SYNOPSIS
Objectives.
The goals of this project were to assess the feasibility of conducting rapid human immunodeficiency virus (HIV) testing in outreach and community settings to increase knowledge of HIV serostatus among groups disproportionately affected by HIV and to identify effective nonclinical venues for recruiting people in the targeted populations.
Methods.
Community-based organizations (CBOs) in seven U.S. cities conducted rapid HIV testing in outreach and community settings, including public parks, homeless shelters, and bars. People with reactive preliminary positive test results received confirmatory testing, and people confirmed to be HIV-positive were referred to health-care and prevention services.
Results.
A total of 23,900 people received rapid HIV testing. Of the 267 people (1.1%) with newly diagnosed HIV infection, 75% received their confirmatory test results and 64% were referred to care. Seventy-six percent were from racial/ethnic minority groups, and 58% identified themselves as men who have sex with men, 72% of whom reported having multiple sex partners in the past year. Venues with the highest proportion of new HIV diagnoses were bathhouses, social service organizations, and needle-exchange programs. The acceptance rate for testing was 60% among sites collecting this information.
Conclusions.
Findings from this demonstration project indicate that offering rapid HIV testing in outreach and community settings is a feasible approach for reaching members of minority groups and people at high risk for HIV infection. The project identified venues that would be important to target and offered lessons that could be used by other CBOs to design and implement similar programs in the future.
Of the approximately 1.1 million people living with human immunodeficiency virus (HIV) in the United States, it is estimated that 25% of them are unaware of their HIV status.1 In 2003, the Centers for Disease Control and Prevention (CDC) launched the Advancing HIV Prevention (AHP) initiative, which was aimed at increasing early diagnosis of HIV-positive people and referring those individuals to health-care and prevention services.2 The AHP initiative highlights the availability of simple, rapid HIV tests waived under the Clinical Laboratory Improvement Amendments, which allow testing to be conducted by non-laboratorians in a variety of nonclinical settings, with test results available to clients in as soon as 10 minutes. As part of this initiative, CDC funded community-based organizations (CBOs) in seven cities across the United States to conduct and evaluate new models for providing HIV testing using rapid HIV tests in outreach and community settings.3
Data from HIV testing performed at publicly funded counseling and testing sites using conventional HIV enzyme immunoassay (EIA) testing from 1999 through 2002 found that 19% to 22% of people with preliminary positive HIV tests did not return for their test results.4 A survey among high-risk individuals recruited in bars, outreach settings, and sexually transmitted disease (STD) clinics found that 10% to 27% of them reported failing to return for HIV test results at least once.5 People least likely to receive HIV test results also tended to be those at highest risk for infection. HIV and acquired immunodeficiency syndrome (AIDS) prevalence is high among African Americans, yet the proportion of African Americans who return to receive their HIV test results and posttest counseling is lower than that for white people who have been tested.4
Implementing rapid HIV testing programs in outreach and community settings, and targeting minority groups and people at high risk for HIV infection hold promise as a way to identify people who have unrecognized HIV infection. Previous rapid testing programs in outreach settings—using either the laboratory-based Single Use Diagnostic System (SUDS) rapid test (Abbott-Murex, Norcross, Georgia)6–8 or the point-of-care OraQuick® Rapid HIV-1 Antibody Test (OraSure Technologies, Bethlehem, Pennsylvania)9,10—have been successful in increasing the proportions of people who receive their preliminary HIV test results on the same day as their test.7,9,10 The rate of acceptance of rapid HIV testing in outreach settings has varied from 14% to more than 70%, depending on the project and venue.8,10,11 Negative rapid HIV test results are considered to be conclusive, but reactive rapid tests are considered to be preliminary positive results that need to be confirmed by a Western blot or other test. Although those who have reactive rapid tests need to provide specimens for confirmatory testing and return to receive their confirmatory test results, HIV counseling and testing staff have the opportunity to immediately provide posttest counseling to these individuals and link them to appropriate medical and support services.
From 2004 to 2006, eight CBOs in seven U.S. cities conducted a project to determine the acceptability and feasibility of offering HIV counseling and rapid testing in a variety of outreach and community settings frequented by people at high risk for HIV infection. These settings included public parks, places where commercial sex workers were known or thought to congregate, homeless shelters, CBO-affiliated community clinics, and bars. The primary objectives of this project included increasing knowledge of HIV serostatus among people who belong to groups disproportionately affected by HIV (e.g., racial/ethnic minority groups) or who are at risk for HIV infection, and identifying potential nonclinical venues for recruiting people belonging to groups targeted by the project.
METHODS
CBOs worked with community planning groups, health departments, and other local organizations in seven cities (Boston; Chicago; Detroit; Kansas City, Missouri; Los Angeles; San Francisco; and Washington, D.C.) to identify people who belong to groups disproportionately affected by HIV, people at high risk for HIV infection, and people who are less likely to access traditional HIV counseling, testing, and referral services. CBO staff selected a variety of community settings in which to conduct rapid HIV testing, choosing locations thought to be frequented by people at risk for HIV infection.
CBOs provided HIV counseling and rapid testing in mobile testing units (MTUs) in community and outreach locations such as on street corners, outside bars, near parks, and during special events (e.g., health fairs and gay pride festivals). At venues such as community clinics (e.g., free clinics or community health centers), social service organizations, homeless shelters, and drug treatment facilities, testing was conducted in either a building or an MTU, depending upon the site.
Seven of the eight participating CBOs used vans or recreational vehicles that were customized so that HIV counseling and testing services could be provided in them. The vans and recreational vehicles were equipped with separate rooms to allow staff members to conduct private counseling and testing sessions to several clients concurrently. The eighth CBO conducted outreach testing in a climate-controlled tent that was customized for providing HIV counseling and testing services and that could be set up at various public locations, such as parks. The tent contained a waiting area as well as partitions that could be dropped down to increase privacy. CBOs used various methods to promote rapid HIV testing in outreach and community venues, including posting signs on MTUs, posting or distributing materials in targeted areas, partnering with other agencies to obtain client referrals, working with community gatekeepers (people with access to specific groups targeted in the project), and running print, television, and radio advertisements.
People were eligible to receive a rapid HIV test if they self-reported that they were HIV-negative or did not know their HIV status, they met the age requirements for consent in the state in which testing was offered, and they were able to provide informed consent. CBO staff approached people at selected venues and offered them free HIV testing, explaining that results would be available in as few as 20 minutes. Additionally, some people who saw the MTUs approached CBO staff and asked to be tested, or came specifically to clinic settings for testing after learning about testing availability through advertising or word-of-mouth. Some CBOs provided small, nonmonetary incentives such as snacks, or donated hats or gloves to people receiving testing. One CBO provided up to a $20 grocery gift card to participants as an incentive to get tested.
Not all project sites systematically collected data on the number of people who declined testing. Two project sites, Detroit and Washington, collected data from people who refused to be tested during specific time periods during the project. The acceptance rate was calculated by dividing the number of people who accepted testing by the total number of people approached for testing during the periods in which refusal data were collected. In Detroit, refusal data were collected over 51 nonconsecutive days in a one-year time period, and 544 people (149 who accepted testing and 395 who declined testing) were approached and offered testing. In Washington, refusal data were collected over 55 nonconsecutive days during a two-year time period, and 3,764 people (2,436 who accepted testing and 1,328 who declined testing) were approached and offered testing.
People who agreed to be tested were escorted to a private room or space within an MTU or in the building in which testing was being conducted, and trained HIV counseling and testing staff obtained written consent, provided pretest counseling, and performed rapid HIV testing using the OraQuick® Rapid HIV-1 Antibody Test or the OraQuick Advance® Rapid HIV-1/2 Antibody Test on either oral fluid or finger-stick whole-blood specimens. In rare instances, conventional testing using an HIV EIA was performed when rapid HIV test kits were not available.
For people with reactive rapid HIV test results, serum or oral fluid specimens were collected for confirmatory testing by Western blot. CBO staff provided posttest counseling (which included counseling to reduce risk behaviors), scheduled follow-up appointments to provide confirmatory test results, and collected contact information to locate people who did not return for their confirmatory results. People who were homeless were asked to provide the names of shelters, places where they spent time, or other CBOs through which they might be contacted. In some instances, nonmonetary incentives (e.g., bus tokens) were offered to encourage people to return for their confirmatory test results. CBO staff referred people with confirmed HIV infection to HIV care, treatment, prevention, and support services. Because of concerns that they might not return for their confirmatory test results, some clients were referred to HIV care and prevention services when they received their preliminary test results.
CBO staff used standard data collection forms provided by CDC to collect information about demographic and behavioral risk characteristics and HIV testing history. Data were also collected on the confirmatory testing process and referrals to medical care and other services for those with confirmed HIV infection. The data for the two CBOs that were located in Los Angeles were combined for this analysis. Descriptive analyses were performed using SAS version 9.1.12
CDC determined this project to be a public health program evaluation of the implementation of rapid HIV testing and counseling in nonclinical settings; therefore, review by CDC's Institutional Review Board was not required.
RESULTS
The characteristics of people who were tested in this project have been summarized in detail elsewhere.3 A total of 24,172 people received HIV testing during the project period. Of these, 272 were excluded from this analysis because age information was missing, they reported previously being diagnosed with HIV infection, they were tested with a conventional rather than a rapid HIV test, or they had missing information for their test results. Of the 23,900 people included in this analysis, 6,855 (29%) were tested in community clinics, 6,304 (26%) were tested on street corners or in parks, 3,890 (16%) were tested at a social service organization (either a funded CBO or a collaborating CBO), and 6,851 (29%) were tested in a variety of venues including bars, drug treatment facilities, community special events, and homeless shelters. Outreach strategies were specific to each CBO site; therefore, not all CBOs conducted rapid HIV testing and counseling in the same types of venues.
Half of the people who were tested reported that they did not have health insurance. Lack of health insurance was highest among people tested at needle-exchange sites (72%), homeless shelters (67%), and social service organizations (61%). A total of 30% of participants had never been tested for HIV, and of those who had, 43% had not been tested in the past year.
HIV risk factors and new HIV diagnoses
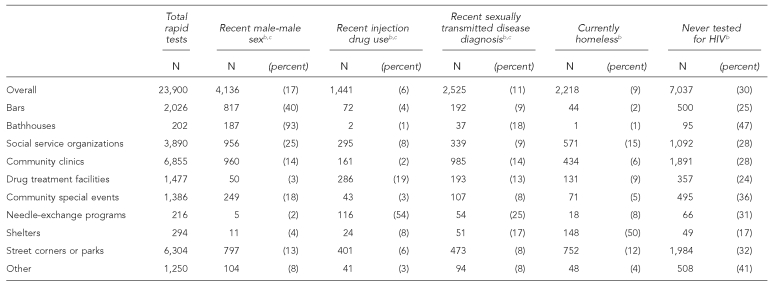
The proportions of people with selected risk characteristics varied by the venue in which testing was conducted (Table 1). The proportions of people who reported being diagnosed with an STD in the past year were highest in needle-exchange programs (25%), bathhouses (18%), and homeless shelters (17%). High proportions of people tested in bathhouses (93%), in bars (40%), and at social service organizations (25%) identified themselves as men who have sex with men (MSM). Fifty-four percent of people tested at needle-exchange program sites and 19% of people tested at drug treatment facilities reported injection drug use in the past year. The highest proportions of homeless people were tested in homeless shelters (50%), at social service organizations (15%), and on street corners or in parks (12%). Among people who had never been tested for HIV, the highest proportions that were tested in the project were tested in bathhouses (47%) and at community special events (36%).
Table 1. Characteristics of people who received rapid HIV tests by venue in which testing was conducted—seven U.S. cities, 2004–2006a.
aTesting was conducted in eight community-based organizations (CBOs) in seven cities. Information for the two CBOs in Los Angeles was combined for this analysis.
bCategories contain some missing data.
cIn the past 12 months
HIV = human immunodeficiency virus
A total of 331 people (1.4%) received preliminary positive HIV test results, and 267 people (1.1%) were newly diagnosed with HIV. Of the 64 who were not confirmed positive, 40 declined confirmatory testing, 17 were false positive, two had indeterminate results, and information was missing on five people. Of the 286 people who received confirmatory testing, 208 (73%) received their test results. Among those with confirmed HIV infection, 200 (75%) received their confirmatory test results, and 171 (64%) of these people accepted a referral to follow-up care. Information on whether people who were referred to follow-up care actually attended their first appointment was not systematically collected by most CBOs, so this information was not available for most people with confirmed positive test results. Receipt of confirmatory test results was highest in bathhouses (100%), needle-exchange programs (100%), social service organizations (88%), and community clinics (85%); receipt of test results was lowest in street corner or park outreach settings (49%) and at community special events (40%).
Among the 267 people with new HIV diagnoses, 76% were from racial/ethnic minority groups. A total of 155 (58%) identified themselves as MSM, and 111 (72%) of these men reported having multiple sex partners, 34 (22%) reported being diagnosed with an STD, and 15 (10%) reported using injection drugs in the past year. Of the 112 people with confirmed infection who did not identify as MSM, 63% were male, 34% were female, and 3% were transgender. Forty-eight people (43%) reported having multiple sex partners, 14 (13%) reported being diagnosed with an STD, and 14 (13%) reported using injection drugs in the preceding year. Of people with newly diagnosed HIV infection, 106 (40%) indicated that they had been tested for HIV within the past 12 months.
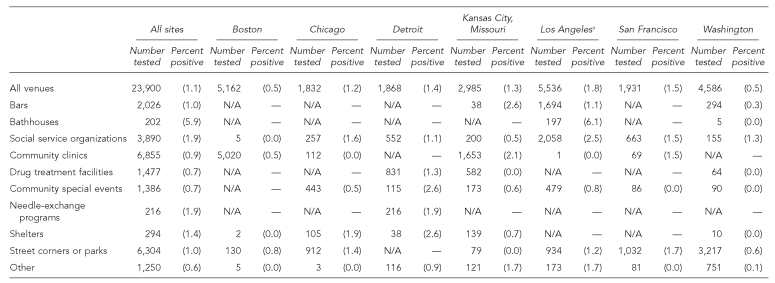
The proportion of people tested who had newly confirmed HIV infection ranged from 0.5% to 1.8% in the seven cities in which the project was conducted and was highest in Los Angeles and lowest in Boston and Washington (Table 2). The venues in which the highest proportions of test results were confirmed positive were bathhouses (5.9%), social service organizations (1.9%), and needle-exchange programs (1.9%). Proportions of test results that were confirmed positive varied by types of venues within cities. For instance, in Detroit, the proportion was highest among those tested at community special events and in homeless shelters, whereas in Los Angeles, it was highest among those tested at social service organizations and bathhouses.
Table 2. Number of people tested for HIV infection and proportion of people with newly confirmed HIV infection, by venue and city—seven U.S. cities, 2004–2006.
aTesting was conducted in eight community-based organizations (CBOs) in seven cities. Information for the two CBOs in Los Angeles was combined for this analysis.
HIV = human immunodeficiency virus
N/A = not applicable
Acceptance of testing venues
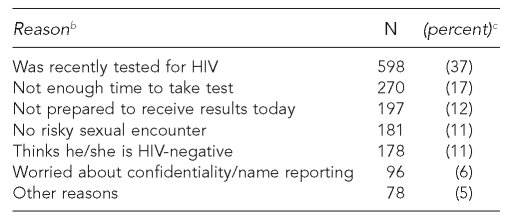
People who were tested at all participating CBOs were asked if they thought that the venues in which they were tested were appropriate settings for testing, and 98% indicated that they were. Data for people who refused HIV testing, however, were collected only by CBOs in Detroit and Washington. At these two sites, 4,308 people were approached and offered testing during time periods in which refusal data were collected, and 2,585 (60%) accepted testing. The most common reasons cited by the 1,598 people who offered a reason for refusing testing were having been tested for HIV recently (37%), not having enough time to take the test (17%), and not being prepared to receive test results on the day that testing was conducted (12%) (Table 3). Only a very small percentage of people who declined testing (<1%) indicated that it was because they did not want to be tested in the type of venue where testing was being offered.
Table 3. Reasons cited by 1,598 people who refused rapid HIV testing in outreach settings—Detroit and Washingtona.
aInformation was collected during limited time periods during the project at the community-based organizations in Detroit and Washington.
bA total of 125 (7%) of the people refusing testing did not provide a reason for refusal.
cPercentages might not add up to 100% because of rounding.
HIV = human immunodeficiency virus
DISCUSSION
The results from this project indicate that offering rapid HIV testing in outreach and community settings is a feasible approach for reaching minorities and people at high risk for HIV infection. Overall, CBOs were able to reach a large number of people who were members of racial/ethnic minority groups or who reported having had multiple sex partners in the past year.3 MSM accounted for more than half of the people with newly diagnosed HIV infection in this project.
Needle-exchange programs and drug treatment facilities were the venues in which the highest proportion of people reporting intravenous drug use were tested; however, a low proportion of all tests were conducted at these venues, and only 11% of people with newly diagnosed HIV infection reported intravenous drug use in the past year.
Fifty percent of people tested reported having health insurance, and among those without health insurance, 47% had visited a health-care provider in the past year. This indicates that opportunities existed for testing an appreciable number of these high-risk people in clinical settings.3 However, no information was collected in this project about the types of health-care providers seen or the nature of clinical interactions.
The project reached an appreciable number of people who had not been previously tested for HIV and a substantial number of people who had not been tested in the past year. The high proportion of people who reported behaviors placing them at risk for HIV infection in the past 12 months suggests an ongoing need for HIV testing in outreach and community settings. At the two sites that collected information about why people refused testing, the primary reason cited for refusing testing was having recently been tested for HIV. CBOs implementing rapid HIV testing programs in nonclinical settings should identify venues where they can best target people who have not previously been tested. Bathhouses and community special events (e.g., gay pride events and community health fairs) were the two venues identified by this project in which more than one-third of people who received HIV testing had never previously been tested for HIV.
The overall proportion of new HIV diagnoses among people tested was 1.1%. The proportions of people with newly confirmed HIV infection among those tested varied by the type of venue and the city in which HIV testing was conducted. This variation highlights the importance of developing outreach testing approaches that are specific to the communities being served. To ensure that CBO testing programs are reaching groups at high risk for HIV infection, CBO staff should evaluate program data periodically, including test logs, to monitor the effectiveness of testing in outreach and community settings. CBOs should consult with health department staff, other social service organizations, and people at high risk for HIV infection to identify new sites in which to conduct targeted HIV testing.
Although using rapid HIV testing allowed participating CBOs to provide negative test results and preliminary positive test results within 20 to 40 minutes after conducting a test, providing confirmatory test results to people with reactive rapid tests and linking those individuals with confirmed infection to follow-up care and prevention services were challenges for most CBOs.13 The proportion of people with preliminary positive test results who returned to receive the results of their confirmatory tests varied by type of venue. The proportion of people who returned for confirmatory results was lowest among people tested in outreach settings at community special events, on street corners, and in parks. However, the proportion returning for confirmatory results was higher in this project than it was in a similar rapid HIV testing program targeting high-risk people using an MTU.9,14 At venues such as social service organizations, community clinics, and bathhouses, the proportion returning for confirmatory results was very high and comparable to that found in previous studies,10,11,14 but fewer than half of those tested in street outreach or special events received their confirmatory test results. Thus, CBOs that plan to conduct HIV testing in such settings should explore the specific reasons why clients with preliminary positive test results do not return for their confirmatory test results, and develop appropriate strategies to overcome these barriers.
Data collected by two CBOs about acceptance of rapid testing showed that 60% of people who were offered the testing agreed to be tested. Overall, more than one-third of respondents who refused testing did so because they had been tested for HIV recently, and almost one-quarter declined testing because they thought that they had not had risky sexual encounters or they believed themselves to be HIV-negative. Findings from the National HIV Behavioral Surveillance System showed that half of MSM who were surveyed and who reported that they had not been tested for HIV in the preceding 12 months cited not believing they were at risk for infection as a reason for not getting tested.15
Limitations
The findings in this analysis are subject to several limitations. People offered HIV testing in this project were not systematically selected, so they may not be representative of people served by participating CBOs or other CBOs. In addition, participating CBOs did not consistently collect information about the number of people who refused testing or reasons for refusal. The data we collected provide some insight into the acceptance of testing and reasons for refusing testing, but only two CBOs collected this information. Because the information was not collected from a systematic sample of people these organizations tested, it may not be representative of all people who were offered testing in these CBOs, this project, or in other outreach and community settings. Lastly, in certain types of venues, such as homeless shelters, substance-abuse treatment centers, and community clinics, testing may have been conducted within the facilities or in an MTU outside the facilities and, therefore, some people who were tested at these locations may not have accessed services at these venues.
CONCLUSIONS
Almost 24,000 people were tested in various types of venues in outreach and community settings in this project, and 267 people with unrecognized HIV infection were identified. Most of those with confirmed infection were from racial/ethnic minority groups, anda many reported one or more behaviors in the past year that put them at risk for HIV infection. The project was effective in reaching minorities and people at high risk of infection, identifying types of venues that would be important to target, and offering lessons that could be used by other CBOs to design and implement HIV testing programs in outreach and community settings.
Acknowledgments
The authors thank Chris Hubbard and the Whitman Walker Clinic in Washington, D.C., for their assistance during the development of this article.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Glynn M, Rhodes P. Estimated HIV prevalence in the United States at the end of 2003 (abstract T1-B1101); Programs and abstracts of the 2005 National HIV Prevention Conference; 2005 Jun 12–15; Atlanta. [cited 2008 Aug 26]. Also available from: URL: http://www.aegis.com/conferences/nhivpc/2005/t1-b1101.html. [Google Scholar]
- 2.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–32. [PubMed] [Google Scholar]
- 3.Rapid HIV testing in outreach and other community settings—United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56(47):1233–7. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (US) HIV counseling and testing at CDC-supported sites—United States, 1999–2004. [cited 2007 Nov 7];2006 1-7, 15. Available from: URL: http://www.cdc.gov/hiv/topics/testing/reports.htm.
- 5.Sullivan PS, Lansky A, Drake A HITS-2000 Investigators. Failure to return for HIV test results among persons at high risk for HIV infection: results from a multistate interview project. J Acquir Immune Defic Syndr. 2004;35:511–8. doi: 10.1097/00126334-200404150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Keenan PA, Keenan JM. Rapid HIV testing in urban outreach: a strategy for improving posttest counseling rates. AIDS Educ Prev. 2001;13:541–50. doi: 10.1521/aeap.13.6.541.21439. [DOI] [PubMed] [Google Scholar]
- 7.Kassler WJ, Dillon BA, Haley C, Jones WK, Goldman A. On-site, rapid HIV testing with same-day results and counseling. AIDS. 1997;11:1045–51. doi: 10.1097/00002030-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Kendrick S, Kroc K, Withum D, Rydman RJ, Branson B, McAuley J, et al. Impact of rapid HIV testing in three public venues (abstract #529); 40th Annual Meeting of Infectious Disease Society of America; 2002 Oct 24–27; Chicago. [cited 2007 Dec 12]. Available from: URL: http://www.cdc.gov/hiv/topics/testing/resources/abstracts/rt-impact.htm. [Google Scholar]
- 9.Liang TS, Erbelding E, Jacob CA, Wicker H, Christmyer C, Brunson S, et al. Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient Care STDS. 2005;19:253–7. doi: 10.1089/apc.2005.19.253. [DOI] [PubMed] [Google Scholar]
- 10.Buchér JB, Thomas KM, Guzman D, Riley E, Dela Cruz N, Bangsberg DR. Community-based rapid HIV testing in homeless and marginally housed adults in San Francisco. HIV Med. 2007;8:28–31. doi: 10.1111/j.1468-1293.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 11.Spielberg F, Branson BM, Goldbaum GM, Lockhart D, Kurth A, Celum CL, et al. Overcoming barriers to HIV testing: preferences for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr. 2003;32:318–27. doi: 10.1097/00126334-200303010-00012. [DOI] [PubMed] [Google Scholar]
- 12.SAS Institute Inc. SAS: Version 9.1. Cary (NC): SAS Institute Inc.; 2003. [Google Scholar]
- 13.Clark HA, Bowles KE, Song B, Heffelfinger JD. Implementation of rapid HIV testing programs in community and outreach settings: perspectives from staff at eight community-based organizations in seven U.S. cities. Public Health Rep. 2008;123(Suppl 3):86–93. doi: 10.1177/00333549081230S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutchinson AB, Branson BM, Kim A, Farnham PG. A meta-analysis of the effectiveness of alternative HIV counseling and testing methods to increase knowledge of HIV status. AIDS. 2006;20:1597–604. doi: 10.1097/01.aids.0000238405.93249.16. [DOI] [PubMed] [Google Scholar]
- 15.Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003–April 2005. MMWR Surveill Summ. 2006;55(6):1–16. [published erratum appears in MMWR Morb Mortal Wkly Rep 2006; 55(27):752] [PubMed] [Google Scholar]