Abstract
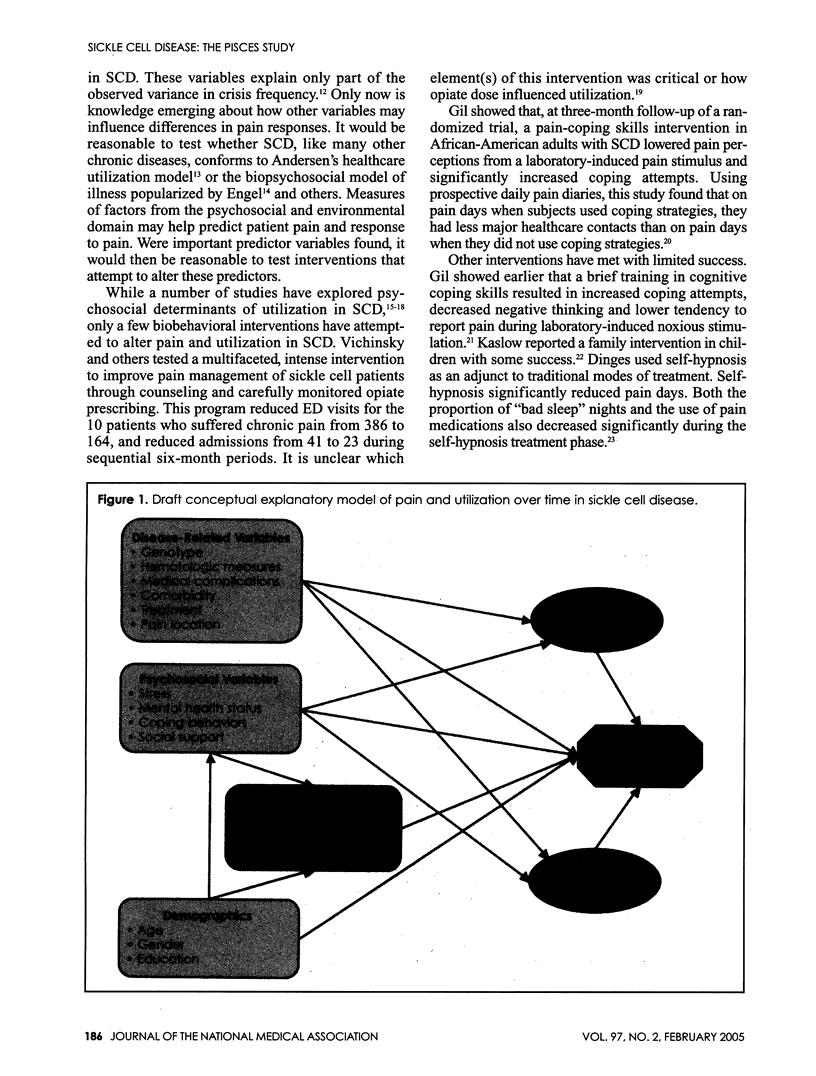
Until recent decades, sickle cell disease (SCD) was associated with recurrent, disabling pain, organ failure and death in childhood or early adulthood. SCD treatment advances have now decreased pain and prolonged survival, but episodic or chronic pain may still require substantial analgesic use and frequent hospitalization for pain episodes. This pain is poorly characterized and often poorly treated. Adult patients may face barriers to comprehensive SCD care, stigmatization of their care-seeking behavior by providers and lack of family support, forcing them into maladaptive coping strategies. The Pain in Sickle Cell Epidemiology Study (PiSCES) attempts to develop and validate a biopsychosocial model of SCD pain, pain response and healthcare utilization in a large, multisite adult cohort. PiSCES participants complete a baseline survey and six months of daily pain diaries in which they record levels of SCD-related pain and related disability and distress as well as responses to pain (e.g., medication use, hospital visits). PiSCES will advance methods of measuring pain and pain response in SCD by better describing home-managed as well as provider-managed pain. PiSCES will assess the relative contributions of biological (disease-related), psychosocial and environmental (readiness to utilize) factors to overall pain and pain response in SCD, suggesting targets for biobehavioral interventions over time. Importantly, PiSCES will also identify "triggers" of SCD pain episodes and healthcare utilization in the moment of pain, suggesting targets for timely care that mutes pain episodes.
Full text
PDF









Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baum K. F., Dunn D. T., Maude G. H., Serjeant G. R. The painful crisis of homozygous sickle cell disease. A study of the risk factors. Arch Intern Med. 1987 Jul;147(7):1231–1234. [PubMed] [Google Scholar]
- Charache S., Terrin M. L., Moore R. D., Dover G. J., Barton F. B., Eckert S. V., McMahon R. P., Bonds D. R. Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia. N Engl J Med. 1995 May 18;332(20):1317–1322. doi: 10.1056/NEJM199505183322001. [DOI] [PubMed] [Google Scholar]
- Davis H., Schoendorf K. C., Gergen P. J., Moore R. M., Jr National trends in the mortality of children with sickle cell disease, 1968 through 1992. Am J Public Health. 1997 Aug;87(8):1317–1322. doi: 10.2105/ajph.87.8.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinges D. F., Whitehouse W. G., Orne E. C., Bloom P. B., Carlin M. M., Bauer N. K., Gillen K. A., Shapiro B. S., Ohene-Frempong K., Dampier C. Self-hypnosis training as an adjunctive treatment in the management of pain associated with sickle cell disease. Int J Clin Exp Hypn. 1997 Oct;45(4):417–432. doi: 10.1080/00207149708416141. [DOI] [PubMed] [Google Scholar]
- Gaston M. H., Verter J. I., Woods G., Pegelow C., Kelleher J., Presbury G., Zarkowsky H., Vichinsky E., Iyer R., Lobel J. S. Prophylaxis with oral penicillin in children with sickle cell anemia. A randomized trial. N Engl J Med. 1986 Jun 19;314(25):1593–1599. doi: 10.1056/NEJM198606193142501. [DOI] [PubMed] [Google Scholar]
- Gaston M., Rosse W. F. The cooperative study of sickle cell disease: review of study design and objectives. Am J Pediatr Hematol Oncol. 1982 Summer;4(2):197–201. [PubMed] [Google Scholar]
- Gil K. M., Carson J. W., Sedway J. A., Porter L. S., Schaeffer J. J., Orringer E. Follow-up of coping skills training in adults with sickle cell disease: analysis of daily pain and coping practice diaries. Health Psychol. 2000 Jan;19(1):85–90. doi: 10.1037//0278-6133.19.1.85. [DOI] [PubMed] [Google Scholar]
- Gil K. M., Wilson J. J., Edens J. L., Webster D. A., Abrams M. A., Orringer E., Grant M., Clark W. C., Janal M. N. Effects of cognitive coping skills training on coping strategies and experimental pain sensitivity in African American adults with sickle cell disease. Health Psychol. 1996 Jan;15(1):3–10. doi: 10.1037//0278-6133.15.1.3. [DOI] [PubMed] [Google Scholar]
- Gil Karen M., Carson James W., Porter Laura S., Ready Jawana, Valrie Cecelia, Redding-Lallinger Rupa, Daeschner Charles. Daily stress and mood and their association with pain, health-care use, and school activity in adolescents with sickle cell disease. J Pediatr Psychol. 2003 Jul-Aug;28(5):363–373. doi: 10.1093/jpepsy/jsg026. [DOI] [PubMed] [Google Scholar]
- Gil Karen M., Carson James W., Porter Laura S., Scipio Cindy, Bediako Shawn M., Orringer Eugene. Daily mood and stress predict pain, health care use, and work activity in African American adults with sickle-cell disease. Health Psychol. 2004 May;23(3):267–274. doi: 10.1037/0278-6133.23.3.267. [DOI] [PubMed] [Google Scholar]
- Grant M. M., Gil K. M., Floyd M. Y., Abrams M. Depression and functioning in relation to health care use in sickle cell disease. Ann Behav Med. 2000 Spring;22(2):149–157. doi: 10.1007/BF02895779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaslow N. J., Collins M. H., Loundy M. R., Brown F., Hollins L. D., Eckman J. Empirically validated family interventions for pediatric psychology: sickle cell disease as an exemplar. J Pediatr Psychol. 1997 Apr;22(2):213–227. doi: 10.1093/jpepsy/22.2.213. [DOI] [PubMed] [Google Scholar]
- Lee A., Thomas P., Cupidore L., Serjeant B., Serjeant G. Improved survival in homozygous sickle cell disease: lessons from a cohort study. BMJ. 1995 Dec 16;311(7020):1600–1602. doi: 10.1136/bmj.311.7020.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991 Jan 15;133(2):144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- Murray N., May A. Painful crises in sickle cell disease--patients' perspectives. BMJ. 1988 Aug 13;297(6646):452–454. doi: 10.1136/bmj.297.6646.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt O. S., Brambilla D. J., Rosse W. F., Milner P. F., Castro O., Steinberg M. H., Klug P. P. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994 Jun 9;330(23):1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- Platt O. S., Thorington B. D., Brambilla D. J., Milner P. F., Rosse W. F., Vichinsky E., Kinney T. R. Pain in sickle cell disease. Rates and risk factors. N Engl J Med. 1991 Jul 4;325(1):11–16. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- Reese F. L., Smith W. R. Psychosocial determinants of health care utilization in sickle cell disease patients. Ann Behav Med. 1997 Spring;19(2):171–178. doi: 10.1007/BF02883334. [DOI] [PubMed] [Google Scholar]
- Scott R. B. Health care priority and sickle cell anemia. JAMA. 1970 Oct 26;214(4):731–734. [PubMed] [Google Scholar]
- Steinberg Martin H., Barton Franca, Castro Oswaldo, Pegelow Charles H., Ballas Samir K., Kutlar Abdullah, Orringer Eugene, Bellevue Rita, Olivieri Nancy, Eckman James. Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: risks and benefits up to 9 years of treatment. JAMA. 2003 Apr 2;289(13):1645–1651. doi: 10.1001/jama.289.13.1645. [DOI] [PubMed] [Google Scholar]
- Wierenga K. J., Hambleton I. R., Lewis N. A. Survival estimates for patients with homozygous sickle-cell disease in Jamaica: a clinic-based population study. Lancet. 2001 Mar 3;357(9257):680–683. doi: 10.1016/s0140-6736(00)04132-5. [DOI] [PubMed] [Google Scholar]
- Wison Schaeffer J. J., Gil K. M., Burchinal M., Kramer K. D., Nash K. B., Orringer E., Strayhorn D. Depression, disease severity, and sickle cell disease. J Behav Med. 1999 Apr;22(2):115–126. doi: 10.1023/a:1018755831101. [DOI] [PubMed] [Google Scholar]




