Abstract
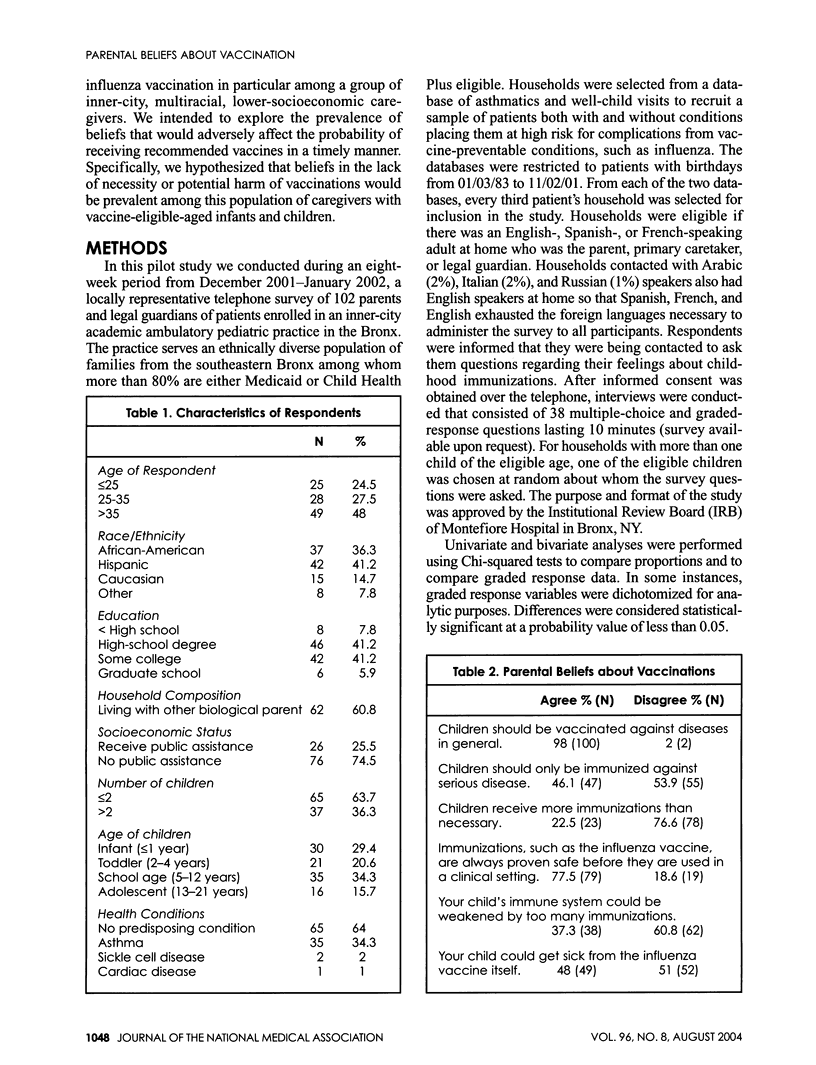
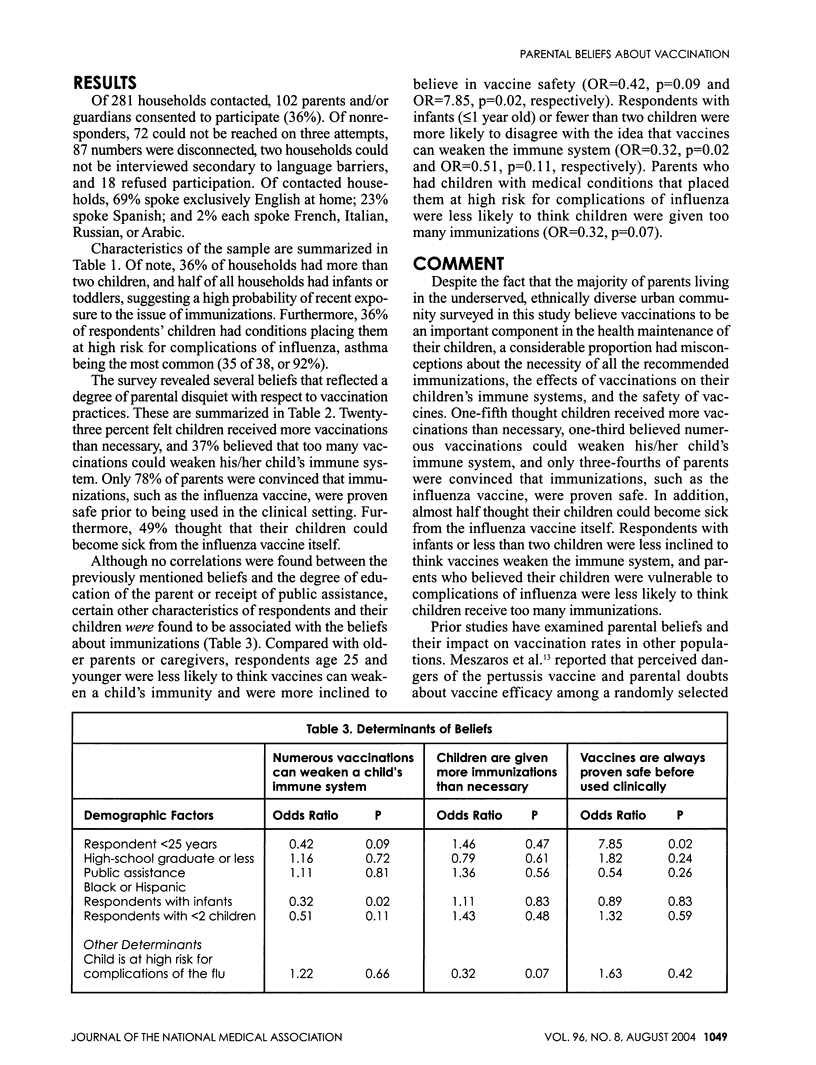
To characterize the knowledge and attitudes of an ethnically diverse group of inner-city parents regarding childhood immunizations, we conducted structured telephone interviews with 102 primary caretakers at an academic ambulatory pediatric practice during the winter of 2001-2002. The sample was ethnically diverse, with 36% African-American, 41% Hispanic, and 15% white. Half the households had infants or toddlers in the home, and 36% had children with conditions placing them at high risk for influenza. Almost all parents felt that their children should be immunized against diseases in general (98%), but significant proportions also believed that children received more immunizations than necessary (23%), that immunizations could weaken a child's immune system (36%), or that the influenza vaccine could itself make a child ill (48%). Younger parents, those with infants, and parents of children at risk for complications of influenza were less likely to hold these beliefs while race/ethnicity, marital status, parent's education, or socioeconomic status could not be shown to have any effect. We conclude that many inner-city parents question the effects of childhood immunizations and hold erroneous beliefs about them irrespective of age, race, socioeconomic status, or educational background. Practitioners should address these beliefs in efforts to diminish disparities in immunization levels associated with inner-city multiethnic populations.
Full text
PDF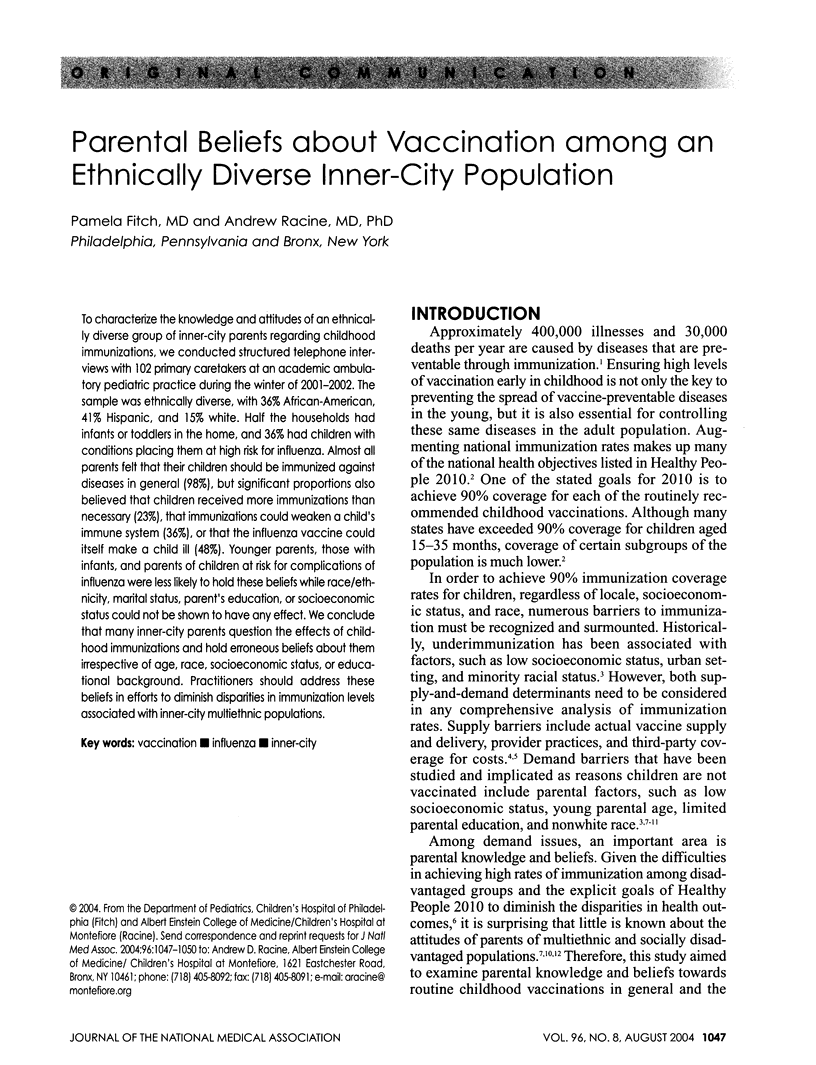

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bates A. S., Wolinsky F. D. Personal, financial, and structural barriers to immunization in socioeconomically disadvantaged urban children. Pediatrics. 1998 Apr;101(4 Pt 1):591–596. doi: 10.1542/peds.101.4.591. [DOI] [PubMed] [Google Scholar]
- Brenner R. A., Simons-Morton B. G., Bhaskar B., Das A., Clemens J. D., NIH-D.C. Initiative Immunization Working Group Prevalence and predictors of immunization among inner-city infants: a birth cohort study. Pediatrics. 2001 Sep;108(3):661–670. doi: 10.1542/peds.108.3.661. [DOI] [PubMed] [Google Scholar]
- Cohen Jon. Public health. U.S. vaccine supply falls seriously short. Science. 2002 Mar 15;295(5562):1998–2001. doi: 10.1126/science.295.5562.1998. [DOI] [PubMed] [Google Scholar]
- Gellin B. G., Maibach E. W., Marcuse E. K. Do parents understand immunizations? A national telephone survey. Pediatrics. 2000 Nov;106(5):1097–1102. doi: 10.1542/peds.106.5.1097. [DOI] [PubMed] [Google Scholar]
- Lannon C., Brack V., Stuart J., Caplow M., McNeill A., Bordley W. C., Margolis P. What mothers say about why poor children fall behind on immunizations. A summary of focus groups in North Carolina. Arch Pediatr Adolesc Med. 1995 Oct;149(10):1070–1075. doi: 10.1001/archpedi.1995.02170230024003. [DOI] [PubMed] [Google Scholar]
- Luman Elizabeth T., McCauley Mary Mason, Shefer Abigail, Chu Susan Y. Maternal characteristics associated with vaccination of young children. Pediatrics. 2003 May;111(5 Pt 2):1215–1218. [PubMed] [Google Scholar]
- Lutwick S. M. Pediatric vaccine compliance. Pediatr Clin North Am. 2000 Apr;47(2):427–434. doi: 10.1016/s0031-3955(05)70215-7. [DOI] [PubMed] [Google Scholar]
- Meszaros J. R., Asch D. A., Baron J., Hershey J. C., Kunreuther H., Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol. 1996 Jun;49(6):697–703. doi: 10.1016/0895-4356(96)00007-8. [DOI] [PubMed] [Google Scholar]
- Shefer A., Briss P., Rodewald L., Bernier R., Strikas R., Yusuf H., Ndiaye S., Wiliams S., Pappaioanou M., Hinman A. R. Improving immunization coverage rates: an evidence-based review of the literature. Epidemiol Rev. 1999;21(1):96–142. doi: 10.1093/oxfordjournals.epirev.a017992. [DOI] [PubMed] [Google Scholar]
- Taylor J. A., Darden P. M., Slora E., Hasemeier C. M., Asmussen L., Wasserman R. The influence of provider behavior, parental characteristics, and a public policy initiative on the immunization status of children followed by private pediatricians: a study from Pediatric Research in Office Settings. Pediatrics. 1997 Feb;99(2):209–215. [PubMed] [Google Scholar]
- Waldhoer T., Haidinger G., Vutuc C., Haschke F., Plank R. The impact of sociodemographic variables on immunization coverage of children. Eur J Epidemiol. 1997 Feb;13(2):145–149. doi: 10.1023/a:1007359632218. [DOI] [PubMed] [Google Scholar]
- Wood D., Halfon N., Donald-Sherbourne C., Mazel R. M., Schuster M., Hamlin J. S., Pereyra M., Camp P., Grabowsky M., Duan N. Increasing immunization rates among inner-city, African American children. A randomized trial of case management. JAMA. 1998 Jan 7;279(1):29–34. doi: 10.1001/jama.279.1.29. [DOI] [PubMed] [Google Scholar]


