Abstract
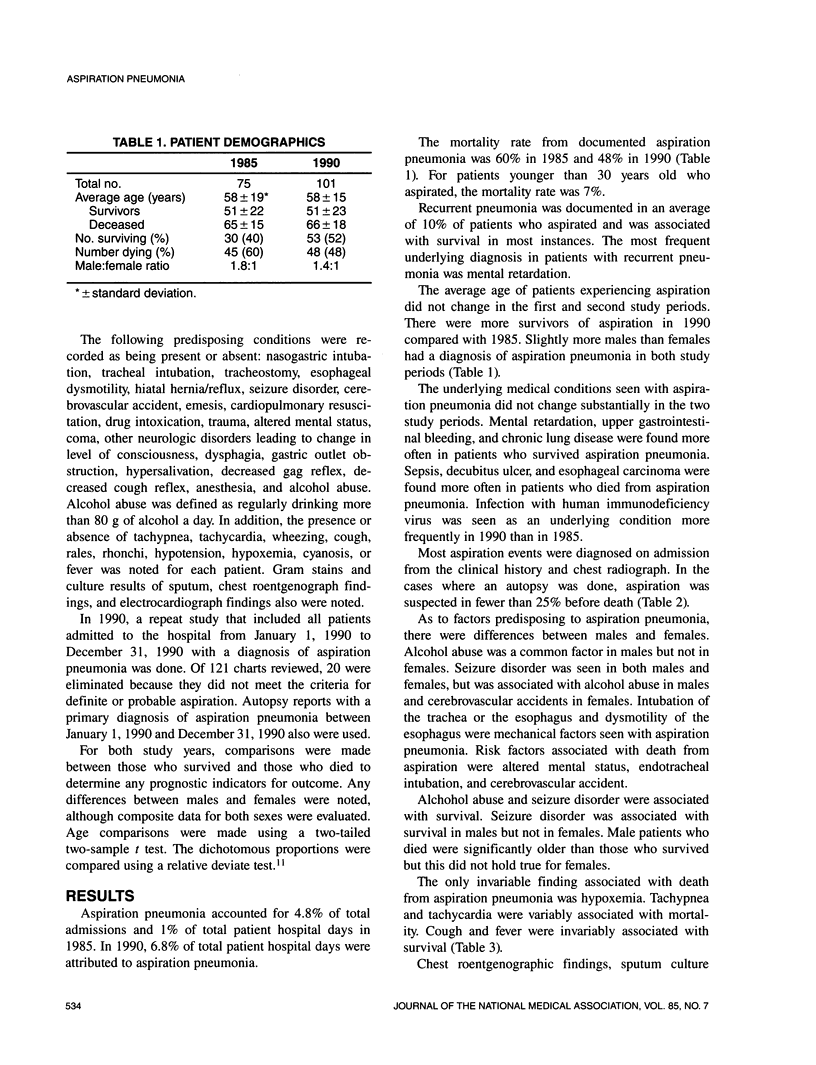
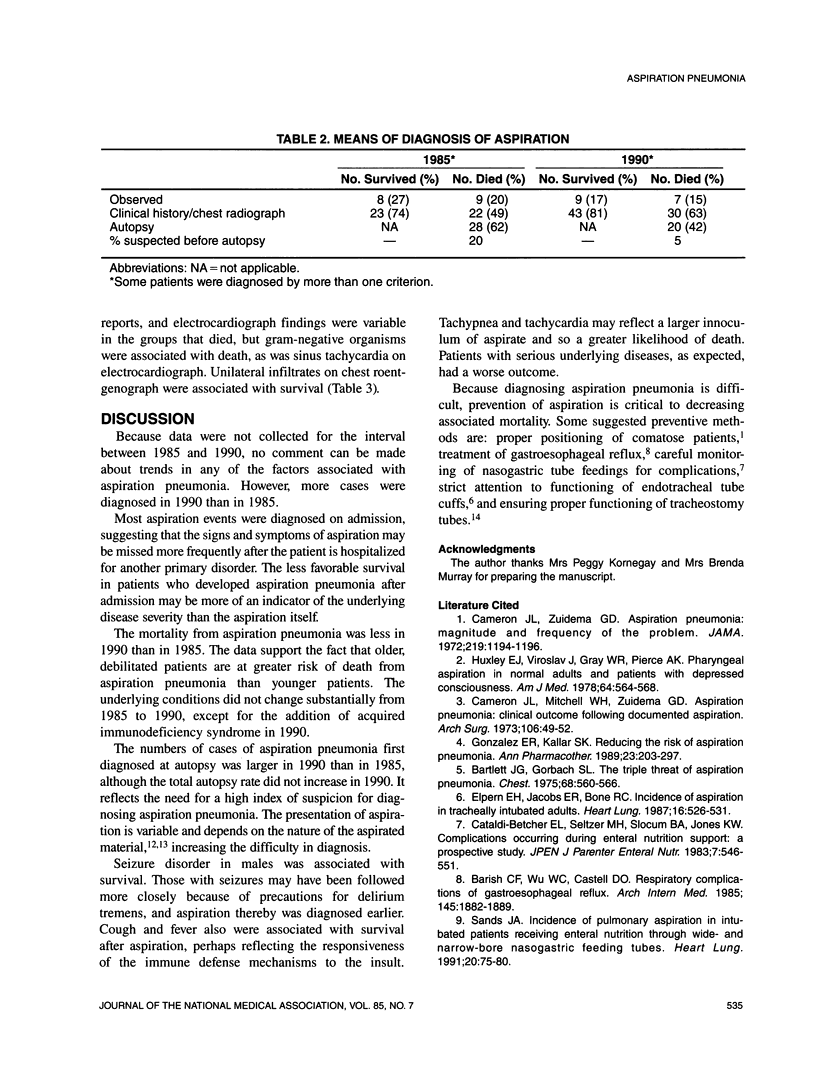
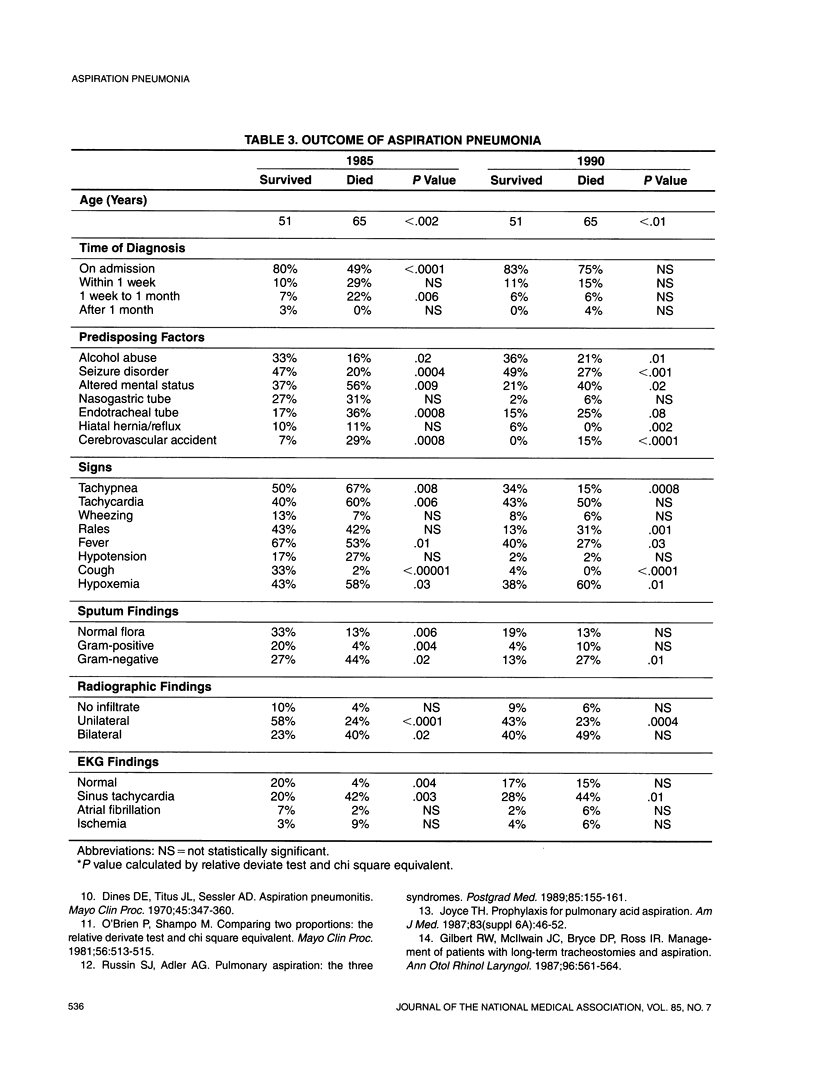
Because aspiration pneumonia contributes significantly to morbidity and mortality in hospitalized patients, this study was undertaken to identify risk factors for morbidity and mortality associated with aspiration pneumonia. Patients with a discharge diagnosis of aspiration pneumonia in 1985 and 1990 were studied. Factors associated with death from aspiration pneumonia were: altered mental status, cerebrovascular accident, endotracheal intubation, tachycardia, and hypoxemia. Fever, cough, and unilateral infiltrates on chest radiograph were associated with survival. Attention to proper positioning of comatose patients, aggressive treatment of gastroesophageal reflux, and strict attention to endotracheal tubes and tracheostomies should decrease the morbidity and mortality associated with aspiration pneumonia.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barish C. F., Wu W. C., Castell D. O. Respiratory complications of gastroesophageal reflux. Arch Intern Med. 1985 Oct;145(10):1882–1888. [PubMed] [Google Scholar]
- Bartlett J. G., Gorbach S. L. The triple threat of aspiration pneumonia. Chest. 1975 Oct;68(4):560–566. doi: 10.1378/chest.68.4.560. [DOI] [PubMed] [Google Scholar]
- Cameron J. L., Mitchell W. H., Zuidema G. D. Aspiration pneumonia. Clinical outcome following documented aspiration. Arch Surg. 1973 Jan;106(1):49–52. doi: 10.1001/archsurg.1973.01350130051011. [DOI] [PubMed] [Google Scholar]
- Cataldi-Betcher E. L., Seltzer M. H., Slocum B. A., Jones K. W. Complications occurring during enteral nutrition support: a prospective study. JPEN J Parenter Enteral Nutr. 1983 Nov-Dec;7(6):546–552. doi: 10.1177/0148607183007006546. [DOI] [PubMed] [Google Scholar]
- Dines D. E., Titus J. L., Sessler A. D. Aspiration pneumonitis. Mayo Clin Proc. 1970 May;45(5):347–360. [PubMed] [Google Scholar]
- Elpern E. H., Jacobs E. R., Bone R. C. Incidence of aspiration in tracheally intubated adults. Heart Lung. 1987 Sep;16(5):527–531. [PubMed] [Google Scholar]
- Gilbert R. W., Bryce D. P., McIlwain J. C., Ross I. R. Management of patients with long-term tracheotomies and aspiration. Ann Otol Rhinol Laryngol. 1987 Sep-Oct;96(5):561–564. doi: 10.1177/000348948709600516. [DOI] [PubMed] [Google Scholar]
- Gonzalez E. R., Kallar S. K. Reducing the risk of aspiration pneumonitis. DICP. 1989 Mar;23(3):203–208. doi: 10.1177/106002808902300302. [DOI] [PubMed] [Google Scholar]
- Huxley E. J., Viroslav J., Gray W. R., Pierce A. K. Pharyngeal aspiration in normal adults and patients with depressed consciousness. Am J Med. 1978 Apr;64(4):564–568. doi: 10.1016/0002-9343(78)90574-0. [DOI] [PubMed] [Google Scholar]
- O'Brien P. C., Shampo M. A. Statistics for clinicians. 8. Comparing two proportions: the relative deviate test and chi-square equivalent. Mayo Clin Proc. 1981 Aug;56(8):513–515. [PubMed] [Google Scholar]
- Russin S. J., Adler A. G. Pulmonary aspiration. The three syndromes. Postgrad Med. 1989 Jan;85(1):155-6, 159-61. doi: 10.1080/00325481.1989.11700542. [DOI] [PubMed] [Google Scholar]
- Sands J. A. Incidence of pulmonary aspiration in intubated patients receiving enteral nutrition through wide- and narrow-bore nasogastric feeding tubes. Heart Lung. 1991 Jan;20(1):75–80. [PubMed] [Google Scholar]


