Abstract
Identifying the properties of a molecule involved in the efficient activation of the innate and adaptive immune responses that lead to long-lasting immunity is crucial for vaccine and adjuvant development. Here we show that the papaya mosaic virus (PapMV) is recognized by the immune system as a pathogen-associated molecular pattern (PAMP) and as an antigen in mice (Pamptigen). A single immunization of PapMV without added adjuvant efficiently induced both cellular and specific long-lasting antibody responses. PapMV also efficiently activated innate immune responses, as shown by the induction of lipid raft aggregation, secretion of pro-inflammatory cytokines, up-regulation of co-stimulatory molecules on dendritic cells and macrophages, and long-lasting adjuvant effects upon the specific antibody responses to model antigens. PapMV mixed with Salmonella enterica serovar Typhi (S. typhi) outer membrane protein C increased its protective capacity against challenge with S. typhi, revealing the intrinsic adjuvant properties of PapMV in the induction of immunity. Antigen-presenting cells loaded with PapMV efficiently induced antibody responses in vivo, which may link the innate and adaptive responses observed. PapMV recognition as a Pamptigen might be translated into long-lasting antibody responses and protection observed. These properties could be used in the development of new vaccine platforms.
Keywords: adjuvants, antigens, memory, papaya mosaic virus, vaccination
Introduction
The onset of the immune response against a given pathogen depends on the recognition of microbial components by non-clonal (innate) and clonal (adaptive) receptors expressed on the appropriate cells. Innate receptors known as pattern-recognition receptors (PRR) allow the recognition of microbial products known as pathogen-associated molecular patterns (PAMP).1 In contrast, the adaptive immune response is characterized by clonally expressed B-cell receptor (BCR) or T-cell receptor (TCR) recognition of molecules, which define the antigenicity of these molecules.2 The outcome of the immune response activated through these receptors is that protection or immunity (which may last for many years or a lifetime) is generated against the infecting pathogen3,4 and this phenomenon is the basis of vaccination. However, the immunological mechanisms mediating the induction of long-term immunity remain obscure.
High, long-lasting protective antibody titres are induced mainly after pathogenic infection, or by vaccination with an attenuated pathogen or with purified antigens mixed with adjuvants.5,6 Two key factors achieve this response. First, antigen immunogenicity depends on the antigen molecular nature and structure.2 Thus, viruses that infect mammals exhibit a quasicrystalline, highly organized surface with a regular array of epitopes that efficiently cross-link epitope-specific membrane immunoglobulins on B cells, inducing a T-cell-independent antibody response.7 Second, the presence of adjuvants increases the magnitude and duration of the immune response by activating the innate immune system.8 The adjuvant effect of most molecules depends on activation of the innate immune response through PRR.9 This opens the possibility that pattern recognition through the innate immune system could be responsible for shaping the long-lasting protective response induced by pathogens or vaccines.
Plant viruses are effective tools for antigen expression.10 Unlike conventional live attenuated or recombinant vaccines, plant viruses are considered non-pathogenic for mammals10 and fulfil the immunogenic properties described for mammal-infecting viruses. Thus, they represent an excellent non-infectious model for using to study immunogenicity and adjuvanticity. Our experimental model is the papaya mosaic virus (PapMV), a potexvirus that infects Carica papaya (papaya) leaves.11,12 The PapMV virion is a flexible rod, 500 nm long and 15 nm in diameter, composed of 1400 subunits of the viral coat protein (CP) assembled around the genomic positive single-stranded RNA.13 In this study, we show that a single immunization with PapMV in the absence of added adjuvant efficiently induced both cellular and specific long-lasting antibody responses. In addition, PapMV efficiently activated innate immune responses and, when used as an adjuvant for model antigens or for an experimental vaccine, promoted a long-lasting specific antibody response and increased the protective capacity of the experimental vaccine. We propose that this strong immunogenicity shown by PapMV is the consequence of its recognition both as a PAMP and as an antigen [pathogen-associated molecular pattern and antigen (Pamptigen)] by the immune system, thus translating the innate immune recognition into long-lasting antibody responses and protection. These properties could be used in the development of new vaccine platforms to support the induction of long-lasting immunity.
Materials and methods
Bacterial strains
The wild-type S. typhi strain was obtained from the American Type Culture Collection 9993 (ATCC, Manassas, VA). Isogenic Salmonella mutant strain STYF302 (ΔompF, Kanamycin resistance (KmR)), expressing OmpC, has been described previously.14,15
Antigens
PapMV was purified as described previously.16 Lipopolysaccharide (LPS)-free ovalbumin (OVA) grade VI was from Sigma-Aldrich (St Louis, MO, USA). Hen egg-white lysozyme (HEL) was from Research Organics Inc. (Cleveland, OH, USA). LPS was from Escherichia coli O111:B4 (Sigma-Aldrich). Outer membrane protein C (OmpC) was purified from S. typhi STYC302 (ΔompF, KmR), as described previously.15
Mice
BALB/c (Harlan, Mexico City, Mexico) and C3H/HeJ17 mice, 6–8 weeks of age, were housed in the animal facilities of the Experimental Medicine Department, Faculty of Medicine, UNAM, and were cared for in conformity with good laboratory practice guidelines. These studies were reviewed and approved by the IMSS National Scientific Research Committee (project no. 2005-785-016).
Immunizations
Groups of mice were immunized intraperitoneally (i.p.) on day 0 with 30 μg of PapMV diluted in sterile isotonic saline solution (saline) to a total volume of 0·5 ml. To study the effects of adjuvant, groups of mice were immunized i.p. on day 0 with 2 mg of OVA or HEL alone, or with 30 μg of PapMV and 2 mg of OVA or HEL in complete Freund's adjuvant (CFA) 1:1 (v/v) or with 5 μg of LPS from E. coli O111:B4 (Sigma-Aldrich). To study the adjuvant effect of PapMV in the anti-OmpC response, mice were immunized i.p. on day 0 with 10 μg of OmpC alone or with 30 μg of PapMV and 10 μg of OmpC in incomplete Freund's adjuvant (IFA) 1:1 (v/v). On day 15, mice received 10 μg of OmpC i.p. without adjuvant. Control mice were injected with saline or with 30 μg of PapMV only. Blood samples were collected at various time-points, as indicated in each figure. Individual serum samples were stored at −20° until analysis. The number of mice used in the experiment is indicated in the figure legends.
Determination of antibody titres by enzyme-linked immunosorbent assay
High-binding 96-well polystyrene plates (Corning, New York, NY, USA) were coated with 1 μg/ml of PapMV, 10 μg/ml of OmpC, 100 μg/ml of HEL or 150 μg/ml of OVA in 0·1 m carbonate–bicarbonate buffer (pH 9·5). Enzyme-linked immunosorbent assay (ELISA) was performed as described previously.15 Antibody titres are given as –log2 dilution × 40 or as the inverse of serum dilution. A positive titre was defined as three standard deviations (3 SD) above the mean value of the negative control.
Delayed-type hypersensitivity test
BALB/c mice were immunized subcutaneously (s.c.) in the footpad with 30 μg of wild-type PapMV, 30 μg of ultraviolet light-inactivated PapMV, buffer (Tris–HCl, pH 6·8) or sterile pyrogen-free saline solution. Seven days after immunization, mice were challenged by s.c. injection of 3 μg of PapMV into the right ear. Ear thickness was measured before the challenge and 24 hr after injection using a digital micrometer (Mituyoto, Tokyo, Japan).
Generation of bone marrow-derived macrophages
Bone marrow-derived macrophages (BMDM) were obtained from the femurs of BALB/c mice (6–8 weeks of age) and cultured in Dulbecco's modified Eagle's minimal essential medium (DMEM) with bone marrow medium [30% L cell-conditioned medium, 20% heat-inactivated fetal bovine serum (FBS) and 50% DMEM)], as described previously.18
Generation of bone marrow-derived dendritic cells
Bone marrow-derived dendritic cells (BMDC) were generated by 6 days of culture of BALB/c bone marrow cells with granulocyte–macrophage colony-stimulating factor (GM-CSF)-containing supernatant from the cell line X63-GM-CSF (kindly provided by Dr Antonius Rolink, University of Basel, Basel, Switzerland). Dendritic cells (DC) were further purified using Optiprep density-gradient centrifugation (Sigma-Aldrich Co., Basel, Switzerland). CD11c+ B220− cells were more than 95% pure when analysed by flow cytometry.
Peritoneal macrophage purification
Thioglycolate-elicited macrophages were collected from the peritoneal cavity of BALB/c mice, cultured at 1 × 106cells per well in DMEM (containing 10% FCS, l-glutamine 2 mM, penicillin 100 U/ml, streptomycin 100 μg/ml) overnight at 37°. Non-adherent cells were removed by washing with cold phosphate-buffered saline (PBS).
Lipid raft aggregation
Ten-thousand BMDM were cultured on sterile circular slides and stimulated for 30 min with 1 μg/ml of PapMV in 100 μl of DMEM. After the stimulus was removed, the slides were washed twice with PBS containing 2% FBS and once with PBS alone. The cells were fixed using 3% p-formaldehyde and incubated at 4° for 20 min. Cells were washed as described above. Cholera toxin B subunit (CTB) coupled to fluorescein isothiocyanate (FITC) (CTB–FITC, 1:500; Sigma-Aldrich) was added and the slides were incubated in the dark at room temperature. Non-specific binding sites were blocked with goat serum (1:100 dilution) for 1 hr at room temperature. After incubation, the slides were washed three times with PBS and then rat anti-PapMV (1:100 dilution) was added. The slides were incubated overnight at 4°. As an isotype control, mouse anti-PapMV (1:100) was used. The slides were washed three times with PBS and incubated for 1 hr at room temperature with tetramethylrhodamine isothiocyanate-tagged anti-rat IgG (1:200). The slides were washed three times with PBS, mounted and assessed using a confocal microscope (Zeiss Axiovert 100 M microscope with lsm510 expert mode software; Carl Zeiss, Aalen, Germany).
BMDM, peritoneal macrophage and BMDC stimulation, and determination of cytokine production
One-million BMDM, peritoneal macrophages or BMDC were stimulated with 1 μg/ml of PapMV or with 100 ng/ml of LPS from E. coli O111:B4 (Sigma-Aldrich). Unstimulated cells were used as a control. At the time-points indicated in the graphs, the culture supernatant was harvested and stored at −70° until analysis. Tumour necrosis factor-α (TNF-α) and interleukin (IL)-6 were quantified by ELISA (all OptEIA sets; BD Pharmingen, San Diego, CA, USA), following the manufacturer's instructions. The concentration of final reaction product was determined at 450 nm in an ELISA plate reader (Dynex Technologies MRII, Chantilly, VA) with biolinx 2.22 software (Dynex Technologies). The detection limit was 15·6 pg/ml for both cytokines. Mouse interferon-α (IFN-α) concentration in cell culture supernatants was measured using ELISA (PBL Biomedical Laboratories, NJ, USA) according to the manufacturer's instructions.
In vivo DC, macrophage and B-lymphocyte activation assay
BALB/c mice (7 weeks of age) were immunized i.p. with 30 μg of PapMV and 50 μg of Poly I:C suspended respectively in 500 μl of saline. Saline (500 μl) was used as a control, and 24 hr after immunization lymph nodes and spleens were obtained. Cell suspensions were prepared from these organs, and flow cytometry staining was performed using phycoerythrin (PE)–CD11c, allophycocyanin–CD11b, B220–peridinin chlorophyll protein (PerCP), FITC–CD80, FITC–CD86, FITC–CD40, FITC–CD69 and FITC–major histocompatibility complex class II (MHC class II) antibodies (all purchased from BD Pharmingen).
Transference of BMDM
BMDM were pulsed with 30 μg/ml of PapMV in 5 ml of DMEM containing 10% FBS and incubated for 3 hr at 37°. The supernatant was removed, the cells were washed four times with PBS, and, before harvesting, the last cell wash was collected. Totals of 104, 105 and 106 harvested cells were immediately transferred i.v. into BALB/c mice in a final volume of 300 μl. Culture supernatant, the last cell wash supernatant, 105 unstimulated BMDM and 30 μg of PapMV were suspended in a final volume of 300 μl and transferred i.v. into the control mice. The numbers of mice used are indicated in the figure legends.
Protection assay
BALB/c mice were immunized i.p. on day 0 with 10 μg of OmpC or 10 μg of OmpC that had been incubated previously for 1 hr with 30 μg of PapMV at 4°. A boost on day 15 was performed using 10 μg of OmpC only. Control mice were injected with saline or 30 μg PapMV alone. The challenge was performed on day 21 with 100 and 500 lethal dose 50% (LD50) of 5% mucin-suspended S. typhi, and the survival rate was registered for 10 days after the challenge, as described previously.19 The numbers of mice used are indicated in the figure legends.
B-cell activation and proliferation
One-million splenic B cells per well were incubated with PapMV (1 μg/ml) and harvested after 18 hr to assess the activation markers, and were harvested again after 80 hr to assess cell differentiation into plasma cells. LPS (10 μg/ml) from E. coli O111:B4 (Sigma-Aldrich) was used as a positive control. Flow cytometry staining was performed with CD44–FITC, MHC class II–PE, CD86–FITC, CD22–PE, CD138–PE and B220–allophycocyanin antibodies (BD Pharmingen). One-million cells were incubated for 15 min with a mixture of fluorescein-, PE- and allophycocyanin-conjugated antibodies. Cell proliferation was tested using fifty-million splenic cells suspended in 1 ml of PBS containing 1 μl of a 1 mm solution of 5(6)-carboxyfluorescein diacetate N-succinimidyl ester (CFSE) (Molecular Probes, Eugene, OR, USA). Cells were stimulated as described above. Data were acquired using a FACSCalibur (Becton Dickinson, San Jose, CA, USA) and analysed using cellquest software (Becton Dickinson).
Results
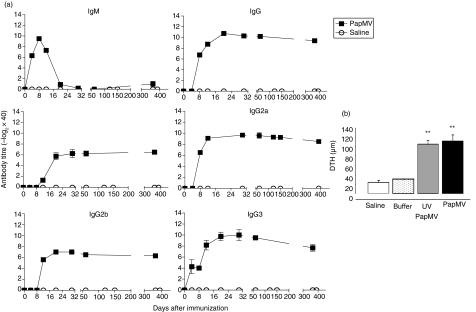
PapMV induces a long-lasting antibody immune response
B-cell activation is facilitated by antigenic organization and molecular repetitiveness (more than 20 subunits), as shown in a paracrystalline array.20 PapMV virions contain about 1400 copies of a single CP arranged in a helical form.21 We immunized BALB/c mice i.p. with 30 μg of PapMV and measured PapMV-specific antibody titres for 1 year. During the primary antibody response on day 8, we observed a 1024-fold increase in IgM titre and a 256-fold increase in IgG titre (Fig. 1a). In the absence of boosting, the IgM response decreased to the basal level on day 20 and remained there until day 365. In contrast, the IgG titre reached its maximum, a 1024-fold increase, around day 21 and remained at this level until the end of the experiment 1 year later. PapMV induced production of the four subclasses of IgG. The antibody titres of the IgG subclasses were observed first between days 4 and 12 and all reached their maximum values around day 20, where they remained until day 365 (Fig. 1a). Similar results were obtained when 50 μg of PapMV was used for immunization (data not shown). In addition, i.v. and s.c. immunization with PapMV induced similar antibody kinetics (data not shown). This antibody response was observed for 1 year after a single immunization without adjuvants.
Figure 1.
Papaya mosaic virus (PapMV) induces T-cell and long-lasting antibody immune responses. (a) Titres of anti-PapMV IgM and IgG, and of IgG subclasses IgG1, IgG2a, IgG2b and IgG3, were measured in female BALB/c mice immunized intraperitoneally (i.p.) with 30 μg of PapMV or with saline. Blood samples were collected at the time-points depicted. Results are expressed as the mean ± standard deviation (SD) of five mice per group. Data correspond to one representative result from five independent experiments. (b) T-cell responses were assessed by the delayed-type hypersensitivity (DTH) test. Groups of five female BALB/c mice were immunized subcutaneously (s.c.) in the footpad with 30 μg of wild-type PapMV or with 30 μg of ultraviolet light (UV) light-inactivated PapMV. Buffer (Tris–HCl, pH 6·8) alone or saline was used as a control. On day 7, the mice were challenged with 3 μg of PapMV administered s.c. in the ear. Ear thickness was measured using a micrometer before and 24 hr after injection. Means were analysed by the Student's t-test. Significant differences are indicated by asterisks: **P < 0·001. One representative result from two independent experiments is shown.
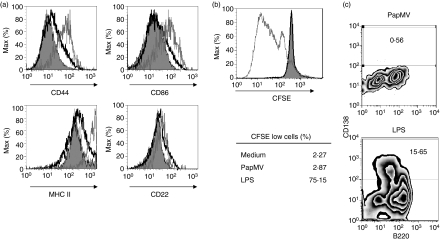
PapMV did not induce naïve B-lymphocyte proliferation in vitro (Fig. 2b); however, it induced minor up-regulation of activation markers such as CD44, CD86, CD22 and MHC class II (Fig. 2a). Additionally, PapMV induced in vivo up-regulation of CD69 and CD40 on B cells (Fig. 3). PapMV did not induce B-cell differentiation into plasma cells in vitro (Fig. 2c). The experiments were repeated by adding IL-4 to the PapMV stimulus or by using 30 or 50 μg/ml of PapMV (data not shown), confirming that PapMV did not activate B cells from naïve mice and did not prepare B cells for activation by IL-4. We conclude that PapMV is not a thymus-independent type 1 antigen. However, it induces some up-regulation of activation marker expression levels in B cells.
Figure 2.
Papaya mosaic virus (PapMV) did not induce in vitro naïve B-lymphocyte proliferation; however, it induced a small shift in the expression of activation markers on these cells. Flow cytometric analysis of B cells was performed after stimulation with PapMV. (a) Induction of B-cell activation markers. (b) B-cell proliferation. Naïve B cells were pulsed after 18 hr with 100 μg/ml of lipopolysaccharide (LPS) (grey solid line) or with 1 μg/ml of PapMV (black solid line); non-pulsed cells are shown by shading. (c) To assess B-cell differentiation into plasma cells induced by PapMV, cells were stimulated with the virus for 80 hr and stained for B220 and CD138. One representative result from three experiments is shown. CFSE, 5(6)-carboxyfluorescein diacetate N-succinimidyl ester.
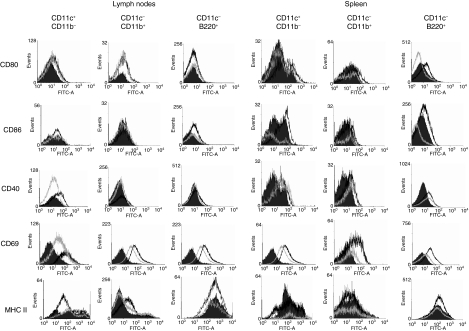
Figure 3.
Papaya mosaic virus (PapMV) induces co-stimulatory molecule up-regulation in dendritic cells (DC), macrophages and B cells in vivo. BALB/c mice were immunized intraperitoneally (i.p.) with 30 μg of saline-diluted PapMV (grey line) or with 50 μg of Poly I:C (black line), and control mice were injected with saline (filled histogram). Twenty-four hours after immunization, lymph nodes and spleen cells were collected and stained. Flow cytometry was performed to analyse cell populations defined as: CD11c+ CD11b− (DCs), CD11c− CD11b+ (macrophages) and CD11c− B220+ (B cells). A representative result of two experiments is shown. FITC, fluorescein isothiocyanate; MHC II, major histocompatibility complex class II.
To determine whether the antibody response observed was influenced by the presence of undetected traces of LPS or polysaccharides,22,23 which could have contaminated the PapMV preparation during purification, C3H/HeJ mice [an LPS hyporesponsive Toll-like receptor 4 (TLR-4) mutant strain] were immunized with 30 μg of PapMV. IgM and IgG titre kinetics were similar to those observed in BALB/c mice (data not shown). Thus, undetected contamination with TLR-4 ligands that could be present in the PapMV did not contribute to the antibody response observed. These results show that the PapMV is a strong immunogenic particle able to induce a sustained and specific long-lasting antibody response comprising all IgG subclasses.
PapMV-induced T-cell responses
The presence of all IgG subclasses revealed that T cells must help in the response induced by PapMV. A delayed-type hypersensitivity (DTH) test was performed to test the capacity of PapMV to induce systemic T-cell responses. Groups of five BALB/c mice were immunized s.c. with 30 μg of intact or UV-inactivated PapMV. UV-inactivated PapMV was used to control the influence of virus viability in the response observed, even though the plant virus replication machinery is not compatible with mammalian systems and plant viruses are non-pathogenic in mammals.10 PapMV and UV-inactivated PapMV induced a strong DTH response compared with the control (Fig. 1b). Thus, PapMV induced a strong T-cell response in addition to the sustained long-lasting antibody response. Taken together, these results show that PapMV is a highly immunogenic antigen for both the humoral and cellular immune responses.
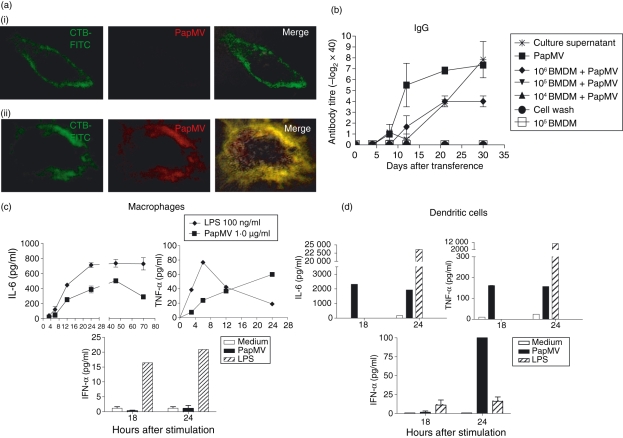
PapMV induces the aggregation of lipid rafts on BMDM
During the molecular recognition process on antigen-presenting cells (APC), a cluster of surface molecules present in lipid raft aggregates, allowing the induction of a signalling cascade to induce cell activation.24 To determine whether PapMV induces lipid raft aggregation, murine BMDM were stimulated with 1 μg/ml of PapMV for 30 min. The cells were then stained with cholera toxin subunit B coupled with FITC to target the lipid raft-resident glycolipid, GM1. PapMV stimulated the BMDM, which showed an increased aggregation of lipid rafts. Moreover, on these cells, PapMV co-localized with these aggregated lipid rafts (Fig. 4a panel ii). By contrast, lipid raft aggregation was not observed in unstimulated cells (Fig. 4a panel i). Aggregation was manifested as the accumulation of lipid rafts in localized regions of the stimulated cells, whereas FITC staining in unstimulated cells was homogenous around the cell periphery. These results suggest that PapMV is recognized at the surface of BMDM.
Figure 4.
Papaya mosaic virus (PapMV) efficiently activates antigen-presenting cells (APC) and these cells participate in the induction of the specific antibody response. (a) Aggregation of lipid rafts induced by PapMV. (i) Unstimulated cells. (ii) Cells pulsed with 1 μg/ml of PapMV. Original magnification ×100. (b) Bone marrow-derived macrophages (BMDM) pulsed with PapMV efficiently induced specific IgG titres. BMDM were stimulated with 30 μg/ml of PapMV and transferred intravenously (i.v.) to BALB/c mice. Non-pulsed cells, culture supernatant, final-wash supernatant and 30 μg of PapMV were injected i.v. as controls. The PapMV-specific IgG titres in mice sera were measured by enzyme-linked immunosorbent assay (ELISA) at the time-points depicted in the graph. Results are expressed as the mean ± standard deviation (SD) of six mice per group. Data correspond to one representative result from three independent experiments. (c,d) Production of inflammatory cytokines in macrophages and dendritic cells induced by 1 μg/ml of PapMV or by 100 ng/ml of lipopolysaccharide (LPS) from Escherichia coli UHO111 (as a positive control). Results are expressed as the mean ± SD of four wells per time chased. Data correspond to one representative result from three independent experiments. CTB, cholera toxin B subunit; FITC, fluorescein isothiocyanate; IFN-α, interferon-α; IL-6, interleukin-6; TNF, tumour necrosis factor.
PapMV induces pro-inflammatory cytokine secretion in APC
To determine whether the lipid raft aggregation induced by PapMV is associated with cell activation, we measured cytokine secretion after PapMV stimulation. BMDM were stimulated with 0·01, 0·1 (data not shown) or 1 μg/ml of PapMV, and the secretion of TNF-α and IL-6 was measured in the culture supernatants. As a control, 100 ng/ml of E. coli UHO111 LPS was used. Only stimulation with 1 μg/ml of PapMV induced IL-6 secretion in BMDM 12 hr after the initial stimulation. The maximum amount of IL-6 was detected at 50 hr, after which time IL-6 concentrations in the culture supernatants decreased (Fig. 4c). TNF-α secretion was detected in culture supernatants 4 hr after stimulation with 1 μg/ml of PapMV, and an increased amount of TNF-α was present in cell supernatants during the 24 hr of the experiment (Fig. 4c). Thus, in addition to lipid raft aggregation, PapMV induces the secretion of pro-inflammatory cytokines in BMDM. As DC are an important link between innate and adaptive immune responses, we evaluated the production of IL-6 and TNF-α by BMDC pulsed with PapMV. Both cytokines were observed in BMDC culture supernatants 18 and 24 hr after PapMV stimulation (Fig. 4d). Because type I IFN is suggested to contribute to the generation of a virus-specific adaptive immune response, we measured IFN-α production by macrophages and DC after PapMV stimulation. Peritoneal macrophages and BMDC were pulsed with PapMV, and, after 24 hr of stimulation, IFN-α was measured in the cell supernatants. Peritoneal macrophages did not produce IFN-α after PapMV stimulation (Fig. 4c), whereas PapMV-stimulated BMDC produced this cytokine more efficiently than did BMDC stimulated with LPS (Fig. 4d).
BMDM bearing PapMV participate in the induction of the specific antibody response
APC can directly deliver antigen to B cells for the induction of the antibody response.25,26 To address the contribution of APC in the induction of the antibody responses against PapMV, BMDM were cultured with 30 μg/ml of PapMV for 3 hr. After incubation, cells were injected i.v. into BALB/c mice at one of three doses (104, 105 or 106 cells). As the control for the free virus, the cell culture supernatant from the PapMV-stimulated cells and the last wash supernatant of these cells were independently injected i.v. in mice. As a positive control, mice were injected i.v. with 30 μg of PapMV, and 105 non-pulsed BMDM were transferred as a control (Fig. 4b). Neither 104 nor 105 PapMV-pulsed cells induced a specific IgG titre. By contrast, transfer of 106 PapMV-stimulated cells induced a specific antibody titre on day 12 after transfer. The titre increased 16-fold around day 20 and remained at this level until the last day tested (day 30; Fig. 4b). Neither the last cell wash supernatant nor the 105 unstimulated BMDM induced a PapMV-specific antibody titre, showing that transferred cells did not contain free virus and that the antibody response induced was specific. Moreover, both the culture supernatant from PapMV-stimulated BMDM, and PapMV injected i.v. induced specific antibody titres (Fig. 4b).
These results show that BMDM were able to provide PapMV to B cells efficiently, inducing a specific antibody immune response. This mechanism could also be involved in translating the innate immune response induced by PapMV into a specific long-lasting antibody response.
PapMV induces the up-regulation of activation markers on DC, macrophages and B cells in vivo
If PapMV is indeed recognized by the immune system as a PAMP, it should drive the maturation of immature DC or activate APC, as do other PRR agonists. To characterize the capacity of PapMV to stimulate APC in vivo, we isolated lymph nodes and spleens of mice immunized with PapMV and analysed the up-regulation of co-stimulatory and activation molecules (CD80, CD86, CD40, CD69 and MHC class II). Mice were immunized i.p. with 30 μg of PapMV, 50 μg of Poly I:C (both in saline) or saline alone (control). Twenty-four hours after immunization, lymph nodes and spleen cells were harvested. As shown in Fig. 3, PapMV induced the up-regulation of CD80 and CD69 in lymph node (LN) DC (CD11c+ CD11b−) and CD40 and CD69 in spleen DC. For macrophages (CD11c− CD11b+), up-regulation of CD80 and CD69 was observed in LN, whereas CD40 and CD69 up-regulation was observed in the spleen. CD69 was up-regulated in LN B lymphocytes (CD11c− B220+), and CD40 and CD69 were up-regulated in splenic B cells. The TLR-3 agonist, Poly I:C, induced the up-regulation of the markers tested, although the profile observed was markedly different from that induced by PapMV (Fig. 3).
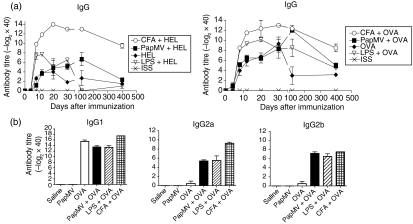
PapMV strengthens the antibody response to model antigens
Adjuvants are substances capable of augmenting the antibody response or the cellular immune response against poor immunogenic antigens.27 Adjuvant effects are mediated by the activation of DC and macrophages through PRR such as TLR.28 As mentioned above, PapMV induced the activation and maturation of APC, suggesting that it has intrinsic adjuvant properties. To determine whether PapMV is an adjuvant that can promote a long-lasting antibody response to other antigens, BALB/c mice were immunized i.p. on day 0 with 2 mg of OVA or HEL, either alone or together with the following adjuvants: PapMV, CFA or LPS. The IgG titre specific for OVA or HEL was measured by ELISA at the time-points indicated (Fig. 5a). The adjuvant effect of PapMV was observed on the total IgG response to OVA and HEL in immunized animals. An adjuvant effect induced by PapMV was observed for HEL on day 30 after immunization, when the antibody titre increased eightfold compared with the antibody titre induced by HEL alone. This difference in antibody titre was maintained until day 120, but not to day 400 (Fig. 5a). Although LPS induced an adjuvant effect only in the first 30 days after immunization, CFA showed the strongest adjuvant effect from day 8 to the end of the experiment on day 400 after immunization (Fig. 5a). For immunization with OVA, the adjuvant effect on total IgGtitres was observed only until day 120 after the first immunization, after which the antibody titre decreased with time, but was still fourfold higher than for OVA on day 400 (Fig. 5a). Further analysis was performed on day 20 to identify which IgG subclasses were induced by OVA and by OVA co-immunized with adjuvants (where PapMV did not show an adjuvant effect on the total IgG response). PapMV, LPS and CFA induced OVA-specific IgG2a and IgG2b titres, whereas OVA alone induced only IgG1-specific antibody titres (Fig. 5a). No adjuvant effect for IgG1 was observed when OVA was co-administered with any of the adjuvants used. Thus, PapMV, LPS and CFA induce an adjuvant effect on the IgG subclass responses to OVA. Moreover, PapMV exhibits adjuvant properties that induce a long-lasting increase in specific antibody titres to model antigens. Taken together, these data suggest that PapMV has intrinsic adjuvant properties that may have mediated the translation of the innate response into an antigen-specific long-lasting antibody response.27
Figure 5.
Papaya mosaic virus (PapMV) strengthens the antibody response to model antigens. (a) Groups of three female BALB/c mice were immunized with 2 mg of ovalbumin (OVA) or hen egg-white lysozyme (HEL), either alone or with the following adjuvants: 30 μg of PapMV, complete Freund's adjuvant (CFA) (1:1, v/v) or 5 μg of lipopolysaccharide (LPS) from Escherichia coli O111:B4. Control mice were injected with saline only (isotonic saline solution (ISS)). Serum was obtained from the immunized mice at the time-points depicted. A representative result from two experiments is shown. (b) The PapMV adjuvant effect is characterized by the induction of higher OVA-specific IgG2a and IgG2b titres. Analysis of IgG subclasses present on day 20 in serum from mice immunized with OVA, PapMV–OVA, LPS–OVA and CFA–OVA.
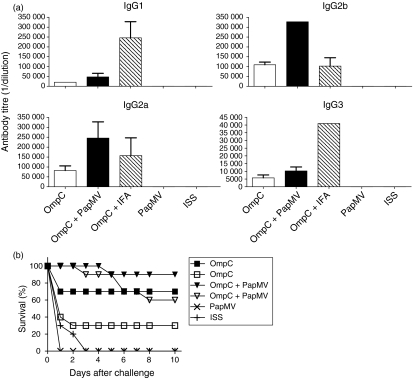
Co-administration of PapMV and S. typhi OmpC porin increases the OmpC protective capacity against S. typhi challenge
An adjuvant is also used to promote the antigen protective capacity.27 To test whether the adjuvant properties of PapMV could increase the protection of a vaccine, we co-administered PapMV with an experimental vaccine to typhoid fever, composed of S. typhi OmpC porin, developed in our laboratory.15,29 Compared to mice immunized with the OmpC porin, mice immunized with OmpC mixed with PapMV showed a survival rate 30% higher after challenge with 100 and 500 LD50 of S. typhi (Fig. 6b). No protection was observed in mice immunized only with PapMV on days 0 and 15 and challenged on day 21 (Fig. 6b) or in mice immunized with PapMV and challenged 24 hr later (data not shown). These data reject the idea that the protection observed is the result of enhanced inflammation induced by PapMV. To test if increased protection correlates with an increase in the antibody titre specific for OmpC, we measured the PapMV adjuvant effect on the OmpC-specific antibody titres. PapMV co-immunization with OmpC induced an increase in the anti-OmpC IgG1, IgG2a, IgG2b and IgG3 titres (Fig. 6a).These results further corroborate that the adjuvant properties of PapMV potentiate both innate and adaptive immune responses elicited by OmpC to achieve protection against S. typhi challenge.
Figure 6.
Papaya mosaic virus (PapMV) promotes the increase of antibody titres and potentiates the protection induced by an experimental vaccine. (a) Groups of five female BALB/c mice were immunized intraperitoneally (i.p.) on day 0 with 10 μg of outer membrane protein C (OmpC) alone or together with 30 μg of PapMV or Freund's incomplete adjuvant (IFA) (1:1, v/v). On day 15, all mice were boosted with 10 μg of OmpC only. Control mice were injected with saline only (isotonic saline solution (ISS)). Antibody titres were measured by enzyme-linked immunosorbent assay (ELISA) on day 21 after the first immunization. (b) PapMV increased the protective capacity of OmpC porin. Groups of 10 female BALB/c mice were immunized i.p. with 10 μg of OmpC either alone or with 30 μg of PapMV. The booster was given on day 15 using Omp C alone. Control mice were injected with saline (ISS) or PapMV. The challenge of experimental groups was performed on day 21 with a 100 (filled symbols) or a 500 (open symbols) 50% lethal dose (LD50) of Salmonella enterica serovar Typhi (S. typhi), and the survival rate was recorded for 10 days after the challenge. Control groups were challenged with 20 LD50 of S. typhi. A representative result of three experiments is shown.
Discussion
The characterization and study of molecules able to induce long-lasting immune responses, and the mechanisms involved in their recognition, are important for understanding the generation of long-term immunity.15,30 We found, in this study, that PapMV is a strong immunogenic antigen able to induce a long-lasting antibody response with a single dose and without added adjuvants (Fig. 1a). We also observed that PapMV induces a T-cell response (Fig. 1b). Because PapMV is not pathogenic in mammals,10 the mammalian immune system has had no evolutionary selective pressure to generate immunity against PapMV. Therefore, the highly immunogenic activity of this virus suggests that the molecular patterns recognized by PRR on cells from the innate immune system and by B and T cells – rather than pathogenicity of the virus – might be the driving force in the recognition of PapMV. The relationship between the distribution of epitopes within a molecule and the capacity to activate B lymphocytes independently of T cells has been described previously,31 suggesting that highly repetitive and organized antigens promote the establishment of a long-lasting B-cell response. Similarly to many vertebrate pathogenic viruses, PapMV repetitive-pattern epitopes may cross-link specific immunoglobulins efficiently on B-cell surfaces. The specificity of PapMV recognition by B cells is supported by the observation that PapMV is not a type 1 thymus-independent antigen (Fig. 2). However, the small up-regulation of B-cell activation markers observed both in vitro and in vivo suggest that PapMV could also be recognized by non-BCR receptors on B cells. The contribution of non-BCR receptors, such as TLRs, expressed on B cells, to the humoral immune response is a topic of debate.32,33 TLR stimulation has been proposed as a third signal required for the activation of human naïve B cells34 or as a signal to maintain B-cell memory compartments.35 Thus, PapMV could stimulate B cells to favour processes such as antigen presentation, co-stimulation or as survival signal for some B cells.
Recognition of repetitive, organized molecular patterns is also important to activate the innate immune response. This has been studied for mannose-binding lectin,36 for a polymeric bacterial protein that signals through TLR-437 and for highly ordered flagellin, a TLR-5 agonist, for which immunogenicity is dependent on its level of polymerization.38Accordingly, PapMV particles efficiently activated innate immune system cells, as shown in Figs 3 and 4. Although we did not identify the PRR involved in the innate immune activation, this response indicated that PapMV is recognized by the immune system similarly to PAMP. Because PAMP are important components of many adjuvants, we tested the adjuvant properties of PapMV. PapMV promoted long-lasting antibody responses to HEL and to OVA (Fig. 5a) and has been found to potentiate the protective capacity of an experimental vaccine19,29 (Fig. 6). Previously, we have reported a lack of adjuvanticity of the monomeric form of PapMV CP, indicating the critical function of multimerization in the induction of an antibody response to the expressed antigen.39 These data confirm that PapMV activates immune responses similarly to PAMP.
Antigen presentation by APCs to T cells has shown the importance of the innate immune system to activate the adaptive immune system. APCs loaded with PapMV efficiently induced antibody responses (Fig. 4b), as previously observed for a mammalian infecting virus.25 These data, and the effects elicited by PapMV on APCs (Figs 3 and 4), suggest that PapMV-stimulated APCs provide the antigen and the cytokine environment needed to promote an efficient T-cell-dependent antibody response, and this might be the mechanism involved in translating intrinsic adjuvant signals delivered by PapMV into the long-lasting antibody response observed. We propose that PapMV is sensed by the immune system both as PAMP and as antigen (Pamptigen), simultaneously activating innate and adaptive immune responses, which would favour the induction of a memory compartment. Pamptigens could also bind both BCRs and PRRs, such as TLRs, on specific B cells, leading to the differentiation of antibody-secreting cells or to the generation of memory B cells. A Pamptigen could reduce the antigen threshold required to activate the immune response. Therefore, small amounts of the persistent antigen could maintain a high antibody titre. Most non-infectious antigens, such as OVA or HEL, or PAMP (such as LPS), do not induce long-lasting antibody titres on their own. Our results suggest that the innate immune response makes an important contribution to the development or to the maintenance of long-lasting antibody responses.
The strong immunogenicity and intrinsic adjuvant properties of PapMV translate into a specific long-lasting antibody response to both PapMV and to model co-immunized antigens. As PapMV can be produced using inexpensive procedures and is stable at room temperature, it offers biotechnology useful advantages to develop new adjuvant or vaccine platforms39 to induce long-lasting immunity.
Acknowledgments
This study was funded by the Mexican National Science and Technology Council (CONACyT) Projects SEP-CONACyT 33137-M and 45261-M and by the Fund for Research Development (FOFOI) from IMSS Projects 2003-020, 2004-052 and 2006-022 awarded to C. López-Macías. R. Pastelin-Palacios acknowledge funding from Programa de Apoyo a Proyectos de Investigación e Innovación Tecnológica (PAPIIT), UNAM, Project: IN224907 and SEP-CONACyT 43911-M. The PhD students acknowledge scholarships received from CONACyT and IMSS. We acknowledge the excellent work on animal care performed by Mr Ricardo Vargas Orozco and Daniel Sánchez Almaraz, DVM. We thank Dr Edmundo Calva from the Biotechnology Institute, UNAM, for providing strain STYF302.
Abbreviations
- APC
antigen-presenting cell
- BCR
B-cell receptor
- BMDC
bone marrow-derived dendritic cells
- BMDM
bone marrow-derived macrophages
- CFA
complete Freund's adjuvant
- CFSE
5(6)-carboxyfluorescein diacetate N-succinimidyl ester
- CP
coat protein
- CTB
cholera toxin B subunit
- DC
dendritic cell
- DMEM
Dubecco's modified Eagle's minimal essential medium
- DTH
delayed-type hypersensitivity
- ELISA
enzyme-linked immunosorbent assay
- FBS
fetal bovine serum
- FCS
fetal calf serum
- FITC
fluorescein isothiocyanate
- HEL
hen egg- white lysozyme
- i.p.
intraperitoneal
- IFA
incomplete Freund's adjuvant
- IL
interleukin
- LD50
50% lethal dose
- LPS
lipopolysaccharide
- MHC class II
major histocompatibility complex class II
- OmpC
outer membrane protein C
- OVA
ovalbumin
- PAMP
pathogen-associated molecular pattern
- Pamptigen
pathogen-associated molecular pattern and antigen
- PapMV
papaya mosaic virus
- PBS
phosphate-buffered saline
- PE
phycoerythrin
- PerCP
peridinin chlorophyll protein
- PRR
pattern recognition receptor
- s.c.
subcutaneous
- SD
standard deviation
- TCR
T-cell receptor
- TLR
Toll-like receptor
- TNF-α
tumour necrosis factor-α
Conflict of interest
The authors have no financial conflict of interest.
N. Majeau, D. Leclerc and C. López-Macías are co-inventors on a patent pending for the use of PapMV as an adjuvant.
References
- 1.Janeway CAJ. Approaching the asymptote? Evolution and revolution in immunology. Cold Spring Harb Symp Quant Biol. 1989;54(Pt 1):1–13. doi: 10.1101/sqb.1989.054.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Sela M. Antigenicity: some molecular aspects. Science. 1969;166:1365–74. doi: 10.1126/science.166.3911.1365. [DOI] [PubMed] [Google Scholar]
- 3.Zinkernagel RM, Bachmann MF, Kundig TM, Oehen S, Pirchet H, Hengartner H. On immunological memory. Annu Rev Immunol. 1996;14:333–67. doi: 10.1146/annurev.immunol.14.1.333. [DOI] [PubMed] [Google Scholar]
- 4.Kaech SM, Wherry EJ, Ahmed R. Effector and memory T-cell differentiation: implications for vaccine development. Nat Rev Immunol. 2002;2:251–62. doi: 10.1038/nri778. [DOI] [PubMed] [Google Scholar]
- 5.Hofer T, Muehlinghaus G, Moser K, et al. Adaptation of humoral memory. Immunol Rev. 2006;211:295–302. doi: 10.1111/j.0105-2896.2006.00380.x. [DOI] [PubMed] [Google Scholar]
- 6.Zinkernagel RM. On natural and artificial vaccinations. Annu Rev Immunol. 2003;21:515–46. doi: 10.1146/annurev.immunol.21.120601.141045. [DOI] [PubMed] [Google Scholar]
- 7.Bachmann MF, Rohrer UH, Kundig TM, Burki K, Hengartner H, Zinkernagel RM. The influence of antigen organization on B cell responsiveness. Science. 1993;262:1448–51. doi: 10.1126/science.8248784. [DOI] [PubMed] [Google Scholar]
- 8.Dougan G, Hormaeche C. How bacteria and their products provide clues to vaccine and adjuvant development. Vaccine. 2006;24(Suppl. 2):S2–S9. doi: 10.1016/j.vaccine.2005.01.104. [DOI] [PubMed] [Google Scholar]
- 9.Kaisho T, Akira S. Toll-like receptors as adjuvant receptors. Biochim Biophys Acta. 2002;1589:1–13. doi: 10.1016/s0167-4889(01)00182-3. [DOI] [PubMed] [Google Scholar]
- 10.Pogue GP, Lindbo JA, Garger SJ, Fitzmaurice WP. Making an ally from an enemy: plant virology and the new agriculture. Annu Rev Phytopathol. 2002;40:45–74. doi: 10.1146/annurev.phyto.40.021102.150133. [DOI] [PubMed] [Google Scholar]
- 11.Erickson JW, Abouhaidar M, Bancroft JB. The specificity of papaya mosaic virus assembly. Virology. 1978;90:60–6. doi: 10.1016/0042-6822(78)90333-1. [DOI] [PubMed] [Google Scholar]
- 12.Erickson JW, Bancroft JB. The kinetics of papaya mosaic virus assembly. Virology. 1978;90:47–53. doi: 10.1016/0042-6822(78)90331-8. [DOI] [PubMed] [Google Scholar]
- 13.Sit TL, Abouhaidar MG, Holy S. Nucleotide sequence of papaya mosaic virus RNA. J Gen Virol. 1989;70(Pt 9):2325–31. doi: 10.1099/0022-1317-70-9-2325. [DOI] [PubMed] [Google Scholar]
- 14.Martinez-Flores I, Cano R, Bustamante VH, Calva E, Puente JL. The ompB operon partially determines differential expression of OmpC in Salmonella typhi and Escherichia coli. J Bacteriol. 1999;181:556–62. doi: 10.1128/jb.181.2.556-562.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Secundino I, Lopez-Macias C, Cervantes-Barragan L, et al. Salmonella porins induce a sustained, lifelong specific bactericidal antibody memory response. Immunology. 2006;117:59–70. doi: 10.1111/j.1365-2567.2005.02263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tremblay MH, Majeau N, Gagne ME, et al. Effect of mutations K97A and E128A on RNA binding and self assembly of papaya mosaic potexvirus coat protein. FEBS J. 2006;273:14–25. doi: 10.1111/j.1742-4658.2005.05033.x. [DOI] [PubMed] [Google Scholar]
- 17.Poltorak A, He X, Smirnova I, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–8. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 18.Alpuche-Aranda CM, Racoosin EL, Swanson JA, Miller SI. Salmonella stimulate macrophage macropinocytosis and persist within spacious phagosomes. J Exp Med. 1994;179:601–8. doi: 10.1084/jem.179.2.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Isibasi A, Ortiz-Navarrete V, Paniagua J, Pelayo R, Gonzalez CR, Garcia JA, Kumate J. Active protection of mice against Salmonella typhi by immunization with strain-specific porins. Vaccine. 1992;10:811–3. doi: 10.1016/0264-410x(92)90041-h. [DOI] [PubMed] [Google Scholar]
- 20.Mond JJ, Stein KE, Subbarao B, Paul WE. Analysis of B cell activation requirements with TNP-conjugated polyacrylamide beads. J Immunol. 1979;123:239–45. [PubMed] [Google Scholar]
- 21.Zhang H, Todderud E, Stubbs G. Crystallization and preliminary X-ray analysis of papaya mosaic virus coat protein. J Mol Biol. 1993;234:885–7. doi: 10.1006/jmbi.1993.1634. [DOI] [PubMed] [Google Scholar]
- 22.Dauphinee SM, Karsan A. Lipopolysaccharide signaling in endothelial cells. Lab Invest. 2006;86:9–22. doi: 10.1038/labinvest.3700366. [DOI] [PubMed] [Google Scholar]
- 23.Hsu HY, Hua KF, Lin CC, Lin CH, Hsu J, Wong CH. Extract of Reishi polysaccharides induces cytokine expression via TLR4-modulated protein kinase signaling pathways. J Immunol. 2004;173:5989–99. doi: 10.4049/jimmunol.173.10.5989. [DOI] [PubMed] [Google Scholar]
- 24.Simons K, Toomre D. Lipid rafts and signal transduction. Nat Rev Mol Cell Biol. 2000;1:31–9. doi: 10.1038/35036052. [DOI] [PubMed] [Google Scholar]
- 25.Ludewig B, Maloy KJ, Lopez-Macias C, Odermatt B, Hengartner H, Zinkernagel RM. Induction of optimal anti-viral neutralizing B cell responses by dendritic cells requires transport and release of virus particles in secondary lymphoid organs. Eur J Immunol. 2000;30:185–96. doi: 10.1002/1521-4141(200001)30:1<185::AID-IMMU185>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 26.Wykes M, Pombo A, Jenkins C, MacPherson GG. Dendritic cells interact directly with naive B lymphocytes to transfer antigen and initiate class switching in a primary T-dependent response. J Immunol. 1998;161:1313–9. [PubMed] [Google Scholar]
- 27.Pulendran B, Ahmed R. Translating innate immunity into immunological memory: implications for vaccine development. Cell. 2006;124:849–63. doi: 10.1016/j.cell.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 28.Krieg AM. CpG motifs: the active ingredient in bacterial extracts? Nat Med. 2003;9:831–5. doi: 10.1038/nm0703-831. [DOI] [PubMed] [Google Scholar]
- 29.Salazar-Gonzalez RM, Maldonado-Bernal C, Ramirez-Cruz NE, et al. Induction of cellular immune response and anti-Salmonella enterica serovar typhi bactericidal antibodies in healthy volunteers by immunization with a vaccine candidate against typhoid fever. Immunol Lett. 2004;93:115–22. doi: 10.1016/j.imlet.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Zinkernagel RM, Hengartner H. Protective ‘immunity’ by pre-existent neutralizing antibody titers and preactivated T cells but not by so-called ‘immunological memory’. Immunol Rev. 2006;211:310–9. doi: 10.1111/j.0105-2896.2006.00402.x. [DOI] [PubMed] [Google Scholar]
- 31.Fehr T, Bachmann MF, Bluethmann H, Kikutani H, Hengartner H, Zinkernagel RM. T-independent activation of B cells by vesicular stomatitis virus: no evidence for the need of a second signal. Cell Immunol. 1996;168:184–92. doi: 10.1006/cimm.1996.0065. [DOI] [PubMed] [Google Scholar]
- 32.Pasare C, Medzhitov R. Control of B-cell responses by Toll-like receptors. Nature. 2005;438:364–8. doi: 10.1038/nature04267. [DOI] [PubMed] [Google Scholar]
- 33.Gavin AL, Hoebe K, Duong B, Ota T, Martin C, Beutler B, Nemazee D. Adjuvant-enhanced antibody responses in the absence of toll-like receptor signaling. Science. 2006;314:1936–8. doi: 10.1126/science.1135299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruprecht CR, Lanzavecchia A. Toll-like receptor stimulation as a third signal required for activation of human naive B cells. Eur J Immunol. 2006;36:810–6. doi: 10.1002/eji.200535744. [DOI] [PubMed] [Google Scholar]
- 35.Bernasconi NL, Traggiai E, Lanzavecchia A. Maintenance of serological memory by polyclonal activation of human memory B cells. Science. 2002;298:2199–202. doi: 10.1126/science.1076071. [DOI] [PubMed] [Google Scholar]
- 36.Sheriff S, Chang CY, Ezekowitz RA. Human mannose-binding protein carbohydrate recognition domain trimerizes through a triple alpha-helical coiled-coil. Nat Struct Biol. 1994;1:789–94. doi: 10.1038/nsb1194-789. [DOI] [PubMed] [Google Scholar]
- 37.Berguer PM, Mundinano J, Piazzon I, Goldbaum FA. A polymeric bacterial protein activates dendritic cells via TLR4. J Immunol. 2006;176:2366–72. doi: 10.4049/jimmunol.176.4.2366. [DOI] [PubMed] [Google Scholar]
- 38.Hayashi F, Smith KD, Ozinsky A, et al. The innate immune response to bacterial flagellin is mediated by Toll-like receptor 5. Nature. 2001;410:1099–103. doi: 10.1038/35074106. [DOI] [PubMed] [Google Scholar]
- 39.Denis J, Majeau N, Acosta-Ramirez E, et al. Immunogenicity of papaya mosaic virus-like particles fused to a hepatitis C virus epitope: evidence for the critical function of multimerization. Virology. 2007;363:59–68. doi: 10.1016/j.virol.2007.01.011. [DOI] [PubMed] [Google Scholar]