Abstract
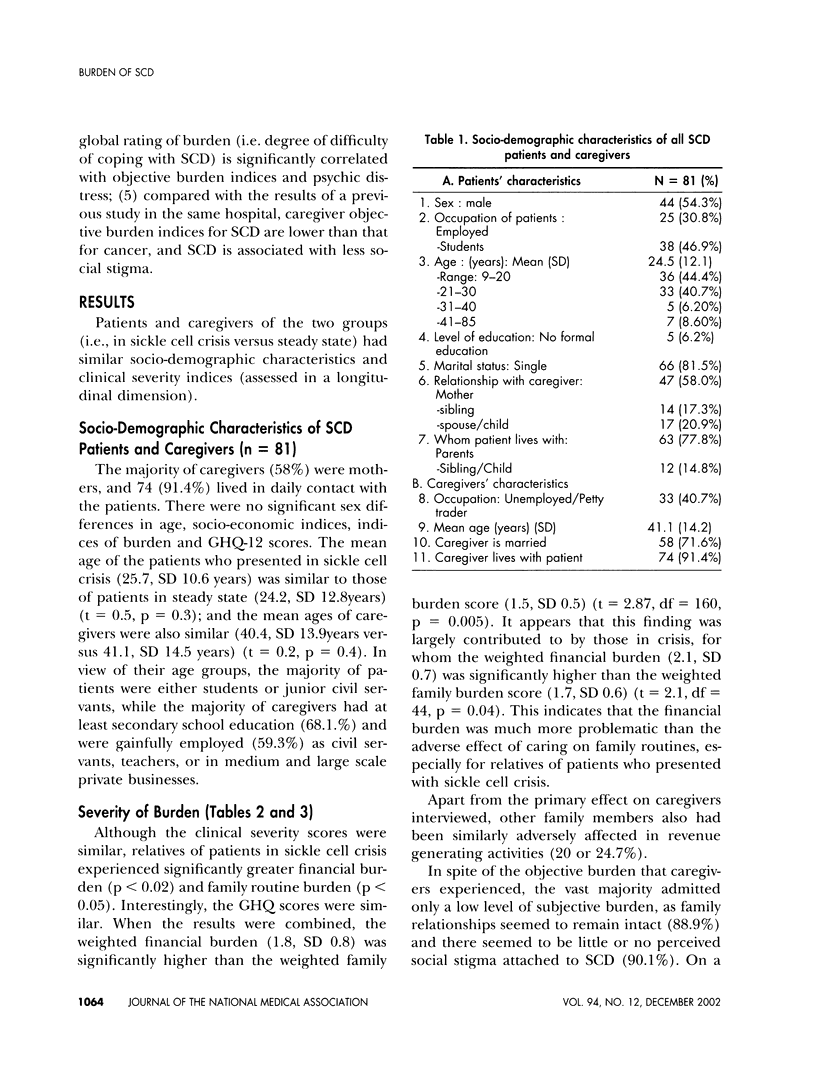
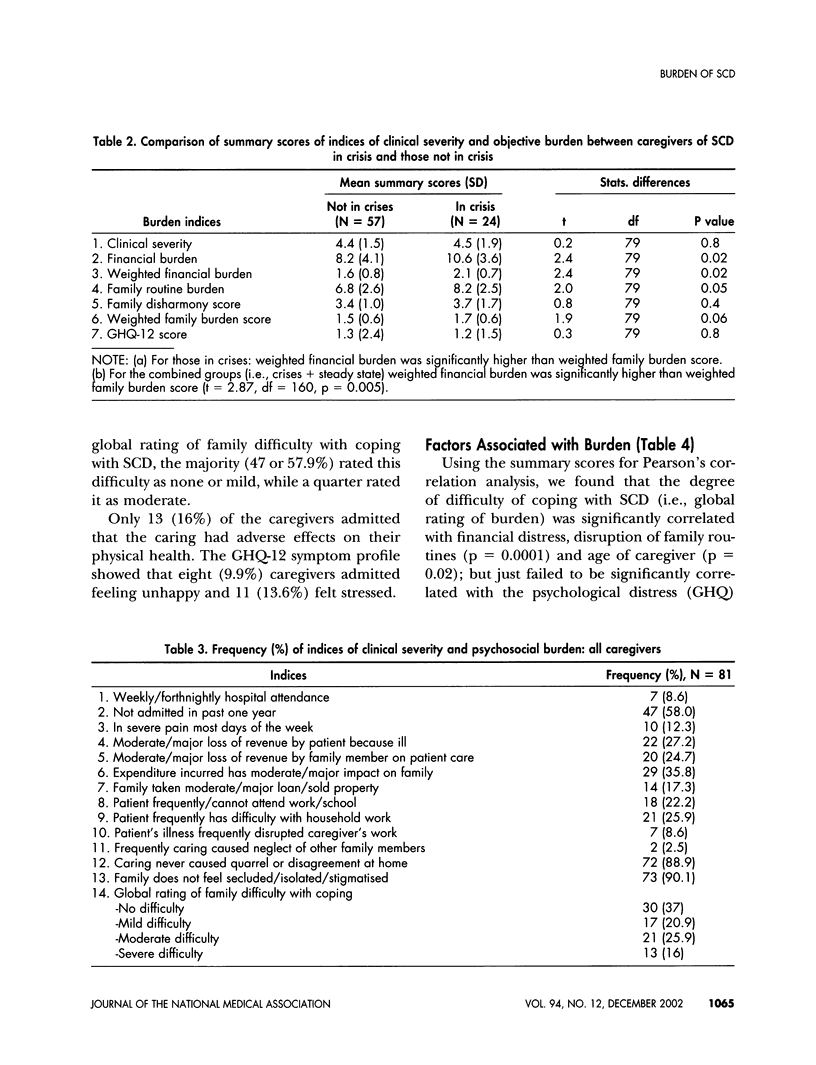
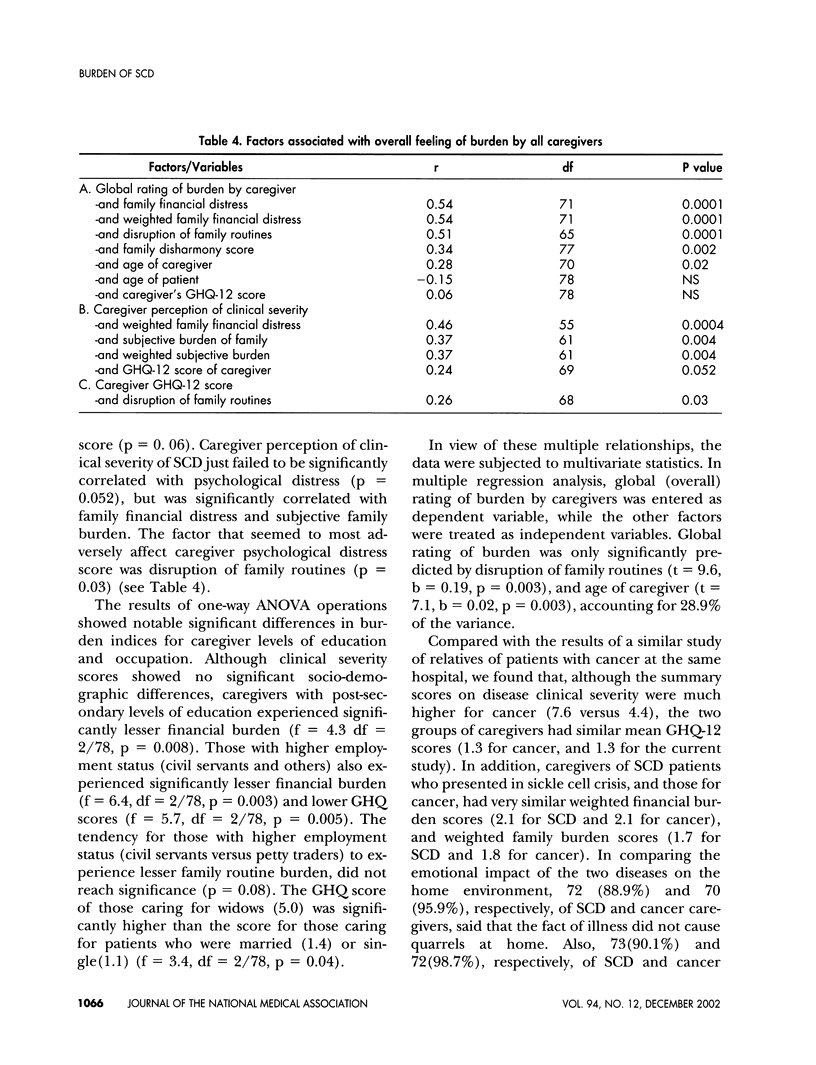
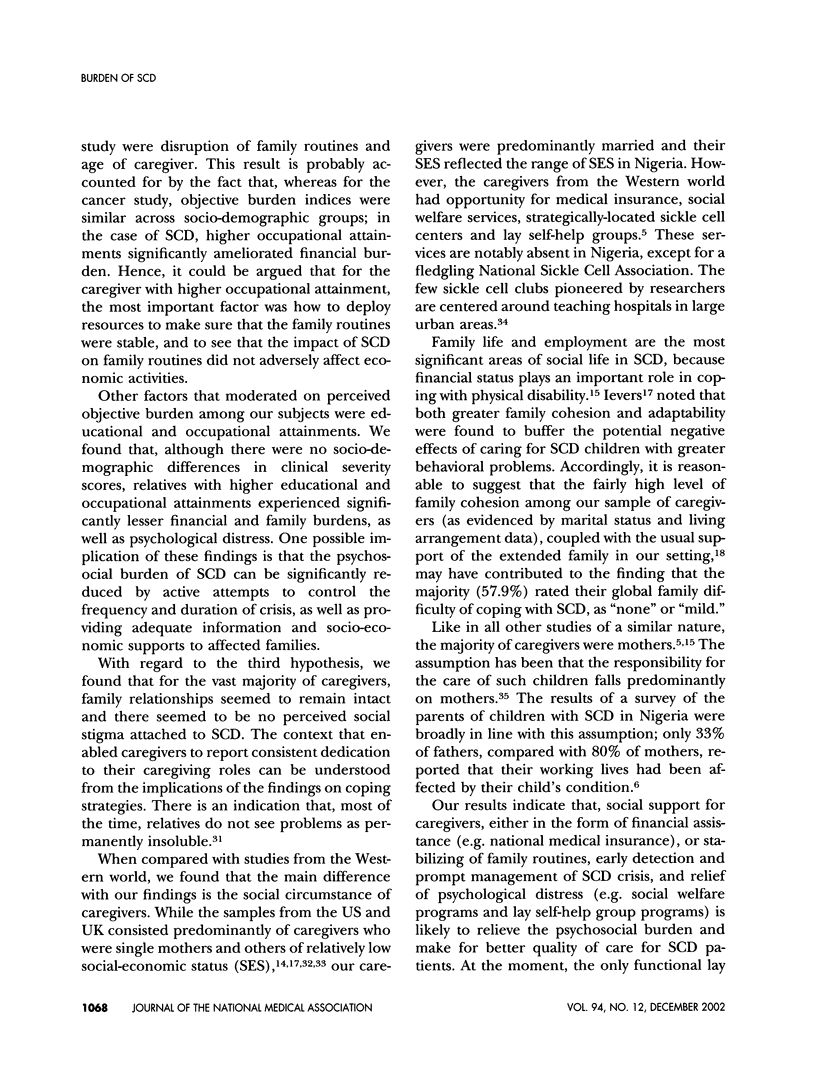
In Nigeria, with a high prevalence of sickle cell disease (SCD), families bear most of the burden of care for patients with this chronically disabling illness, because there are no national social welfare provisions. To assess the severity of indices of psychosocial burden among relatives of 24 SCD patients in crisis, in comparison with relatives of 57 SCD patients in stable condition. Cross-sectional study, using a burden instrument and Goldberg's General Health Questionnaire. Objective burden indices were significantly higher for SCD in crisis. The financial burden of SCD in crisis was significantly higher than the burden of disruption of family routines. 57.9% of all caregivers experienced little or no difficulty coping with SCD. Relatives with higher educational and occupational attainments (compared with those with lower attainments) experienced significantly lesser financial burden, disruption of family routines, and psychological distress. Compared with a similar study of cancer patients, relatives of patients in SCD crisis perceived similar financial, family routine burdens and psychological distress scores. Compared with US and UK reports, our caregivers were predominantly married and reflected the national range of socioeconomic groups. Global rating of burden was significantly predicted by disruption of family routines and higher age of caregivers. The psychosocial burden of SCD can be significantly reduced by controlling the frequency and duration of crises, as well as providing adequate information and socioeconomic support to families. Hematology staff should be sensitive to the psychosocial dimensions of SCD.
Full text
PDF







Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abiodun O. A. Psychosocial complications and management of sickle cell disease. East Afr Med J. 1993 Jan;70(1):40–42. [PubMed] [Google Scholar]
- Akinyanju O. O., Anionwu E. N. Training of counsellors on sickle-cell disorders in Africa. Lancet. 1989 Mar 25;1(8639):653–654. doi: 10.1016/s0140-6736(89)92152-1. [DOI] [PubMed] [Google Scholar]
- Bamisaiye A., Bakare C. G., Olatawura M. O. Some social-psychologic dimensions of sickle cell anemia among Nigerians. Clin Pediatr (Phila) 1974 Jan;13(1):56–59. doi: 10.1177/000992287401300107. [DOI] [PubMed] [Google Scholar]
- Brozović M., Davies S. C., Brownell A. I. Acute admissions of patients with sickle cell disease who live in Britain. Br Med J (Clin Res Ed) 1987 May 9;294(6581):1206–1208. doi: 10.1136/bmj.294.6581.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadman D., Rosenbaum P., Boyle M., Offord D. R. Children with chronic illness: family and parent demographic characteristics and psychosocial adjustment. Pediatrics. 1991 Jun;87(6):884–889. [PubMed] [Google Scholar]
- Famuyiwa O. O., Asuni T. A standardized schedule for burden on the family of sickle-cell anaemia sufferers. J Trop Med Hyg. 1991 Aug;94(4):277–282. [PubMed] [Google Scholar]
- Fleming A. F., Storey J., Molineaux L., Iroko E. A., Attai E. D. Abnormal haemoglobins in the Sudan savanna of Nigeria. I. Prevalence of haemoglobins and relationships between sickle cell trait, malaria and survival. Ann Trop Med Parasitol. 1979 Apr;73(2):161–172. doi: 10.1080/00034983.1979.11687243. [DOI] [PubMed] [Google Scholar]
- Gentry B. F., Varlik L., Dancer J. Adolescents' perceptions of psychosocial factors related to sickle cell disease. Percept Mot Skills. 1998 Apr;86(2):626–626. doi: 10.2466/pms.1998.86.2.626. [DOI] [PubMed] [Google Scholar]
- Hoenig J., Hamilton M. W. The schizophrenic patient in the community and his effect on the household. Int J Soc Psychiatry. 1966 Summer;12(3):165–176. doi: 10.1177/002076406601200301. [DOI] [PubMed] [Google Scholar]
- Hurtig A. L., Koepke D., Park K. B. Relation between severity of chronic illness and adjustment in children and adolescents with sickle cell disease. J Pediatr Psychol. 1989 Mar;14(1):117–132. doi: 10.1093/jpepsy/14.1.117. [DOI] [PubMed] [Google Scholar]
- Ievers C. E., Brown R. T., Lambert R. G., Hsu L., Eckman J. R. Family functioning and social support in the adaptation of caregivers of children with sickle cell syndromes. J Pediatr Psychol. 1998 Dec;23(6):377–388. doi: 10.1093/jpepsy/23.6.377. [DOI] [PubMed] [Google Scholar]
- Iloeje S. O. Psychiatric morbidity among children with sickle-cell disease. Dev Med Child Neurol. 1991 Dec;33(12):1087–1094. doi: 10.1111/j.1469-8749.1991.tb14831.x. [DOI] [PubMed] [Google Scholar]
- King E. H. Child-rearing practices: child with chronic illness and well sibling. Issues Compr Pediatr Nurs. 1981 May-Jun;5(3):185–194. doi: 10.3109/01460868109105397. [DOI] [PubMed] [Google Scholar]
- Martyns-Yellowe I. S. The burden of schizophrenia on the family. A study from Nigeria. Br J Psychiatry. 1992 Dec;161:779–782. doi: 10.1192/bjp.161.6.779. [DOI] [PubMed] [Google Scholar]
- Nadel C., Portadin G. Sickle cell crises: psychological factors associated with onset. N Y State J Med. 1977 Jun;77(7):1075–1078. [PubMed] [Google Scholar]
- Ohaeri J. U., Campbell O. B., Ilesanmi A. O., Omigbodun A. O. The psychosocial burden of caring for some Nigerian women with breast cancer and cervical cancer. Soc Sci Med. 1999 Dec;49(11):1541–1549. doi: 10.1016/s0277-9536(99)00223-3. [DOI] [PubMed] [Google Scholar]
- Ohaeri J. U., Odejide O. A. Somatization symptoms among patients using primary health care facilities in a rural community in Nigeria. Am J Psychiatry. 1994 May;151(5):728–731. doi: 10.1176/ajp.151.5.728. [DOI] [PubMed] [Google Scholar]
- Ohaeri J. U. Perception of the social support role of the extended family network by some Nigerians with schizophrenia and affective disorders. Soc Sci Med. 1998 Nov;47(10):1463–1472. doi: 10.1016/s0277-9536(98)00111-7. [DOI] [PubMed] [Google Scholar]
- Ohaeri J. U., Shokunbi W. A., Akinlade K. S., Dare L. O. The psychosocial problems of sickle cell disease sufferers and their methods of coping. Soc Sci Med. 1995 Apr;40(7):955–960. doi: 10.1016/0277-9536(94)00154-l. [DOI] [PubMed] [Google Scholar]
- Ohaeri J. U., Sunmola A. M. The pattern of dreams of a sample of Nigerians. J Anal Psychol. 1994 Jul;39(3):361–372. doi: 10.1111/j.1465-5922.1994.00361.x. [DOI] [PubMed] [Google Scholar]
- Platt O. S., Brambilla D. J., Rosse W. F., Milner P. F., Castro O., Steinberg M. H., Klug P. P. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994 Jun 9;330(23):1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- Platt S. Measuring the burden of psychiatric illness on the family: an evaluation of some rating scales. Psychol Med. 1985 May;15(2):383–393. doi: 10.1017/s0033291700023680. [DOI] [PubMed] [Google Scholar]
- Thompson R. J., Jr, Gil K. M., Abrams M. R., Phillips G. Stress, coping, and psychological adjustment of adults with sickle cell disease. J Consult Clin Psychol. 1992 Jun;60(3):433–440. doi: 10.1037//0022-006x.60.3.433. [DOI] [PubMed] [Google Scholar]