Abstract
We investigated whether a vaccine derived from an apathogenic reassortant type A H5N1 influenza strain could induce immune responses in vivo that mediated protection from highly pathogenic avian influenza virus infection in mice. After two subcutaneous immunizations with formalin-inactivated H5N1 whole virus particles (whole particle vaccine), significant killing specific for cells presenting a nucleoprotein peptide from the vaccine strain of the virus was observed. Similar vaccination with viruses treated with ether and formalin, which are commonly used for humans as ether-split vaccines, induced little or no cytotoxic T-cell response. Furthermore, whole particle vaccines of the apathogenic H5N1 strain were more effective than ether-split vaccines at inducing antibody production able to neutralize a highly pathogenic H5N1 strain. Finally, whole particle vaccines of H5N1 protected mice against infection by an H5N1 highly pathogenic avian influenza virus more effectively than did ether-split vaccines. These results suggest that formalin-inactivated virus particles of apathogenic strains are effective for induction of both cytotoxic T-lymphocyte and antibody responses against highly pathogenic avian influenza viruses in vivo, resulting in protection from infection by a highly pathogenic H5N1 virus.
Keywords: cytotoxic T lymphocyte, H5N1, virus library, virus particle
Introduction
The H5N1 influenza viruses are an emerging type of highly pathogenic avian influenza virus that have caused more than a hundred deaths in humans.1,2 Because highly pathogenic strains of H5N1 influenza viruses express haemagglutinin (HA) proteins with a unique cleavage site digested by not only trypsin-like proteases but also the other ubiquitous proteases,3 highly pathogenic avian strains replicate not only in the upper respiratory tract but also in other organs.4,5 In addition, it is believed that most humans do not possess natural immunity against the H5N1 influenza viruses because these viruses have not been in wide circulation in the population. Therefore, preparation of vaccines against H5N1 influenza viruses is an urgent issue.
Protection against viral infection or its consequences is dependent on both innate immunity and acquired immunity.6 Acquired immunity, including cytotoxic T-lymphocyte (CTL) and antibody responses, has a critical role in durable protection after vaccination. However, in influenza virus infection, it has not been determined which is more critical for protection, CTL or antibody responses. Antibody responses induced by vaccination with inactivated influenza viruses protect mice from a challenge virus.7 On the other hand, elimination of influenza viruses was delayed and survival was severely impaired in mice lacking the CTL responses as a result of administration of depleted anti-CD8 antibody or disruption of major histocompatibility complex (MHC) class I expression.8,9 Thus, CTL responses are also thought to contribute to protection against influenza virus infection. Therefore, vaccines that induce both CTL and antibody responses are thought to be more effective than those eliciting only a CTL or an antibody response.
Viral infection and live-attenuated vaccines have been shown to induce vigorous antigen-specific CTL responses.10,11 However, live vaccines have several risks, including reversion of virulence and induction of severe diseases in immunocompromised individuals. Therefore, at present, inactivated vaccines against influenza viruses are favoured and in widespread use. It is uncertain whether the ether and formalin-inactivated vaccines (ether-split vaccines) commonly used in humans, which induce mainly antibody responses, provoke optimal cellular immunity that might be critical in host defence against highly pathogenic viral strains. In our previous study, a formalin-inactivated vaccine (whole particle vaccine) that retained the structure of virus particles induced protective antibodies against highly pathogenic avian influenza viruses.12
The ability of this vaccine preparation to induce CTL responses and the contribution of CTL responses to protection from infection have not been examined in mice. Indeed, it has been reported that formalin-inactivated vaccines do not induce CTL responses specific for influenza virus antigens.7 On the other hand, heat-inactivated viral particles and killed whole virus induced CTL responses.13,14 Because of the controversy concerning CTL induction by inactivated whole viral particles,7,13–15 here we have examined whether formalin-inactivated whole particle vaccines induced CTL responses in mice.
In many studies, CD8+ T-cell responses against influenza virus infection are analysed by means of an in vitro chromium release assay, MHC class I–peptide tetramer staining, and intracellular cytokine staining.16,17 However, the chromium release assay is usually preceded by an in vitro culture restimulation step before the assay and intracellular cytokine staining also requires culture to induce the accumulation of cytokines. Tetramer staining indicates the frequency of cells that express T-cell receptors (TCR) specific for antigens but does not demonstrate their function. In contrast, an in vivo killing assay is able to directly demonstrate CTL function in the vaccinated host.18 These factors may contribute to the conflicting nature of reports on the ability of formalin-treated virus to elicit cell-mediated immunity. Therefore, we examined CTL responses using the in vivo CTL killing assay.
Here we used an apathogenic reassortant strain obtained from migratory ducks as a vaccine strain and determined the formulation of an influenza virus vaccine that induced both CTL and antibody responses. We demonstrate that whole particle vaccines of apathogenic H5N1 influenza viruses induce in vivo CTL responses and antibodies specific for viral antigens more effectively than ether-split vaccines lacking whole viral particles. In addition, the immune responses induced by the whole particle vaccine of apathogenic reassortant H5N1 virus protected immunized mice from lethal H5N1 highly pathogenic avian influenza virus infections more effectively than did the ether-split vaccine. These results suggested that the formulation of antigens affected CTL activation and antibody production and that the whole particle vaccines of apathogenic influenza viruses might be promising against highly pathogenic avian influenza virus infections and a potential human pandemic.19
Materials and methods
Influenza viruses and vaccines
An influenza A virus, A/Aichi/2/68 (H3N2) [Aichi (H3N2)], was prepared from the culture supernatant of infected Madin–Darby canine kidney (MDCK) cells.20 A genetic reassortant influenza virus, A/R(duck/Mongolia/54/01–duck/Mongolia/47/01) (H5N1) [R (Mong-Mong) (H5N1)] (National Center for Biotechnology Information taxonomy database ID: 376899), was generated by mixed infection with A/duck/Mongolia/54/01 (H5N2) and A/duck/Mongolia/47/01 (H7N1).21 A highly pathogenic avian influenza virus, A/Vietnam/1194/2004 (H5N1) [VN1194 (H5N1)] was prepared from the allantoic fluid of infected embryonated hen eggs. The viruses were propagated in the allantoic cavities of 10-day-old embryonated hen eggs at 35° for 36 to 48 hr. Then the viruses were purified by ultracentrifugation (112 500 g for 90 min) of allantoic fluid through a 10–50% sucrose density gradient. Formalin-inactivated vaccines were prepared with 0·1% formalin at 4° for a week. The purified fixed viruses were then suspended in phosphate-buffered saline (PBS). For preparation of ether-split vaccine, viruses were purified by ultracentrifugation in a 10–50% sucrose density gradient, the purified viruses were suspended in PBS, and an equal volume of ether was added to the purified viruses with 0·01% Tween-80 and stirred for 30 min at room temperature. The mixture was centrifuged, and the aqueous phase was collected, evaporated, and further treated with 0·1% formalin at 4° for 1 week. Inactivation of viruses in the vaccines was confirmed by the absence of detectable haemagglutination activity following inoculation of treated materials into embryonated eggs.12 The amount of whole particle or ether-split vaccines was indicated as that of the entire protein including HA and the other viral protein.
Immunization
C57BL/6 mice (B6) (6–10 weeks old) were obtained from Japan SLC, Inc., (Hamamatsu, Japan). Influenza virus vaccines in 100 μl saline were inoculated subcutaneously (s.c.) into mice. In some experiments, mouse interferon-α (IFN-α; PBL Medical Laboratories, New Brunswick, NJ) or CpG5002 (5′-TCCATGACGTTCTTGATGTT-3′, Hokkaido System Science, Sapporo, Japan22) was s.c. inoculated with the vaccines into mice. In some experiments, vaccines in an emulsion with complete Freund's adjuvant (CFA; Difco Laboratories, Detroit, MI) were s.c. injected into mice. A live influenza virus, Aichi (H3N2) [104 plaque-forming units (PFU)], was inoculated either s.c. (in 100 μl PBS) or intranasally (i.n.) (in 15 μl PBS) into mice. A highly pathogenic avian influenza virus VN1194 (H5N1) [3 × 104 50% tissue infectious dose (TCID50) = 100 × 50% lethal dose (LD50)], was i.n. (in 30 μl PBS) inoculated into mice. We had confirmed that 15 and 30 μl of solution reached the lungs via the nasal cavity. All experiments were performed with the approval of the Shiga University of Medical Science or Hokkaido University Animal Experiment Committee.
In vivo CTL assay
Spleen cells (2 × 107 cells/ml) from naïve B6 mice were incubated with 0·5 μm OVA257-264 peptide (SIINFEKL) or influenza virus nucleoprotein (NP) NP366-374 peptide (ASNENMDAM for H3N2 or ASNENMETM for H5N1) for 2 hr at 37°. After washing twice with PBS, the recovered cells (2 × 107 cells/ml) were labelled with different concentrations of carboxyfluorescein diacetate succinimidyl ester (CFDA-SE/CFSE) (0·25 μm or 2·5 μm, Molecular Probes, Eugene, OR) at room temperature for 10 min. Labelling was stopped with one half volume of fetal calf serum (FCS) followed by two additional washes. Five million cells carrying each peptide were mixed and injected intravenously (i.v.) into immunized mice. At 14 hr after injection, the spleens were harvested to prepare single cell-suspensions and CFSE-positive cells were analysed by flow cytometry with exclusion of dead cells by propidium iodide or ethidium monoazide bromide (Molecular Probes) staining. Nucleoprotein-specific killing was calculated as follows: specific killing (%) = {1 – [(number of cells carrying NP366-374 in immunized mice (CFSE high))/(number of cells carrying OVA257-264 in immunized mice (CFSE low))]/[(number of cells carrying NP366-374 in normal mice (CFSE high))/(number of cells carrying OVA257-264 in normal mice (CFSE low))]} × 100.18 Statistical significances were calculated using the two-tailed Student's t-test.
Chromium release assay
Eight days after the second immunization with vaccines in the absence of adjuvant, the primed splenocytes of B6 mice were cultured with interleukin-2 (1 ng/ml) and 30-Gy irradiated syngeneic spleen cells preloaded with NP366-374 peptides (5 μm) in RPMI-1640 supplemented with 10% FCS and 50 μm 2-mercaptoethanol at 37° for 5 days and then used as effector cells. Target cells were labelled with Na251CrO4 (Perkin-Elmer, Boston, MA) and NP/OVA peptide (5 μm) for 90 min at 37°; then 104 target cells were added to serially diluted effector cells in 96-well U-bottom plates. After a 5-hr incubation at 37°, the supernatants were harvested and counted in a gamma counter. The specific lysis of target cells was determined as follows: specific lysis (%) = [(experimental release – spontaneous release)/(maximum release – spontaneous release)] × 100.23,24
Virus titration
MDCK cells were cultured in Eagle's minimal essential medium (MEM) supplemented with 10% FCS, l-glutamine and antibiotics. Diluted suspensions of lung tissue homogenates were added onto confluent MDCK cell monolayers in six-well plates and incubated at room temperature for 1 hr for adsorption. The suspension was removed and cells were covered with MEM containing 1% agar and 5 μg/ml trypsin (Difco Laboratories). After incubation at 35° for 2 days, the plaque number was counted. The limit of detection in this assay was 0·5 × 103 PFU/g.25
Enzyme-linked immunosorbent assay (ELISA)
ELISA was performed by a previously reported method with modifications.26 Briefly, 96-well plates were coated with 50 μl purified Aichi (H3N2) or R (Mong-Mong) (H5N1) (20 μg/ml) disrupted with 0·05 m Tris–HCl (pH 7·8) containing 0·5% Triton X-100 and 0·6 m KCl.12 After washing three times with PBS containing 0·05% Tween-20, PBS with 3% BSA was added for blocking. Serially diluted sera were incubated overnight in the coated plates. After washing five times, biotinylated anti-immunoglobulin G1 (IgG1; clone A85-1) or anti-IgG2a (clone R19-15) (BD Biosciences, San Jose, CA) (0·5 μg/ml × 50 μl) was added and the plates were incubated for 3 hr. After five further washes, horseradish peroxidase-conjugated Extravidin (Sigma-Aldrich, St. Louis, MO) (1/3000 × 100 μl) was added and incubation was continued for 3 hr. To measure total IgG, horseradish peroxidase-conjugated rabbit anti-mouse IgG (Bio-Rad Laboratories, Hercules, CA) (1/2000 × 50 μl) was used. Horseradish peroxidase activity was assessed by 3,3′,5,5′′-tetramethyl benzidine substrate (100 μl). The reaction was stopped by 1 m HCl (100 μl). Optical density was measured at 450 nm.
Virus neutralization assay and haemagglutination inhibition (HI)
Sera from immunized mice were pretreated with receptor-destroying enzyme (RDEII; Denka Seiken, Tokyo, Japan). For neutralization, serially diluted sera were mixed with 200 TCID50 of VN1194 (H5N1) for 1 hr. The mixture was then added onto an MDCK cell monolayer in 96-well plates. After 1 hr of incubation, medium was added and cells were cultured for 3 days. Neutralization titres were determined by calculating the highest concentration of serum showing 50% inhibition of cytopathic effects. For the HI test, serially diluted sera were mixed with 16 HA units of virus antigen for 1 hr at room temperature. The mixture was then incubated with chicken red blood cells. After 30 min incubation, HI titres were determined.
Flow cytometry
Cells from immunized mice were stained with phycoerythrin-conjugated Db-NP366-374 (ASNENMDAM) pentamer (ProImmune Ltd, Oxford, UK) at the manufacturer's recommendation. Thereafter, surface CD8 was stained with fluorescein isothiocyanate-conjugated antibody (eBioscience, San Diego, CA). After washing and lysing the red blood cells, cells were stained with ethidium monoazide bromide (Molecular Probes). After cells were fixed with 4% paraformaldehyde, cells were analysed with a flow cytometer.
Results
Live viruses induce nucleoprotein-specific CTL responses in vivo
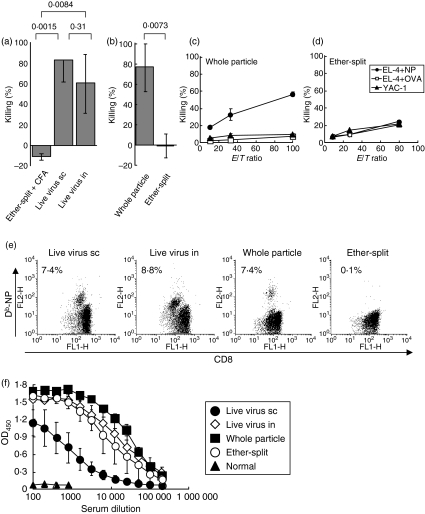
We first examined whether standard inactivated vaccines induced CTL responses specific for influenza viruses as assessed in vivo rather than in vitro, as more commonly performed. B6 mice were immunized s.c. with an H3N2 ether-split vaccine in an emulsion with CFA to enhance the responses. Thereafter, CTL responses specific for NP were estimated by injecting CFSE-labelled target cells carrying NP366-374 peptide, which is a well-characterized epitope in H-2b mice.17 NP366-374-specific killing was not observed in such immunized mice. In contrast, NP366-374-specific CTL responses were seen in mice inoculated s.c. or i.n. with live H3N2 influenza viruses (Fig. 1a). Therefore, the live viruses were a potent stimulator for CTL responses in vivo, as previously demonstrated.10,11
Figure 1.
In vivo cytotoxic T-lymphocyte responses against target cells carrying nucleoprotein (NP) peptide and antibody responses specific for H3N2 viral antigens in mice immunized with H3N2 live influenza viruses or inactivated vaccines. (a) B6 mice were injected subcutaneously (s.c.) or intranasally (i.n.) with live influenza virus Aichi (H3N2) (104 PFU) or s.c. with ether-split vaccines (100 μg). The vaccine was injected in an emulsion with CFA. Seven days after the immunization, syngeneic spleen cells pulsed with NP366-374 or OVA257-264 were injected intravenously (i.v.) as target cells. After 14 hr, killing specific for NP366-374 was analysed in the spleen. (b) B6 mice were s.c. immunized with whole particle or ether-split H3N2 vaccine (100 μg) without adjuvant twice with a 1-week interval between injections. Averages and standard deviations of three mice in each group are shown. P values were calculated by Student's t-test. (c, d) B6 mice were s.c. immunized with H3N2 whole particle vaccines (c) or ether-split vaccines (d) without adjuvant as described above. Eight days after the second immunization, primed spleen cells were cultured with syngeneic spleen cells carrying NP366-374. After 5 days of culture, antigen-specific cytotoxicity was assessed by a 51Cr release assay at the indicated effector-to-target cell (E : T) ratio. EL-4 plus NP366-374 and EL-4 plus OVA257-264 were used as specific and non-specific target cells, respectively. YAC-1 was used to assess natural killer cell activity. Data are presented as averages and standard deviations of triplicates. (e, f) B6 mice were inoculated with live Aichi (H3N2) (104 PFU) s.c. or i.n. Blood was collected from the mice 2 weeks after infection. B6 mice were s.c. immunized with whole particle or ether-split H3N2 vaccine (100 μg) without adjuvant twice with a 1-week interval between injections. Blood was collected from the mice 1 week after the second immunization. (e) Blood cells were stained with anti-CD8 and Db-NP366-374. CD8+ cells were shown in the dot plots and the percentage of NP-specific cells in CD8+ cells was indicated as averages of two or three mice. (f) Diluted serum was incubated with H3N2 viral antigens. IgG was determined with ELISA. Averages of OD450 absorption and standard deviations of three mice in each group are shown.
Whole virus particle vaccines of H3N2 influenza viruses inactivated by formalin-induced nucleoprotein-specific CTL responses in vivo and protection against influenza viral replication
Despite the induction of CTL responses, live-attenuated vaccines of influenza viruses are not used for aged or immunocompromised individuals because of the risk of complications.27 Therefore, we searched for inactivated vaccines, other than an ether-split vaccine, that were capable of inducing both CTL and antibody responses. B6 mice were immunized twice s.c. with an equivalent protein amount of whole particle or ether-split vaccines of H3N2 virus without adjuvant and CTL responses specific for NP were analysed in vivo. Target cells carrying NP366-374 were killed more effectively in mice immunized with whole particle vaccines than in mice immunized with ether-split vaccines (Fig. 1b). The NP-specific target lysis was confirmed by a chromium release assay in which spleen cells from mice immunized with whole particle vaccines, but not from mice immunized with ether-split vaccines, specifically killed target cells carrying NP366-374 (Fig. 1c,d).
Staining with the Db-NP pentamer indicated that immunization with whole particle vaccines without adjuvant augmented a comparable level of NP-specific CD8+ T cells to infection with live virus i.n. and s.c. (Fig. 1e). In contrast, ether-split vaccines augmented very few NP-specific CD8+ T cells. These results were correlated to the CTL activities in vivo and in vitro.
Serum IgG production specific for H3N2 influenza viruses induced by whole particle vaccines was compared to that induced by ether-split vaccines. Whole particle vaccines induced more potent virus-specific IgG responses than did ether-split vaccines or live virus at the time-point of 2 weeks after the initial immunization (Fig. 1f). Intranasal infection of virus induced more potent virus-specific IgG than s.c. infection, probably because of replication of virus in airway. Therefore, whole particle vaccines of H3N2 virus induced both cellular and humoral immune responses more effectively than did ether-split vaccines.
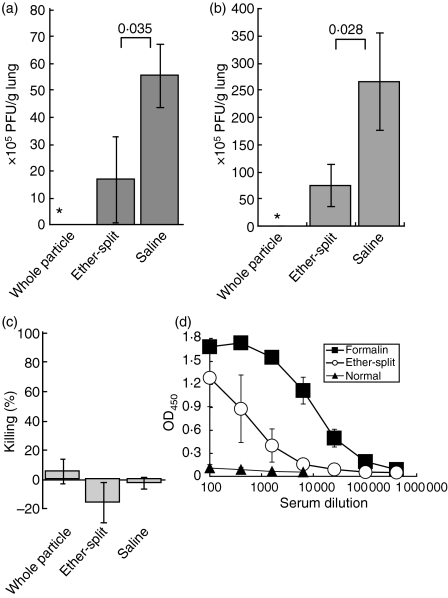
We next examined whether the immune responses induced by whole particle vaccines were sufficient to protect from influenza virus infection. B6 mice were immunized with the whole particle vaccines in the absence of adjuvant as described in Fig. 1(b). One week after the last immunization, the mice were inoculated i.n. with the influenza virus Aichi (H3N2). Five days after the infection, plaque-forming units in the lungs were counted. The whole particle vaccine inhibited viral replication (Fig. 2a). Although the ether-split vaccine did not induce CTL activity, it was able to reduce viral replication compared with the saline control, although not nearly as completely as the whole particle vaccine. Furthermore, on day 2 after virus challenge, even 5 months after the last vaccination, virus was not detected in the lungs of mice immunized with whole particle vaccines, whereas a small amount of virus was detected in the lungs of mice immunized with ether-split vaccines (Fig. 2b). At this time, CTL activities in vivo were not detected in mice immunized with vaccines, indicating that memory CTL was not reactivated on day 2 after the challenge (Fig. 2c). In contrast, virus-specific IgG was detected in the sera of mice immunized with whole particle or ether-split vaccines 5 months after vaccination, although the IgG titre induced by ether-split vaccines 5 months after vaccination was lower than that 1 week after vaccination (Figs 1f and 2d). These results suggest that the antibody response, but not CTL responses, induced by vaccination contribute mainly to inhibit viral replication at least in H3N2 virus infection or in the case that a vaccine strain is closely related to a challenge strain.
Figure 2.
Prevention of influenza virus replication by formalin-inactivated whole particle vaccines. B6 mice were s.c. immunized with whole particle or ether-split H3N2 vaccines (100 μg) without adjuvant twice with a 1-week interval between injections. Control mice were injected with saline. (a) Seven days after the second immunization, Aichi (H3N2) (104 PFU) in 15 μl PBS was inoculated i.n. Five days after infection, viral titres in the lungs were examined by a plaque-forming assay. Virus was below the detection limit in the lungs of mice immunized with whole particle vaccines (*< 0·5 × 103 PFU/g lung). (b, c) Five months after vaccination, Aichi (H3N2) (104 PFU) was inoculated i.n. (b) Two days after infection, viral titres in the lungs were examined. (c) One day after infection, target cells carrying NP366-374 were injected i.v. for in vivo cytotoxic T-lymphocyte assay. Nucleoprotein (NP)-specific killing was analysed 14 hr after injection as described in Fig. 1. Averages and standard deviations of three mice in each group are shown. P-values were calculated by Student's t-test. (d) Diluted sera of mice vaccinated 5 months before were incubated with H3N2 viral antigens. The IgG was determined using ELISA. Averages of OD450 absorption and standard deviations of three mice in each group are shown.
CTL responses induced by H5N1 influenza virus vaccines
Next, we confirmed the effects of whole particle vaccines using H5N1 influenza virus vaccines. Because of the risks of incomplete inactivation and accidental infection during the preparation of vaccines, it might not be suitable to use highly pathogenic avian influenza viruses in vaccine production. Furthermore, it is difficult to expand the viruses in hen eggs because the viruses kill the embryos before they have grown sufficiently for vaccine preparation. Therefore, it was necessary to select vaccine strains taking safety and effective preparation into consideration. Thus, we used an apathogenic reassortant strain obtained from migratory ducks, R (Mong-Mong) (H5N1), as a vaccine strain.21
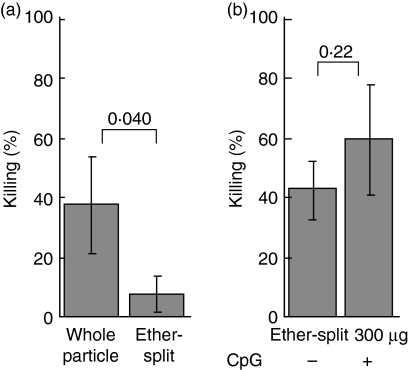
B6 mice were immunized s.c. with H5N1 vaccines without adjuvant and in vivo CTL assays were performed as described in Fig. 1(b). Ether-split vaccines alone induced weak CTL responses, whereas whole particle vaccines elicited more vigorous CTL responses (Fig. 3a). Thus, as seen with the H3N2 vaccine (Fig. 1b), particles were better able to induce CTL responses compared to the soluble antigens in ether-split vaccines.
Figure 3.
In vivo cytotoxic T-lymphocyte responses against targets carrying nucleoprotein peptide in mice immunized with inactivated H5N1 influenza viruses. (a) B6 mice were s.c. immunized with H5N1 vaccines (100 μg) without adjuvant twice with a 1-week interval between injections. (b) B6 mice were s.c. immunized with H5N1 ether-split vaccines (300 μg) twice with a 1-week interval with or without CpG (1 μg). One week after the last immunization, killing activity specific for NP366-374 was analysed in spleens. Three mice were used in each group. P-values were calculated by Student's t-test.
To determine whether the weak responses obtained with the ether-split vaccines were the result of the small dose used (100 μg/mouse), 300 μg of ether-split vaccine was administered to each B6 mouse (Fig. 3b). High-dose immunization induced better CTL responses to NP compared to the low-dose vaccination with this preparation. Therefore, the ineffective CTL induction seen with ether-split vaccines was not only caused by the formulation but also by the amount of antigen.
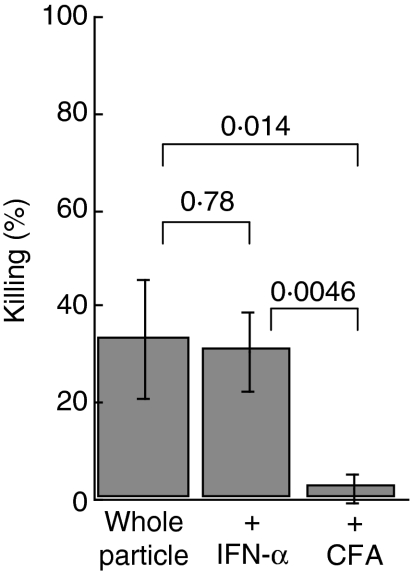
IFN-α and CFA do not enhance CTL responses in vivo
In an attempt to augment the CTL activity induced by the whole particle H5N1 vaccine, we added adjuvants to the preparation. IFN-α has been reported to work as an adjuvant when protein is used as an antigen.28,29 Therefore, we injected IFN-α with the whole particle vaccine s.c. However, administration of IFN-α did not enhance in vivo target killing responses with this vaccine (Fig. 4). We also used CFA as an adjuvant, but CFA with the whole particle vaccine actually inhibited the induction of NP-specific CTL responses.
Figure 4.
In vivo cytotoxic T-lymphocyte responses induced by whole particle vaccines with adjuvants. B6 mice were s.c. immunized with H5N1 whole particle vaccines (100 μg) twice with a 1-week interval between injections. Mouse IFN-α (2500 units) was co-administered in one group (middle column). The vaccine was injected in an emulsion with complete Freund's adjuvant (right column). Seven days after the second immunization, syngeneic target cells carrying NP366-374 or OVA257-264 were injected intravenously. After 14 hr, killing activity specific for NP366-374 was analysed in the spleens. Averages and standard deviations of three mice in each group are shown. P-values were calculated by Student's t-test.
Finally, we investigated the adjuvant activity of CpG oligonucleotides in combination with the whole particle or ether-split H5N1 vaccine. The addition of CpG showed tendency to enhance CTL activity in vivo but this was statistically insignificant (Fig. 3b and data not shown). Therefore, at present, CpG shows no advantage as adjuvant in inoculation with influenza virus vaccines.
Production of antibodies specific for H5N1 influenza virus induced by whole particle and ether-split vaccines
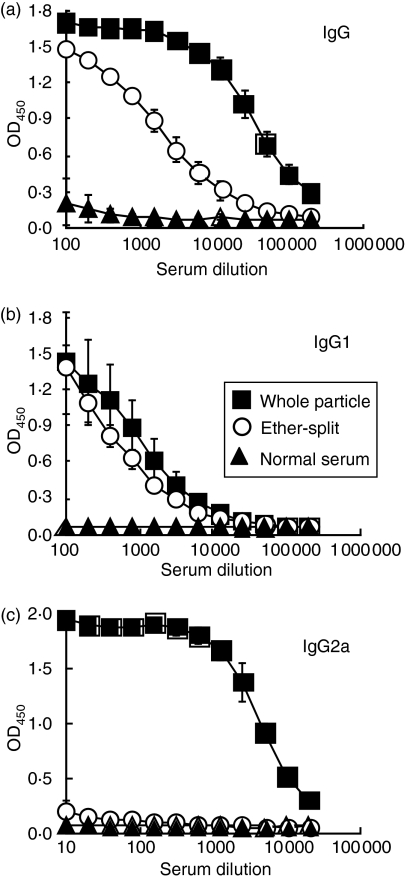
Serum IgG production specific for viral antigens of H5N1 influenza viruses induced by whole particle vaccines was compared with that induced by ether-split vaccines. Whole particle vaccines induced more potent virus-specific IgG responses than did ether-split vaccines (Fig. 5), especially IgG2a (Fig. 5c). This suggests that whole particle vaccines may induce T helper type 1 responses more effectively than ether-split vaccines.
Figure 5.
Antibody responses specific for H5N1 viral antigens in mice immunized with whole particle or ether-split vaccine. B6 mice were s.c. immunized with H5N1 whole particle vaccines or ether-split vaccines without adjuvant twice with a 1-week interval between injections, as described in Fig. 3. One week after the second immunization, sera were collected. Diluted sera were incubated with H5N1 viral antigens. IgG (a), IgG1 (b) and IgG2a (c) were determined by specific secondary antibodies. Averages of OD450 absorption and standard deviations of three mice in each group are shown.
We next examined whether antibodies induced by whole particle vaccines and ether-split vaccines had neutralizing activity. Sera were collected from mice that had been immunized with the whole particle vaccine or the ether-split vaccine, and then these sera were incubated with a highly pathogenic avian influenza virus VN1194 (H5N1). Fifty per cent neutralization titre showed that the whole particle vaccines induced more effective neutralizing antibody than did the ether-split vaccines (Table 1).
Table 1.
Neutralization of a highly pathogenic influenza virus (H5N1) with sera from immunized mice
| Vaccine | 50% neutralization titre (log2)1 | ||
|---|---|---|---|
| Exp. 1 | Exp. 2 | Exp. 3 | |
| Whole particle2 | 1·00 | 0·83 | 0·83 |
| Ether-split | <0 | <0 | <0 |
B6 mice were immunized as described in Figs 3 and 5. Sera were collected from three mice in each experiment. Diluted sera were incubated with a highly pathogenic influenza virus VN1194 (H5N1).
Average and standard deviation of 50% neutralization titres of sera from mice immunized with whole particle vaccines is 0·89 ± 0·098. P-value is less than 0·01 between whole particle and ether-split vaccines with Student's t-test when 50% neutralization titres of sera derived from mice immunized with ether-split vaccines are calculated as 0.
Because neutralization titres were low against the VN1194 (H5N1) strain (Table 1), an HI assay was performed to confirm the reactivity of sera with HA of immunogen. In a comparison between two virus strains, sera from immunized mice showed higher HI titres with immunogen R (Mong-Mong) (H5N1) than with VN1194 (H5N1) (Table 2). In addition, sera from mice immunized with whole particle vaccines showed higher HI titres than did sera from mice immunized with ether-split vaccines against both R (Mong-Mong) (H5N1) and VN1194 (H5N1). Therefore, the lower activity of neutralization and HI against the VN1194 strain was based on cross-reaction affected by the differences in amino acids between these two strains.
Table 2.
Haemagglutination inhibition with sera from immunized mice
| Vaccine | HI titre1 | |||||
|---|---|---|---|---|---|---|
| R (Mong-Mong)2 | VN11943 | |||||
| Exp. 1 | Exp. 2 | Exp. 3 | Exp. 1 | Exp. 2 | Exp. 3 | |
| Whole particle | 128 | 64 | 64 | 64 | 16 | 16 |
| Ether-split | 2 | 16 | 32 | 2 | 4 | 8 |
B6 mice were immunized as described in Figs 3 and 5. Sera were collected from three mice in each experiment. Diluted sera were incubated with HA antigen of R (Mong-Mong) or a highly pathogenic influenza virus VN1194 (H5N1).
Averages and standard deviations of HI titres against R (Mong-Mong) are 85·3 ± 37·0 and 16·7 ± 15·0 using sera from mice immunized with whole particle vaccines and ether-split vaccines, respectively. P-value is 0·04 between whole particle and ether-split vaccines with Student's t-test.
Averages and standard deviations of HI titres against VN1194 are 32·0 ± 27·7 and 4·67 ± 3·06 using sera from mice immunized with whole particle vaccines and ether-split vaccines, respectively. P value is > 0·05 between whole particle and ether-split vaccines with Student's t-test.
Prevention of a highly pathogenic avian influenza virus infection in mice immunized with whole particle vaccines of an apathogenic H5N1 virus
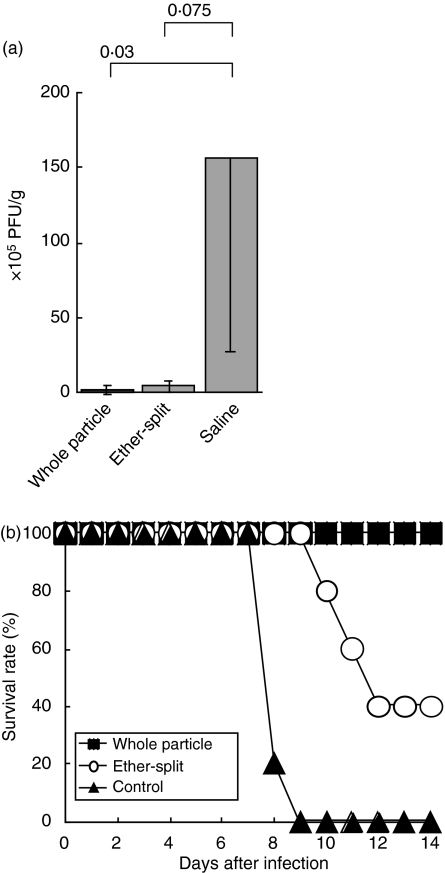
Finally, we examined whether the whole particle vaccine derived from an apathogenic H5N1 influenza virus protected against lethal infection with a highly pathogenic avian influenza virus. B6 mice were s.c. injected with vaccines of R (Mong-Mong) (H5N1) without adjuvant as described in Figs 3 and 5. Eight weeks after the last vaccination, mice were challenged with VN1194 (H5N1) i.n. using a dose 100 times higher than the mean lethal dose (100 × LD50). Five days after infection, plaque-forming units in the lungs were counted. The whole particle vaccine significantly inhibited viral replication (Fig. 6a). The ether-split vaccine reduced viral replication compared with the saline control, although the difference was not statistically significant.
Figure 6.
Survival of mice immunized with whole particle or ether-split vaccines after challenge with a highly pathogenic H5N1 virus. B6 mice were subcutaneously (s.c.) immunized with H5N1 whole particle vaccines or ether-split vaccines without adjuvant twice with a 1-week interval between injections as described in Figs 3 and 5. Saline was used for control mice. Either 8 weeks (a) or 1 week (b) after the second immunization, all mice were challenged i.n. with 100 × LD50 of VN1194 (H5N1) in 30 μl PBS. (a) Five days after infection, viral titres in the lungs were examined by a plaque-forming assay as described in Fig. 2. (b) Protective effects of vaccines were shown as the per cent survival of mice immunized with vaccines. Four or five mice were used in each group.
Furthermore, 1 week after the last immunization, VN1194 (H5N1) was inoculated i.n. with 100 × LD50. Control mice died within 9 days after challenge, whereas all the mice immunized with the whole particle vaccines survived until the end of the experiment (Fig. 6b). Two out of five mice survived after immunization with the ether-split vaccines. Therefore, the ether-split vaccines showed partial protection, but were clearly less effective than whole particle vaccines. Since the ether-split vaccines did not induce measurable neutralizing antibodies (Table 1), weak CTL responses against NP might partially contribute to the protective immunity against highly pathogenic avian influenza virus infection, but not be sufficient for prevention.
Overall, these results indicate that whole particle vaccines derived from an apathogenic strain induced both CTL and antibody responses effectively and protected from lethal H5N1 influenza virus infection.
Discussion
Both antibodies and CTL specific for highly pathogenic avian influenza viruses are likely to be important for resistance because these virus strains replicate not only in the upper respiratory tract but also in the lung and intestine.4,5 Therefore, an ideal vaccine against highly pathogenic avian influenza viruses should induce durable CTL and antibody responses both systemically and locally.30 In the present study, we showed that whole particle vaccines induced both CTL and antibody responses specific for influenza viruses. CTL responses were induced more effectively by whole particle vaccines than by ether-split vaccines when the ether-split vaccines were used in an amount equivalent to that of the whole particle vaccines. This suggests that the formulation of vaccines, using particle or soluble protein, is critical to the effective priming of CTL precursors. Furthermore, the ether-split vaccines commonly used in humans contain no adjuvant to reduce the possibility of detrimental side effects. The whole particle vaccine against H5N1 influenza virus does not require an adjuvant to elicit CTL responses, making it practical for human use.
In previous studies, it was demonstrated that inactivated vaccines against influenza viruses, including whole particle vaccines, induced antibodies specific for the virus but not effective CTL responses.7,31,32 However, in the present study, whole particle vaccines against influenza viruses induced CTL responses compatible with the results using the other whole particle viruses including the H1N1 subtype,13,14 and even ether-split vaccines elicited CTL responses at a high dose. Therefore, the difference between our data and those from other studies might be dependent on the dose of vaccine used. This suggests that the dose of vaccine can be reduced when we use whole particle vaccines instead of ether-split vaccines.
Although both CTL and antibody responses contribute to the clearance of influenza virus,7–9 the presence of specific antibody against Aichi (H3N2) without CTL activity, which is seen immediately after a challenge infection given several months after vaccination, protected against homotypic strain infection. These results indicated that antibody responses might be more critical for the prevention of virus growth than CTL responses (Fig. 2). However, the low neutralization titre against the challenge strain VN1194 (H5N1) in sera from mice immunized with H5N1 vaccines suggests that CTL responses might have a crucial role in protection from lethal infection with highly pathogenic strains or infection with strains with low homology with vaccine strains.
It is tempting to speculate that whole particle vaccines induced CTL responses more effectively than ether-split vaccines because of the key role of antigen-presenting cells (APC), especially dendritic cells, in the activation of CTL precursors. First, the whole particles might be acquired by the APC more effectively than ether-split vaccines, as previously demonstrated using heat-inactivated whole particle vaccines.13 Antigen acquisition with the whole particles by the APC might increase the amount of presented peptides derived from viral internal protein, such as NP. In addition, it was reported that heat-inactivated viral particles did not show haemagglutination activity but the antigens derived from the particles were still presented on the APC effectively. On the other hand, formalin-inactivated whole particle vaccines maintained haemagglutination activity.13 Therefore, it might be possible that formalin-inactivated whole particle vaccines were more easily incorporated into the APC using HA-sialic acid interaction than were the ether-split vaccines. We are now examining this issue.
Second, maturation of dendritic cells by stimulation with Toll-like receptor (TLR) ligands is required for optimal activation of naïve CD8+ T cells. There is a possibility that whole particle vaccines might stimulate plasmacytoid dendritic cells to induce the production of type I IFN in a TLR-dependent manner and indirectly activate myeloid dendritic cells and CTL precursors because ultraviolet-inactivated influenza virus induced IFN-α production in plasmacytoid dendritic cells.33 On the other hand, CpG oligonucleotides, a ligand of TLR9, did not show significant enhancement of CTL responses when using whole particle vaccines. This might be the result of the presence of natural adjuvants in these vaccines. Influenza viruses have been reported to contain single-stranded and partially double-stranded RNA.34,35 Therefore, whole particle vaccines might have a capacity to stimulate TLRs and enhance cross-priming compared with ether-split vaccines.
CTL responses specific for NP were inhibited when we used CFA as an adjuvant. Suppressive effects of CFA on CTL responses have been described in some reports.36–38 CFA increases the number of Mac-1+ cells but reduces the number of CD4+ cells and downregulates CTL activities.36 Furthermore, LPS-activated B cells inhibit Th1 responses.38 In addition, when we immunized with whole particle vaccines in the presence of CFA, IgG1 responses but not IgG2a responses were enhanced in contrast with immunization with whole particle vaccines alone (unpublished data). Further studies are needed to discover appropriate adjuvants to induce dendritic cell maturation in combination with whole particle vaccines to elicit more effective CTL responses for inhibiting virus replication and spread.
In the present study, we have also provided some new insight into the generation of influenza vaccine strains. Vaccines derived from reassortant viruses without the procedure of reverse genetics worked as effective vaccines. The vaccine strain used in the present study was a reassortant virus derived from H5N2 and H7N1 viruses because an antigenically related and non-highly pathogenic virus was not available from human or avian isolates. To extend this strategy to the other strains, such as highly pathogenic H7N7 viruses, we have isolated 49 viruses carrying different combinations of HA and neuraminidase (AN) subtypes to prepare a reassortant virus library with the other combinations.39 Thus, we would select vaccine strains from a set of viruses with 135 theoretical combinations of 15 HA and nine NA to prepare for any genetic reassortants (antigenic shifts).
In this study, vaccines derived from apathogenic strains of ducks induced protective immunity against a highly pathogenic avian influenza virus strain isolated from a human. There are amino acid sequence homologies between the vaccine strain (R (Mong-Mong)(H5N1)) and the challenge strain (VN1194 (H5N1)) we employed, such as 92% in HA (gene accession numbers BAE96567 and AAT73273), 90% in NA (BAE96569 and AAT73327), and 98% in NP (BAE96568 and AAT70629) (calculation using BLAST 2 sequences, National Center for Biotechnology Information). The whole particle vaccines might induce qualitatively and quantitatively sufficient immune responses for host protection based on cross-reaction. In addition, use of apathogenic strains for vaccines might not have the disadvantages such as rapid death of embryos, a low yield of viral recovery, or a requirement of higher biosafety level in vaccine preparation. Therefore, it might not be necessary that vaccine strains for human application are derived from viruses that spread in humans. Since it is not possible to perform challenge trials in humans with highly pathogenic avian influenza viruses, we are now trying to validate the utility of our approach by trying whole particle vaccines of apathogenic H5N1 viruses in non-human primates followed by challenge experiments with a highly pathogenic avian influenza virus.
Acknowledgments
We thank Dr Ronald N. Germain for discussions and for reading this manuscript, and Drs Yoshihiro Sakoda and Hidefumi Kojima for giving us instruction on viral experiments and a chromium release assay, respectively. This work was supported by the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases, MEXT Japan and Northern Advancement Center for Science and Technology.
Abbreviations
- APC
antigen-presenting cell
- CFA
complete Freund's adjuvant
- CFSE
carboxyfluorescein diacetate succinimidyl ester
- CpG
cytosine-phosphate-guanine
- CTL
cytotoxic T lymphocyte
- FCS
fetal calf serum
- HA
haemagglutinin
- HI
haemagglutination inhibition
- IFN
interferon
- IgG1
immunoglobulin G1
- i.v.
intravenously
- MDCK
Madin–Darby canine kidney
- MEM
minimal essential medium
- MHC
major histocompatibility complex
- NP
nucleoprotein
- OVA
ovalbumin
- PBS
phosphate-buffered saline
- PFU
plaque-forming unit
- s.c.
subcutaneous
- TCID50
50% tissue infectious dose
- TCR
T-cell antigen receptor
- TLR
Toll-like receptor
References
- 1.Doherty PC, Turner SJ, Webby RG, Thomas PG. Influenza and the challenge for immunology. Nat Immunol. 2006;7:449–55. doi: 10.1038/ni1343. [DOI] [PubMed] [Google Scholar]
- 2.Russell CJ, Webster RG. The genesis of a pandemic influenza virus. Cell. 2005;123:368–71. doi: 10.1016/j.cell.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 3.Stieneke-Grober A, Vey M, Angliker H, Shaw E, Thomas G, Roberts C, Klenk HD, Garten W. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoprotease. EMBO J. 1992;11:2407–14. doi: 10.1002/j.1460-2075.1992.tb05305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tran TH, Nguyen TL, Nguyen TD, et al. Avian influenza A (H5N1) in 10 patients in Vietnam. N Engl J Med. 2004;350:1179–88. doi: 10.1056/NEJMoa040419. [DOI] [PubMed] [Google Scholar]
- 5.Uiprasertkul M, Puthavathana P, Sangsiriwut K, et al. Influenza A H5N1 replication sites in humans. Emerg Infect Dis. 2005;11:1036–41. doi: 10.3201/eid1107.041313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pulendran B, Ahmed R. Translating innate immunity into immunological memory: implications for vaccine development. Cell. 2006;124:849–63. doi: 10.1016/j.cell.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 7.Reiss CS, Schulman JL. Cellular immune responses of mice to influenza virus vaccines. J Immunol. 1980;125:2182–8. [PubMed] [Google Scholar]
- 8.Eichelberger M, Allan W, Zijlstra M, Jaenisch R, Doherty PC. Clearance of influenza virus respiratory infection in mice lacking class I major histocompatibility complex-restricted CD8+ T cells. J Exp Med. 1991;174:875–80. doi: 10.1084/jem.174.4.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bender BS, Croghan T, Zhang L, Small PA., Jr Transgenic mice lacking class I major histocompatibility complex-restricted T cells have delayed viral clearance and increased mortality after influenza virus challenge. J Exp Med. 1992;175:1143–5. doi: 10.1084/jem.175.4.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armerding D, Rossiter H, Ghazzouli I, Liehl E. Evaluation of live and inactivated influenza A virus vaccines in a mouse model. J Infect Dis. 1982;145:320–30. doi: 10.1093/infdis/145.3.320. [DOI] [PubMed] [Google Scholar]
- 11.Blazevic V, Trubey CM, Shearer GM. Comparison of in vitro immunostimulatory potential of live and inactivated influenza viruses. Hum Immunol. 2000;61:845–9. doi: 10.1016/s0198-8859(00)00170-1. [DOI] [PubMed] [Google Scholar]
- 12.Takada A, Matsushita S, Ninomiya A, Kawaoka Y, Kida H. Intranasal immunization with formalin-inactivated virus vaccine induces a broad spectrum of heterosubtypic immunity against influenza A virus infection in mice. Vaccine. 2003;21:3212–8. doi: 10.1016/s0264-410x(03)00234-2. [DOI] [PubMed] [Google Scholar]
- 13.Cho Y, Basta S, Chen W, Bennink JR, Yewdell JW. Heat-aggregated noninfectious influenza virus induces a more balanced CD8+-T-lymphocyte immunodominance hierarchy than infectious virus. J Virol. 2003;77:4679–84. doi: 10.1128/JVI.77.8.4679-4684.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMichael AJ, Gotch F, Cullen P, Askonas B, Webster RG. The human cytotoxic T cell response to influenza A vaccination. Clin Exp Immunol. 1981;43:276–84. [PMC free article] [PubMed] [Google Scholar]
- 15.Mbawuike IN, Wyde PR. Induction of CD8+ T cells by immunization with killed influenza virus and effect of chorea toxin B subunit. Vaccine. 1993;11:1205–13. doi: 10.1016/0264-410x(93)90044-x. [DOI] [PubMed] [Google Scholar]
- 16.Belz GT, Wodarz D, Diaz G, Nowak MA, Doherty PC. Compromised influenza virus-specific CD8+-T-cell memory in CD4+-T-cell-deficient mice. J Virol. 2002;76:12388–93. doi: 10.1128/JVI.76.23.12388-12393.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turner SJ, Kedzierska K, Komodromou H, et al. Lack of prominent peptide–major histocompatibility complex features limits repertoire diversity in virus-specific CD8+ T cell populations. Nat Immunol. 2005;6:382–9. doi: 10.1038/ni1175. [DOI] [PubMed] [Google Scholar]
- 18.Nelson D, Bundell C, Robinson B. In vivo cross-presentation of a soluble protein antigen: kinetics, distribution, and generation of effector CTL recognizing dominant and subdominant epitopes. J Immunol. 2000;165:6123–32. doi: 10.4049/jimmunol.165.11.6123. [DOI] [PubMed] [Google Scholar]
- 19.Takada A, Kuboki N, Okazaki K, et al. Avirulent avian influenza virus as a vaccine strain against a potential human pandemic. J Virol. 1999;73:8303–7. doi: 10.1128/jvi.73.10.8303-8307.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogasawara K, Naruse H, Itoh Y, Gotohda T, Arikawa J, Kida H, Good RA, Onoé K. A strategy for making synthetic peptide vaccines. Proc Natl Acad Sci USA. 1992;89:8995–9. doi: 10.1073/pnas.89.19.8995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Isoda N, Sakoda Y, Kishida N, Bai G-R, Matsuda K, Umemura Kida H. Pathogenicity of a highly pathogenic avian influenza virus, A/chicken/Yamaguchi/7/04 (H5N1) in different species of birds and mammals. Arch Virol. 2006;151:1267–79. doi: 10.1007/s00705-005-0723-6. [DOI] [PubMed] [Google Scholar]
- 22.Nakamura I, Kajino K, Bamba H, Itoh F, Takikita M, Ogasawara K. Phenotypic stability of mature dendritic cells tuned by TLR or CD40 to control the efficiency of cytotoxic T cell priming. Microbiol Immunol. 2004;48:211–9. doi: 10.1111/j.1348-0421.2004.tb03508.x. [DOI] [PubMed] [Google Scholar]
- 23.Ito D, Ogasawara K, Iwabuchi K, Inuyama Y, Onoé K. Induction of CTL responses by simultaneous administration of liposomal peptide vaccine with anti-CD40 and anti-CTLA-4 mAb. J Immunol. 2000;164:1230–5. doi: 10.4049/jimmunol.164.3.1230. [DOI] [PubMed] [Google Scholar]
- 24.Kojima H, Kanno Y, Hase H, Kobata T. CD4+ CD25+ regulatory T cells attenuate the phosphatidylinositol 3-kinase/Akt pathway in antigen-primed immature CD8+ CTLs during functional maturation. J Immunol. 2005;174:5959–67. doi: 10.4049/jimmunol.174.10.5959. [DOI] [PubMed] [Google Scholar]
- 25.Ninomiya A, Ogasawara K, Kajino K, Takada A, Kida H. Intranasal administration of a synthetic peptide vaccine encapsulated in liposome together with an anti-CD40 antibody induces protective immunity against influenza A virus in mice. Vaccine. 2002;20:3123–9. doi: 10.1016/s0264-410x(02)00261-x. [DOI] [PubMed] [Google Scholar]
- 26.Kida H, Brown LE, Webster RG. Biological activity of monoclonal antibodies to operationally defined antigenic regions on the hemagglutinin molecule of A/Seal/Massachusetts/1/80 (H7N7) influenza virus. Virology. 1982;122:38–47. doi: 10.1016/0042-6822(82)90375-0. [DOI] [PubMed] [Google Scholar]
- 27.Bridges CB, Harper SA, Fukuda K, Uyeki TM, Cox NJ, Singleton JA. Advisory Committee on Immunization Practices. Prevention and control of influenza. Recommendations of the advisory committee on immunization practices (ACIP) MMWR Recomm Rep. 2003;52(1):34. quiz CE1-4. Erratum in MMWR Morb Mortal Wkly Rep 52:526. [PubMed] [Google Scholar]
- 28.Proietti E, Bracci L, Puzelli S, et al. Type I IFN as a natural adjuvant for a protective immune response: lessons from the influenza vaccine model. J Immunol. 2002;169:375–83. doi: 10.4049/jimmunol.169.1.375. [DOI] [PubMed] [Google Scholar]
- 29.Le Bon A, Etchart N, Rossmann C, Ashton M, Hou S, Gewert D, Borrow P, Tough D. Cross-priming of CD8+ T cells stimulated by virus-induced type I interferon. Nat Immunol. 2003;4:1009–15. doi: 10.1038/ni978. [DOI] [PubMed] [Google Scholar]
- 30.Seo SH, Peiris M, Webster RG. Protective cross-reactive cellular immunity to lethal A/Goose/Guangdong/1/96-like H5N1 influenza virus is correlated with the proportion of pulmonary CD8+ T cells expressing gamma interferon. J Virol. 2002;76:4886–90. doi: 10.1128/JVI.76.10.4886-4890.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sha Z, Compans RW. Induction of CD4+ T-cell-independent immunoglobulin responses by inactivated influenza virus. J Virol. 2000;74:4999–5005. doi: 10.1128/jvi.74.11.4999-5005.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ennis FA, Cruz J, Jameson J, Klein M, Burt D, Thipphawong J. Augmentation of human influenza A virus-specific cytotoxic T lymphocyte memory by influenza vaccine and adjuvanted carriers (ISCOMS) Virology. 1999;259:256–61. doi: 10.1006/viro.1999.9765. [DOI] [PubMed] [Google Scholar]
- 33.Lee HK, Lund JM, Ramanathan B, Mizushima N, Iwasaki A. Autophagy-dependent viral recognition by plasmacytoid dendritic cells. Science. 2007;315:1398–400. doi: 10.1126/science.1136880. [DOI] [PubMed] [Google Scholar]
- 34.Noda T, Sagara H, Yen A, Takada A, Kida H, Cheng RH, Kawaoka Y. Architecture of ribonucleoprotein complexes in influenza A virus particles. Nature. 2006;439:490–2. doi: 10.1038/nature04378. [DOI] [PubMed] [Google Scholar]
- 35.Cheong HK, Cheong C, Lee YS, Seong BL, Choi BS. Structure of influenza virus panhandle RNA studied by NMR spectroscopy and molecular modeling. Nucleic Acids Res. 1999;27:1392–7. doi: 10.1093/nar/27.5.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qin HY, Sadelain MW, Hitchon C, Lauzon J, Singh B. Complete Freund's adjuvant-induced T cells prevent the development and adoptive transfer of diabetes in nonobese diabetic mice. J Immunol. 1993;150:2072–80. [PubMed] [Google Scholar]
- 37.Ulaeto D, Lacy PE, Kipnis DM, Kanagawa O, Unanue ER. A T-cell dormant state in the autoimmune process of nonobese diabetic mice treated with complete Freund's adjuvant. Proc Natl Acad Sci USA. 1992;89:3927–31. doi: 10.1073/pnas.89.9.3927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tian J, Zekzer D, Hanssen L, Lu Y, Olcott A, Kaufman DL. Lipopolysaccharide-activated B cells down-regulate Th1 immunity and prevent autoimmune diabetes in nonobese diabetic mice. J Immunol. 2001;167:1081–9. doi: 10.4049/jimmunol.167.2.1081. [DOI] [PubMed] [Google Scholar]
- 39.Kida H, Sakoda Y. Library of influenza virus strains for vaccine and diagnostic use against highly pathogenic avian influenza and human pandemics. Dev Biol (Basel) 2006;124:69–72. [PubMed] [Google Scholar]