Abstract
Objectives:
This research studied motivations for, barriers to, and effects of online health information seeking and explored lay information mediary behavior (LIMB) characteristics in the consumer health information domain. Lay information mediaries (LIMs) seek information on behalf or because of others, without necessarily being asked to do so or engaging in follow up, and have represented more than 50% of health information seekers in prior studies.
Methods:
A web-based survey was posted on NC Health Info (NCHI) with 211 respondents, self-identified per the information need that brought them to NCHI as 20% LIMs (n = 43), 58% direct users (n = 122), and 22% health or information providers (n = 46). Follow-up telephone interviews were performed with 10% (n = 21). Interview analysis focused on lay participants (n = 15 LIMs and direct users combined). Interviewees were reclassified post-survey as 12 LIMs and 3 direct users when studied information behavior extended beyond NCHI search. Interview data were analyzed using grounded theory approach.
Results:
Surveyed LIMs were 77% female (n = 33) and searched on behalf or because of family members (81%, n = 35) and people they felt “extremely close” to (77%, n = 33). LIMs reported various information seeking barriers “sometimes” to “often.” LIMs searched mostly without prompting (51%, n = 22). Interview results triangulated survey findings regarding gender, tie strength, and prompting.
Conclusions:
LIMB may be related to gender and relationship tie strength and appears more internally than externally motivated. Further LIMB research is warranted.
Highlights
Lay information mediaries (LIMs) seek information on behalf or because of others without necessarily being asked to do so or engaging in follow up.
Most LIMs surveyed were female (77%, n = 33).
LIMs helped others overcome information-seeking barriers and affective and physical illness challenges (i.e., LIMs helped when patients were too weak or overwhelmed to seek, process, or share health information).
Results, such as those regarding information-seeking barrier experiences, suggest LIM information needs may differ from patient or direct-user needs.
Implications
LIMs may not self-identify and can have both intrinsically and extrinsically motivated information needs. Librarians should be aware of LIMs' potential hidden information needs and uses.
LIMs may also be recognized as “go-to” health information sources. Librarians may want to ask patients which people they consider their health information decision–making allies and tailor health information and outreach to them.
Further lay information mediary behavior research is warranted.
Introduction
“Seeking is of two strong emotions…
of tremendous frustration, and tremendous elation”
— NC Health Info user
Through web pages, email, instant messaging, forums, blogs, wikis, and so on, the Internet enables people to seek information about health concerns and issues for themselves as well as for other people—a growing phenomenon known as lay information mediary behavior (LIMB) [1]. Today's consumers are assuming increasingly active roles in health care as they participate in shared decision making and self-care [2,3]. Evolving health care policies requiring greater patient participation in medical decision making, rising chronic disease rates, and a growing aging population promise to magnify the impact of care giving and illness on patients, their families, friends, work colleagues, and providers [4–7]. For consumers, this impact frequently correlates with an increased need for health information. The purpose of this paper is to share findings on how three types of users—lay information mediary (LIM), direct user, and service provider—seek health information online, with a focus on identifying emergent LIMB characteristics in the consumer health information (CHI) domain.
Background and Theoretical Framework
Consumer Health Information–Seeking Challenges
The reasons people choose whether and how to engage in health information seeking are complex and vary depending on individual needs and circumstances [3, 8–12]. While the Internet expands opportunities to seek health information, numerous challenges to information seeking in general and online in particular exist. Both patients and their families express reluctance to “bother busy health professionals with [their] questions” [13]. Lack of health literacy—defined by the Institute of Medicine as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [14]—can negatively impact health outcomes by affecting consumers' ability to function and make informed health-related decisions in the health care environment and everyday life [15,16]. Consumers may be unfamiliar with health care systems, including what they offer and how they are best navigated [17,18]. Underserved groups—such as the homeless, disabled, and those distinguished by various cultural and socioeconomic factors—often lack access to digital information resources or culturally appropriate information [19–22].
Conceptual and linguistic mismatches between patients and health care providers or information system designers can also complicate health information acquisition [23]. Providers and information system designers frequently assume that patients desire formal, objective biomedical information, while patients, their families, and their friends often prefer more subjective, informal information about the realities of coping with illness in daily life [24–27]. Though Tetzlaff observes that “under conditions of personal stress people can be motivated to pursue salient technical material well beyond their customary reading level” [28], consumers may rely on linguistic gatekeepers, who can translate “medicalese” for them [3,28,29]. More information technology–literate individuals can also help others circumnavigate Internet searching challenges, usability issues, and impermanence of some websites [30].
The Lay Information Mediary (lim) Phenomenon in the Consumer Health Information (chi) Domain
In the library and information science (LIS) literature, those who seek information on behalf or because of others, with or without necessarily being asked to do so or engaging in follow up, have been referred to as LIMs.† This concept was key to the current study, an outcome of which was a model of LIMB [1]. Several previous studies have investigated aspects of LIMB outside the CHI domain [31–35].‡ While librarians, social workers, providers, and others seek information on behalf of others in a professional–client relationship, LIM studies have focused on lay information behavior as that is where the least is known. This study extended previous LIM-related LIS and health care studies by concentrating on LIMB and on the LIM's perspective in the CHI-seeking domain.
LIM Internet searching has been reported in over 50%–80% of populations studied [36–38], and references to aspects of LIMB in health information seeking abound. Ferguson described family, friends, and peers who search on behalf of patients and others as agents, e-patients, and patient-helpers. He noted their active presence in online environments and credited them with providing significant interpretive and psychosocial patient support [37,39,40]. In related findings, La Porta et al. found that online health information seekers were “more likely to contact” the National Cancer Institute's Cancer Information Service on behalf of others [41]. Emerging social networking technologies foster these and other LIM-related behaviors in online health information seeking and use [42–44]. Eysenbach defined “apomediaries” as “(peers) and/or technology (e.g., collaborative filtering tools) …(that) ‘stand by’ (information seekers) and provide added value” as they guide people to health information online [45].
LIM-related behavior in the context of CHI-seeking studies has been observed in various populations, including African Americans [19,46,47], Latino immigrants [48], women [18,49], adolescents [50], genetics information seekers [51], chronically ill children [52], online help seekers [53], Hispanic Internet users [54], and the elderly [19]. Lay health promoters; natural, teen, and peer helpers; and others also engage in LIMB on behalf of peers or significant others in their social or wider community network [55–58]. In caregiving, many providers refer to these significant others as “hidden patients” and have emphasized the importance of supporting their health as caregivers via informational and health care interventions [13, 36, 59–61]. Hepworth's study of informal caregivers provides valuable insight yet omits exploration of possible intrinsically motivated caregiver information needs [62]. Little is known about the motivations and effects of LIMB seeking in consumer health, yet LIMs' potential impact on those they search for is considerable.
Current Study and Methods
The current study focused on LIMB by investigating how three types of users—LIM, direct user, and service provider—sought CHI online and interacted with the consumer health website NC Health Info (NCHI) [63]. NCHI is a resource combining local North Carolina provider and health care services information with MedlinePlus database access. NCHI was the pilot project for the National Library of Medicine's (NLM's) Go Local initiative. Jointly created by the University of North Carolina–Chapel Hill's Health Sciences Library and School of Information and Library Science in collaboration with NLM, it was launched in January 2003. The Go Local approach seeks to be more responsive to contemporary health information seekers' needs. It centralizes health resources by and in states via digital information portals to local health services and education [64].
Four questions guided the study:
What circumstances trigger people to seek health information online?
What barriers do people encounter in the process of searching for online health information?
How do people use health information found online, particularly that obtained via NCHI?
What are the characteristics of LIM seeking in the CHI domain?
Following institutional review board approval, data were collected through online surveys and follow-up telephone interviews. Three sets of surveys and interview scripts were developed, one for each of the following user types:
LIM searchers (LIMs): people seeking for information on behalf or because of someone else;
direct users: people seeking for information for themselves; and
service providers (providers): people seeking for information in a professional capacity (i.e., as an information or health care provider, such as a physician, nurse, social worker, etc.).
Based on previous LIMB-related research, it was hypothesized that LIMs would intentionally seek information on behalf of others and expected that they would search primarily on behalf of those with whom they had strong ties. It was also predicted that LIM information seeking might occur without an explicit request or follow-up with the person precipitating the search [10, 31–35]. Due to the study's focus on nonprofessional information mediaries, data collection and analysis emphasized LIMs and direct users.
Surveys
Surveys consisted of thirty-three to forty-five questions, depending on user type (Appendix A online). Surveys included questions about respondents' health information needs, barriers faced in obtaining or providing health information, anticipated and actual information uses and outcomes, nature of LIM or provider contacts and relationships, and participant demographics. Survey questions about barriers were based on Baker and Manbeck's identification of barriers to obtaining or providing health information [65]. Specific questions regarding improvements to the NCHI website were also asked. The study focused on people's CHI seeking in context of actual behavior—as opposed to posing hypothetical questions out of context. Participants were asked questions relating to the purpose of their visit to NCHI and other past health information–seeking situations. This “person-in-situation” focus is part of the user-centered research paradigm espoused by Dervin and recognized for its ability to reveal user behaviors often hidden by more theoretical approaches [66]. The response structure for survey questions included frequency-based Likert scales and open-ended text boxes.
Survey instruments were pretested by thirty-five volunteer LIS graduate students. Pretesters identified no problems with question content or comprehensibility. Suggested improvements highlighted technical or usability details (e.g., preference for checkboxes vs. radio buttons) and resulted in only minor instrument revisions.
Surveys were deployed using the University of Washington's online survey tool, WebQ, and ran on the NCHI website for 21 consecutive days in February 2004. Pop-up methodology was used to randomly invite survey participants with frequency set to 50% during the first 2 weeks and changed to 80% the final week to increase participant recruitment. On the main survey web page, participants were asked whether they were seeking information for themselves (direct user), on behalf of another (LIM), or as information or health care service providers, and participants were routed to the corresponding survey instrument. No survey participation incentive was offered. Participants could view survey and NCHI website windows simultaneously, which enabled those who were new to the site to answer survey questions while they viewed various web pages.
Interviews
Survey respondents were invited to participate in semi-structured follow-up interviews during surveys. This mixed method approach balanced the broader, more prescriptive survey questions with an opportunity for participants to provide more spontaneous, in-depth accounts of general CHI seeking and LIMB. No interview participation incentive was offered. Interview guides included fifteen to seventeen questions, depending on user type (Appendix B online). Interview question topics were similar to survey question topics and informed by preliminary survey results. This set the stage for interviews by identifying helpful probe questions and alerting researchers to participants' potential health information–seeking concerns and emerging themes. Interview guides were pretested on approximately six LIS graduate students to ensure that the questions were comprehensible and worked as anticipated. Five LIS graduate student researchers conducted the interviews and kept detailed field notes. Data integrity was further ensured by regular peer debriefing.
Interviews occurred between February 10 and April 19, 2004. Interview instruments were revised during the first week of interviews based on feedback from early interview experiences. Revisions included the addition or refinement of question probes and the deletion of a few words in a question, to enhance understandability. Interviews averaged twenty-five minutes and were audio-recorded except for one email interview response from a participant who could not be reached via telephone.
Survey and Interview Data Analysis
Quantitative survey data analysis was completed using SPSS and Excel. Open-ended survey responses were coded using content analysis. Reliability and validity of these results were ensured via a consensus-building process among researchers.
Interview recordings were transcribed by two transcribers and independently coded by a team of three LIS graduate students led by a fourth coder who was an experienced qualitative researcher–LIS graduate student. Two coders also served as interviewers. Data were analyzed using the grounded theory approach and Atlas.ti [67]. Codebook and coding revisions were iteratively reviewed by the coders under the guidance of two experienced LIS researchers (Fisher and Durrance). Intra-coder and inter-coder checks as well as analysis of data for observer-effect evidence reinforced analysis reliability. Inter-coder reliability checks included several meetings of all coders, during which study purpose, data, and codebook were reviewed. Additionally, emerging themes were compared with study findings on related phenomena. After review and discussion of coding decisions, including inter- and intra-coder reliability checks on a random selection of approximately 7 transcripts, the researchers made minor adjustments to the codebook. Final inter-coder agreement rate was 100%, measured informally as group consensus rate. This approach was based on recommendations from Lincoln and Guba for ensuring trustworthiness of qualitative research methods [68].
Following an overview of study participants and survey findings, interview findings are shared under seven themes.
Results
Survey Participant Characteristics
During the survey, NCHI had 11,611 unique visitors, 27,246 total visits, and 95,648 page views. Eliminating duplicate responses yielded 211 survey respondents: 43 LIMs (20%), 122 direct users (58%), and 46 providers (22%). Due to a design oversight, participation rate was not tracked, but an estimated 6,967 survey invitations were viewed. The overall survey participation rate was estimated at 3%. While web surveys often have low view and participation rates, this study's sample size and selection method precluded extensive statistical analysis. However, by study design, in-depth statistical analysis was not intended. Participation was judged sufficient given the study's exploratory purpose [69].
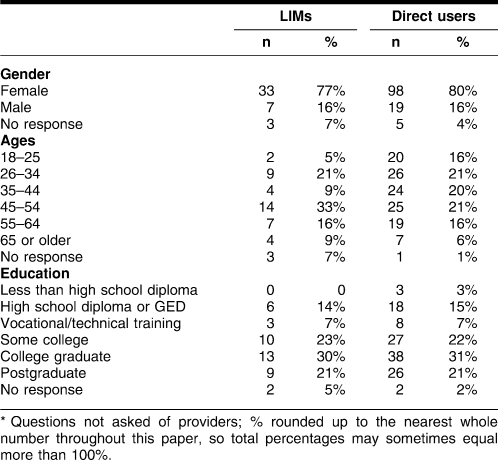
Most LIMs were female (77%, n = 33), age 45–54 (33%, n = 14), and college graduates (30%, n = 13). Direct users were primarily female (80%, n = 98), age 26–34 (21%, n = 26), and college graduates (31%, n = 38) (Table 1).
Table 1.
Survey participant demographics (lay information mediaries [LIMs]: n = 43 LIMs, direct users: n = 122)*
Providers were not surveyed about their age, gender, or education, though some post–high school education can be assumed for most. Providers were typically either educators (health educators, elementary teachers, etc.) or social workers (15%, n = 7 for both). Nurses represented 13% of providers (n = 6), while 11% (n = 5) were health administrators. Four providers (9%) were medical librarians. Few (less than 4%, n = 2) identified themselves as physicians, although it was conceivable that some health administrators or nonresponders were physicians; 8 did not respond. Most respondents lived or worked (providers) in North Carolina (LIMs: 70%, n = 30; direct users: 78%, n = 95; providers: 65%, n = 30).
Survey Results
Health Information–Seeking Triggers
A variety of circumstances triggered people to seek health information online. When asked, “What is the primary reason you are visiting NCHI today?”, both LIMs and direct users most commonly responded, “information on a specific condition” (LIMs: 47%, n = 20; direct users: 42%, n = 51), “information about a health-related program or service” (LIMs: 42%, n = 18; direct users: 30%, n = 36), or “for a health care provider” (LIMs: 19%, n = 8; direct users: 23%, n = 28); 4 direct users did not respond. Providers' chief needs were finding “information on a health-related program or service” (67%, n = 31) and “information on a specific condition” (24%, n = 11).
Health Information–Seeking Barriers
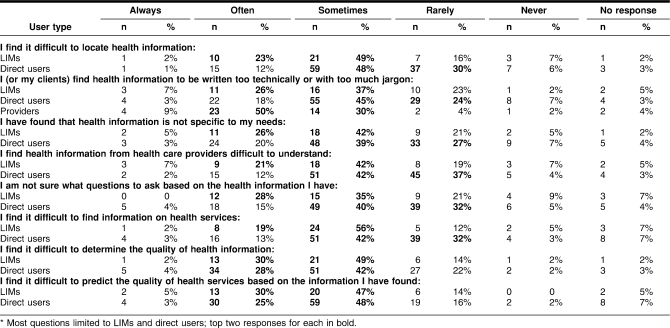
To elicit information about barriers people encounter while searching for health information online, survey respondents were asked to rate how frequently they encountered various obstacles using a five-point Likert scale (“always,” “often,” “sometimes,” “rarely,” and “never”). Results provided preliminary evidence of differences between LIMs' and direct users' information needs and challenges (Table 2).
Table 2.
Information seeking barriers encountered (LIMs: n = 43, direct users: n = 122, providers: n = 46)*
LIMs generally reported experiencing barriers “sometimes” to “often,” while direct users typically experienced barriers “sometimes” to “rarely.” Explanations offered in “other” narrative responses about barriers indicated that LIM barriers might be more related to health services offered or affective responses to the nature of their loved ones' situations rather than typical searcher deficiencies or information literacy challenges. One LIM commented, “My elderly parent is going to live with my daughter and there are so many issues to resolve I don't know where to begin.” Three LIMs indicated barriers were related to financing health care for their significant others involving Medicaid acceptance issues, cost, or insurance rules and allowances. Another LIM needed help locating a cardiologist and primary care practitioner for her mother but reported challenges knowing how to choose one “close by to (her) daughter,” possibly due to insufficient knowledge of local geography or applicable resources.
Neither LIMs nor direct users appeared to be uncomfortable asking health information questions. Both groups mostly reported being uncomfortable “asking questions about a certain topic” “rarely” (LIMs: 40%, n = 17; direct users: 38%, n = 46) to “sometimes” (LIMs: 26%, n = 11; direct users: 24%, n = 29); 4 LIMs and 8 direct users did not respond.
Ways People Use Chi Found Online, Particularly Nc Health Info (nchi) Information and Other Outcomes
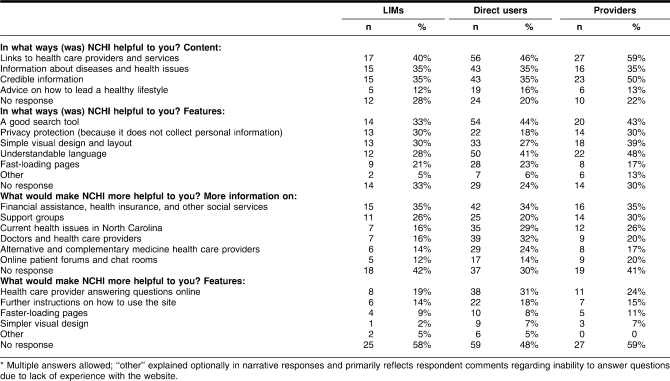
The majority of all respondents were first-time NCHI visitors (LIMs: 84%, n = 36; direct users: 83%, n = 101; providers: 72%, n = 33). Respondents were asked about their health information–seeking experiences using NCHI via a set of questions soliciting their opinions about what content or features were helpful to them and what content or features would “make NCHI more helpful” in the future. All respondents indicated that “links to health care providers and services” were currently most helpful while “advice on how to lead a healthy lifestyle” was least helpful. All respondents specified that “more information on financial assistance, health insurance, and other social services” was the most important content to add. The most commonly suggested feature among all respondents was “a health care provider answering questions online” (Table 3).
Table 3.
Existing helpful and desired NC Health Info (NCHI) content and features (LIMs: n = 43, direct users: n = 122, providers: n = 46)
Questions represented in Table 3 had high nonresponse rates, which could indicate that the questions inadequately assessed respondents' interests and needs. However, narrative “other” responses revealed that the majority of comments for these questions referred to the fact that several respondents were new to the NCHI site and had trouble answering these questions. Additional outcomes related to how participants used online health information, including NCHI-related and LIMB-related information, are reported below and in interview results.
Emerging Characteristics of Lay Information Mediary Behavior (limb) in the Chi Domain
Some characteristics of LIMB in the CHI domain have been referred to above. For the search that brought them to NCHI, LIMs searched on behalf of North Carolina residents 77% of the time (n = 33); 2 did not respond. The individuals for whom LIMs reported seeking information usually had less education than the LIMs themselves: only 16% (n = 7) were college graduates as opposed to 30% (n = 13) of LIMs; 23% (n = 10) of those whom LIMs searched on behalf of had not graduated from college and another 23% (n = 10) had “some college” education; 2 did not respond. Ages of those whom LIMs searched for were fairly evenly distributed, with a slight decrease in ages 55–64 (7%, n = 3) and a slight increase in those ages 65-plus (19%, n = 8); 2 did not respond.
LIMs typically engaged in their NCHI search on behalf of a family member (81%, n = 35) or a friend (9%, n = 4). Five percent (n = 2) searched for either a coworker/colleague or “other” (reported as a “brother's friend” or “for work”). LIMs described their relationship with the person for whom they sought information as “extremely close” 77% of the time (n = 33); 1 did not respond. More female LIMs surveyed searched on behalf of females (54%, n = 23) than on behalf of males (42%, n = 18); 2 did not respond.
When asked “how did you know that this search would be of interest to the person for whom you are seeking?”, 51% (n = 22) of surveyed LIMs said they volunteered to search on behalf of another because they were “interested in the person's situation.” Another 26% (n = 11) of LIMs reported being asked or prompted to search by others, and 19% (n = 8) described “other” reasons; 2 did not respond. These “other” responses suggested more affective or intrinsic reasons for LIMB; several revealed possible feelings of personal obligation or self-benefit (Table 4 online).
When asked, “where else have you turned for information” on the topic that brought them to NCHI, LIMs most frequently reported turning to other people—health care providers (61%, n = 23/38) and friends or relatives (42%, 16/38). LIMs also identified these people as the “most helpful” information resources for their current topic. Direct users reported turning to health care providers (43%, n = 39/91) and other websites most (42%, n = 38/91) and similarly identified these sources as “most helpful” (Tables 5 and 6 online). “Other” sources that LIMs consulted were typically miscellaneous (not specifically named) websites or search engines (n = 6), then friends (n = 4) and family (n = 3) (in addition to those reported above). “Most helpful” “other sources” for LIMs were professional organizations such as American Medical Association websites (n = 7). Direct users also consulted other miscellaneous websites or search engines (n = 9), though they more frequently turned to disease-related organizations (e.g., American Cancer Society) (n = 11). Direct users found these disease-related organizations “most helpful” (n = 6).
A more in-depth picture of LIMB characteristics emerged in the interview results, below.
Interview Participant Characteristics
Of the 211 survey respondents, 10% (n = 21) completed follow-up telephone interviews (self-identified for the survey as 2 LIMs, 13 direct users, and 6 providers). Because this paper centered on nonprofessionals or LIMB, interview results presented here emphasize LIM and direct-user participants (n = 15).
Though only 2 interviewees self-identified as LIMs for the searching incident that brought them to NCHI, 10 of 13 direct users (77%) interviewed described LIMB when reporting their non-NCHI health information–seeking behavior. Both original LIMs also described their own direct-user behavior. This behavior was included in the interview analysis as LIM or direct-user behavior on a per-reported instance basis and coded to reflect actual participant behavior (i.e., participants were labeled as LIMs or direct users depending on their behavior). A detailed interview coding scheme was developed to provide an audit trail for this. The total number of LIMs in interviews was 12 of 15 (80%); 3 of these 15 participants (20%) reported only direct-user behavior.
Interview Results
Emerging Limb Characteristics
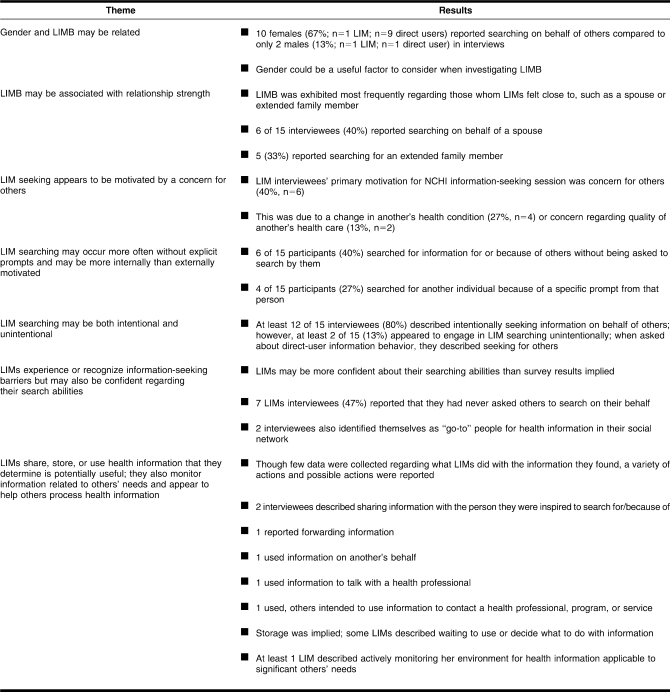
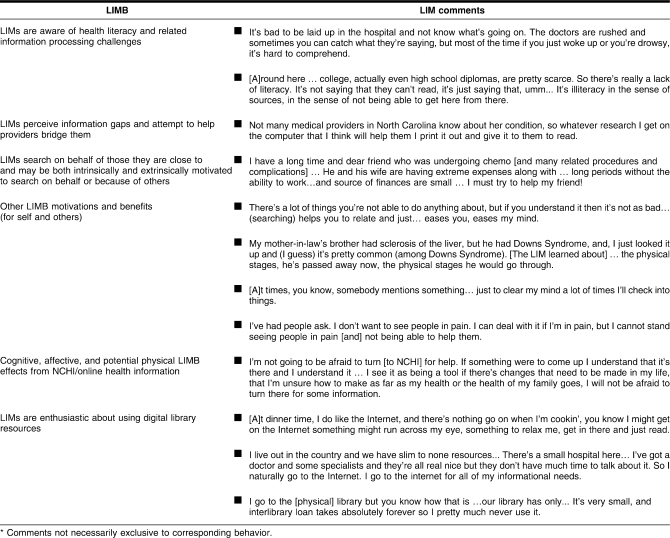
During interviews, several characteristics of LIMB emerged, identified as the following seven themes (Tables 7 and 8):
Table 7.
Emerging lay information mediary behavior (LIMB) interview themes (n = 15)
Table 8.
Selected LIM behaviors and narrative comments*
Gender and LIMB may be related.
LIMB may be associated with relationship strength.
LIM seeking appears to be motivated by a concern for others.
LIM searching may occur more often without explicit prompts and may be more internally than externally motivated.
LIM searching can be both intentional and unintentional.
LIMs experience or recognize information seeking barriers but may also be confident regarding their search abilities.
LIMs share, store, or use health information that they determine is potentially useful; they also monitor information related to others' needs and appear to assist others in processing information.
Nchi Use Outcomes
The impact of studied single information-seeking encounters with NCHI was difficult to assess. When asked what impact or anticipated impact NCHI use might have on future health management, 4 of 15 LIM and direct-user interviewees (27%) reported either no specific actions taken as a direct result of their NCHI use or that it was too early to tell whether there had been an impact. However, 3 themes began to emerge regarding NCHI use (users could provide more than 1 answer to this question). Six LIM (n = 2) and direct-user (n = 4) participants described a wide range of effects, summarized as:
affective: related to emotions (e.g., lessened worry about health care/procedures)
cognitive: improved understanding of issues, terminology, etc.
physical: led to a lifestyle or health behavior change, such as quitting smoking
These effects contributed to a conceptual model to be used for investigating emerging LIMB characteristics in future research [1] (Table 8).
Based on Durrance's “willingness to return” measure for information service evaluation, NCHI appeared successful because 18 of 21 total interviewees (86%) replied that they would use NCHI again [70]. Many said so with great enthusiasm; a few indicated they had already used NCHI repeatedly.
Discussion
The current study explored LIMB and information needs, seeking, and use among three online searcher types via a holistic approach that considered actual information uses and encompassed social, cognitive, affective, and physical factors related to health information seeking [1,65,71,72]. This investigation further demonstrated that NCHI and the Go Local model are promising tools for serving the varied needs of those studied.
Seeking health information proved to be a highly personal activity driven by situational and contextual factors. Several studies corroborated the findings concerning gender, preferences for providers and family or friends as information sources, tie strength, and various information needs reported [36, 46, 48, 49, 53, 54, 73–76]. Moreover, NCHI users described many of the same previously identified barriers to health information seeking, including those involving health literacy. Notably, LIMs appeared to play a role in helping those for whom they searched to overcome these barriers as well as those associated with affective and physical aspects of illness (i.e., when patients were too weak or overwhelmed to seek, process, or share health information themselves).
For the majority of reported barriers, LIMs indicated that they might have faced greater challenges than direct users, which could also indicate LIMs have a more realistic, health-literate, or cautious view of barriers related to CHI seeking. Another possibility was that direct users might be more familiar with a specific health concern through experience and interaction with the health care system than LIMs. LIMs' relationship to barriers appeared complex. Even a self-described and presumably successful “go-to” LIM interviewed, who reported regularly searching for and sharing information with others, revealed that she sometimes had difficulty assessing an information resource's authority. Another self-described “go-to” LIM reported difficulty finding information and determining its quality; she also said it was hard to find her own information, although she demonstrated good grasp of medical terms. One frequent LIM searcher reported difficulty in finding information but not in understanding it or asking questions. Another LIM interviewed indicated no problems with medical terminology but did acknowledge she had problems finding information that fitted her needs.
While several participants described general frustrations with seeking health information online, the majority demonstrated remarkable tenacity and faith that further seeking (sometimes offline) would enable them to fulfill their information needs. When asked, “What do you do to overcome challenges to getting the health and health services information you need?”, most surveyed replied that they would “keep going,” “find better key words,” or “persist in asking.” Zeng et al. found similar “positive attitudes” regarding health information seeking even with “failed queries.” Their suggestion that this might relate to users' “complex hidden goals” in information retrieval is worth considering in further research [71].
LIMs' and other users' desire to share information or communicate online with providers may alleviate fears that health information seeking will distance patients and providers. Respondents were also enthusiastic about using digital library resources. Throughout surveys and interviews, many expressed appreciation for and trust in professionally curated, online resources such as NCHI, MedlinePlus, and other National Institutes of Health–sponsored resources. Study results confirmed user interest in geographically based health services information and suggested that LIMs might be important participants in everyday health information seeking and related preventive, maintenance, and coping health behaviors for both patients and their significant others. When they seek and share health information for themselves and others, LIMs may help restore the order of everyday personal, family, or work life disrupted by illness [27,77,78].
Similar to LIMs in other domains, CHI-seeking LIMs monitored, shared, and stored information for themselves and others; sought and shared information as an expression of caring; and used searching to maintain or strengthen relationships or alleviate stress [31–35]. CHI-seeking LIMs might differ from other LIMs in that their searching appears more purposeful than not in its orientation to problem solving and decision support. Hypotheses that LIMs would intentionally seek information on behalf of others, that they would search primarily on behalf of those with whom they had strong ties, and that LIM information seeking might occur without an explicit request or follow-up with the person precipitating the search were borne out by results. Results depicting some direct users as unaware of their own LIM searching behaviors suggested that LIM searching might be disguised to some LIMs, possibly due to the self-benefit such seeking offered to them (i.e., in their minds, they were seeking for themselves). This failure to self-identify has also been observed in LIM-related natural helper and caregiver studies [79,80].
Limitations
Due to the conveniently recruited, small sample sizes and self-selection, the generalizability of results to the public-at-large is limited and statistical analysis of comparisons between user types is unwarranted. Limitations common to survey research include possible recall and response bias. Information regarding NCHI site promotional activities during sample recruitment period is unknown but could have affected participant representation. The only substantive participant complaint received regarding the survey was that some new NCHI users felt they lacked the time to familiarize themselves with the site before answering survey questions. In hindsight, some survey questions could have been prescriptive or confusing to respondents. A few questions excluded an option to provide “other” responses. Questions asking respondents to choose the “most helpful” resources and directing them to “choose all that apply” were intended to maximize participant input, but such instructions could have seemed contradictory to respondents. Also, provider questions worded as “my clients find” and so on might reflect providers' own opinions and experiences more than those of their clients, though such provider opinions proved valuable in their own right.
Several unanticipated yet compelling aspects of LIMB emerged during the study. These findings may both imply limitations and inspire further research questions regarding LIMB studies, such as: how can LIMs be best identified and studied, while accounting for everyday, iterative human health information behavior? The survey invited participants to self-identify as those “searching for another,” yet findings revealed that LIMs might also search for information “because of” or in response to another's health situation. Findings related to potential distinctions between these two search motivations are worth further exploration, as is consideration of why some participants failed to or had difficulty self-identifying as LIMs—was this due to study design, to LIMB characteristics, or both?
Study timing could affect applicability of some results. Data collection took place over a few months in 2004, with a gap of up eight weeks between some surveys and follow-up interviews. Future research will elucidate whether this is a true concern. As an exploratory investigation, study benefits outweighed limitations. The study's combined survey and interview approach demonstrated some triangulation of results (e.g., on LIM searching and gender, tie strength, prompting, etc.) and yielded rich preliminary insights into the complex phenomenon of LIMB in the CHI domain.
Implications and Conclusions
Implications for Health Librarians
Findings suggest several implications for librarians and information system developers serving hospital, public library, Internet, and community-based CHI seekers. Though LIMs frequently turn to other people when seeking information, little is known about their actual use of health library services in-person or virtually and related outcomes. To better understand LIMs' relationship to library resources, librarians might collect data regarding LIM use, keeping in mind that some such users may not self-identify. Librarians should be aware that LIMs who approach information services and providers may have both incomplete background information and “hidden” questions, information needs and uses that extend beyond presently known caregiver or patient needs. Librarians and clinicians can also query their patients/clients regarding which people they recognize as their primary information providers and health care decision–making partners and provide outreach services to them (keeping in mind that these people may not always be patients' spouses or others who typically are provided with patient-education and other information). Establishing and encouraging ongoing communication with LIMs and increasing LIM-specific services can foster a professional–lay partnership between information providers and LIMs that could enhance LIMs' ability to serve their significant others' needs as well as their own.
Conclusions
As Kleinman et al. have noted, the “great majority of health care takes place in the popular domain,” which includes family, social networks, and community [81]. This “popular” domain is central to LIM “work,” especially that related to two prevalent contemporary health care issues: chronic illness and elder care. Successful adaptation to lifestyle changes and compliance with any accompanying treatment regimens required by such situations depend on smooth integration of new health care routines into everyday life—something LIMs may be uniquely placed to facilitate. LIMs may also be especially adept at bridging cultural and digital divides for populations experiencing health disparities [31,32,54]. Pettigrew et al. have asserted that LIM-related information behaviors “foster social cohesion” because they are engaged in by people who are “socially connected and aware” of the information needs or interests of those around them. These “connected” individuals may be particularly helpful in communities considered to be “information poor” [82]. It is possible that their ability to build social capital in communities may also translate to an ability to help improve health outcomes by connecting community members with information helpful to health-related decision-making, coping, and preventive health behaviors.
While several health care studies have considered LIM-related information needs, these needs have frequently remained unmet and perhaps misunderstood [6, 83–85]. Few, if any, such studies have (1) conducted research from the information professionals' unique LIS perspective or (2) designed information-centric interventions tailored specifically to the LIM perspective (i.e., simultaneously serving both internally and externally motivated information needs LIMs appear to have, etc.). Librarians and other researchers may aid individual, community, and public health outcomes by investigating a variety of LIMB questions. A larger, systematic, and longitudinal study incorporating varied populations and integrated methods would enrich understanding and applicability of study results. Related research questions include asking (1) how LIM information needs differ from those of other health information seekers, (2) whether (and if so, why) LIMs conduct more frequent health information searches, and (3) whether LIMs have a more realistic view of the barriers and outcomes related to health literacy and using health information. Wathen and Harris recently studied women's health information seeking behavior in rural Canada and found that those they termed lay “intermediaries” played a “key role” in health information seeking [18]. They further noted that such LIM-related types could provide validation, comfort, and support, similar to what Saxton and Richardson described in professional intermediary research [86].
The authors suggest that future research should consider such possible LIMB effects and explore what affective personality attributes and identifiable social types may be common in LIMs [87]. It is also important to understand what the possible ethical considerations of LIMB are, how LIMs determine others' needs, and whether and how they judge the relevance of their findings or engage in follow-up activities with those for whom they search. Investigating these and other questions can further inform future LIM-oriented information system design and evaluation to support this growing population of health information seekers.
Electronic Content
Acknowledgments
This research was supported by a grant from the Institute of Museum and Library Services. Abrahamson's work was supported in part by National Institutes of Health grant no. 2T15LM007088 from the National Library of Medicine. The authors gratefully acknowledge Phillip M. Edwards, Eunice Kua, Dianne Ludwig, Maria Souden, and Kate Zoellner for their valuable contributions to data collection and analysis. In addition, the authors thank 2003–2004 NC Health Info staff, including Brian Hilligoss and Christie Silbajoris, AHIP, for their assistance and the research participants for sharing their health information–seeking experiences.
Footnotes
Based on a presentation at MLA '05, the 105th Annual Meeting of the Medical Library Association; San Antonio, TX; May 16, 2005.
Supplemental Appendixes A and B and Tables 4, 5, and 6 are available with the online version of this journal.
The “Discussion” section in Abrahamson and Fisher [1] provides rationale for use of the term “mediary.” It states: “according to Roget's New Millennium Thesaurus, ‘mediary’ encompasses many of the terms and behaviours that comprise [lay information mediary behavior (LIMB)], including proxy, agent, broker, etc. In [library and information science] and research from other disciplines, the term ‘mediate’ is commonly used to describe what professional information providers or intermediaries do. Because [lay information mediaries (LIMs)] may mediate on their own behalf, it makes conceptual sense to drop the inter- prefix (as they do not stand between anyone or intermediate when mediating on their own behalf).” The term “mediary” thus more accurately describes the full spectrum of LIM behavior than “intermediary.”
See Abrahamson and Fisher [1] for an overview of LIMB and an in-depth literature review regarding LIM-related types. N.B., this work previously referred to “lay information mediaries” as “proxies” [1]. Those LIMs seeking information on behalf or because of were originally referred to as “imposers” in Abrahamson and Fisher [1]; they are now referred to as “muses.” These changes were made to better reflect all dimensions of LIMB as described in Abrahamson and Fisher [1].
Contributor Information
Jennie A. Abrahamson, National Library of Medicine Fellow, Department of Medical Informatics and Clinical Epidemiology, Oregon Health & Science University, Mail Code: BICC, 3181 Southwest Sam Jackson Park Road, Portland, OR 97239 jenniea@u.washington.edu.
Karen E. Fisher, Associate Professor, The Information School, University of Washington, Box 352840, Seattle, WA 98195 fisher@u.washington.edu.
Anne G. Turner, Resource Center Director, The Cross Cultural Health Care Program, 4700 42nd Avenue Southwest, Suite 580, Seattle, WA 98116 resource@xculture.org.
Joan C. Durrance, Margaret Mann Collegiate Professor of Information, School of Information, University of Michigan, 1085 South University-3084 West Hall, Ann Arbor, MI 48109-1107 durrance@umich.edu.
Tammara Combs Turner, Senior Program Manager, Microsoft Corporation, One Microsoft Way, Redmond, WA 98052 tcombs@microsoft.com.
References
- 1.Abrahamson J.A., Fisher K.E. “What's past is prologue”: towards a general model of lay information mediary behaviour. Inform Res [Internet] 2007. Oct, [cited 23 Jun 2008]. < http://www.InformationR.net/ir/12-4/colis/colis15.html>.
- 2.Brennan P.F., Starren J.B. Consumer health informatics and telehealth. In: Shortliffe EH, Cimino JJ, eds. Biomedical informatics: computer applications in health care and biomedicine. 3rd ed. New York, NY: Springer; 2006. pp. 511–36. (Health informatics series). [Google Scholar]
- 3.Stavri P.Z. Personal health information-seeking: a qualitative review of the literature. Medinfo. 2001;10(pt 2):1484–8. [PubMed] [Google Scholar]
- 4.Deeken J.F., Taylor K.L., Mangan P., Yabroff K.R., Ingham J.M. Care for the caregivers: a review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage. 2003 Oct;26(4):922–53. doi: 10.1016/s0885-3924(03)00327-0. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman J. Awash in information, patients face a lonely, uncertain road. N Y Times [Internet] 2005. Aug 14, [cited 18 Apr 2008]. < http://www.nytimes.com/2005/08/14/health/14patient.html>. [PubMed]
- 6.Lim J., Zebrack B. Caring for family members with chronic physical illness: a critical review of caregiver literature. Health Qual Life Outcomes. 2004 Sep 17;2:50. doi: 10.1186/1477-7525-2-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Layne L.L. “How's the baby doing? ” struggling with narratives of progress in a neonatal intensive care unit. Medical Anthro Qtrly. 1996;10(4):624–56. doi: 10.1525/maq.1996.10.4.02a00130. [DOI] [PubMed] [Google Scholar]
- 8.Leydon G.M., Boulton M., Moynihan C., Jones A., Mossman J., Boudioni M., McPherson K. Cancer patients' information needs and information seeking behaviour: in depth interview study. BMJ. 2000 Apr 1;320(7239):909–13. doi: 10.1136/bmj.320.7239.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller S.M. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Cancer. 1995;76(2):167–77. doi: 10.1002/1097-0142(19950715)76:2<167::aid-cncr2820760203>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 10.Baker L.M., Pettigrew K.E. Theories for practitioners: two frameworks for studying consumer health information-seeking behavior. Bull Med Libr Assoc. 1999 Oct;87(4):444–50. [PMC free article] [PubMed] [Google Scholar]
- 11.Case D.O., Andrews J.E., Johnson J.D., Allard S.L. Avoiding versus seeking: the relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. J Med Libr Assoc. 2005 Jul;93(3):353–62. [PMC free article] [PubMed] [Google Scholar]
- 12.Brashers D.E., Goldsmith D.J., Hsieh E. Information seeking and avoiding in health contexts. Hum Commun Res. 2002;28(2):258–271. [Google Scholar]
- 13.Kristjanson L.J., Aoun S. Palliative care for families: remembering the hidden patients. Can J Psychiatry. 2004 Jun;49(6):359–65. doi: 10.1177/070674370404900604. [DOI] [PubMed] [Google Scholar]
- 14.Nielsen-Bohlman L., Panzer A.M., Kindig D.A. Institute of Medicine. Health literacy: a prescription to end confusion. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 15.McCray A.T. Promoting health literacy. J Am Med Inform Assoc. 2005 Mar;12(2):152–63. doi: 10.1197/jamia.M1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burkell J. What are the chances? evaluating risk and benefit information in consumer health materials. J Med Libr Assoc. 2004 Apr;92(2):200–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Baker L.M., Connor J.J. Physician-patient communication from the perspective of library and information science. Bull Med Libr Assoc. 1994 Jan;82(1):36–42. [PMC free article] [PubMed] [Google Scholar]
- 18.Wathen C.N., Harris R.M. An examination of the health information seeking experiences of women in rural Ontario, Canada. Inform Res [Internet] 2006. Jul, [cited 25 Feb 2007]. < http://www.informationr.net/ir/11-4/paper267.html>.
- 19.Detlefsen E.G. “Where am I to go? ” use of the Internet for consumer health information by two vulnerable communities. Lib Trends. 2004 Fall;53(2):283–300. [Google Scholar]
- 20.Cashen M.S., Sklar B.M., Nguyen H.H., Just M., Galzagorry G., Bakken S. Implementing a web-based information resource at an inner-city community church: lessons learned. Comput Inform Nurs. 2002 Nov;20(6):244–50. doi: 10.1097/00024665-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Berland G.K., Elliott M.N., Morales L.S., Algazy J.I., Kravitz R.L., Broder M.S., Kanouse D.E., Muñoz J.A., Puyol J.A., Lara M., Watkins K.E., Yang H., McGlynn E.A. Health information on the Internet: accessibility, quality, and readability in English and Spanish. JAMA. 2001 May 23–30;285(20):2612–21. doi: 10.1001/jama.285.20.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fogel J. Internet use for cancer information among racial/ethnic populations and low literacy groups. Cancer Control. 2003 Sep;10(5 suppl):45–51. doi: 10.1177/107327480301005s07. [DOI] [PubMed] [Google Scholar]
- 23.Soergel D., Tse T., Slaughter L. Helping healthcare consumers understand: an “interpretive layer” for finding and making sense of medical information. Medinfo. 2004;11(pt 2):931–5. [PubMed] [Google Scholar]
- 24.Brashers D.E., Neidig J.L., Goldsmith D.J. Social support and the management of uncertainty for people living with HIV or AIDS. Health Commun. 2004;16(3):305–31. doi: 10.1207/S15327027HC1603_3. [DOI] [PubMed] [Google Scholar]
- 25.Forsythe D.E. New bottles, old wine: hidden cultural assumptions in a computerized explanation system for migraine sufferers. Med Anthropol Q. 1996 Dec;10(4):551–74. doi: 10.1525/maq.1996.10.4.02a00100. [DOI] [PubMed] [Google Scholar]
- 26.Ewing D. Family caregiver Internet experiences: a dissertation. Portland, OR: Oregon Health & Science University; 2003. [Google Scholar]
- 27.Kleinman A. The illness narratives: suffering, healing, and the human condition. New York, NY: Basic Books; 1988. [Google Scholar]
- 28.Tetzlaff L. Consumer informatics in chronic illness. J Am Med Inform Assoc. 1997 Jul;4(4):285–300. doi: 10.1136/jamia.1997.0040285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dervin B. Communication gaps and inequities: moving toward a reconceptualization. In: Dervin B., Voigt M., editors. Prog Commun Sci. 1980(v.2);73–112. Reprinted in: Dervin B, Foreman-Wernet L, Lauterbach E, eds. Sense-making methodology reader: selected writings of Brenda Dervin. Cresskill, NJ: Hampton Press; 2003. [Google Scholar]
- 30.Cline R.J., Haynes K.M. Consumer health information seeking on the Internet: the state of the art. Health Educ Res. 2001 Dec;16(6):671–92. doi: 10.1093/her/16.6.671. [DOI] [PubMed] [Google Scholar]
- 31.Metoyer-Duran C. Information-seeking behavior of gatekeepers in ethnolinguistic communities: overview of a taxonomy. Libr Inf Sci Res. 1991;13:319–46. [Google Scholar]
- 32.Metoyer-Duran C. Information gatekeepers. Annu Rev Inf Sci Technol. 1993;28:111–50. [Google Scholar]
- 33.Gross M. The imposed query. RQ. 1995;35(2):236–43. [Google Scholar]
- 34.Erdelez S. Information encountering. In: Fisher K.E., Erdelez S., McKechnie L.E.F., editors. Theories of information behavior. Medford, NJ: Information Today; 2005. pp. 179–84. [Google Scholar]
- 35.Rioux K. Information acquiring-and-sharing. In: Fisher K.E., Erdelez S., McKechnie L.E.F., editors. Theories of information behavior. Medford, NJ: Information Today; 2005. pp. 169–73. [Google Scholar]
- 36.Fox S. Online health search 2006 [Internet]. Pew Internet & American Life Project; 2006 [cited 1 Mar 2007]. < http://www.pewinternet.org/pdfs/pip_online_health_2006.pdf>.
- 37.Ferguson T. What epatients do online: a tentative taxonomy. Ferguson Rep [Internet]. 2002 Sep;(9) [cited 18 Apr 2008]. < http://www.fergusonreport.com>.
- 38.Lorence D.P., Park H., Fox S. Assessing health consumerism on the web: a demographic profile of information-seeking behaviors. J Med Syst. 2006 Aug;30(4):251–8. doi: 10.1007/s10916-005-9004-x. [DOI] [PubMed] [Google Scholar]
- 39.Ferguson T., Frydman G. The first generation of e-patients. BMJ. 2004 May 15;328(7449):1148–9. doi: 10.1136/bmj.328.7449.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferguson T. Online patient-helpers and physicians working together: a new partnership for high quality health care. BMJ. 2000 Nov 4;321(7269):1129–32. doi: 10.1136/bmj.321.7269.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.La Porta M., Hagood H., Patt J., Hodorowski J.K., Treiman K. The NCI's Cancer Information Service: meeting the public's cancer information needs via the Internet. J Cancer Educ. 2007 Spring;22(1 suppl):S26–34. doi: 10.1007/BF03174343. [DOI] [PubMed] [Google Scholar]
- 42.Lorence D., Chen L. A study of peer-to-peer information in a domain of uncertainty: the case of epilepsy. Health Informatics J. 2007 Dec;13(4):303–16. doi: 10.1177/1460458207082979. [DOI] [PubMed] [Google Scholar]
- 43.Kamel Boulos M.N., Wheeler S. The emerging Web 2.0 social software: an enabling suite of sociable technologies in health and health care education. Health Info Libr J. 2007 Mar;24(1):2–23. doi: 10.1111/j.1471-1842.2007.00701.x. [DOI] [PubMed] [Google Scholar]
- 44.Boase J., Horrigan J.B., Wellman B., Rainie L. The strength of Internet ties: the Internet and email aid users in maintaining their social networks and provide pathways to help when people face big decisions [Internet] Pew Internet & American Life Project; 2006 [cited 20 Feb 2007]. < http://www.pewinternet.org/pdfs/PIP_Internet_ties.pdf>.
- 45.Eysenbach G. From intermediation to disintermediation and apomediation: new models for consumers to access and assess the credibility of health information in the age of Web 2.0. Medinfo. 2007;12(pt 1):162–6. [PubMed] [Google Scholar]
- 46.Morey O. Health information ties: preliminary findings on the health information seeking behaviour of an African-American community. Inform Res [Internet] 2007 Jan;12(2) [cited 25 Feb 2007]. < http://www.InformationR.net/ir/12-2/paper297.html>.
- 47.Spink A., Jaeckel G., Sidberry G. Information seeking and information needs of low income African American households: Wynnewood health neighborhood project. Proc Annu Soc Inf Sci Meet. 1997;34:271–9. [Google Scholar]
- 48.Courtright C. Health information seeking among Latino newcomers: an exploratory study. Inf Res [Internet] 2005 Jan;10(2) [cited 25 Feb 2007]. < http://www.informationr.net/ir/10-2/paper224.html>.
- 49.Warner D., Procaccino J.D. Toward wellness: women seeking health information. J Am Soc Inf Sci Technol. 2004 Jun;55(8):709–30. [Google Scholar]
- 50.Gray N.J., Klein J.D., Cantrill J.A., Noyce P.R. Adolescents' perceptions of the Internet as a health information source. Int J Pharm Pract. 2002;10:R53. [Google Scholar]
- 51.Case D.O., Johnson J.D., Andrews J.E., Allard S.L., Kelly K.M. From two-step flow to the Internet: the changing array of sources for genetics information seeking. J Am Soc Inf Sci Technol. 2004;55(8):660–9. [Google Scholar]
- 52.Østerlund C.S., Doda N.P., Smith C.A. Mother knows best: medical record management for patients with spina bifida during the transition from pediatric to adult care. AMIA Annu Symp Proc. 2005. pp. 580–4. [PMC free article] [PubMed]
- 53.Ybarra M.L., Suman M. Help seeking behavior and the Internet: a national survey. Int J Med Inform. 2006 Jan;75(1):29–41. doi: 10.1016/j.ijmedinf.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 54.Peña-Purcell N. Hispanics' use of Internet health information: an exploratory study. J Med Libr Assoc. 2008 Apr;96(2):101–7. doi: 10.3163/1536-5050.96.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Eng E., Parker E. Natural helper models to enhance a community's health. In: DiClemente R.J., Crosby R.A., Kegler M.C., editors. Emerging theories in health promotion practice and research: strategies for improving public health. San Francisco, CA: Jossey-Bass; 2002. pp. 126–56. [Google Scholar]
- 56.Lester B.S., Prady S., Finegan Y., Hoch D. How online patient networks can enhance quality and reduce errors. Online Patient Netw [Internet] 2004 Oct/Dec [cited 14 Feb 2007]. < http://www.psqh.com/octdec04/lesterfineganhoch.html>.
- 57.Warner D.G., Olney C.A., Wood F.B., Hansen L., Bowden V.M. High school peer tutors teach MedlinePlus: a model for Hispanic outreach. J Med Libr Assoc. 2005 Apr;93(2):243–52. [PMC free article] [PubMed] [Google Scholar]
- 58.Olney C.A., Warner D.G., Reyna G., Wood F.B., Siegel E.R. MedlinePlus and the challenge of low health literacy: findings from the Colonias project. J Med Libr Assoc. 2007 Jan;95(1):31–9. [PMC free article] [PubMed] [Google Scholar]
- 59.Meissner H.I., Anderson D.M., Odenkirchen J.C. Meeting information needs of significant others: use of the cancer information service. Patient Educ Couns. 1990 Apr;15(2):171–9. doi: 10.1016/0738-3991(90)90060-x. [DOI] [PubMed] [Google Scholar]
- 60.Ell K. Social networks, social support and coping with serious illness: the family connection. Soc Sci Med. 1996 Jan;42(2):173–83. doi: 10.1016/0277-9536(95)00100-x. [DOI] [PubMed] [Google Scholar]
- 61.Medalie J.H. The caregiver as the hidden patient: challenges for medical practice. In: Kahana E., Biegel D.E., Wykle M.L., editors. Family caregiving across the lifespan. Thousand Oaks, CA: Sage Publications; 1994. pp. 312–30. [Google Scholar]
- 62.Hepworth M. A framework for understanding user requirements for an information service: defining the needs of informal carers. J Am Soc Inf Sci Technol. 2004;55(8):695–708. [Google Scholar]
- 63.University of North Carolina at Chapel Hill. NC Health Info [Internet] Chapel Hill, NC: The University; 2008 [cited 20 Jun 2008]. < http://www.nchealthinfo.org>. [Google Scholar]
- 64.Jenkins C.G., Marshall J.G., McDuffee D. MedlinePlus goes local in NC: context and concept. J Consum Health Internet. 2004;8(4):1–8. doi: 10.1300/J381v08n04_01. [DOI] [Google Scholar]
- 65.Baker L.M., Manbeck V. Consumer health information for public librarians. Lanham, MD: Scarecrow Press; 2002. [Google Scholar]
- 66.Dervin B. What we know about information seeking and use and how research discourse community makes a difference in our knowing [background paper prepared for Health Information Programs Development, National Library of Medicine, Oct 22, 2001] [Internet] Columbus, OH: Ohio State University; [cited 19 Apr 2008]. < http://communication.sbs.ohio-state.edu/sense-making/art/artabsdervin01nlm.html>. [Google Scholar]
- 67.Glaser B.G., Strauss A.L. The discovery of grounded theory: strategies for qualitative research. Chicago, IL: Aldine; 1967. [Google Scholar]
- 68.Lincoln Y.S., Guba E.G. Naturalistic inquiry. Newbury Park, CA: Sage; 1985. [Google Scholar]
- 69.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res [Internet] 2004 Sep 29;6(3):e34. doi: 10.2196/jmir.6.3.e34. [cited 1 May 2008]. < http://www.jmir.org/2004/3/e34/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Durrance J.C. Factors that influence reference success: what makes questioners willing to return. Ref Librar. 1995;23(49/50):243–65. [Google Scholar]
- 71.Zeng Q.T., Kogan S., Plovnick R.M., Crowell J., Lacroix E.M., Greenes R.A. Positive attitudes and failed queries: an exploration of the conundrums of consumer health information retrieval. Int J Med Inform. 2004 Feb;73(1):45–55. doi: 10.1016/j.ijmedinf.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 72.Toms E.G., Latter C. How consumers search for health information. Health Informatics J. 2007 Sep;13(3):223–35. doi: 10.1177/1460458207079901. [DOI] [PubMed] [Google Scholar]
- 73.Bundorf M.K., Wagner T.H., Singer S.J., Baker L.C. Who searches the Internet for health information. Health Serv Res. 2006 Jun;41(3 pt 1):819–36. doi: 10.1111/j.1475-6773.2006.00510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lambert S.D., Loiselle C.G. Health information seeking behavior. Qual Health Res. 2007 Oct;17(8):1006–19. doi: 10.1177/1049732307305199. [DOI] [PubMed] [Google Scholar]
- 75.Rice R.E. Influences, usage, and outcomes of Internet health information searching: multivariate results from the Pew surveys. Int J Med Inform. 2006 Jan;75(1):8–28. doi: 10.1016/j.ijmedinf.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 76.Cotten S.R., Gupta S.S. Characteristics of online and offline health information seekers and factors that discriminate between them. Soc Sci Med. 2004 Nov;59(9):1795–806. doi: 10.1016/j.socscimed.2004.02.020. [DOI] [PubMed] [Google Scholar]
- 77.Becker G. Order and chaos. In: Becker G., editor. Disrupted lives: how people create meaning in a chaotic world. Berkeley, CA: University of California Press; 1997. pp. 37–58. [Google Scholar]
- 78.Ayers S.L., Kronenfeld J.J. Chronic illness and health-seeking information on the Internet. Health (London) 2007 Jul;11(3):327–47. doi: 10.1177/1363459307077547. [DOI] [PubMed] [Google Scholar]
- 79.Israel B.A. Social networks and social support: implications for natural helper and community level interventions. Health Educ Q. 1985;12(1):65–80. doi: 10.1177/109019818501200106. [DOI] [PubMed] [Google Scholar]
- 80.Wolpe G.L. A crisis of caregiving, a crisis of faith. In: Levine C., editor. Always on call: when illness turns families into caregivers. 2nd ed. Nashville, TN: Vanderbilt University Press; 2004. pp. 34–44. [Google Scholar]
- 81.Kleinman A., Eisenberg L., Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978 Feb;88(2):251–8. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 82.Pettigrew K.E., Durrance J.C., Unruh K. Facilitating community information seeking using the Internet: findings from three public library-community network systems. J Am Soc Inf Sci Technol. 2002;53(11):894–903. [Google Scholar]
- 83.James N., Daniels H., Rahman R., McConkey C., Derry J., Young A. A study of information seeking by cancer patients and their carers. Clin Oncol (R Coll Radiol) 2007 Jun;19(5):356–62. doi: 10.1016/j.clon.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 84.Echlin K.N., Rees C.E. Information needs and information-seeking behaviors of men with prostate cancer and their partners: a review of the literature. Cancer Nurs. 2002 Feb;25(1):35–41. doi: 10.1097/00002820-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 85.Bar-Tal Y., Barnoy S., Zisser B. Whose informational needs are considered? a comparison between cancer patients and their spouses' perceptions of their own and their partners' knowledge and informational needs. Soc Sci Med. 2005 Apr;60(7):1459–65. doi: 10.1016/j.socscimed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 86.Saxton M.L., Richardson J.V. Understanding reference transactions: transforming an art into a science. London, UK: Elsevier Science; 2002. [Google Scholar]
- 87.Turner T., Fisher K.E. Social types in technical newsgroups: implications for information flow. Int J Commun Law Policy [Internet] 2006 Autumn;11 [cited 27 Feb 2007]. < http://www.ciaonet.org/olj/ijclp/ijclp_11/ijclp_11h.pdf>.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.