Item content, scaling, and data analytical options. Annals of Behavioral Medicine. 2003a;26(2):76–103. doi: 10.1207/s15324796abm2602_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine. 2003b;26(2):104–123. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartzberg SS. Struggling for meaning: How HIV-positive gay men make sense of AIDS. Professional Psychology: Research and Practice. 1993;24(4):483–490. [Google Scholar]
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22(5):487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- Serovich JM, Kimberly JA, Mosack KE, Lewis TL. The role of family and friend social support in reducing emotional distress among HIV-positive women. AIDS Care. 2001;13(3):335–341. doi: 10.1080/09540120120043982. [DOI] [PubMed] [Google Scholar]
- Siegel K, Schrimshaw EW. Perceiving benefits in adversity: Stress-related growth in women living with HIV/AIDS. Social Science and Medicine. 2000;51(10):1543–1554. doi: 10.1016/s0277-9536(00)00144-1. [DOI] [PubMed] [Google Scholar]
- Siegel K, Schrimshaw EW, Pretter S. Stress-related growth among women living with HIV/AIDS: examination of an explanatory model. Journal of Behavioral Medicine. 2005;28(5):403–414. doi: 10.1007/s10865-005-9015-6. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS & Behavior. 2006;10(3):227–245. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Wilson VB, editors. Assessing alcohol problems: A guide for clinicians and researchers. 2. Washington, D.C: NIAAA; 2003. pp. 75–79. [Google Scholar]
- Stanton AL, Danoff-Burg S, Sworowski LA, Collins CA, Branstetter AD, Rodriguez-Hanley A, et al. Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients. Journal of Clinical Oncology. 2002;20(20):4160–4168. doi: 10.1200/JCO.2002.08.521. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4. Allyn & Bacon; 2001. [Google Scholar]
- Taylor SE. Adjustment to Threatening Events: A theory of cognitive adaptation. American Psychologist. 1983;38(11):1161–1173. [Google Scholar]
- Taylor SE, Kemeny ME, Reed GM, Bower JE, Gruenewald TL. Psychological resources, positive illusions, and health. American Psychologist. 2000;55(1):99–109. doi: 10.1037//0003-066x.55.1.99. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G. Benefit-finding and benefit-reminding. In: Snyder CR, Lopez SJ, editors. The handbook of positive psychology. New York: Oxford University Press; 2002. [Google Scholar]
- Thornton AA. Perceiving benefits in the cancer experience. Journal of Clinical Psychology in Medical Settings. 2002;9(2):153–165. doi: 10.1007/s10880-011-9270-3. [DOI] [PubMed] [Google Scholar]
- Tomich PL, Helgeson VS. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychology. 2004;23(1):16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- Updegraff JA, Taylor SE, Kemeny M, Wyatt G. Positive and negative effects of HIV infection in women with low socioeconomic resources. Personality & Social Psychology Bulletin. 2002;28(3):382–394. [Google Scholar]
- Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS & Behavior. 2006;10(5):473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volberding PA. HIV therapy in 2003: Consensus and controversy. Aids. 2003;17(Supp 1):4–11. doi: 10.1097/00002030-200304001-00002. [DOI] [PubMed] [Google Scholar]
- Weaver K, Llabre M, Lechner S, Antoni MH, Duran R, Schneiderman N. Benefit finding predicts HAART adherence and, indirectly, HIV viral load in women, but not in gay men [abstract]; 2005, April; Paper presented at the meeting of the Society of Behavioral Medicine; Boston, MA. [Google Scholar]