SYNOPSIS
Objectives.
The goals of this research were to evaluate perceptions of staff about the effectiveness of methods used by eight community-based organizations (CBOs) to implement human immunodeficiency virus (HIV) counseling and rapid testing in community and outreach settings in seven U.S. cities, and to identify operational challenges.
Methods.
A survey was administered to CBO staff to determine their perceptions about the effectiveness of methods used to select testing venues, promote their testing programs, recruit people for testing, provide test results, and link HIV-positive people to health care. Using a Likert scale, respondents rated the effectiveness of methods, their agreement with statements about using mobile testing units (MTUs) and rapid HIV test kits, and operational challenges.
Results.
Most respondents perceived the methods they used for selecting testing venues, and particularly using recommendations from people receiving testing, to be effective. Most respondents also thought their promotional activities were effective. Respondents believed that using MTUs improved their capacity to reach high-risk individuals, but that MTUs were associated with substantial challenges (e.g., costs to purchase and maintain them). Programmatic challenges included training staff to provide counseling and testing, locating and providing confirmatory test results to people with reactive rapid tests, and sustaining testing programs.
Conclusions.
CBO staff thought the methods used to select venues for HIV testing were effective and that using MTUs increased their ability to provide testing to high-risk individuals. However, using MTUs was expensive and posed logistical difficulties. CBOs planning to implement similar programs should take these findings into consideration and pay particular attention to training needs and program sustainability.
In the United States, approximately one-fourth of the estimated 1.1 million people living with human immunodeficiency virus (HIV) are unaware of their HIV status.1 One way to increase the number of people who are aware of their HIV status is to expand HIV counseling and testing efforts to reach more people and to specifically target people who are at high risk for infection but who may not access HIV testing and health-care services. Studies have shown that offering HIV counseling and testing in community or outreach settings can be an effective strategy for identifying people with unrecognized HIV infection.2–7 In the 50 states and territories that reported HIV testing data to the Centers for Disease Control and Prevention (CDC) in 2004, nearly 2% of people who were tested in outreach/field settings had positive test results.3 Some studies of HIV testing among high-risk people in nonclinical or outreach settings have found even higher rates of HIV seroprevalence, ranging from 4% to 25%.4–7
Community-based organizations (CBOs) serve populations who are at high risk for HIV infection8 and are well positioned to offer HIV counseling and testing services tailored to members of these high-risk groups. People at high risk for HIV infection often face barriers to accessing testing in traditional clinical settings, including a lack of transportation, reluctance to visit HIV or sexually transmitted disease (STD) clinics, or lack of access to clinics outside of regular business hours.9,10 CBOs can eliminate some of the barriers to testing by using mobile testing units (MTUs), such as vans or tents, to offer HIV testing in outreach settings, including during evenings or on weekends.
Compared with people tested for HIV using conventional tests, people who are tested using rapid tests are more likely to receive their HIV test results.11 Thus, incorporating rapid HIV testing into mobile HIV testing programs may make these programs more feasible and help ensure that people receive their test results. Rapid point-of-care HIV tests can be performed on oral fluid or finger-stick blood specimens, they do not require venipuncture, and they provide negative or reactive (preliminary positive) results in as few as 10 minutes.12 Only people who have preliminary positive rapid test results require additional testing (i.e., confirmatory Western blot testing) and follow-up appointments to receive their confirmatory test results.
As a response to the U.S. HIV epidemic, CDC launched the Advancing HIV Prevention (AHP) initiative in 2003 and funded nine projects to demonstrate key AHP strategies.13 To evaluate the AHP initiative's second priority strategy, which was to implement new models for diagnosing HIV infections outside medical settings, CDC funded eight CBOs in seven U.S cities to perform HIV counseling and rapid HIV testing in community and outreach settings. The purpose of this project was to offer rapid HIV testing to people belonging to racial/ethnic minority groups, people at high risk for HIV infection, or people who were less likely to access HIV counseling and testing services in traditional medical settings.
At the conclusion of the project, CDC administered a survey to participating CBO staff to evaluate their perceptions of the effectiveness of the methods they used to implement HIV counseling and rapid testing in community and outreach settings, to identify challenges associated with implementing testing in these settings, and to identify effective practices for recruiting and testing people at high risk for HIV infection that other CBOs might use.
METHODS
Demonstration project
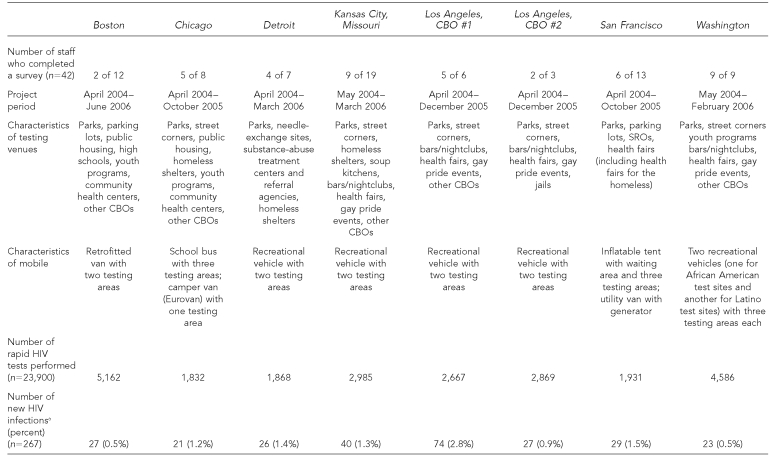
CDC funded CBOs in Boston; Chicago; Detroit; Kansas City, Missouri; Los Angeles; San Francisco; and Washington, D.C., to provide HIV counseling and rapid testing to members of populations disproportionately affected by HIV (e.g., African Americans, Latinos, men who have sex with men [MSM], transgender people, commercial sex workers, and homeless people) in community and outreach settings. Methods used in this project have been described in detail elsewhere.2,14 Characteristics of the CBOs and their counseling and testing programs are presented in Table 1.
Table 1. Characteristics of rapid HIV testing programs implemented by eight CBOs in outreach and community settings in seven U.S. cities, 2004–2006.
aTotals exclude people with unconfirmed reactive rapid test results or a previous HIV diagnosis.
HIV = human immunodeficiency virus
CBO = community-based organization
SRO = single-room occupancy hotel
Data collection
At the conclusion of the project period, a self-administered survey was distributed to staff at participating CBOs. All participating staff were eligible, and program directors and managers, HIV testing counselors, and outreach workers were particularly encouraged to respond to the survey, which took approximately 10 to 15 minutes to complete. Respondents provided written consent, were given the option of completing a paper or electronic survey, and returned either a hard copy or an electronic file to CDC. The survey and accompanying protocol were reviewed, and the survey was determined to be nonresearch because it was considered to be a programmatic evaluation of an AHP demonstration project and was, therefore, exempt from review by CDC's Institutional Review Board.
The survey included questions on the methods that CBOs used to select testing venues, advertise and promote their rapid HIV testing program, and provide confirmatory test results to people with reactive rapid HIV test results, as well as questions on using MTUs to perform rapid HIV testing in outreach settings. The content of the survey was selected based on input that CBO staff provided during site visits, conference calls, and meetings of project investigators. Most questions used a five-point Likert scale for respondents to rate their perceptions of the effectiveness of program methods and how challenging they found various programmatic elements. Program directors and managers were also asked to comment on their perceptions about the sustainability of their rapid HIV testing programs. All respondents were given the opportunity to provide general comments at the end of the survey.
Data analysis
We calculated the frequencies of responses rated on a Likert scale using SAS version 9.1.15 For the purpose of this analysis, Likert scales were collapsed from five to three categories. For questions about perceptions of effectiveness of methods, the “not effective” and “somewhat effective” categories were collapsed into a category termed “ineffective,” the neutral category remained the same, and the “effective” and “very effective” categories were collapsed into a category labeled “effective.” In like manner, items asking respondents to rate their agreement with statements were collapsed into three categories (“disagree,” “neutral,” and “agree”), and items about the challenges of programmatic elements were also collapsed into three categories (“not challenging,” “neutral,” and “challenging”).
RESULTS
Of the 68 people who were employed at the eight CBOs and had worked on the project, 42 completed a survey (survey response rate = 62%). Respondents included 24 HIV testing counselors, 10 program directors/coordinators, four outreach workers, and four other staff who filled supporting roles. The median length of time that respondents were employed with their respective CBO was 16 months. At the end of the project, 33 (78%) of the respondents were still employed by the participating CBOs.
Selecting rapid HIV testing venues in community and outreach settings
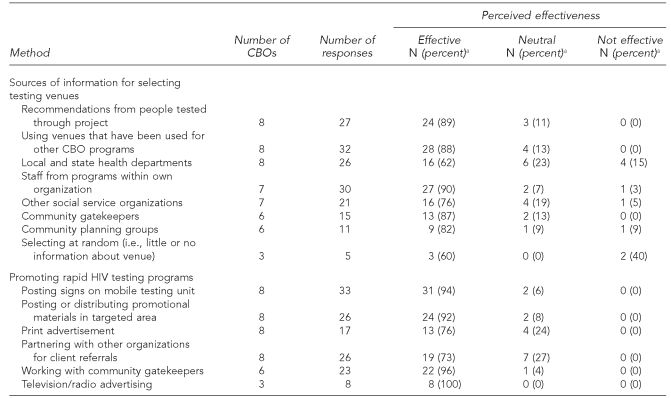
Respondents were asked to rate the effectiveness of eight methods used by their CBOs to select rapid HIV testing venues in community and outreach settings, and the majority believed each of the methods was effective (Table 2). Of the three methods used by all eight participating CBOs, 89% of respondents believed selecting testing venues based on recommendations from people who were tested in the project was effective, 88% considered selecting venues with which the CBO was already familiar to be effective, and 62% thought that consulting with local and state health departments to select venues in areas with a higher prevalence of HIV and/or sexually transmitted infections was effective.
Table 2. Methods used to select venues for HIV testing and to promote testing programs implemented by eight CBOs in community and outreach settings in seven U.S. cities, 2004–2006.
aRow percentages might not add up to 100% because of rounding.
HIV = human immunodeficiency virus
CBO = community-based organization
Advertising and promoting rapid HIV testing programs
Respondents were asked to rate the effectiveness of six methods that their CBOs used for advertising and promoting their HIV testing programs, and a majority indicated that all six methods were effective (Table 2). Of the methods used by all CBOs, those thought to be effective by the highest proportion of staff were posting signs on MTUs (94%), posting or distributing promotional materials in targeted areas (92%), and using printed advertisements (76%). Six CBOs worked with community gatekeepers to promote their testing programs, and 96% of respondents from these CBOs considered this to be an effective method for promoting their programs.
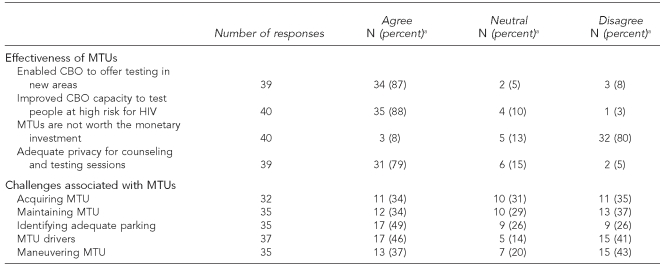
Using MTUs to perform rapid HIV testing in outreach settings
Overall, respondents agreed that using MTUs improved the capacity of their CBO to reach people at high risk of infection, enabled their CBO to offer testing in areas that were previously inaccessible, and provided adequate privacy for performing counseling and rapid HIV testing (Table 3). The majority of respondents disagreed with the statement, “MTUs were not worth the monetary investment (i.e., purchase price, registration fees, insurance, fuel, and maintenance).”
Table 3. Perceptions about the effectiveness and challenges of using MTUs at rapid HIV testing programs implemented by eight CBOs in community and outreach settings in seven U.S. cities, 2004–2006.
aRow percentages might not add up to 100% because of rounding.
MTU = mobile testing unit
HIV = human immunodeficiency virus
CBO = community-based organization
One respondent commented on the importance of using MTUs coupled with recruitment efforts for encouraging people to test, stating, “Many would not have tested if the MTU did not go to their neighborhoods or [if they did not have] a peer recruiter referral.”
Respondents identified a number of logistical challenges associated with using MTUs. Forty-nine percent indicated that finding adequate parking for MTUs was challenging, and 46% believed that finding qualified drivers for MTUs was challenging. Approximately one-third of respondents considered purchasing, maintaining, and maneuvering MTUs to be challenges.
Using rapid HIV tests
Respondents were asked to indicate their level of agreement with two statements about using rapid HIV test kits. All respondents had previous experience offering conventional HIV testing in nonclinical settings using HIV enzyme immunoassays or enzyme-linked immunosorbent assays, which typically allow results to be provided one to two weeks after testing. Overall, 92% of respondents agreed that they preferred using rapid HIV test kits to using conventional HIV testing and that using rapid HIV test kits made it easier to conduct testing in community and outreach settings.
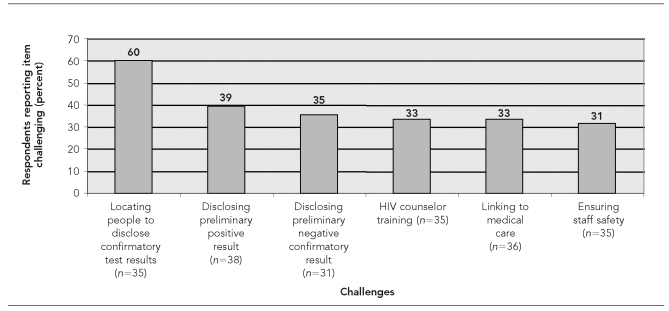
Overall challenges
CBO staff members were asked to identify the greatest challenges to performing HIV counseling and rapid testing in nonclinical settings. Overall, 60% of respondents found that locating people who had reactive rapid tests to disclose their confirmatory test results was challenging (Figure). One respondent commented:
We have experienced significant challenges in getting high-risk homeless and substance-abusing [people who tested positive] to follow up and engage in medical care and treatment. Oftentimes when these individuals leave the testing van, they become lost to us.
Figure. Challenges to implementing rapid HIV testing in community and outreach settings that were most frequently cited by staff who participated in rapid HIV testing programs implemented by eight CBOs in seven U.S. cities, 2004–2006.
HIV = human immunodeficiency virus
CBO = community-based organization
Another CBO staff member pointed out the difficulty of locating people to provide confirmatory test results, even when contact information had been provided to CBO staff:
Linking persons who test positive for HIV infection into appropriate medical treatment and care is challenging because the testing occurs in the field and is not centrally located to a treatment site. Once the person leaves the MTU, it is difficult to contact individuals because the contact information is many times false.
Challenges that were identified by a substantial proportion of respondents included delivering preliminary positive test results in outreach settings (39%), delivering negative confirmatory test results to people who had reactive tests (35%), and linking people with confirmed infection to medical care (33%) (Figure).
Sustainability
Of the 10 program directors and coordinators who responded to the survey, six indicated that obtaining training for their staff to conduct rapid HIV testing was one of the biggest challenges for their program, and five program directors and coordinators stated that maintaining an adequate supply of test kits, maintaining MTUs, and staff burnout were challenges for their programs. In addition, four program directors and coordinators indicated that their CBOs would not be able to continue to offer HIV testing programs in community and outreach settings unless new funding sources were identified after this project ended.
Despite the considerable challenges that were identified in this project, many of the comments of respondents about providing rapid HIV testing in outreach and community settings were overwhelmingly positive. One respondent said:
Mobile HIV testing is a great way to get to the population[s] that need it the most. I would love to work on this type of project again, and I hope that this project shows the necessity of this type of testing process for future HIV prevention programs.
DISCUSSION
Results from this survey suggest that respondents perceived that locating people with reactive rapid HIV tests to disclose their confirmatory test results was one of the greatest challenges to providing rapid HIV testing in community and outreach settings. This perception is supported by data collected during the project2 and from other studies.16,17
Thirteen percent of people with newly diagnosed HIV infection did not receive their confirmatory test results, and information about receipt of confirmatory results was missing for an additional 12% of people with new HIV diagnoses.2 CBOs that work with a large number of transient people, such as the homeless, may face even greater difficulties locating and providing confirmatory test results to people with reactive tests, and they may need to design novel methods to ensure that these people receive their confirmatory test results and that those with confirmed HIV infection are linked to appropriate health-care and prevention services.
Lessons learned
CBOs learned several lessons about using MTUs to provide rapid HIV testing in outreach settings. The costs of acquiring and maintaining MTUs are considerable and may increase program costs for conducting HIV testing in outreach settings.18 Using rapid HIV test kits obviates the need for people with negative test results to return for appointments to receive test results, and respondents indicated that they prefer rapid HIV testing to conventional HIV testing approaches. However, CBOs that perform HIV counseling and rapid testing in outreach settings using MTUs need to develop effective ways to provide confirmatory results to people with reactive rapid tests. Despite the challenges associated with operating MTUs, respondents believed that using MTUs was an effective way to reach and provide HIV testing to people at risk for HIV infection. Other research suggests that the clients may also prefer rapid HIV testing to conventional HIV testing.10,19–22
Our findings highlight several issues that are important for CBOs to consider prior to implementing rapid HIV testing programs in community or outreach settings. CBOs need to plan for and ensure that staff members who will perform HIV counseling and rapid HIV testing receive appropriate training. In addition, CBOs that are considering implementing HIV testing programs should develop plans for sustaining these programs before they implement them, particularly if the availability of federal funding to support these programs is uncertain, limited, or absent. Opportunities for partnerships, particularly with health departments, will likely increase in the future. In 2006, the National Alliance of State and Territorial AIDS Directors surveyed staff of state and local health departments and found that 91% of respondents planned to support rapid HIV testing in the next year and considered outreach venues and CBO sites as priority testing venues.21
Limitations
The results of this analysis were subject to several limitations. Data were gathered using a cross-sectional survey and represented the opinions of a small number of staff from CBOs that participated in this project. CBO staff were not systematically selected to participate in the survey, so they may not be representative of staff from their own CBOs or other CBOs that might conduct HIV testing. Also, there was variation in the length of time that respondents had worked at the participating CBOs (median of 16 months with a range of three to 36 months), and the number of staff who participated in the survey varied by CBO. Fewer than five staff members from three of the CBOs—including the CBO that performed the most rapid HIV tests (5,162 tests, which was 22% of the total tests)—completed the survey. In addition, although the overall survey response rate among CBO staff was relatively high (62%), item response rates varied widely and ranged from 12% to 79%. Scores of perceived effectiveness for items with very low response rates are subject to greater bias and should be interpreted with caution.
CONCLUSIONS
We surveyed 42 people from eight CBOs that implemented rapid HIV testing programs and found that most respondents thought the methods they used for selecting venues and using MTUs for outreach testing were effective. They also identified a number of important challenges to providing counseling and rapid HIV testing in community and outreach settings. Using MTUs can increase the ability of CBOs to provide testing to people at high risk for HIV infection, but they are expensive to purchase, operate, and maintain, and their use poses some logistical difficulties. CBOs planning to implement similar programs should take these findings into consideration, pay particular attention to the training needs of HIV counseling and testing staff, and consider ways to enhance and ensure sustainability during all phases from development to implementation of their HIV testing programs. Our findings provide lessons that can inform the design and operations of HIV testing programs that other CBOs implement in the future.
Acknowledgments
The authors thank Scott Kellerman, MD, MPH, for his assistance with developing the protocol for the demonstration project, along with the following people for their assistance with collecting data: Daisy Aguirre, Bienestar Human Services, Los Angeles; Azul Mares-DelGrasso, AIDS Healthcare Foundation, Los Angeles; Cicily Emerson, MSW, Tenderloin Health, San Francisco; Jenny Tsang, MPH, The Night Ministry, Chicago; Jonathan Pincus, MD, Dotwell, Dorchester, Massachusetts; Cindy Bolden Calhoun, Community Health Awareness Group, Detroit; Holly Buckendahl, MSW, Kansas City Free Clinic, Kansas City, Missouri; and Debra Dekker, PhD, Whitman Walker Clinic, Washington, D.C.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Glynn M, Rhodes P. Estimated HIV prevalence in the United States at the end of 2003 (abstract T1-B1101); Programs and abstracts of the 2005 National HIV Prevention Conference; 2005 Jun 12–15; Atlanta. [cited 2007 Oct 24]. Also available from: URL: http://www.aegis.com/conferences/nhivpc/2005/t1-b1101.html. [Google Scholar]
- 2.Rapid HIV testing in outreach and other community settings—United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56(47):1233–7. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (US) [cited 2007 Oct 24];HIV counseling and testing at CDC-supported sites—United States, 1999–2004. 2006 :1–7. 15. Available from: URL: http://www.cdc.gov/hiv/topics/testing/reports.htm. [Google Scholar]
- 4.Liang TS, Erbelding E, Jacob CA, Wicker H, Christmyer C, Brunson S, et al. Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient Care STDS. 2005;19:253–7. doi: 10.1089/apc.2005.19.253. [DOI] [PubMed] [Google Scholar]
- 5.Buchér JB, Thomas KM, Guzman D, Riley E, Dela Cruz N, Bangsberg DR. Community-based rapid HIV testing in homeless and marginally housed adults in San Francisco. HIV Med. 2007;8:28–31. doi: 10.1111/j.1468-1293.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 6.Rapid HIV testing among racial/ethnic minority men at gay pride events—nine U.S. cities, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56(24):602–4. [PubMed] [Google Scholar]
- 7.HIV prevalence, unrecognized infection, and HIV testing among men who have sex with men—five U.S. cities, June 2004–April 2005. MMWR Morb Mortal Wkly Rep. 2005;54(24):597–601. [PubMed] [Google Scholar]
- 8.Kelly JA, Heckman TG, Stevenson LY, Williams PN, Ertl T, Hays RB, et al. Transfer of research-based HIV prevention interventions to community service providers: fidelity and adaptation. AIDS Educ Prev. 2000;12(5) Suppl:87–98. [PubMed] [Google Scholar]
- 9.Spielberg F, Branson BM, Goldbaum GM, Lockhart D, Kurth A, Celum CL, et al. Overcoming barriers to HIV testing: preferences for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr. 2003;32:318–27. doi: 10.1097/00126334-200303010-00012. [DOI] [PubMed] [Google Scholar]
- 10.Molitor F, Walsh RM, Leigh JP. Determinants of longer time from HIV result to enrollment in publicly funded care and treatment in California by race/ethnicity and behavioral risk. AIDS Patient Care STDS. 2002;16:555–65. doi: 10.1089/108729102761041119. [DOI] [PubMed] [Google Scholar]
- 11.Hutchinson AB, Branson BM, Kim A, Farnham PG. A meta-analysis of the effectiveness of alternative HIV counseling and testing methods to increase knowledge of HIV status. AIDS. 2006;20:1597–604. doi: 10.1097/01.aids.0000238405.93249.16. [DOI] [PubMed] [Google Scholar]
- 12.Branson BM. State of the art for diagnosis of HIV infection. Clin Infect Dis. 2007;45(Suppl 4):S221–5. doi: 10.1086/522541. [DOI] [PubMed] [Google Scholar]
- 13.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–32. [PubMed] [Google Scholar]
- 14.Bowles KE, Clark HA, Tai E, Sullivan PS, Song B, Tsang J, et al. Implementing rapid HIV testing in outreach and community settings: results from an Advancing HIV Prevention demonstration project conducted in seven U.S. cities. Public Health Rep. 2008;123(Suppl 3):78–85. doi: 10.1177/00333549081230S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SAS Institute Inc. SAS: Version 9.1. Cary (NC): SAS Institute Inc.; 2003. [Google Scholar]
- 16.Salaru G, Martin EG, Paul SM, Berenzy L, Wolski M, Vega I, et al. HIV discordant follow-up: an evolving process (abstract #196T); 2007 National HIV Prevention Conference; 2007 Dec 2–5; Atlanta. [Google Scholar]
- 17.Martin E, Salaru G, Paul SM, Berenzy L, Wolski M, Vega I, et al. At the laboratory interface: HIV discordant follow-up (poster #14); 2007 HIV Diagnostics Conference; 2007 Dec 5–7; Atlanta. [Google Scholar]
- 18.Shrestha RK, Clark HA, Sansom SL, Song B, Buckendahl H, Calhoun CB, et al. Cost-effectiveness of finding new HIV diagnoses using rapid HIV testing in community-based organizations. Public Health Rep. 2008;123(Suppl 3):94–100. doi: 10.1177/00333549081230S312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.San Antonio-Gaddy M, Richardson-Moore A, Burstein GR, Newman DR, Branson BM, Birkhead GS. Rapid HIV antibody testing in the New York State Anonymous HIV Counseling and Testing Program: experience from the field. J Acquir Immune Defic Syndr. 2006;43:446–50. doi: 10.1097/01.qai.0000243055.65698.51. [DOI] [PubMed] [Google Scholar]
- 20.Kassler WJ, Dillon BA, Haley C, Jones WK, Goldman A. On-site, rapid HIV testing with same-day results and counseling. AIDS. 1997;11:1045–51. doi: 10.1097/00002030-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Smith LV, Rudy ET, Javanbakht M, Uniyal A, Sy LS, Horton T, et al. Client satisfaction with rapid HIV testing: comparison between an urban sexually transmitted disease clinic and a community-based testing center. AIDS Patient Care STDS. 2006;20:693–700. doi: 10.1089/apc.2006.20.693. [DOI] [PubMed] [Google Scholar]
- 22.National Alliance of State and Territorial AIDS Directors. [cited 2007 Oct 24];Rapid HIV testing assessment, October 2006. Available from: URL: http://www.nastad.org/Docs/highlight/20061030_NASTAD_RT_Implementation_2006_FINAL.pdf.